Symptoms accompanying diabetes mellitus can be divided into 2 groups:
- signs associated directly with high blood sugar levels;
- problems that accompany organ damage that occurs as a result of long-term elevated blood sugar levels.
Classification of diabetes mellitus according to WHO
The modern classification of diabetes mellitus according to WHO includes 4 types and groups designated as borderline disorders of glucose homeostasis.
- Diabetes mellitus type 1 (insulin-dependent diabetes): immune-mediated, idiopathic.
- Diabetes mellitus type 2 (previously called the senile type - non-insulin-dependent diabetes).
- Other specific types of diabetes.
- Gestational diabetes mellitus (during pregnancy).
- Borderline disturbances of glucose homeostasis.
- Increased (borderline) fasting glucose.
- Impaired glucose tolerance.
Primary manifestations of diabetes mellitus in women
Modern women experience enormous daily stress, which has a negative impact not only on their physical but also on their emotional state. Exhaustive work, chronic stress, hypovitaminosis, lack of natural products, constant lack of sleep, increased anxiety for children - all this provokes metabolic disorders in the female body, leading to the development of diabetes. The first signs of diabetes in women are not immediately detected, as they are often mistaken for symptoms of hormonal changes, premenstrual syndrome, or explained by the onset of menopause.
The first signs of diabetes in women include:
- decreased performance, lack of energy and weakness;
- headache for no apparent reason;
- feeling of fatigue that occurs immediately after a heavy meal;
- increased drowsiness;
- feeling of thirst;
- excess weight or sudden weight loss due to excessively increased appetite;
- increased blood pressure;
- severe skin itching, especially in the groin area;
- disturbances in the emotional-volitional sphere, manifested by increased nervousness and irritability;
- pustular lesions of the skin;
- increased fragility of hair and nails, hair loss.
Classification of diabetes mellitus and WHO statistics
According to the latest WHO statistics, the vast majority of people affected have type 2 disease (92%), with type 1 disease accounting for about 7% of diagnosed cases. Other types account for about 1% of cases. Gestational diabetes affects 3-4% of all pregnant women. WHO experts also often mention the term prediabetes. It assumes a condition when the measured blood sugar values already exceed the standard, but do not yet reach the values characteristic of the classical form of the disease. Prediabetes in many cases precedes the immediate development of the disease.
Development and manifestation of gestational diabetes
Gestational diabetes is a disorder of carbohydrate metabolism that is first detected during pregnancy.
This form is the most common type of diabetes that develops during pregnancy and usually disappears after childbirth. Gestational diabetes occurs in approximately 2-3% of pregnant women. It should be remembered that a clear diagnosis of gestational diabetes can be carried out as part of an examination after a certain time after birth (preferably 3-6 months). It is possible that any other type of diabetes, which is perceived as gestational, appeared during pregnancy. If the disease does not disappear after delivery, the patient should be properly monitored and, if necessary, treated. Since blood sugar levels are only slightly elevated, women usually experience absolutely no problems. Sometimes there may be a slight thirst and, therefore, greater fluid intake.
Elevated blood sugar levels, which are a sign of poor diabetes control, can cause late complications. These include accelerated fetal growth associated with increased nutrient supply. This leads to abnormal fat deposition, an increase in the subcutaneous layer of fat, and organomegaly appears (enlarged spleen, liver and heart). Larger children of mothers with undertreated diabetes have a higher risk of developing the disease later in life.
On the other hand, complications of diabetes mellitus may also result in slower fetal growth. This occurs as a result of impaired blood flow to the placenta, which is caused by changes in the mother's blood vessels.
Finally, complications include sudden death of the fetus in the womb during the last weeks of pregnancy, which occurs approximately 4 times more often in women with diabetes than in healthy women. But the exact mechanism of this phenomenon is unknown. Early diagnosis and treatment normalize blood sugar levels, and complications during pregnancy and childbirth do not occur. It is for these purposes that it is now recommended that all pregnant women be screened for gestational diabetes.
Epidemiology
According to WHO data, currently in Europe, about 7-8% of the total population with this disease is registered.
According to the latest WHO data, in 2019 there were more than 750,000 patients, while in many patients the disease remains undetected (more than 2% of the population). The development of the disease increases with age, which is why more than 20% of the disease can be expected among the population over the age of 65 years. The number of patients has doubled over the past 20 years, and the current annual increase in registered diabetics is about 25,000-30,000 people. The increasing prevalence, in particular, of type 2 disease throughout the world indicates the emergence of an epidemic of this disease. According to WHO, it currently affects about 200 million people in the world and it is expected that by 2025 more than 330 million people will suffer from this disease. Metabolic syndrome, which is often part of type 2 disease, can affect up to 25%-30% of the adult population.
Specific symptoms
The disease manifests itself not only with the above symptoms, but also with some specific signs.
These include:
- inflammation of the reproductive organs in men caused by a constant urge to urinate;
- pain felt in the legs and arms;
- poor healing of any abrasions and wounds;
- decreased pain sensitivity;
- weakened immunity;
- weight gain or loss;
- the appearance of xanthoma on the body;
- intensive hair growth throughout the body or hair loss on the legs;
- increased excitability;
- the occurrence of causeless attacks of nausea and vomiting;
- insomnia;
- pain in the heart or head.
A sharp deterioration in health should also not be ignored. It can also be an indirect sign of the onset of the development of any disease, including diabetes.
Video material about the symptoms of sugar disease:
In children
The disease is most often diagnosed in young patients after the onset of dangerous complications - ketoacidosis and coma.
Children often present with vomiting syndrome, in which episodes of ketosis occur regularly. This condition mainly affects patients with a predisposition to acetonemic syndrome. Its exacerbation can be provoked by ARVI and infections. The syndrome often resolves on its own as the child grows older.
If it appears in infants under one year of age and continues to appear for longer than 7 years, you need to consult an endocrinologist and, if necessary, check the blood for glucose levels.
First manifestations:
- sudden loss of body weight;
- polyuria;
- polydipsia.
The development of ketoacidosis is accompanied by symptoms such as:
- pain in the abdominal area;
- nausea or vomiting;
- dry skin;
- rapid breathing;
- dizziness;
- the presence of acetone (in urine, vomit);
- unconscious state.
Detection of these signs should motivate you to visit a specialist as soon as possible. This is due to the rapid progression of the disease in children and the rapid development of complications.
Video from Dr. Komarovsky about the disease in children:
In men
Diabetes is characterized by impaired innervation and blood supply to the reproductive organs, leading to changes in the sexual sphere in men.
Main symptoms:
- drop in libido;
- erectile dysfunction and instability;
- infertility caused by a decrease in the motility and number of active forms of sperm.
An increased concentration of glucose often causes itching in the genital area.
Among women
The development of diabetes also negatively affects reproductive functions in women.
The main manifestations of such violations are:
- decreased sexual interest;
- irregular onset of regular menstruation;
- development of candidiasis in the vagina;
- dryness and itching sensation on the surface of the genital mucosa;
- infertility.
In case of successful conception, diabetes often becomes the cause of recurrent miscarriage or leads to numerous complications during pregnancy, as well as after childbirth. The disease not only worsens the well-being of the expectant mother, but also increases the risk of developing various pathologies in the child.
This negative impact of diabetes explains the need for every expectant mother to undergo appropriate research in order to early detect elevated glucose levels and loss of glucose tolerance.
Video about gestational diabetes during pregnancy:
Diagnostics according to WHO standards
Diagnosis is based on the presence of hyperglycemia under certain conditions. The presence of clinical symptoms is not constant, and therefore their absence does not exclude a positive diagnosis.
The diagnosis of the disease and borderline disorders of glucose homeostasis is determined on the basis of blood glucose levels (= venous plasma glucose concentration) using standard methods.
Divided:
- fasting plasma glucose (at least 8 hours after the last meal);
- random blood glucose levels (at any time of the day without taking into account food intake);
- glycemia at 120 minutes of an oral glucose tolerance test (OGTT) with 75 g of glucose.
The disease can be diagnosed in 3 different ways:
- presence of classic symptoms of the disease + random glycemia ≥ 11.1 mmol/l;
- fasting blood glucose ≥ 7.0 mmol/l;
- glycemia at the 120th minute of OGTT ≥ 11.1 mmol/l.
Alarming Consequences
Long-term elevated blood glucose levels lead to:
- increased susceptibility to infections, especially skin, genital and urinary tract infections;
- deterioration of the condition of small vessels, leading to damage to the eyes, nerves, kidneys, etc. diabetic foot syndrome;
- disruption of large vessels with a high risk of heart attack, stroke and peripheral artery disease.
There are no exceptions when it is the symptoms associated with these late complications that help to detect diabetes mellitus for the first time.
Normal values
Normal fasting blood glucose values range from 3.8 to 5.6 mmol/L.
Normal glucose tolerance is characterized by glycemia at 120 minutes of OGTT <7.8 mmol/l with normal fasting glucose.
Incidental capillary blood glucose greater than 11.0 mmol/L in symptomatic individuals leads to re-diagnosis, which is based on the need to confirm the provisional diagnosis with a glucose level greater than 6.9 mmol/L. If there are no symptoms, a fasting blood glucose test is performed under standard conditions.
Fasting blood glucose levels below 5.6 mmol/l exclude diabetes.
Fasting glycemia many times higher than 6.9 mmol/l confirms the diagnosis of diabetes mellitus.
Glycemia from 5.6 to 6.9 mmol/l (the so-called cut-off fasting blood glucose level) requires an OGTT examination.
During a glucose tolerance test, a positive diagnosis is indicated by glycemia after 2 hours greater than or equal to 11.1 mmol/L.
When diagnosing, the blood glucose test must be repeated and based on 2 determinations.
For the differential diagnosis of type 1 and type 2 disease, C-peptides can be used as an indicator of endogenous insulin secretion, if there is uncertainty in the clinical picture. Examination on an empty stomach under basal conditions and after stimulation with a normal standard breakfast is recommended. In type 1 diabetes, the basal value sometimes even drops to zero. With type 2, its value is normal, but with insulin resistance, it can be increased. As type 2 disease progresses, however, the level of C-peptides decreases.
Almost asymptomatic disease
Long-term symptoms of type 2 diabetes include fatigue, slightly increased thirst, and frequent urination. It is also no exception that the patient does not register any symptoms in the early stages of the disease. The disease can attract attention with symptoms associated with increased blood sugar or complications that develop covertly and unnoticed over many years. The doctor suspects type 2 diabetes based on symptoms or hyperglycemia (excessive blood glucose levels) and glycosuria (glucose in the urine). The disease is subsequently confirmed by a blood test.
Common signs, which due to their inconspicuous nature often go unnoticed, may include:
- thirst with increased fluid intake and frequent urination; this condition is caused by high blood sugar. Sugar binds water and transports it into the urine, leading to dehydration;
- unreasonable fatigue and weakness;
- blurred vision along with headache;
- a feeling of poor blood circulation in the peripheral parts of the body (legs, arms) - a tingling sensation;
- frequent, sharp feelings of hunger, which, however, lead to weight loss.
If any of these symptoms occur repeatedly, it is recommended to visit a doctor and consult with him about whether diabetes mellitus is the cause of the condition. Especially if the person belongs to a risk group.
Risk factors for developing type 2 diabetes include:
- history of type 2 diabetes mellitus;
- age over 45 years;
- proven impaired glucose tolerance;
- lack of physical activity;
- overweight;
- poor nutrition;
- long-term stress;
- gestational diabetes.
Clinical picture
Typical symptoms include thirst, polydipsia and polyuria (along with nocturia) when the disease is advanced.
In other cases, the patient notices weight loss with normal appetite and nutrition, fatigue, ineffectiveness, malaise, or fluctuations in visual acuity. With severe decompensation, it can lead to bruising. Very often, especially at the beginning of type 2 disease, there are no symptoms at all, and the definition of hyperglycemia can be a surprise.
Other symptoms are often associated with the presence of microvascular or macrovascular complications and therefore only occur after several years of diabetes. These include paresthesia and night pain in the legs with peripheral neuropathy, gastric emptying disorders, diarrhea, constipation, bladder emptying disorders, erectile dysfunction and other complications, for example, the manifestation of autonomic neuropathy of the competent organs, visual impairment due to retinopathy.
Also, manifestations of coronary heart disease (angina pectoris, symptoms of heart failure) or lower extremities (claudication) are a sign of accelerated development of atherosclerosis after a longer course of the disease, although in some patients with advanced symptoms of atherosclerosis these symptoms may be absent. In addition, diabetics tend to have recurrent infections, especially of the skin and genitourinary system, and periodontopathy is more common.
Diagnosis of the disease is preceded by a short (with type 1) or longer (with type 2) period, which is asymptomatic. Already at this time, mild hyperglycemia causes the formation of micro- and macrovascular complications, which may be present, especially in patients with type 2 disease, already at the time of diagnosis.
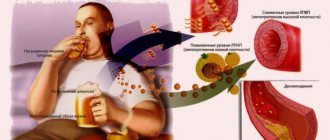
In the case of macrovascular complications in type 2 diabetes, this risk increases several times with the accumulation of atherosclerotic risk factors (obesity, hypertension, dyslipidemia, hypercoagulability) accompanying a condition characterized by insulin resistance, and referred to as multiple metabolic syndrome (MMS), metabolic syndrome X or Riven syndrome.
Signs of complications
Diabetic foot
In medicine, the diabetic foot is understood as a complex anatomical and functional change in the tissues of the distal parts of the lower extremities in patients suffering from diabetes. This is the most serious complication of the pathology in question, often leading to gangrene, amputation of limbs and disability.
If you have a history of diabetes, the health of your legs should be monitored very carefully. There are three main forms of diabetic foot: neuropathic (predominant damage to nerves), ischemic (predominant damage to blood vessels and impaired blood flow), mixed.
Among the complaints of patients preceding diabetic foot, experts identify unpleasant feelings, burning and stabbing sensations in the legs, goosebumps, and a feeling of electric shock. If these troubles disappear when walking, this indicates the beginning of the development of the neuropathic form of diabetic foot. It is also important to pay attention if your feet periodically lose sensitivity. If painful sensations occur directly when walking or at night (can be calmed only by hanging the limbs from the edge of the bed), then this means the beginning of the development of an ischemic form of diabetic foot called “ischemic foot”.
Among the signs indicating the start of development of a diabetic foot, experts identify pale skin on the legs or the appearance of pigment spots on them, peeling and dry skin in this area, the appearance of different-sized blisters on the skin with clear liquid, frequent calluses, cracks between the toes, deformation of the nails. plates on the legs, thickening of keratinization of the skin of the feet, spontaneous fractures of small bones on the legs. If a person notices at least a few of these signs, he should urgently seek medical help.
Signs of retinopathy
Diabetic ophthalmology is manifested by changes in the blood vessels in the retina of the eye, leading to disruption of microcirculation in it. This disorder leads to diabetic retinopathy. This complication develops gradually and even in the later stages it can be almost invisible to a person.
The main signs of diabetic retinopathy are:
- the appearance of “floaters” before the eyes;
- blurred vision;
- decreased visual acuity in later stages;
- hemorrhages in the vitreous body and retina.
In this case, diabetic ophthalmology can manifest itself in two main forms - non-proliferative (background) or proliferative retinopathy of the retina. With background retinopathy, the pathology primarily affects the retina itself. If there are disturbances in the capillary vessels of the retina, hemorrhages, retinal edema, and deposits of metabolic products occur. Background retinopathy is common in elderly patients with diabetes. It provokes a gradual decrease in visual acuity.
Based on the background, proliferative retinopathy develops if the deficiency of oxygen supply to the retina continues to grow. In this case, there is a pathological formation of new blood vessels growing from the retina into the vitreous body. This process leads to hemorrhages in the vitreous body and a sharp increase in the progression of vision loss in humans and irreversible blindness. In adolescence, such a transition of the complication from one form to another can occur in a couple of months, followed by retinal detachment and complete loss of vision.
Signs of encephalopathy
Diabetic encephalopathy occurs as a complication of diabetes mellitus, due to diffuse degenerative damage to the brain. The prevalence of encephalopathy directly depends on the type of diabetes, and its symptoms depend on the duration of the disease and its severity. It is a late complication and appears 10-15 years after the onset of diabetes.
Its immediate cause is metabolic disorders typical of diabetes, leading to damage to brain tissue and blood vessels. The above processes lead to impaired brain activity and decreased cognitive functions. The development of encephalopathy occurs very slowly, which makes it difficult to identify its symptoms in the early stages.
The main symptoms of diabetic encephalopathy are:
- headaches and dizziness;
- emotional instability, high fatigue, sleep disturbances and other neurasthenic disorders;
- instability of a person's gait;
- doubling of objects when looking at them, blurred vision, flashing “spots” before the eyes;
- mental, depressive disorders;
- confusion;
- deterioration of mental activity, memory, ability to concentrate;
- strokes, transient ischemic attacks, other pathologies of cerebral circulation;
- the occurrence of seizures.
At the initial stages, there are practically no clinical complications, but with the development of encephalopathy, the symptoms begin to appear more clearly. Symptoms are identical for both types of diabetes.
Frequent accompaniments of diabetes are atherosclerosis, arterial hypertension and obesity. Due to the obliteration of blood vessels when atherosclerosis occurs, the risk of ischemic strokes and heart attacks increases. When microcirculation in the renal vessels is disrupted, irreversible renal failure occurs, which over time leads to the complete cessation of renal function. This in turn leads to the need for replacement therapy for renal failure using lifelong dialysis.
Diabetic coma
A diabetic coma is understood as a serious disturbance of metabolic processes in the body of a patient suffering from diabetes. Coma can occur either with a strong increase or with a strong decrease in the level of sugar in a person’s blood. This condition requires urgent medical attention, since in its absence serious complications and even death are possible.
The coma develops in stages, but quite rapidly. The first sign of falling into a coma may be a fainting state, a rapid increase in blood sugar, nausea and vomiting, drowsiness, pain in the abdomen a day or more before the immediate coma. Another symptom of a diabetic coma may be the strong smell of acetone from the patient’s mouth. Cramps, thirst, and decreased sensitivity may also occur.
During a hypoglycemic coma, the concentration of sugar in the blood decreases sharply. The indicator can reach 2.5 mmol per liter and below. Among the obvious symptoms of such a coma are causeless anxiety, fear of the patient, a feeling of weakness, convulsions, drop in blood pressure, and loss of consciousness. Precursors of hypoglycemic coma may include:
- general malaise;
- lack of appetite;
- diarrhea or constipation;
- dizziness, headaches, tachycardia.
Lack of help for this condition can lead to extremely serious consequences. Since hypoglycemic coma develops rapidly, the assistance provided must be prompt.
Ordinary people can diagnose a diabetic coma by a sharp decrease in the patient's blood pressure, weakening of the pulse, and softness of the eyeballs. Only a qualified doctor can bring a person to his senses in this state, so an ambulance should be called as soon as possible.
Diabetes mellitus type 1
The WHO definition characterizes this disease as a known form of diabetes mellitus, however, it is much less common in the population than full-blown type 2 disease. The main consequence of this disease is increased blood sugar levels.
Causes
This disease has no known cause and affects young, previously healthy people. The essence of this disease is that for some unknown reason the human body begins to produce antibodies against the pancreatic cells that form insulin. Therefore, type 1 diseases are largely similar to other autoimmune diseases, such as multiple sclerosis, systemic lupus erythematosus and many others. Pancreatic cells are killed by antibodies, resulting in decreased insulin production.
Insulin is a hormone needed to transport sugar into most cells. In case of its deficiency, sugar, instead of being a source of energy for cells, accumulates in the blood and urine.
Manifestations
The disease may be accidentally discovered by a doctor during a routine examination of the patient without obvious symptoms, or various signs may appear, such as feeling tired, night sweats, weight loss, mental changes and abdominal pain. Classic symptoms of diabetes include frequent urination with large volumes of urine followed by dehydration and thirst. Sugar in the blood is present in excess, in the kidneys it is transported into the urine and attracts water. As a result of increased water loss, the body becomes dehydrated. If this phenomenon is not treated, and the concentration of sugar in the blood reaches a significant level, it leads to distortion of consciousness and coma. This condition is known as hyperglycemic coma. In patients with type 1 diabetes, this situation produces ketone bodies in the body, which is why this hyperglycemic state is called diabetic ketoacidosis. Ketone bodies (especially acetone) cause a specific unpleasant odor from the mouth and in the urine.
Too much load
Unlike type 1 diabetics, type 2 diabetes produces insulin in normal amounts, at least at the onset of the disease. However, tissues have a lower sensitivity to its action (insulin resistance). Therefore, the pancreas begins to produce more of this hormone, which over time may result in the risk of hyperglycemia (high blood glucose). Sooner or later it comes to an increase in blood sugar levels with all the ensuing consequences. Due to excessive stress placed on the insulin-producing cells of the pancreas, they become depleted and, ultimately, production of the hormone decreases.
LADA-diabetes
On a similar principle, a special subtype of type 1 diabetes arises, defined by WHO as LADA (Latent Autoimmunity Diabetes in Adults). The main difference is that LADA, as opposed to “classical” type 1 diabetes, occurs at an older age, and therefore can be easily replaced by type 2 disease.
Causes
Similar to type 1 diabetes, the cause of this subtype is unknown. The basis is an autoimmune disease in which the body's immune system damages the cells of the pancreas that produce insulin; its deficiency subsequently leads to diabetes. Due to the fact that this subtype of the disease develops in older people, the lack of insulin can be aggravated by the poor tissue response to it, which is typical for people who are obese.
Manifestations
The manifestations are not particularly different from classic diabetes (type 1 or 2); there is excessive thirst and urination, the presence of sugar in the urine, fatigue, weakness, nausea, abdominal pain, vomiting, etc.
Development and manifestation of diabetes in children
If a child gets diabetes, we are always talking about type 1 disease.
The disease occurs when the body loses the ability to produce the hormone insulin. When, under the influence of autoimmunity, beta cells begin to be destroyed and their number decreases, no symptoms appear for a certain time. The destruction of beta cells can continue unnoticed for months or even years. Therefore, it is so difficult to determine the initial factor that caused the development of the disease. When the number of beta cells begins to approach a critical limit, a person becomes vulnerable. His body ceases to be able to increase insulin production when suddenly necessary. It is at this time that diabetes can manifest itself. A person needs more insulin. A critical moment in the form of a flu or sore throat is enough for a lack of insulin to appear in the child’s body, and with it the first signs of diabetes.
If the flu or sore throat does not affect the child at the moment, little will change in the development of the disease: after a few weeks or months, with a further decrease in beta cells, a lack of insulin will appear. The disease that precedes the appearance of the first symptoms of diabetes is not the cause, but the initiating factor. As a result, a lack of insulin and an increase in glucose in the blood are revealed. The body, getting rid of its excess, transports it into urine. Glucose in the urine attracts water and causes excessive urination. Young children may experience nocturnal enuresis.
Diabetes mellitus type 2
The WHO classification of diabetes mellitus defines type 2 disease as a widespread disease, affecting 7-10% of the population. If we talk about patients with diabetes mellitus in general, most of them suffer from this type. Type 2 has only one common characteristic with type 1 – high glycemia.
Causes
The causes are more difficult to understand than for type 1 diabetes. In this disease, the body's immune response against the cells of the islets of Langerhans that form insulin does not reach. Type 2 diabetes mellitus can be characterized as a complex metabolic disease determined by the following risk factors:
- large waist circumference (i.e., apple-shaped obesity); A waist circumference of more than 100 cm for women and 90 cm for men is considered especially risky;
- high levels of cholesterol and other fats;
- high glycemic value;
- high blood pressure;
- genetic predisposition.
Risk factors
The typical patient with type 2 diabetes is an older person, often an obese man, usually with high blood pressure, abnormal concentrations of cholesterol and other fats in the blood, and a history of type 2 diabetes in other family members (genetics).
Development
Type 2 diabetes develops approximately as follows: there is a person with a genetic predisposition to developing this disease (this predisposition is present in many people). This person lives and eats unhealthy (animal fats are especially risky), moves little, smokes frequently, and drinks alcohol, as a result of which he gradually develops obesity. Complex metabolic processes begin to occur. Fat stored in the abdominal cavity has the special property of releasing fatty acids to a large extent. Sugar can no longer be easily transported from the blood into the cells, even when more than enough insulin is formed. Glycemia after eating decreases slowly and reluctantly. At this stage, you can cope with the situation without injecting insulin. However, changes in diet and general lifestyle are necessary.
Diabetes classification
According to the classification , one should distinguish:
- diabetes;
- prediabetes;
- gestational in pregnant women.
According to ICD 10 (international classification of diseases), the modern classification looks like this:
- Type 1 – insulin dependent, code E10 (use of insulin is mandatory);
- Type 2 – insulin-independent, code E11 (provokes excess weight and impaired blood supply);
- code E12 – caused by malnutrition (occurs against the background of starvation or impaired liver and kidney function);
- code E13 – mixed;
- code E14 – unspecified type of pathology.
Why is diabetes dangerous? Because there is a difference in the symptoms of each class of disease, and each type causes serious disruptions in the functioning of the internal systems of the body.
1 type
Insulin-dependent type 1 diabetes mellitus is a disease that is formed as a result of cellular destruction of the pancreas, resulting in the accumulation of excess sugar in the body. This pathology develops with a lack of insulin, which is necessary for proper carbohydrate metabolism.
The affected gland cannot cope with the production of sufficient amounts of the hormone. In this regard, the absorption of glucose into cells becomes more difficult and the blood sugar level increases. The main way to compensate for the deficiency of the hormone is to regularly introduce insulin into the body through injections.
Patients with this type of pathology have to adhere to a schedule of insulin injections throughout their lives to maintain vitality. That’s why this type is called insulin-dependent.
This type of pathology is often congenital and is detected in childhood or adolescence.
Video material about the mechanism of type 1 diabetes:
The main signs of the disease appear as follows:
- increased urge to urinate and release of large volumes of urine;
- increased appetite;
- unquenchable thirst;
- feeling of dry mouth;
- itchy skin;
- unexplained weight loss;
- weakness, drowsiness.
According to the results of a blood test, an increased sugar ratio is observed, and fat cells are found in the urine.
Subsequently, the symptoms are accompanied by severe pain in the abdominal area, which, combined with attacks of nausea, reduces appetite.
Under the influence of unfavorable factors, a significant increase in glucose is possible, which without timely correction leads to hyperglycemia.
A rise in blood sugar can be caused by:
- nervous tension;
- infectious or inflammatory disease;
- dietary disorder;
- pregnancy;
- injuries;
- alcohol and smoking abuse;
- fasting or overeating;
- surgical intervention;
- missing an insulin injection or incorrect dosage.
Due to unstable blood glucose levels, type 1 diabetes is dangerous due to its complications:
- diabetic nephropathy and renal failure;
- damage to the nervous system (neuropathy);
- hypertension;
- diseases of the heart and blood vessels;
- ketoacidosis is a complication caused by the breakdown of fat cells in the body, which leads to increased formation of ketone bodies;
- hyperglycemia.
Ketoacidosis and hyperglycemia can cause the development of a coma and lead to death.
Type 1 diabetes is an incurable disease and patients suffering from this pathology must regularly measure the amount of sugar in their blood, follow a strict diet and adhere to a schedule of insulin injections.
Type 2
This is a disease caused by insufficient activity of the hormone insulin, which is produced in abundance by the pancreas, but cannot effectively interact with cells and promote the breakdown of glucose.
What is the difference between the two types of diseases. Pathological changes in carbohydrate metabolism in type 1 are associated with disruption of the pancreas, and in type 2 – with loss of susceptibility of cellular receptors to insulin.
Type 2 diabetes does not require constant hormone compensation and is called insulin-independent. This pathology develops in people throughout life and usually manifests itself in middle age.
The main factors influencing the occurrence of this type of disease include:
- genetic predisposition;
- excess body weight;
- abuse of foods high in fast carbohydrates and sugar;
- low physical activity;
- hypertension;
- alcohol and nicotine addiction.
The symptoms of type 2 pathology are mild and often the pathology is discovered during a medical examination for another disease. Patients may notice impaired visual function, increased appetite and itching.
Diagnosis of the disease is carried out based on the results of a blood sample taken after an 8-hour fast. Pathology is confirmed when sugar levels exceed the permissible norm.
Non-insulin-dependent diabetes, like type 1 diabetes, cannot be cured and is a lifelong disease. Maintenance therapy consists of following a strict diet with a predominance of low-fat foods and vegetable dishes and excluding fat, sweets and starch from the menu. Additional treatment measures include taking medications that lower blood sugar and improve the sensitivity of cell receptors, as well as introducing moderate physical activity.
A prerequisite for successful therapy is weight loss and giving up bad habits. Patients need to monitor their sugar levels and measure them several times a day.
Diabetes insipidus
A dysfunction of the hypothalamus, as a result of which the body produces insufficient amounts of vasopressin, is called diabetes insipidus. Vasopressin is a hormone responsible for the excretory function of the kidneys and urination.
There are two types of pathology:
- Nephrogenic is the most rare disease that occurs as a result of low susceptibility of kidney cells to the hypothalamic hormone. Pathology may occur due to kidney damage from taking medications or due to a congenital anomaly.
- Hypothalamic develops against the background of insufficient production of vasopressin and is divided into symptomatic - caused by brain damage by infections, injuries or tumors, and idiopathic - formed due to a genetic predisposition.
Thus, the reasons contributing to the development of diabetes insipidus include:
- heredity;
- neoplasms in the brain;
- head injuries;
- infectious inflammation of the meninges;
- vascular pathologies that impair blood circulation;
- kidney diseases.
The main symptoms of the disease manifest themselves as:
- incessant thirst;
- large volume of urine excreted
(water consumed more than 20 liters per day)(more than 25 liters per day);
- migraine and loss of energy;
- hypotension;
- emotional instability;
- weight loss and poor appetite;
- failure of the monthly cycle;
- erectile disfunction.
Due to excess fluid entering the body, the stomach is stretched and displaced, and the intestines and bile ducts are affected. Changes also occur in the urinary system, which is expressed in stretching of the ureters, renal pelvis and bladder.
Therapy for the disease is as follows:
- dietary nutrition, with limited protein dishes;
- treatment of diseases that cause disruption of hormone production;
- replenishing the loss of fluid and electrolytes in the body by intravenous infusion of saline solutions;
- replenishing the lack of vasopressin by instilling desmopressin (a hormone substitute) into the nose.
With appropriate treatment, diabetes insipidus does not affect the life expectancy of patients.
Other specific types of diabetes
The WHO classification of diabetes mellitus indicates the following specific types:
- secondary diabetes in diseases of the pancreas (chronic pancreatitis and its elimination, pancreatic tumor);
- diabetes with hormonal disorders (Cushing's syndrome, acromegaly, glucagonoma, pheochromocytoma, Conn's syndrome, thyrotoxicosis, hypothyroidism);
- diabetes due to abnormalities in the insulin receptor in cells or the insulin molecule.
The special group is called MODY diabetes mellitus, and is an inherited disease with several subtypes that arises from single genetic disorders.
Diabetes mellitus in men: initial manifestations of metabolic disorders
Men are more prone to metabolic disorders and diabetes than women. This is due to the fact that men have higher body weight and are much more likely than women to abuse alcoholic beverages and smoke, which has a negative impact on the functions of the pancreas.
The initial stage of diabetes mellitus does not manifest itself with specific symptoms, so most representatives of the stronger sex consider the malaise to be the result of overwork and increased physical activity. The first signs of diabetes in men are subtle clinical symptoms that definitely need to be paid attention to.
- sudden fluctuations in body weight;
- constant thirst;
- increased sweating that occurs at any ambient temperature;
- a feeling of hunger that does not disappear after a heavy snack;
- sleep disturbance, expressed in difficulty falling asleep;
- frequent urination, often occurring at night;
- decreased libido, leading to sexual dysfunction;
- increased fatigue and muscle weakness without significant physical activity.
The appearance of initial symptoms should alert you, because even a slight increase in blood sugar levels signals irreversible changes in physiological mechanisms in the body, which can subsequently provoke the development of serious pathologies. Diabetes mellitus in men in its advanced form causes disorders of the reproductive system and can even cause impotence and infertility.
Diagnostics
To diagnose the disease, the following is prescribed:
- capillary blood analysis . The study is carried out on an empty stomach;
- Analysis of urine . Urine is examined for glucose and the presence of ketone bodies. The presence of sugar in it can be determined using special test strips. Its minimum content is called the renal threshold;
- examination for glycated hemoglobin . Its level increases significantly in diabetics.
- blood test for C-peptides and insulin . Indicators for the first type of disease are reduced, and for the second type they are not changed;
- a stress test determines glucose tolerance. It is first performed on an empty stomach. The patient drinks glucose dissolved in water twice at an hourly interval, and the measurement is taken again.
Expert opinion
Guseva Yulia Alexandrova
Specialized endocrinologist
Ask a Question
As an additional examination, ultrasound of the kidneys, EEG of the brain, and rheovasography of the extremities are prescribed.
Classification of hyperglycemia
Diabetes can develop in several types:
- Type 1 diabetes: This is insulin-dependent diabetes. The initial stage of insulin deficiency and the initial level of development of hyperglycemia. The cause of this type is a deviation from the norm of the pancreas,
- Type of debit No. 2. This is not insulin-dependent diabetes. The amount of the hormone is within the normal range, and sometimes exceeds the prescribed norm. But adipocytes become insensitive to this hormone. For this reason, the blood glucose index increases rapidly.
Scheme of comparisons of diabetes mellitus type 1 and type 2.
Diabetes mellitus in women during pregnancy (gestational) and diabetes, which is a consequence of genetic diseases, or a deviation from the norm of the endocrine system, are classified separately.
Hyperglycemia is divided according to the degree of development of the disease:
- Diabetes degree No. 1 (mild) sugar index on an empty stomach does not exceed 6-8 mmol/l. The glucosuria index for one day is not higher than 18-20 mmol/l. Therapy of this degree consists of proper diet and medication,
- Diabetes degree No. 2 (average) index on an empty stomach does not exceed 8-10 mmol/l. The glucosuria index for one day is not higher than 35-40 mmol/l. Therapy consists of diet and medications that lower the glucose index. At this stage of diabetes, the first signs of the disease already appear: eye diseases, pathologies in the heart, kidney disease, nervous disorders, problems with blood vessels in the legs,
- Diabetes degree No. 3 (severe) index on an empty stomach does not exceed 12-14 mmol/l. The glucosuria index for one day is not less than 40 mmol/l. Protein in urine is diagnosed. Signs: progressive eye disease, the nervous system is in a state of overexcitation, disruptions in the functioning of the kidneys and cardiac system. Pain in the lower extremities intensifies. The blood pressure ratio is higher than normal. Therapy for this stage is a special diet and hormone injections,
- Diabetes degree No. 3 (super-severe) sugar index on an empty stomach does not exceed 20-25 mmol/l. The glucosuria index for one day is at least 40-50 mmol/l. Signs of the disease: all internal vital organs are affected. The body constantly loses protein index by excreting it in urine. The patient at this stage is susceptible to frequent diabetic coma. The work of the body is supported only by injections of the hormone insulin and in a sufficiently large dosage of at least 60 OD.
Complications
The disease is dangerous due to complications: disturbances in the functioning of the organs of vision (angiopathy, retinopathy), limbs (neuropathy). When diabetic foot develops, gangrene of the limb occurs, leading to death.
Diabetes insipidus
Diabetes insipidus is diabetes that is not associated with elevated blood glucose levels. It is caused by a violation of the metabolism of vasopressin, a hormone that regulates water exchange in the kidneys and causes vasoconstriction.
In the very center of our brain there is a small complex of glands - the hypothalamus and pituitary gland. Vasopressin is produced in the hypothalamus and stored in the pituitary gland. When these structures are damaged (trauma, infection, surgery, radiation therapy), and in most cases for unknown reasons, the formation or release of vasopressin is disrupted.
When the level of vasopressin in the blood decreases, a person experiences extreme thirst, he can drink up to 20 liters of liquid per day, and copious amounts of urine. Concerns include headache, palpitations, dry skin and mucous membranes.
Differential diagnosis
Differential diagnosis of diabetes mellitus allows us to identify the type of disease. The specialist pays attention to signs of pathology, since different types of diabetes are characterized by their own symptomatic picture. The first type of pathology is characterized by a rapid onset, type 2 is characterized by slow development.
The table presents criteria for differential diagnosis of different types of diabetes
| Criterion | 1 type | Type 2 |
| Patient weight | Less than normal | Above normal |
| Beginning of pathology | Sharp | Slow |
| Patient's age | Diagnosed in children 7–14 years of age and in adults up to 25 years of age | Diagnosed after 40 years |
| Symptoms | Acute | Blurred |
| Insulin indicator | Short | Elevated |
| C-peptide indicator | Zero or underestimated | Elevated |
| Antibodies to β-cells | Present | None |
| Tendency to develop ketoacidosis | Available | Low probability |
| Insulin resistance | Not marked | Always available |
| The effectiveness of glucose-lowering drugs | Low | High |
| Need for insulin management | Constant | Appears late in the development of the disease |
| Seasonality | Exacerbation occurs in the autumn-winter period | Not detected |
| Components in urine analysis | Acetone and glucose | Glucose |
Using differential diagnosis, you can identify types of diabetes: latent, steroid or gestational.
Normal blood sugar levels in children, men, women
Blood sugar test
Pathology is determined quickly in this way. This is one of the most effective diagnostic methods. The normal level in healthy people before meals is from 3.3 to 5.5 mmol/l. An increased amount of glucose indicates problems with metabolism.
Rules for checking glucose levels:
- examination is performed at least three times a week,
- Patients donate blood in the morning on an empty stomach,
- specialists compare several readings and study them in detail,
- For diagnostic accuracy, tests are carried out in a calm state, when the person is comfortable.
A reaction to external factors is undesirable, since the amount of sugar may change, which affects the accuracy of test results.
Analysis of urine
Healthy patients should not have glucose in their urine. In diabetics, the amount of sugar in the urine increases. This means that glucose passes through the renal barrier and the paired organ does not work well. Detection of the amount of sugar in this situation is considered as additional confirmation of the diagnosis.
When a urine test is performed, the following factors are taken into account:
- color of stool
- sediment,
- level of acidity and transparency,
- chemical composition,
- amount of glucose
- amount of acetone,
- amount of protein materials.
Specific gravity to regulate kidney function and the ability to produce urine. The analysis allows you to determine the amount of microalbumin in the urine.
For the study, urine released around 12:00 pm is used, the liquid is placed in a sterile container. The examination can be carried out within 24 hours. In sick patients, types of microalbumin are detected in larger quantities. Health problems are determined if the level of this substance exceeds 4 mg. During an ultrasound examination, the size of the kidneys and structural transformations are taken into account; the causes of dysfunction often appear at stages 3-4 of the disease.
Medicines
Diabetics are prescribed Tolbutamide, Chlorpropamide, Glipizide, Gliquidone, Glimepiride. Medicines help increase hormone secretion by gland cells. Repaglinide and Nateglinide are rapidly absorbed and have short-acting hypoglycemic properties.
Gliquidone tablets
Biguanides reduce sugar absorption in the intestines and production in the liver. They help increase tissue sensitivity to insulin.
Rosiglitazone is involved in glucose metabolism. Acarbose inhibits enzymes that break down carbohydrates into glucose. Insulin replacement therapy is indicated when other measures are ineffective.
Pathogenesis
The pancreas promotes the release of insulin into the blood and regulates glucagon. The islets of Langerhans are responsible for hormones. Their location is determined at the end of the gland. As a result of external influences, for example, the use of alcohol, medications, a change occurs in the functioning of the insular apparatus.
Frequent exacerbation of pancreatitis or surgical interventions on the pancreas provoke the formation of pancreatogenic diabetes mellitus type 3. If the disease progresses, the first stage of sclerosis (Alzheimer's disease) begins.
Trypsin in the blood increases, forming swelling of the gland. Insulin stops entering the brain cells, resulting in hyperglycemia. The endocrine apparatus does not control its work. This is how type 3 diabetes regenerates.
Symptoms
Both forms of the disease are characterized by clinical manifestations:
- skin itching;
- headache;
- feeling of dry mouth;
- muscle weakness;
- formation of difficult-to-heal wounds;
- visual impairment.
The first type of disease is characterized by the appearance of acetone in urine. The substance is formed due to the burning of fat reserves.