The human papillomavirus is considered one of the most dangerous, as it can cause cancer, and also has the highest mortality rate. However, today there is a vaccine against it, which we will talk about in our article.
The human papillomavirus (HPV) is one of the most dangerous. It can cause different types of cancer, the most dangerous of which is cervical cancer. Today, many women die from it. The danger of the virus also lies in the fact that it cannot be cured. So it remains in the body forever. However, it is possible to prevent infection or the development of cancer through vaccination. We will talk about it with you further.
Human papillomavirus is a cause of cancer
Human papillomavirus
If we look at the statistics, we will see that in Russia alone, every year 250 thousand women are found to have formations of various types on the cervix. In developed countries, the statistics are far from reassuring. By the way, among women, cervical cancer is one of the common causes of death.
We have already named the papilloma virus as one of the main causes of cancer. This infection is most common among women. The highest risk of infection concerns women who smoke, have chronic inflammation, and weak immunity. Even the immune system of a healthy person is not able to cope with the virus. So only with timely vaccination can you ensure reliable protection.
Up to what age can you get vaccinated?
The human papillomavirus vaccine is given between the ages of 9 and 25-26 years. During this period, a person is either not sexually active or has just started; the likelihood of carrying the virus is low. As a result of vaccination, immunity is formed for a long time (minimum 5 years). Revaccination is not carried out.
If a person is not infected with HPV types 6, 11, 16, 18 and is over 26 years of age, he can be vaccinated.
Vaccination against persistent human papillomavirus in the body is ineffective
What are papillomaviruses?
Papillomaviruses are a separate group of 150 species. They are found all over the world and can seriously harm your health. 99% of infected women typically develop cervical cancer.
The papilloma virus is not harmless for men either. Regardless of gender, the following types of cancer can form:
- Anal cancer
- Cancer of the mouth and pharynx
- Vaginal and vulvar cancer
- Penis cancer
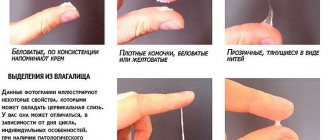
Depending on the strain that enters the body, other diseases and not necessarily cancerous ones may develop. For example, the virus can manifest itself as genital and skin warts. In rare cases, warts appear on mucous membranes.
How is vaccination carried out?
Either of the two vaccines is available in syringes and vials. This vaccine is stored in the refrigerator, but the drug should not be frozen.
Gardasil
After the first injection, they wait 1.5-2 months, then do the next one. The third injection is given after 4-6 months.
Cervarix
The second injection is administered a month after the first, the third injection six months after the second.
Each of the drugs must be injected into the thigh or shoulder and only intramuscularly - this is mandatory. If you just give a subcutaneous injection, there will be no result. After a full course of three vaccinations, the body becomes protected from HPV a month after the third injection.
How is HPV (human papillomavirus) transmitted?
How is HPV transmitted?
Despite the fact that HPV is very common, it has only one method of transmission - through sexual contact. As a rule, immediately after infection and for some time, a person does not feel any changes in the body, since everything happens without symptoms. But you shouldn’t quickly run to your partner with a showdown, because he himself may not know that he has infected you.
By the way, high infection rates are precisely related to the absence of symptoms. For example, you had one partner who infected you and then another appeared, and you yourself still do not know that you are infected. It turns out that the second partner is also infected. And this is how transmission from one to another takes place. A similar situation occurs with HIV or even herpes. Therefore, if you are not too confident in your partner, then you should protect yourself, at least with a condom.
Contraindications and side effects
Before starting vaccination, the doctor must carefully examine the patient and identify possible contraindications. They are:
- pregnancy (with the introduction of Cervaix);
- acute and chronic inflammatory diseases in the active phase;
- hypersensitivity to the components of the drug;
- allergic reactions that occurred during the administration of the first dose of the vaccine;
- pregnancy (due to insufficient knowledge of the effect of the drug on the fetus).
Immediately before vaccination, the attending physician measures the patient’s temperature, examines and auscultates the lungs. If there are no symptoms of colds or other acute diseases, vaccination is permitted.
Despite the fact that the administration of the vaccine is not contraindicated during lactation, experts do not recommend vaccination for breastfeeding women, since this creates an additional burden on the body and can lead to allergies in the child.
Complications from vaccination include allergic reactions - skin rash, urticaria, Quincke's edema and anaphylactic shock. That is why patients are recommended to remain in a medical facility under the supervision of specialists for 30 minutes after vaccination.
The reaction to the vaccine is slight redness and swelling in the area where the drug was administered. Some patients may experience fever, nausea, muscle pain and headaches.
Important to remember! The HPV vaccine has been given to men and women around the world for 10 years. In the vast majority of cases, the vaccine is well tolerated and rarely causes side effects. Over the entire period, only 0.03% of deaths after vaccination were recorded, and in each case they could be associated with other factors.
What do vaccines against HPV (human papillomavirus) consist of?
There are two types of vaccines for this virus, and both of them consist of its empty shell. The vaccine does not contain the DNA of the virus, and therefore it is impossible to become infected through vaccination. Vaccination prevents future infections.
The most dangerous strains today are HPV strains 16 and 18. They provoke the occurrence of cancer of the uterus and anus. In addition, in rare cases, they can cause cancer in other organs.
HPV vaccine
- HPV vaccines are designed to protect against infection and prevent cervical cancer
- The reliability of both vaccines has been proven
- Each vaccine contains an outer shell of the virus and cannot cause infection.
- Vaccination is carried out using intramuscular injections. Three doses given over 6 months
However, there are differences between vaccines:
- Gardasil serum helps protect against HPV strains 6 and 11, which lead to the formation of genital warts. It can be used by both men and women, but in Russia it is registered only for males.
- This serum was tested and approved as a vaccine. It protects against cancer of the vagina, vulva and anus.
- But the second vaccine, Cervarix, is intended for women without age restrictions.
Indications for vaccination
Modern drugs Gardasil and Cervarix are not able to resist emerging infections, so they are administered only to uninfected people in order to create artificial immunity.
Vaccination is given for:
- Prevention of the development of cervical cancer and other oncopathologies of the reproductive organs in women.
- Prevention of cancer of the rectum and penis in men.
- In order to reduce the risk of the formation of precancerous diseases of the genital organs in men and women.
- Preventing the occurrence of genital warts in the anogenital zone.
Since HPV most often enters the body through sexual contact, it is better to administer the vaccine before the start of intimate life. The maximum effect of vaccination is achieved when the drug is administered to adolescents 10-14 years old. The instructions indicate that they can be carried out in women up to 25 years of age, however, with age, the effect of the product decreases.
When the drug is introduced into the body, which already contains pathogenic viruses, vaccination cannot get rid of them, however, according to some experts, it reduces the oncogenic effect. That is why the vaccine can be administered to women under 45 years of age on the recommendation of a doctor if there are indications (complicated heredity, the presence of several risk factors for the development of cervical cancer).
Important! If the girl has already had sexual intercourse, it is better to undergo a serological or PCR test to determine the presence of HPV in the body. If tests reveal highly oncogenic strains of HPV in the body, vaccination is considered inappropriate and is prescribed quite rarely.
Who is the HPV vaccine for?
Who is the vaccine for?
The best time for vaccination is 9-16 years. Ideally, the vaccine should be given before sexual activity begins. This is due to the method of transmission of the virus, and you can become infected already during the first sexual contact. So you shouldn’t joke about it and get all your vaccinations on time.
If the vaccine is given at a later age, after 25 years, then its effectiveness will not be as high. Although, it still exists.
Contraindications
Vaccination must be authorized by a physician and immunologist. Contraindications for its implementation include:
- infectious diseases at the acute stage;
- chronic diseases of the kidneys, liver and other organs;
- presence of diseases caused by HPV;
- allergic reaction to the first dose of the vaccine;
- hypersensitivity to any component of the drugs;
- pregnancy (with vaccination with Cervarix).
The consequences for the child of vaccination with Cervarix during pregnancy have not been studied. The same applies to the lactation period. In this case, you should either use the second vaccine or postpone it. The drug "Gardasil" has passed all studies and is considered absolutely safe for the child, both during pregnancy and during breastfeeding.
Vaccination against HPV (human papillomavirus) - is there a danger: common myths
Adverse reactions
Side effects
All opponents of vaccination believe that there is a high risk of adverse reactions. Supporters argue that the vaccine does not contain viral DNA, which means there is no significant burden on the immune system. In addition, the possibility of use during pregnancy and lactation also indicates safety. It is also important that vaccination is also permissible when taking other drugs, the main thing is that the regimen and dose do not change.
No effect
This is another argument against. In many countries, this vaccination is included in the list of mandatory ones, and numerous studies have proven that the risk of infection is reduced. Thanks to the use of the vaccine, infections have been reduced to a minimum.
Over the past few decades, large studies have continually been conducted to evaluate the effects of the vaccine. It has proven almost 100% effective after a full course of treatment.
This means that the effectiveness has been confirmed. In addition, it has been proven that the vaccine produces cross-immunity, allowing the body to resist other types of HPV that are not included in the vaccines considered.
Infertility
There is an opinion that vaccines against viruses cause infertility and other complications in women. But those who claim this do not take into account the fact that they have been successfully used for more than 10 years and this makes them no longer infertile. And before mass vaccination began, research was carried out for another 5 years.
You can get infected with a virus
Can you get infected from a vaccine?
Let us repeat once again that, contrary to all claims, the virus cannot enter the body through the vaccine. The vaccines used in Russia do not contain the virus, but only fragments of the capsule. Moreover, they are grown in laboratories. It is against them that the body learns to develop protection.
You can become infected by frequently changing partners
Undoubtedly, the infection is sexually transmitted. As we noted above, 80% of the population is infected with this infection. But supposedly only those who often change partners can get the active virus.
English scientists observed girls aged 15-19 years. The experiment lasted three years and after it ended, it turned out that 43% of girls with one partner had an infection. So you don’t have to have many partners to get infected, just one is enough. Although, promiscuity is also bad, because it significantly increases the risk of infection.
Having warts or papillomas on the genitals increases the risk of cervical cancer
Today there are 150 types of HPV. To the joy of many, they are not all oncogenic. For example, the growth of warts on the hands, genital warts and others. It's not all that dangerous. Strains 16, 18, 31, 33, 35 and 39 can lead to cervical cancer. As a rule, when a dangerous strain enters the body, no symptoms appear, and therefore you may not even understand that this has happened.
HPV is a curable disease
HPV is incurable
Today there is not a single remedy that could cope with HPV. Despite this, many clinics offer it. It’s just this way that doctors just make money and nothing more. Unlike herpes, which once it appears remains forever, the papilloma virus can disappear and not manifest itself in any way. In any case, this happens in 75% of situations. This often happens to young girls who have just lost their virginity. Because of this, research is not carried out until age 25 or even 30. It is worth considering that if a dangerous strain has entered the body, the risk of cancer increases significantly.
The vaccine can only be given to girls aged 11-13, and boys do not need it
You can get vaccinated against HPV at any age. More precisely, there is a lower limit, but it is better if the vaccine is administered before the virus enters the body. In other words, before the first sexual intercourse. Another argument in favor of getting vaccinated as early as adolescence is that cervical cancer develops quickly in young people. By the way, this is precisely why in girls under 25 years of age it is most often found in the last stages. As you understand, treatment can’t fix much.
In Western countries, every teenager is vaccinated, not just to prevent infection, but also possible diseases. Vaccination is allowed up to 45 years of age, and later if necessary. This increases the chances of preventing a terrible disease.
Adolescents receive two vaccinations, and adults receive three. Even if you get vaccinated once, the protection will already begin to take effect. Preliminary tests to determine HPV are not required because the virus is most likely already present in the body.
The vaccine protects against all dangerous strains
Today, the vaccines used in Russia allow protection against the 4 most dangerous strains, which helps prevent cancer in 70% of cases. In the West, the 9-valent vaccine is used and it is more effective - 90%. Perhaps such a vaccine will reach Russia, but for now it is better to use at least what is available.
You must understand that despite all the contradictions, you will not find information in any source that papillomavirus can be treated. The only way to protect your family is through vaccination.
Who gets vaccinated against the virus?
The HPV vaccine is used for children and adolescents. It provides 100% protection against strains with a high risk of developing cancer. There are two drugs on the drug market:
- Gardasil (Holland). Protects against types 6, 11, 16 and 18 of the virus.
- Cervarix (Belgium). Countersacts HPV types 16 and 18. Applies to girls only.
Please note that this vaccination does not provide protection against various sexually transmitted diseases. It is also not a contraceptive.
Up to what age can you get vaccinated?
Many people are interested in the age at which vaccinations are carried out. Anyone under 26 years of age can get vaccinated. In world practice, vaccination is given to children aged 9-14 years, and adolescents aged 18-26 years. WHO considers the ideal ages for vaccination to be 10-13 years and 16-23 years.
READ ALSO: possible side effects from the measles, rubella, mumps vaccine in a 6-year-old child
The most rational option is to vaccinate before the first sexual intercourse. That is why in the USA and some developed European countries, children of both sexes aged 10-14 years are subject to mandatory vaccination. Additionally, it can be carried out for girls under the age of 26 who have not been infected with HPV. The fact is that the child’s body responds better to vaccination and receives more powerful protection against papillomavirus, which significantly reduces the likelihood of developing cancer in the future.
HPV vaccination schedule
Vaccines are sold in special syringes or 0.5 ml ampoules. They are stored in the refrigerator. Vaccination can be done at the nearest clinic, gynecological department of a public hospital and a private clinic. Vaccinations are done according to the following scheme:
- Cervarix is administered according to the schedule: the first vaccine, a month later - the second, after 6 months - the third. It is permissible to carry out vaccination according to the accelerated option - the third vaccination is carried out 3-4 months after the second.
- Gardasil is used according to a similar scheme: the first vaccine, after 1.5-2 months - the second, after 6 months - the third (with accelerated vaccination after 3-4 months).
To produce antibodies, the body needs to complete the entire course of vaccination. Immunity to the disease is developed within a month after completing the course.
The drugs are injected intramuscularly into the shoulder or thigh. It is strictly forbidden to do intravenous, subcutaneous and intradermal injection, since antibodies are not produced in this case.
Is vaccination necessary if you have the virus?
Before vaccination, young people and girls who are sexually active are required to be tested for the presence of papillomavirus types 6, 11, 16 and 18. If the result is positive, vaccination is usually not carried out. However, recent research by scientists in this area has shown that infected women who were vaccinated before the age of 35 overcame the course of treatment for papillomavirus faster and more easily. In this regard, some doctors still recommend vaccination if you have human papilloma.
Reviews from doctors and patients
Reviews from patients and doctors about HPV vaccination:
- Yulia, 29 years old . Today at my appointment I found out that I have mild dysplasia. The doctor prescribed some medications. She said that most likely after completing the course I would be vaccinated against HPV, because it is a highly oncogenic virus. I don't have children, so I'm a little worried. After all, there were rumors that this vaccine causes the development of infertility;
- Katya, 32 years old . I had this vaccination 3 years ago. Injected with Cervarix. It was scary because of the rumors about infertility that this medicine causes. But the doctor calmed me down. She said that this could only happen if the injection was given if there were contraindications, but I had none. A year ago I gave birth to a completely healthy son. Therefore, I can safely refute myths about infertility;
- Olga Ivanovna, obstetrician-gynecologist . I recommend that my patients get vaccinated against the papilloma virus. HPV is a dangerous agent that can cause cervical cancer. The ideal period for vaccination is the age of 9-12 years, while girls do not have sexual partners. It is better for adult women to get the vaccine only after consulting a gynecologist. However, vaccination cannot be considered lifelong protection against cervical cancer. Since this type of disease can also be caused by other factors, regular examination for the presence of cancer should not be canceled.
Types of strains
Human papillomavirus infections No. 6 and 11 provoke the appearance of papillomas and condylomas on the genitals. Neoplasms can degenerate into malignant tumors. To prevent such processes, Russia has an immunization program.
To vaccinate against papillomavirus, doctors use 2 drugs:
- Gardasil. Manufacturer: Holland.
- Cervarix. Manufacturer: Belgium.
The drugs promote the production of antibodies that protect the body from viral attacks. To prevent the development of the disease, three injections are indicated. Children can be vaccinated together with vaccines against tetanus, whooping cough, hepatitis B, polio and diphtheria.
If the injection is given to adolescents who are sexually active, the use of contraceptives continues. The drugs do not protect against syphilis, gonorrhea, trichomoniasis and other sexually transmitted infections.
Mechanism of action of the HPV vaccine
Unfortunately, the female body’s immune system is not always sufficient to fight the papilloma virus.
Therefore, the body requires outside help in the form of a vaccine. The HPV vaccine works in the same way as any other vaccine. Antibodies that get inside cause immune memory in the body, which is necessary to protect organs from the influence of a pathogenic virus.
Medicines intended for vaccination do not contain cancer cells or live virus. They contain only protein particles that are similar in appearance to a virus, which is quite enough for the body to recognize a dangerous agent.
Vaccination does not pose a risk to women or girls.
HPV vaccination schedule
HPV vaccination is carried out strictly according to the schedule, which allows you to achieve maximum effectiveness. The vaccination schedule includes three vaccinations.
According to the classical scheme, the interval between the first and second administration of the vaccine is two months, and between the second and third - four.
But if necessary, more frequent administration is also allowed. You can do the second vaccination a month after the first, and the third two months after the second.
"Let's end anti-vaccinationism!"
More precisely, this: we can, of course, talk about mild and passing complications of vaccinations. Various websites that provide information about Gardasil and Cervarix usually give approximately the following list of negative effects: pain and swelling at the injection site, itching, bleeding, headache, fever, nausea, dizziness, fainting.
However, the mention of complications that significantly reduce the quality of life or lead to death causes a strong negative reaction among the medical community.
“Large clinical trials indicate the absence of serious negative effects, and case control studies are unproven,” anti-vaccination activists say.
Meanwhile, both statements require significant clarification, as does the term “anti-vaccinism” itself.
The latter was well written by the editor of the British Medical Journal, Peter Doshi, who believes that calling anyone who expresses doubts about the safety of a particular vaccine an anti-vaccineist is the same as calling a person who expresses doubts about the safety or effectiveness of a particular drug an “anti-drug” . (Read more about his point of view in Russian here).
Moreover, a relatively recent study by British scientists indicates that the more official medicine fights against conditional anti-vaccination, the less people trust it. (More about this here).
This seems surprising only at first glance, because when some topic is prohibited, a dark zone is formed in this place, in which, as is known, monsters are born.
These include, for example, the assertion that the creators of the HPV vaccine intended to use it to limit the fertility of girls in third world countries and, by reducing the population in Asia, Africa and Latin America, to seize their natural resources.
However, the concerns expressed by a number of experts about the safety of Gardasil and Cervarix have nothing to do with delusional theories.
Multiple sclerosis – after or as a consequence?
Photo from sciencenordic.com
Most recently, in May 2019, a meta-analysis of clinical trials of HPV vaccines was published by the Cochrane Expert Group.
The researchers found that the risk of serious complications was about the same in the vaccine and placebo groups, although the number of deaths was higher among those vaccinated, especially in the age group after 25 years. In general, the deviation is within the statistical error: 11:10,000 for unvaccinated people, 14:10,000 for vaccinated people.
Nevertheless, a number of experts insist that there is no need to be complacent about safety, it is necessary to record all cases of serious illness associated with vaccination with Gardasil and Cervarix and analyze them.
More recently, in February 2019, at the ACTRIMS (American Committee on Treatment and Research in Multiple Sclerosis) forum in San Diego (USA), researcher Ye Hu from the University of Miami reported on two cases of multiple sclerosis in adolescents after vaccination with Gardasil.
A 14-year-old boy and a 17-year-old girl developed similar symptoms within two weeks after vaccination (the boy after the third dose, the girl after the first).
Both suffered from blurred vision, and the girl also experienced intermittent muteness and weakness in her legs. Her MRI showed lesions in the frontal and occipito-parietal regions of the brain.
In both adolescents, MRIs showed lesions in the white matter of the brain, and researchers found oligoclonic streaks in the cerebrospinal fluid (a diagnostic sign of multiple sclerosis).
Researchers suggest that Gardasil may increase the risk of onset of nerve fiber demyelination in individuals predisposed to multiple sclerosis, or act as a trigger for MS through activation of the body's immune response.
Some experts believe that the aluminum adjuvant added to vaccines to enhance the immune response may cause excessive activation in some particularly sensitive individuals, leading to the launch of autoimmune processes.
This phenomenon is called “ASIA syndrome” (autoimmune/inflammatory syndrome induced by adjuvants) or “Schoenfield syndrome” after the Israeli scientist Yehuda Schoenfield, who first drew attention to this phenomenon.
An international group of scientists led by Schonfield analyzed 300 cases of the syndrome, 48 of which were associated with vaccines against papillomavirus.
At the same time, 89% of patients (of the total number) received certain clinical diagnoses, the most common of which were: undifferentiated connective tissue disease, fibromyalgia and/or chronic fatigue syndrome, systemic erythematous lupus, neurological autoinflammatory diseases.
Does this mean that MS in both adolescents is necessarily the result of vaccination? No, such a conclusion cannot be made, nor can it be ruled out that the disease is a serious complication.
be careful
The presence of papillomas and warts on the body is the first sign of malignant melanoma!
We hasten to warn you that most drugs that “treat” warts and papillomas are a complete deception of marketers who make hundreds of percentage points on drugs whose effectiveness is zero. They do not cure the disease, but only mask the symptoms.
The pharmacy mafia makes huge money by deceiving sick people.
But what to do? How to treat if there is deception everywhere? Doctor of Medical Sciences Anatoly Makhson conducted his own investigation and found a way out of this situation. In this article, the Doctor also told how to 100% protect yourself from melanoma, for only 149 rubles! Read the article in the official source following the link.
Up to what age can vaccination be carried out?
Usually, papilloma vaccinations are given only to girls, but they are also indicated for boys. In accordance with the recommendations of the Ministry of Health of the Russian Federation, it is necessary to vaccinate against papilloma with both, starting from the age of 12. If the vaccine has not been administered before this age, then vaccinations in sexually mature women and men can be done from 16 to 23 years of age.
Vaccination can cause certain allergic reactions in children, so whether you should vaccinate your child or not - read here.
The use of both vaccines is allowed until the age of 27 years. There is no scientific evidence for administering these vaccines to older people.
Attention! If the body already has the human papillomavirus, vaccination for people over 27 years of age may not be effective!
However, there are studies confirming that the vaccine, when given to women under 35 years of age, facilitated the treatment of the human papillomavirus already present in the body.
Public opinion pros and cons
Any vaccine, no matter how effective it is, always “splits” people into several camps. Among them there are those people who see the effectiveness of the drug. And there are those who oppose this method of preventing disease. But there are also those who seek benefits from this.
In the territory of the former USSR, in particular Russia, the vaccine against papillomavirus is not included in the course of compulsory vaccinations. Therefore, all responsibility is shifted to the shoulders of the parents, whose child will soon begin sexual activity. But in European countries and the United States this caused real confrontation.
Popular To any country with children after yellow fever vaccination
On the one hand, the American National Cancer Institute believes that vaccinating the population saves women from undergoing such unpleasant procedures as biopsies, invasive procedures and PAP smears. They believe that vaccinations against papillomavirus have significantly reduced mortality in recent years. In Russia, doctors only mentioned this when the editorial board of Rossiyskaya Gazeta held a round table.
But, on the other hand, some conservative organizations and religious communities took the side of the parents. The precedent has become that mandatory vaccinations for teenagers deprive parents of their rights.
Another argument against compulsory vaccination was that adolescents, having received protection from such a disease, will begin early sexual activity. Because a fragile consciousness is structured differently. The feeling of security will lead to the fact that he will forget about using a basic condom during sexual intercourse. Health insurance companies also opposed mandatory vaccination of the population. But from their point of view, the costs of the drug are too high.
Contraindications for use
A direct ban on vaccination is:
- allergy to one of the components included in the drug;
- pregnancy;
- exacerbation of many diseases.
If the reason for canceling vaccination is a chronic illness, vaccination is carried out after the patient has recovered.
- severe allergic reaction, for example, severe inflammation at the injection site);
- feverish condition.
Temporary contraindications are the following:
- acute infectious disease;
- exacerbation of a chronic illness;
- thrombocytopenia (decrease in platelet level below 150⋅109/l, which is accompanied by increased bleeding);
- taking anticoagulants (drugs that reduce blood clotting);
Like any vaccination, the HPV vaccine has contraindications, for example, an acute infectious disease.
However, after recovery or improvement of the condition, vaccination is allowed.
Vaccination of patients against human papillomavirus is actively practiced in different countries. The serum was first used in America to vaccinate girls 9-12 years old. Somewhat later, the country began to administer the medicine to boys, teenagers and young adults. Only a few years ago, the age of patients receiving the vaccine increased to 45 years.
In 2006, vaccination was officially permitted in the Russian Federation. Gardasil became an approved drug. In France, since 2007, girls aged 14 to 16 years who are not sexually active or have had a partner for less than 6 months have been actively vaccinated. Around the same time, vaccination was certified in the UK.
In less developed countries, the human papillomavirus vaccine is rarely used and the procedure is not certified, but the government is working to introduce vaccination into a mandatory health care program.
Today, the experience of using vaccines to protect against infectious diseases caused by HPV is practiced in most developed countries. And in some foreign countries, these vaccinations are even included in national immunization programs. So, for example, in the USA such vaccination is carried out among absolutely all girls aged 11-13 years, in Germany - at the age of 13-16 years, in France - at the age of 15, and in Austria - from 10 to 18 years.
The experience of using these vaccinations around the world for many years has proven their high effectiveness for prevention and complete safety.
How is HPV vaccination carried out?
The vaccine against the papilloma virus is injected into the muscles in the forearm or thigh. For a series of vaccinations, the same immunobiological preparations should be used.
Administration of an antiviral agent is not recommended by other methods for the following reasons:
- intravenous administration is contraindicated, because in this case, the entire dose of the drug immediately enters the systemic bloodstream and provokes excessive activation of the immune system, as a result of which foreign substances are destroyed and the antibodies necessary for future protection are not produced. This means that immunity against the papilloma virus will not develop properly.
- It is not advisable to administer an immunobiological drug subcutaneously or intradermally, since it enters the systemic circulation after a long period of time and in a small dose. Antigens are thus also suppressed, and protein compounds in the blood plasma that prevent the proliferation of viruses are not formed, so vaccination is useless. In addition, this method of administration risks the development of a lump or lump at the injection site, which may take 1-2 months to resolve.
- Intramuscular injection into the buttock is prohibited, since there is a high risk of damaging the sciatic nerve or entering the subcutaneous fat layer, which is well developed in this part of the body. If the latter happens, a lump will also form and the graft will be ineffective.
If the vaccine is given to a teenager or young man who is not yet sexually active, then there is no need to pre-test to detect HPV. If the patient already has sexual experience, then before vaccination it is mandatory to carry out diagnostics to identify the presence of oncogenic types of the virus in his body. If the result is positive, then the vaccine is abandoned, since it is not used for medicinal purposes.
If, in parallel with the HPV vaccination, the patient also needs another vaccination, then it is quite possible to combine them. Simultaneous administration of immunobiological drugs against papilloma and other vaccines does not impair the formation of immunity to any of the drugs. If several vaccinations are performed in one day, then different syringes are used for this, and the drugs are injected into different parts of the body.
You should absolutely not mix several drugs in one syringe.
Rehabilitation and complications after vaccination
As is the case with most vaccinations, it is not advisable to get the injection site wet during the day. In addition, injection of the drug can cause certain side effects:
- pain in the injection area, redness, slight swelling;
- hives;
- slight increase in temperature (up to a maximum of 38 ° C);
- chills;
- headache, dizziness;
- general malaise.
In general, the HPV vaccine does not cause any significant complications. These symptoms, if they occur, quickly pass without treatment. If necessary, you can take an analgesic with an antipyretic effect (Paracetamol, etc.). People prone to allergies should take an antihistamine before the injection.
After vaccination, undesirable reactions may occur, for example, in the form of headache or dizziness, which quickly pass
Cases of fainting after vaccination are very rare. Moreover, this was recorded exclusively in teenage boys.
Many parents are concerned about the long-term effects of the HPV vaccine. In particular, we are talking about possible infertility: supposedly the injection causes corresponding changes in the functioning of the reproductive system (on the Internet you can even find articles where it is reported that the vaccine is specially distributed in third world countries to reduce their population, experiments are being carried out on children). In fact, in many countries, adolescents have been vaccinated en masse for more than a decade: this is a sufficient period of time to verify the presence or absence of the indicated effect. Meanwhile, vaccinated girls have already grown up and many have successfully become mothers.