If a married couple has difficulty conceiving, then the issue of determining a favorable period when they need to have an open sex life begins to be discussed. Perhaps the woman’s egg does not mature. To understand whether there is a problem, it is necessary to determine whether ovulation is occurring by ultrasound. It is during this period that the chance of getting pregnant increases.
The procedure for determining ovulation by ultrasound is called folliculometry. It is a complete diagnosis of the reproductive organs of the expectant mother. On the screen, doctors see how the follicles develop.
How to determine ovulation by ultrasound
Determining ovulation by ultrasound has long been widespread. This method is one of the most accurate. The examination itself is carried out using an ultrasonic sensor. The latter is inserted into the vagina, because this is the only way the uzologist can get an image of the internal organs on the screen. By the way, the procedure does not pose any threat and is not painful. The point is to determine the growth of the dominant follicle, the development of the corpus luteum and the state of the endometrial layer.
As practice shows, the results are understandable only to a specialist. In this regard, there is no need to be shy about asking for explanations. The scheduled scan will be saved on the machine. Based on its results, the doctor will prescribe treatment, if necessary.
What is ovulation
Every woman ovulates once a month (from the Latin ovulum - egg, ovulatio - hatching) - During ovulation, a mature egg leaves the ruptured follicle into the fallopian tube, in which the long-awaited (or unexpected) fertilization occurs.
And now the details. Why do you need to determine ovulation? Ovulation is determined in 2 cases:
- If you need to maximize the likelihood of conception. In this case, knowledge of the time of ovulation (real, not calculated for the average woman). If you are going to get pregnant and you do not have and have not had any problems. The ideal option for you is a urine ovulation test (see below)
- If you tried to get pregnant but didn't succeed. Along with the study of the husband's sperm and tubal patency, ovulation testing is included in the standard protocol for examining infertile couples around the world, according to WHO standards. In this case, it is better to start with a blood test for progesterone and/or Ultrasound monitoring.
How to find out if ovulation has occurred?
The only 100% reliable fact that pregnancy has occurred is pregnancy. All other diagnostic methods are less reliable.
How to determine the most optimal time for conception? The egg lives no more than a day. For fertilization, she needs time - 18-20 hours. Total: if within 10 hours the egg does not meet sperm and is not fertilized, it dies. Sperm live in a woman’s genital tract for up to 5 days (in young married couples with ideal health). Conclusion: The ideal time to have sex is during and before ovulation, not after.
Does it make sense to determine basal (rectal) temperature?
Studying basal temperature is the cheapest and most accessible method of studying ovulation. This is where the positive properties are limited: the method is unreliable, unstable and biased. The rate of misinterpretation (even by a doctor) reaches 50%. A lot for a diagnostic test on which a long-term strategy is based. The mechanism for changing basal temperature is as follows: after ovulation, the corpus luteum produces progesterone, which affects some hidden mechanisms in the hypothalamus, which, in turn, increases the overall body temperature by about ½ degree (0.4 minimum). The most annoying thing is that a registered increase in temperature means that ovulation occurred at least yesterday, and sexual activity should have occurred 2 days ago. That. For planning conception, this method is worse than all others. As for the quality of the corpus luteum, measuring blood progesterone is objective and reliable, compared to measuring the length and amplitude of the temperature rise.
Does it make sense to study ovulation using ultrasound (ultrasound?) On what days of the cycle is it best to do this?
If you have a regular menstrual cycle (on average 25-35 days from the first day of one menstruation to the first day of the next), then ovulation will be confirmed in 9 cases out of 10. It is economically feasible to be examined in absentia (blood test for progesterone, or urinary test for ovulation ). If you have doubts about your hormonal health, it is better to start ultrasound monitoring right away. The dominant follicle begins to grow on the 7th day of the cycle. As a rule, it reaches maturity (diameter 16-20 mm) on the 14-15th day. Previously, it was customary to determine the growth rate of the follicle; there were corresponding growth rate standards. Today, in most cases this is not required.
The main goal of Ultrasound Ovulation Monitoring (USMO) is to “pinch the follicle into a fork” between two observations: on the first examination - a mature follicle, on the second - the corpus luteum, and the fluid behind the uterus (pouring out of the follicle and flowing down, i.e. behind the uterus ). Sometimes it is necessary to examine the corpus luteum in the ovary; it can be seen 2-4 days after ovulation, preferably 5-10 days. A normal appearance of the corpus luteum (ideally examined with color Doppler to clarify blood flow) indicates normal ovulation. Ultrasound monitoring is an observation not only of the follicle, but also of the endometrium, its thickness and structure. The endometrium (from the Greek Endo - inside and metra - uterus) is the mucous membrane lining the uterine cavity, an extremely important element. The endometrium must “prepare” to capture the embryo. This preparation takes ¾ of the menstrual cycle
Why do you need to test your blood for progesterone?
Progesterone (lat. pro gestatio - for pregnancy) is a hormone necessary to maintain pregnancy. Progesterone is the main hormone produced by the corpus luteum of the ovary. The cells lining the follicle quickly (within 1 day) degenerate into corpus luteum cells. The corpus luteum begins to produce the hormone immediately after ovulation, progesterone reaches its peak within 7 days. If a woman does not become pregnant, progesterone decreases. Due to the drop in progesterone concentration, menstruation occurs. A study of the peak of progesterone in the middle of the luteal phase (14 days divided in half, we get 7 days after ovulation, or 7 days before menstruation) tells us about a normally functioning corpus luteum. A normal corpus luteum means normal ovulation. Normal ovulation of 2 menstrual cycles in a row indicates the normal functioning of a woman’s entire endocrine system, and is the basis for refusing further hormone research.
Does it make sense to study ovulation with a urinary LH test?
LH is a luteinizing hormone produced by the pituitary gland. Its main function is the initiation of ovulation, which leads to a change in follicle cells with the formation of the corpus luteum (Corpusluteum - yellow body, lat). The yellow color is a sign of a large number of steroid hormones, remember the egg yolk - the mechanism is the same. The urine test for ovulation, also known as the LH test (commercial preparations Eviplan, Frautest), is for some reason not very popular among Russian patients. But in vain. It is the increase in LH concentration that makes it possible to predict ovulation in advance, and not to be a witness to the current (happened) process. The mechanism of ovulation is very complex. This is a whole cascade of inflammatory changes in the follicle, which takes time. Something around 40-42 hours. Ovulation is triggered by the onset of the LH surge. Thus, knowing the time of the onset of the peak, it is possible to predict approximately the time of the onset of ovulation. Maximizing the likelihood of conception is simple: you need to “live” between the LH peak and ovulation, which can be observed on ultrasound. The opposite is that protection from unwanted pregnancy using this method is not reliable and is not recommended. However, ovulation tests are often considered unreliable and often produce false negative (i.e. erroneous) results. The reasons for this are as follows and should be avoided:
- poor quality test. The manufacturer, as a rule, makes a high-quality test, which can easily be spoiled by storing it in a warm place (humid, sunny, etc.). Be careful, follow all storage rules, a complex chemical reaction occurs in a seemingly simple strip. Don’t forget about control: there should be one control strip in any case; if there is none, the place of the “diagnostic test” is in the trash can.
- wrong time of day for research. Our habit fails us all: urine (blood) must be examined in the morning. That's how it is. Indeed, the rise in LH most often begins at 4-5 am. If you test your blood for LH (it’s expensive, and it’s a shame to inject a vein every day), then the morning is what you need. Yes, only LH enters the urine several hours later. We recommend taking an ovulation test between 16-21 hours.
- incorrect cycle time. Either we have to wait many days for ovulation, or we “slept through it.” Ovulation usually occurs 14 days BEFORE menstruation. It is calculated like this:
Step 1 Calculate the average length of the menstrual cycle over the last 3 months.
Step 2. Using the calendar, we calculate the day when the next menstruation should arrive. Step 3. Count back 14 days. 14 days is the duration of the luteal phase in humans. We get the estimated time of ovulation. Step 4. Count back another 3 days (with a margin of 4). We have received a date from which we must be guaranteed to detect ovulation by the LH peak. EVERYTHING about LH. What is the most reliable method for studying ovulation?
The only 100% reliable evidence of ovulation occurring is clinical pregnancy. Everything else is our (doctors’) indirect ideas about it. Here is an approximate rating of ovulation diagnostic methods with our doctors’ subjective ideas about their reliability:
| Clinical pregnancy | 100% |
| Monitoring ovulation during surgery | 98% |
| Ultrasound confirmation | 95% |
| Blood test for progesterone in the mid-luteal phase | 95-98% |
| Urinary LH test | 75% |
| Basal temperature study | 50-60% |
| Research of so-called tests functional diagnostics | 30-60% |
What is the most convenient method of ovulation research?
Another question immediately arises: is it convenient for the doctor or for the patient? This depends on the distance of the patient from the clinic. If it is possible to test your blood for progesterone in a good laboratory, do so. If there is no laboratory nearby, the best test method is a urinary LH test. If you have doubts about your hormonal health (irregular cycle), the best option is ultrasound ovulation monitoring.
How often does ovulation occur normally?
Every month. The ovaries can allow themselves to “rest” for 1-2 cycles a year. As a rule, during times of stress (heat, cold, exams, moving), nature turns on security mode. There is no peak of hormones, ovulation is canceled. A woman’s 9-10 cycles a year are “ovulatory”. Closer to 40 years of age and, especially older, ovulation occurs somewhat less frequently.
When should you think about problems with ovulation?
If you have observed ovulation for 2 cycles in a row, you have no problems with hormonal health. If there was ovulation in the 1st cycle, not in the other, we observe it in the 3rd cycle, if it is there, everything is fine. Irregular menstrual cycles (cycles less than 25 or more than 35) are associated with ovulation pathology.
When should you stimulate ovulation?
In cases where it is absent (anovulation) or rare (oligoovulation). Before stimulation, the doctor must find out its reasons. Various endocrine disorders can catch up with you during pregnancy, causing miscarriage. Tumors of endocrine health organs are also not added. Diagnosis of endocrine problems will be discussed in separate sections.
What is corpus luteum deficiency?
This is a lack of production of corpus luteum hormones. Diagnosis of this condition has traditionally been based on measuring basal temperature. Today, a blood test for progesterone is a more reliable diagnostic method. Ultrasound can also provide additional information. Often, corpus luteum deficiency is not an independent disease. It is usually a sign of “poor” ovulation.
Conclusion.
Diagnosing ovulation and ovulation problems is not a difficult task for an experienced doctor. This material will help you speak the same language with your doctor and make your communication more productive and achieve the desired result with minimal losses - the birth of the desired baby. We are always happy to help!
Preparation
Since the examination is classified as planned, preparation takes place. In particular, doctors advise:
- go to the ultrasound specialist’s office with an empty bladder;
- 2-3 days before the procedure, the patient is advised to stop drinking alcoholic beverages;
- It is better to avoid foods that can cause gas. These include peas, milk, raw vegetables, legumes, carbonated water;
- The last meal should be 12 hours before the procedure.
When is it more effective to do an ultrasound?
To detect ovulation, ultrasound examinations need to be performed about four times. It is during this period that the specialist has the opportunity to monitor the entire process during which the egg matures.
The procedure is carried out every 2-3 days:
- the first is done on the tenth day of the menstrual cycle (prerequisite: the classic cycle is 28 days);
- the second – on the 13th day in order to confirm the presence of a dominant type follicle;
- the third - on the 14th day, when ovulation should occur;
- the fourth is a control procedure and is carried out three days later; necessary in order to finally verify the occurrence of ovulation.
The time of the first ultrasound session may be slightly changed. With a regular menstrual cycle (but it is longer or shorter than usual), the first procedure is carried out four days before the middle. When the cycle is inconsistent, a diagnostic test can be performed four days after menstruation ends.
How does the diagnostic process work?
After the attending physician has determined the date of the study, the woman must come on the appointed day. The procedure itself is very simple, it can be carried out in three ways:
- transvaginally. Then the capsules are examined through the vagina. A condom is placed on the sensor, after which it is inserted inside. After a while, the doctor can assess the condition of the internal organs. By the way, this method is not used if the girl is a virgin or pregnant;
- transbdominal, that is, externally. A special gel is applied to the pubic area, and then a special device is moved over it. A little preparation is needed here, because the scan is done on a full bladder. By the way, this method is considered less informative;
- transrectally, that is, through the anus. On the screen, the ultrasound specialist sees the condition of the ovaries. You should immediately warn about the high degree of pain of this method. It is used if the patient is elderly or a virgin.
When a computer analysis is prescribed for the purpose of pregnancy planning, the first method is used.
In what cases is it necessary to do an ultrasound for ovulation?
Ultrasound examination for the presence of egg maturation is most often carried out for the purpose of pregnancy planning. It is actively used by couples who cannot get pregnant for a long time. At the same time, constant attempts do not give the desired results.
There are many ways to monitor the maturation of an egg - this is by plotting a basal temperature chart, calculating the required days on the calendar, and using special tests.
Special devices have also been developed to determine the level of necessary hormones in saliva. But pelvic ultrasound is considered the most effective; it is this kind of monitoring that almost without error determines the period most suitable for fertilization.
None of the indirect signs can accurately indicate when to expect a positive result. Only an ultrasound examination, interpreted by a specialist, will determine the upcoming pregnancy.
Folliculometry is also necessary in the following situations:
- planning conception after an unsuccessful pregnancy, miscarriage or abortion;
- preparation for artificial insemination - IVF requires careful preparation, and computer diagnostics is the most important stage of planning;
- absence of menstruation for a long time (the phenomenon is called amenorrhea);
- infertility treatment;
- Irregular menstruation: for many girls, menstruation occurs with long delays, and any deviations indicate problems in the body or hormonal imbalances;
- painful periods: severe pain during menstruation is an indicator of problems in the body, this phenomenon sometimes harms the entire reproductive system;
- when identifying diseases associated with disrupted hormonal levels.
As you can see, the list of indications when diagnostics need to be done is long. The harm of ultrasound is minimal in comparison with the results obtained in the process.
You will learn important details about the procedure from the video:
Possible violations
It happens that after visiting folliculometry, the doctor discovers a pathology. This is about:
- regression. It represents the growth of the follicle to a certain size, but at a certain point the enlargement of the membrane stops and goes in the opposite direction;
- peristence. This is normal development of the capsule, however, in the end the egg does not come out;
- follicular cyst. Liquid accumulates due to the integrity of the shell;
- luteinization. The corpus luteum forms, but does not rupture.
When such abnormalities are detected, the study is postponed until the patient gets better.
Signs of ovulation on ultrasound
How will the doctor understand that ovulation has occurred? On the screen he will see signs that will confirm the release of the egg.
- Before the ovulation process itself (somewhere on the third visit to the uzist), maturing follicles were discovered;
- follicle rupture was noticed;
- examination behind the uterus showed accumulation of fluid;
- after the follicle ruptured, ultrasound detected the growth of the corpus luteum;
- the absence of a dominant follicle is the main sign of ovulation.
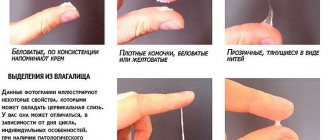
Additional confirmation that ovulation has occurred will be the presence of a large amount of progesterone in the blood. A woman can also indirectly determine that she is ovulating. Signs:
- nagging pain in the abdomen;
- viscous vaginal discharge;
- swelling of the mammary glands;
- change in taste preferences;
- increased appetite;
- frequent mood changes.
Decoding the results
Many people will ask what ovulation looks like on an ultrasound. Only a specialized specialist can know this. Several rounded membranes are often observed on the screen; if one of them is ruptured, then the mature oocyte is ready for fertilization. During the study, the following indicators are determined:
- object growth phase;
- from 1 to 8 days there is nothing;
- the next four days the size of the object increases to 10 mm;
- 12-14 days after the start of the cycle, the indicator reaches 15 mm;
- 15-15 days – 21 mm;
- rupture process;
- the oviparous tubercle is visible;
- the wall thickens;
- if ovulation has occurred, the membrane is no longer visible;
- the corpus luteum is formed;
- in the case of menstruation, small balls are visible, not reaching 8 mm.
Ultrasound to determine ovulation: when to do it, what it looks like
Every woman should know the answer to the question of what an ultrasound for ovulation is and when to do this procedure. After all, accurately determining the day of ovulation helps to understand which days conception is most likely.
Most women do not know how to independently determine the ovulatory period. This becomes a significant obstacle on the path to motherhood.
The ultrasound method for determining ovulation by ultrasound is a solution to this problem.
What is ovulation?
A woman's menstrual cycle consists of several stages. It begins with menstruation, during which the endometrium is removed from the woman’s body. Menstruation usually lasts from 3 to 7 days. After this, follicles begin to mature in the woman’s ovaries.
Approximately 10 days after the start of menstruation, one of the follicles becomes dominant. By the middle of the cycle, the follicle becomes thinner, bursts and releases an egg, which moves through the fallopian tubes and is ready for fertilization. This process is called ovulation. The treated follicle turns into a corpus luteum. If conception does not occur, then a new menstruation begins.
[]glT8feZKu7k[/]
The main signs of the onset of the ovulatory period
Women who know the characteristics of their body well can easily determine the onset of ovulation. But many people mistakenly believe that it should be in the middle of the cycle. And some people think that the release of the egg occurs on the 14th day after the start of menstruation. In fact, it depends on various factors, the main one of which is stable hormonal levels.
Knowing the duration of the menstrual cycle plays a significant role in determining the favorable day of conception. On average it lasts 28 days. In this case, ovulation occurs around day 14. But longer or shorter cycles often occur.
For example, if the menstrual cycle lasts 33 days, then the release of the egg will be approximately on the 19th day. In order to calculate the expected release date of the egg, it is necessary to subtract 14 days from the number of days in the cycle.
This is how long phase 2 lasts for most women.
The most common signs of the ovulatory period are:
- Change in consistency of discharge. Discharge 2 days before the release of the egg changes its consistency to a more viscous one, similar to transparent mucus. Many people compare this discharge to egg white. This consistency helps maintain sperm viability for a long time.
- Change in basal temperature. In the first half of the cycle, the basal temperature reaches approximately 36.8°C. By the day the follicle matures, it rises to above 37°C. A few days before your period, your basal temperature drops sharply.
- Aching pain in the ovary. Quite often, women feel the onset of ovulation precisely because of the appearance of pain in the ovary, in which the dominant follicle bursts.
- Increased sex drive. Ovulation is a factor influencing sexual arousal.
- Swelling of the mammary glands. This sign is not present in everyone, and it is the least reliable, because Breast swelling occurs not only during the release of the egg, but also before the onset of menstruation.
The need for ultrasound examination
If we consider a standard menstrual cycle of 28 days, then the first ultrasound should be done approximately on the 10th day. For a cycle exceeding 28 days, you need to do this procedure 3 days before the middle of the cycle.
If the cycle is irregular, then it makes sense to start doing an ultrasound examination immediately after the end of menstruation. The diagnostic procedure should be repeated once every 2 days until ovulation occurs.
If it does not occur, then observation is scheduled until the start of the next cycle.
The examination is carried out using a transvaginal sensor, which is inserted into the vagina. Before diagnosis, the patient should empty her bladder to obtain the most accurate results. During the ultrasound procedure, a pillow is placed under the patient's pelvis to maximize the view.
During an ultrasound to determine ovulation, the doctor pays attention to the presence of anechoic formations. Ultrasound pays special attention to what the dominant follicle looks like. In the middle of the cycle, the average follicle reaches 2 cm in diameter. There are cases when 2 dominant follicles mature. In such situations, the likelihood of a multiple pregnancy is very high.
In addition to the dominant follicle, the doctor evaluates other indicators: the presence of fluid behind the uterus, the presence and size of the corpus luteum. Thanks to a comprehensive assessment of all indicators, it is possible to identify the overall picture of the patient’s hormonal status and the presence of any abnormalities and diseases.
What deviations can be detected using the procedure?
The purpose of ultrasound to determine the ovulatory period is not only to determine the most favorable days for conception, but also to identify problems in the female reproductive system. For example, some people experience anovulatory cycles frequently. These are cycles in which the process of follicle development is disrupted and the release of the egg does not occur.
[]yVz_M6JNhaY[/]
The most common case is follicle regression. The dominant follicle grows and develops, but then stops developing and shrinks. A fairly common disorder is a follicular cyst. The follicle develops to the desired size, but does not burst. Liquid accumulates in it.
A follicular cyst may burst with the onset of the next menstruation, or it may last for several cycles. A follicular cyst is a benign formation and, as a rule, does not require surgical intervention. Its treatment is carried out with medication. Often with a follicular cyst, menstruation is delayed.
If the cyst is small, it may go unnoticed. Cysts larger than 8 cm in diameter often cause pain in the ovarian area.
Transvaginal ultrasound to determine ovulation is a harmless procedure, so it is recommended not only for women planning a pregnancy, but also for those who are concerned about their health.
Source: https://daohotei.com/medicina/ginekologiya/uzi-na-ovulyatsiyu
Why ovulation may not show
Certain methods for determining a favorable phase for conception may show different results. Expectant mothers often wonder why this happens.
Some use the method of measuring basal temperature, but there are also those who purchase pharmacy tests. The latter show a response based on the LH hormone. If it rises, in theory, “day X” comes. However, tests can be flawed, and ultrasound is the most reliable way to determine the release of an egg.
At the same time, in fact, the water membrane did not burst and the egg remained in place. By the way, incorrect results may be shown if the patient has not properly prepared for the examination.
When to do it?
Many will ask when is the best time to do an ultrasound for ovulation. According to doctors, you need to go for the first folliculometry:
As a rule, diagnostics are done at least three times, the frequency should be two days. If the oocyte is not released, the examination continues until the next bleeding begins. Diagnostics are also prescribed a week after the follicle bursts in order to confirm earlier results. Doctors also refer the woman for a blood test, which should show an increase in progesterone.
What is observed in the second phase
At this stage we are talking about the corpus luteum. Its norm is 12 mm; the appearance of this element means the success of the process and the body’s readiness for pregnancy.
Computer research is the main method for monitoring the formation of the corpus luteum. A week after the day of ovulation it increases to 20 mm. When the indicator increases to 30-40, a cyst is diagnosed. If the mark is fixed at 20-30 mm, then this indicates a normal pregnancy.
If a woman is already carrying a child, then it makes sense to use a gestational age calculator using ultrasound.
The purpose of ovarian ultrasound - what can be seen
Tracking ovulation using ultrasound is the main purpose of folliculometry. The study shows not only folliculogenesis in dynamics, but also the ovarian reserve, various pathologies of follicle formation. By diagnosing the condition of the appendages, the development of more than 20 pathologies can be prevented.
Ultrasound diagnostics can detect the following ovarian conditions:
- Norm. When performing an ultrasound, ovulation represents the presence of fluid in the ovary and the movement of the egg towards the fallopian tubes.
- Polycystic. The presence of more than 26 follicles in the ovaries.
- Regression. The dominant follicle in the ovaries, instead of releasing the egg, begins to shrink.
- Persistence. The size of the follicle reaches its maximum, its growth stops, but the membrane does not burst.
- Follicular cyst. Abnormal growth of the germ cell - from 40 mm, the release of the egg does not occur.
- Luteinization. The development of the corpus luteum begins before the release of the gamete; hormonal levels are normal.
- Lack of follicle. 2-4 follicles are identified, which grow up to 8 mm, after which their regression begins.
Almost all pathologies of folliculogenesis are associated with disturbances in hormone levels, therefore, for a successful pregnancy, the doctor must prescribe hormonal therapy.
Ultrasound for ovulation and pregnancy
Ovulation can be determined after at least 4 sessions. To track the attachment of the fertilized egg, it is necessary to conduct an examination 6 and 8 days after the release of the gamete.
Normally, during the first examination, the doctor should detect the growth of several follicles of equal size from 2 to 6 mm in one of the ovaries. At the second visit, you can accurately determine the dominant follicle in the ovaries, the size of which reaches 8-9 mm. The third study reveals the preovulatory state of the follicle - it grows to 32 mm.
The fourth examination is carried out the day after the third. When performing an ultrasound, ovulation is distinguished by the presence of fluid inside the ovary, the egg is sent to the fallopian tubes. A parallel study of hormone levels is possible.
After the release of the egg, a study is carried out to detect the development of the corpus luteum at the site of the burst follicle. Additionally, examination may be carried out to monitor the condition of the endometrium and the attachment of the fertilized egg.
How long does the ovulation cycle last?
The female body lives according to a certain cycle - menstrual, or monthly. The ideal cycle lasts 28 days - from the beginning of one menstruation to the beginning of the next. But this period may vary for each woman and is 21-35 days. A deviation from the norm of more than 10 days is already considered a pathology and requires a visit to the gynecologist.
The monthly cycle consists of 3 phases:
- Folliculogenesis is the maturation of follicles.
- Ovulation is the release of an egg from the follicle.
- The luteal phase is the degeneration of the ruptured follicle into the corpus luteum.
Follicles are the main component of female ovaries; they are a kind of mini-incubators in which eggs mature for the time being. The supply of follicles in a girl’s eggs is created in the mother’s stomach, and then used up throughout life.
In the first phase of the female cycle, the follicle goes through several stages: primordial (still immature), primary, secondary and tertiary. At the last stage, the follicle is also called the Graafian vesicle - it is a mature cell that is completely ready for ovulation.
Ovulation is the shortest phase, lasting only a few minutes. Usually occurs on the 14th day of the cycle. If it doesn’t last 28 days, then it’s in the middle. At this moment, the follicle bursts, an egg emerges from it and rushes through the fallopian tube into the uterus.
If fertilization does not occur, the egg dies (after 1-5 days), and then the third phase begins - the luteal phase. Having done its job, the follicle connects with connective tissue cells, fills with adipose tissue and turns into the corpus luteum. It begins to produce progesterone, and then gradually resolves over 14-15 days. Then comes menstruation.
The cycle is divided into two parts: the first part of the menstrual period is approximately 7-11 days. At this time, the follicle has matured, and a mature egg is then released from it, ready to be fertilized. After this, the egg, once in the abdominal cavity, is captured by the ampulla of the fallopian tube and begins to move in it. At this moment, sperm should move towards her. If this happens, pregnancy will most likely occur.
The luteal phase begins with ovulation, which lasts 14 days, regardless of how long the menstrual cycle is. During this period, the corpus luteum has matured in the ovary, which helps maintain fertilization at first. If spermatozoa are not encountered on the way to the egg, fertilization does not occur, then the corpus luteum dissolves, the egg dies, the level of hormones in the body decreases, and menstruation begins.
When the last day of menstruation has passed, all the processes described above will begin anew and will be repeated until fertilization occurs. Therefore, the normal course of ovulation in the female body is extremely important!
The ovulation cycle may be disrupted in the following cases: if a woman has had an abortion or pregnancy. After an abortion, the body recovers in about 3 months. Ovulation will be difficult to predict and if there was a delivery, the recovery period after this is about a year.
There are also other reasons why the ovulatory cycle is disrupted:
- Prolonged physical activity.
- Disturbed nutrition.
- Excess weight. Women who suffer from this problem are at risk of hormonal imbalance, so the ovulation process is also disrupted.
- Endocrine factors. Malignant or benign neoplasms, circulatory disorders, taking certain hormonal drugs, disorders or diseases of the thyroid gland - these factors disrupt the functioning of the pituitary gland, so the ovulation process is disrupted.
- Unruptured follicle syndrome. Unfortunately, most often this is the reason why women become infertile. In a normal state, when ovulation occurs, the follicle ruptures and pushes the finished egg into the abdominal cavity, then it enters the fallopian tube and slowly moves along it, but with this syndrome this does not happen, which leads to greater problems with conception. The unruptured follicle then turns into a cyst, and pregnancy does not occur.
- Luteal phase disturbance. The luteal phase is the second (final) phase. Disruption of the luteal phase is a disruption of the endocrine gland, or corpus luteum. In this case, the following may be observed: delayed menstruation, heavy or scanty discharge, infertility or inability to bear a child, etc. Disturbances in the course of this phase can occur due to abortion, starvation, or diseases of the reproductive system.
Methods for determining ovulation
Since the receipt of data on the nature of conception and the regulation of the menstrual cycle, scientists have proposed various ways to control ovulation. To tell the truth, many of them, even very old ones, have not lost their relevance to this day.
- Cervical mucus tension method. Even ancient healers noticed that under the influence of some factors in the middle of the cycle, a woman’s vaginal discharge takes on a special character. This is a profuse, transparent mucous discharge, very similar to the white of a raw egg. The cervical mucus tension method is based on the fact that at the peak of ovulation, the combination of sex hormones determines the maximum viscosity of the mucus - that is, a drop of mucus from the cervix can be stretched between the legs of the tweezers by 5 centimeters or more.
- The “pupil” symptom is based on the same cervical mucus. Considering the large amount and high viscosity of mucus on the day of ovulation, gynecologists, when examining a woman in the mirror, noticed an interesting phenomenon - the cervical canal was stretched by a clot of mucus and looked like the pupil of an eye.
- The symptom of crystallization of cervical mucus was discovered a little later, with the invention of microscopes and magnifying devices. One of the gynecologists came up with the idea to study cervical mucus under a microscope. This is how another interesting phenomenon was discovered - the fern symptom. At the peak of ovulation, under the influence of hormonal levels, the mucus dried on the glass formed a picture resembling a fern branch. When trying to get such a picture on other days of the menstrual cycle, such beauty was not found.
- Basal temperature tests. This is a labor-intensive and discipline-requiring, but extremely accurate method for determining ovulation and the fullness of the phases of the menstrual cycle. Basal (rectal or vaginal) temperature is measured daily with a regular thermometer in the anus or vagina. Measurements should be taken every day in the morning after a night's sleep, without getting out of bed. The obtained data is presented in the form of a graph. Normally, an ovulatory surge is considered to be a temperature difference of more than 0.4 degrees Celsius . Thus, ovulation is the highest peak temperature on the graph.
- Ovulation tests. These test strips are freely available in many pharmacies and are relatively inexpensive. The principle of operation of ovulation tests is similar to pregnancy tests, that is, the test reagent evaluates the concentration of certain hormones characteristic of the ovulatory peak in the urine.
- Ultrasound folliculometry or ultrasound monitoring of ovulation. This is a modern, very reliable and indicative method of monitoring ovulation.
https://youtu.be/yGBZC2VZCeM