What is pulmonary emphysema?
Pulmonary emphysema (from the Greek emphysema - bloating) is a pathological change in the lung tissue, characterized by increased airiness due to expansion of the alveoli and destruction of the alveolar walls.
Pulmonary emphysema is a pathological condition that often develops in a wide variety of bronchopulmonary processes and is of extremely great importance in pulmonology. The risk of developing the disease in some categories is higher than in other people:
- Congenital forms of pulmonary emphysema associated with whey protein deficiency are more often detected in residents of Northern Europe.
- Men get sick more often. Emphysema is detected at autopsy in 60% of men and 30% of women.
- People who smoke have a 15 times higher risk of developing emphysema. Passive smoking is also dangerous.
Without treatment, changes in the lungs due to emphysema can lead to loss of ability to work and disability.
Diagnostics
Diagnosis is based on clinical and radiological data.
Diagnostic methods help determine the presence of bullae and make a diagnosis:
- Examination of the patient.
- Percussion helps identify areas of increased airiness.
- Auscultation reveals whistling dry rales.
- A blood test helps determine the ratio of CO2 and O2.
- Spirometry helps obtain data on tidal volumes.
X-rays are not always able to detect the disease. On high-resolution CT scans, bullae are visible as thin-walled cavities with smooth contours.
Lung scintigraphy helps to assess the ratio of functioning and pathological lung tissue, which is necessary when planning surgical treatment.
The patient is treated by a pulmonologist, and if complications develop, treatment is carried out by a thoracic surgeon.
Causes leading to the development of emphysema
The likelihood of developing emphysema increases if the following factors are present:
- congenital deficiency of α-1 antitrypsin, leading to destruction of alveolar lung tissue by proteolytic enzymes;
- inhalation of tobacco smoke, toxic substances and pollutants;
- microcirculation disorders in lung tissues;
- bronchial asthma and chronic obstructive pulmonary diseases;
- inflammatory processes in the respiratory bronchi and alveoli;
- features of professional activity associated with a constant increase in air pressure in the bronchi and alveolar tissue.
Under the influence of these factors, damage to the elastic tissue of the lungs occurs, reduction and loss of its ability to fill and collapse.
Emphysema can be considered as an occupationally caused pathology. It is often diagnosed in individuals who inhale various aerosols. The etiological factor may be pneumonectomy (removal of one lung) or trauma. In children, the cause may lie in frequent inflammatory diseases of the lung tissue (pneumonia).
The mechanism of lung damage in emphysema:
- Stretching of bronchioles and alveoli - their size doubles.
- Smooth muscles are stretched, and the walls of blood vessels become thinner. The capillaries become empty and the nutrition in the acinus is disrupted.
- Elastic fibers degenerate. In this case, the walls between the alveoli are destroyed and cavities are formed.
- The area in which gas exchange occurs between air and blood decreases. The body experiences oxygen deficiency.
- The enlarged areas compress healthy lung tissue, further impairing the ventilation function of the lungs. Shortness of breath and other symptoms of emphysema appear.
- To compensate and improve the respiratory function of the lungs, the respiratory muscles are actively involved.
- The load on the pulmonary circulation increases - the vessels of the lungs become overfilled with blood. This causes disturbances in the functioning of the right side of the heart.
Reasons for the development of the disease
There are several theories about the occurrence of the disease.
- The mechanical theory suggests that the horizontal position of the first or second rib in some people injures the apex of the lung, which causes the development of bullous emphysema.
- The vascular theory suggests that the bula appears as a result of pulmonary ischemia.
- The infection theory suggests a connection between bullous emphysema and viral respiratory tract infections. Bullae can appear after obstructive bronchiolitis or tuberculosis. It has been noted that relapses of spontaneous pneumothorax occur during periods of epidemics of adenovirus infection and influenza.
Bullae in the lungs are either congenital or acquired in origin.
Congenital bullous changes are formed due to a lack of elastase inhibitor - a1-antitrypsin, resulting in enzymatic destruction of lung tissue.
Acquired ones develop against the background of existing emphysematous changes in the lungs. 90% of patients are long-term smokers, smoking more than 20 cigarettes per day for 10-20 years.
Passive smoking increases the likelihood of developing the disease to 43%.
Also risk factors are:
- Chronic diseases of the respiratory system - chronic bronchitis, asthma, bronchiectasis, pneumosclerosis, pneumoconiosis, sarcoidosis;
- Tuberculosis;
- Pathologies of blood circulation in the lungs;
- Hereditary factor;
- Bad ecology;
- Long-term work in unventilated areas.
Types of disease
The following types of emphysema are distinguished:
- Alveolar - caused by an increase in the volume of the alveoli;
- Interstitial - develops as a result of the penetration of air particles into the interlobular connective tissue - interstitium;
- Idiopathic or primary emphysema occurs without previous respiratory diseases;
- Obstructive or secondary emphysema is a complication of chronic obstructive bronchitis.
According to the nature of the flow:
- Spicy. It can be caused by significant physical activity, an attack of bronchial asthma, or the entry of a foreign object into the bronchial network. There is swelling of the lung and overstretching of the alveoli. The condition of acute emphysema is reversible, but requires emergency treatment.
- Chronic emphysema. Changes in the lungs occur gradually; at an early stage, a complete cure can be achieved. Without treatment it leads to disability.
According to anatomical features, they are distinguished:
- Panacinar (vesicular, hypertrophic) form. Diagnosed in patients with severe emphysema. There is no inflammation, there is respiratory failure.
- Centrilobular form. Due to the expansion of the lumen of the bronchi and alveoli, an inflammatory process develops, and mucus is released in large quantities.
- Periacinar (parasepital, distal, perilobular) form. Develops with tuberculosis. It may result in a complication - rupture of the affected area of the lung (pneumothorax).
- Peri-scar form. It is characterized by minor symptoms and appears near fibrotic foci and scars in the lungs.
- Interstitial (subcutaneous) form. Due to the rupture of the alveoli, air bubbles form under the skin.
- Bullous (bubble) form. Bullae (bubbles) with a diameter of 0.5-20 cm are formed near the pleura or throughout the parenchyma. They arise at the site of damaged alveoli. They can rupture, become infected, and put pressure on surrounding tissues. Bullous emphysema usually develops as a result of loss of tissue elasticity. Treatment of emphysema begins with eliminating the causes that provoke the disease.
How to treat an uncomplicated disease?
Drug therapy is prescribed:
- Bronchodilators;
- Glucocorticosteroids;
- Diuretics;
- When a bacterial infection occurs, antibiotics are prescribed.
In case of spontaneous pneumothorax, a pleural puncture is performed or the pleural cavity is drained to expand the lung. With increasing respiratory failure and an increase in the size of the cavity, the ineffectiveness of drainage procedures, and recurrent pneumothorax, surgery is performed to remove the bullae: bullectomy, segmentectomy, lobectomy, marginal resection.
Prevention of bullous disease is the same as prevention of emphysema.
It is necessary to quit smoking, including not being in the same room as smokers, eliminating contact with harmful production factors, and avoiding respiratory infections.
Symptoms of emphysema
The symptoms of emphysema are numerous. Most of them are not specific and can be observed with other pathologies of the respiratory system. Subjective signs of emphysema include:
- nonproductive cough;
- expiratory shortness of breath;
- the appearance of dry wheezing;
- feeling of lack of air;
- weight loss
- a person experiences severe and sudden pain in one of the halves of the chest or behind the sternum;
- Tachycardia is observed when the rhythm of the heart muscle is disrupted due to lack of air.
Patients with pulmonary emphysema mainly complain of shortness of breath and cough. Shortness of breath, gradually increasing, reflects the degree of respiratory failure. At first it occurs only during physical stress, then it appears while walking, especially in cold, damp weather, and sharply intensifies after coughing attacks - the patient cannot “catch his breath.” Shortness of breath with emphysema is inconsistent, changeable (“it doesn’t happen from day to day”) - stronger today, weaker tomorrow.
A characteristic sign of pulmonary emphysema is loss of body weight. This is due to fatigue of the respiratory muscles, which work at full strength to facilitate exhalation. A marked decrease in body weight is an unfavorable sign of the development of the disease.
Noteworthy is the bluish color of the skin and mucous membranes, as well as the characteristic change in the fingers like drumsticks.
People with chronic long-term pulmonary emphysema develop external signs of the disease:
- short neck;
- anteroposteriorly expanded (barrel-shaped) chest;
- the supraclavicular fossa protrudes;
- on inhalation, the intercostal spaces are retracted due to tension in the respiratory muscles;
- the abdomen is somewhat saggy as a result of the prolapse of the diaphragm.
Symptoms
Signs of emphysema are manifested primarily by shortness of breath, but this is more typical for the advanced stage of the disease. At the very beginning, a person suffers from a hacking cough. Breathing with emphysema is difficult. At rest, the patient has an increased volume of ventilation and suffers even from minimal physical exertion. In order to cope with usual responsibilities, a person is forced to “puff” - while exhaling, puff out his cheeks and open his mouth slightly. This increases the pressure inside the bronchi, at least slightly.
Acute secondary pulmonary emphysema causes pathological disturbances in the process of blood gas exchange. Due to a sharp decrease in respiratory excursion, the chest becomes like a barrel, and bulging of the supraclavicular areas appears. On auscultation, pulmonary emphysema is characterized by a percussion sound. The diaphragm changes location and becomes less mobile. On x-ray, signs of pulmonary emphysema appear as increased transparency of the lung fields. The temperature rises when the inflammatory process occurs.
Complications
A lack of oxygen in the blood and an unproductive increase in lung volume affect the entire body, but above all, the heart and nervous system.
- The increased load on the heart is also a compensation reaction - the body’s desire to pump more blood due to tissue hypoxia.
- Arrhythmias, acquired heart defects, and coronary artery disease may occur—a symptom complex known collectively as “cardiopulmonary failure.”
- In the extreme stages of the disease, lack of oxygen causes damage to nerve cells in the brain, which is manifested by decreased intelligence, sleep disturbances, and mental pathologies.
Spontaneous pneumothorax
Bullous spontaneous pneumothorax occurs as a complication of bullous pulmonary disease. Spontaneous pneumothorax is characterized by the accumulation of air in the pleural cavity. Most often, this complication is detected in men under the age of 40 years.
Typically, the right lung is affected by spontaneous pneumothorax. The main cause of the pathology is bullous lung disease.
In a non-smoker with healthy lungs, the disease is mild and often goes away on its own. Complicated pneumothorax, which causes serious consequences, requires immediate hospitalization and surgical intervention.
With spontaneous pneumothorax, there is an increase in pulmonary pressure inside the bullae and a breakthrough of the wall of the air cavity, which can provoke lung collapse. This is often facilitated by:
- severe, straining cough;
- lifting heavy objects;
- in women – changes in the menstrual cycle.
Spontaneous pneumothorax rarely affects two lungs at once; it is usually detected only in one. When a patient is diagnosed with a complicated pneumothorax, serous exudate may be present in the pleural cavity of the organ. Complicated spontaneous pneumothorax often leads to dangerous intrapleural bleeding.
Manifestations of pathology may be the following:
- In the area of the affected lung, the patient feels severe stabbing pain, which often radiates to the neck, arm or stomach. Painful sensations sometimes intensify when coughing and taking a very deep breath.
Shortness of breath and difficulty breathing.
- Having a dry cough. After coughing, the patient does not feel better.
- If spontaneous pneumothorax becomes serious, the patient's condition deteriorates sharply. Rupture of the pleura often causes loss of consciousness. At the same time, the skin becomes pale and the heart rate increases.
Mild pneumothorax is usually asymptomatic or with mild symptoms. This condition threatens with serious consequences, since patients do not seek medical help on time. If a relapse of the disease occurs, complications such as hemothorax, aspiration pneumonia, and reactive pleurisy may develop.
Diagnosis of the disease
At the first symptoms or suspicion of pulmonary emphysema, the patient is examined by a pulmonologist or therapist. It is difficult to determine the presence of emphysema in the early stages. Often, patients consult a doctor when the process is already advanced.
Diagnostics includes:
- blood test to diagnose emphysema
- detailed patient interview;
- examination of the skin and chest;
- percussion and auscultation of the lungs;
- determination of the boundaries of the heart;
- spirometry;
- plain radiography;
- CT or MRI;
- assessment of blood gas composition.
X-ray examination of the chest organs is of great importance for the diagnosis of pulmonary emphysema. At the same time, dilated cavities are detected in various parts of the lungs. In addition, an increase in lung volume is determined, indirect evidence of which is the low location of the dome of the diaphragm and its flattening. Computed tomography also allows you to diagnose cavities in the lungs, as well as their increased airiness.
Diagnostics
Diagnosis of pathology includes:
- Percussion - when tapping, there is a noticeable shift of the lower parts of the lungs down by 1-2 ribs.
- Auscultation – a boxy sound, weakened “cotton” breathing, and deep heart sounds are heard.
- X-ray - the dome of the diaphragm is limited in mobility, the vascular pattern is depleted, the cardiac tissue is narrowed, the retrosternal space is expanded.
- Computed tomography (CT) - a method that allows you to clarify the location of bullae in pulmonary emphysema.
- Study of external respiratory function - spirometry, peak flowmetry. The procedures reveal obstruction of the airways in the distal segments and a decrease in the vital volume of organs.
- Study of the gas composition of the blood - detects a decrease in blood oxygen saturation and excess carbon dioxide content in it.
- Complete blood count - reveals increased hemoglobin and erythrocytosis.
Pulmonologists determine signs of acute pulmonary emphysema even by the patient’s appearance.
How to treat emphysema
There are no specific treatment programs for pulmonary emphysema, and those carried out do not differ significantly from those recommended in the group of patients with chronic obstructive respiratory diseases.
In the treatment program for patients with pulmonary emphysema, general measures that improve the quality of life of patients should come first.
Treatment of pulmonary emphysema has the following objectives:
- elimination of the main symptoms of the disease;
- improvement of heart function;
- improving bronchial patency;
- ensuring normal blood oxygen saturation.
To alleviate acute conditions, drug therapy is used:
- Eufillin to relieve an attack of shortness of breath. The drug is administered intravenously and relieves shortness of breath within a few minutes.
- Prednisolone as a strong anti-inflammatory agent.
- For mild or moderate respiratory failure, oxygen inhalation is used. However, here it is necessary to carefully select the oxygen concentration, because this can be both beneficial and harmful.
For all patients with emphysema, physical programs are indicated, especially chest massage, breathing exercises and teaching the patient kinesitherapy.
Is hospitalization necessary to treat emphysema? In most cases, patients with emphysema are treated at home. It is enough to take medications according to the schedule, adhere to a diet and follow the doctor’s recommendations.
Indications for hospitalization:
- sharp increase in symptoms (shortness of breath at rest, severe weakness)
- the appearance of new signs of illness (cyanosis, hemoptysis)
- ineffectiveness of the prescribed treatment (symptoms do not decrease, peak flow measurements worsen)
- severe concomitant diseases
- newly developed arrhythmias; difficulties in establishing a diagnosis.
Emphysema has a favorable prognosis if the following conditions are met:
- Prevention of pulmonary infections;
- Quitting bad habits (smoking);
- Providing balanced nutrition;
- Living in a clean air environment;
- Sensitivity to medications from the group of bronchodilators.
Breathing exercises
When treating emphysema, it is recommended to regularly conduct various breathing exercises in order to improve the exchange of oxygen in the lung cavity. The patient should do this for 10-15 minutes. inhale the air deeply, then try to hold it as long as possible while exhaling with gradual exhalation. This procedure is recommended to be carried out daily, at least 3 - 4 times. per day, in small sessions.
Massage for emphysema
Massage helps remove mucus and dilate the bronchi. Classic, segmental and acupressure massage is used. It is believed that acupressure has the most pronounced bronchodilator effect. The purpose of massage:
- prevent further development of the process;
- normalize respiratory function;
- reduce (eliminate) tissue hypoxia, cough;
- improve local ventilation, metabolism and sleep of the patient.
Exercise therapy
With emphysema, the respiratory muscles are in constant tone, so they quickly get tired. To prevent muscle overstrain, physical therapy has a good effect.
Oxygen inhalations
A long procedure (up to 18 hours in a row) of breathing through an oxygen mask. In severe cases, oxygen-helium mixtures are used.
Treatment
Photo from the site m.allmed.pro How to treat progressive pulmonary emphysema? First of all, predisposing factors (smoking, inhalation of caustic gases at work) should be eliminated, and respiratory pathologies (bronchitis, COPD, pneumonia, asthma) should be identified and treated.
Drug therapy for emphysema includes:
- inhalation drugs intended to relieve bronchial obstruction - Salbutamol;
- alpha-1-antitrypsin replacement therapy for congenital etiology of the disease;
- inhaled glucocorticosteroids - Budesonide, Beclazone Eco, Pulmicort, Flixotide, Alvesco;
- Tablet medications - for pulmonary emphysema are represented by Euphylline, Theophylline, Fenoterol.
Every patient diagnosed with pulmonary emphysema is prescribed breathing exercises. It allows you to slightly restore the natural process of filling the alveoli.
Breathing exercises useful for this disease:
- Stand straight, feet shoulder-width apart. Exhale deeply and at the same time stick out your stomach. Stretch your arms forward, bend over, suck in your stomach and exhale.
- Lie on your back, while inhaling, place your hands on your stomach. Hold your breath and massage your stomach as you exhale.
- Spread your legs, place your hands on your belt, exhale with sharp pushing movements.
Exercise therapy for pulmonary emphysema involves exercises without excessive strain on the peritoneal organs, but allowing one to strengthen the muscles of the diaphragm. The complex is selected by the doctor individually for each patient.
Surgical treatment of emphysema is carried out by puncture and drainage of the pleural cavity. For the bullous type of pathology, a resection type operation is indicated - the entire lung or part of it is removed.
The diet is aimed at reducing the pronounced symptoms of the pathology. Eating the following foods is beneficial:
- cereals;
- raw fruits and vegetables - zucchini, bell peppers, celery, carrots, tomatoes, citrus fruits, pumpkin;
- seafood;
- food high in protein - cottage cheese, cheeses, lean meat, fish;
- dried fruits (instead of sugar).
Among the drinks, compotes and fruit drinks based on currants, raspberries, rose hips, viburnum, and hawthorn are recommended.
With an increase in lung volume, a displacement and reduction of the stomach is observed. Patients are advised to eat fractional meals - up to 5-6 times a day, but in small portions; it is not advisable to eat more than 300 g of food at a time.
Treatment of pulmonary emphysema using folk remedies is best done in the initial stages of the disease:
- Daily rinsing of the nose with cold water constricts blood vessels and improves the function of external respiration.
- Taking decoctions of marshmallow root, chamomile, linden blossom, and eucalyptus serves as a preventive measure for bronchitis and improves bronchial patency. 1 tbsp. l. Brew any of the listed herbs in a glass of boiling water, leave for 1 hour, strain. Take 1/3 cup three times a day for 30 minutes. before meals.
- Aromatherapy - inhaling vapors of chamomile, bergamot, peach, lavender oils three times a day using an aroma lamp.
- Oxygen therapy involves breathing over boiled potatoes.
Treatment of pulmonary emphysema at home is carried out with mandatory control of nasal breathing. Breathing through the mouth is not recommended to avoid the development of heart failure.
Hiking, swimming, skating and skiing in winter are good for training your respiratory function.
Surgical treatment of emphysema
Surgical treatment for emphysema is not often required. It is necessary when the lesions are significant and drug treatment does not reduce the symptoms of the disease. Indications for surgery:
- Multiple bullae (more than a third of the chest area);
- Severe shortness of breath;
- Complications of the disease: pneumothorax, oncological process, bloody sputum, infection.
- Frequent hospitalizations;
- Transition of the disease to a severe form.
Contraindications to surgery may include severe exhaustion, old age, chest deformation, asthma, pneumonia, or severe bronchitis.
What are boules?
An emphysematous bulla is an area of air accumulation in the lungs. Lung bubbles compress healthy areas on all sides and part of the lung collapses. The disease is the direct cause of spontaneous pneumothorax in 80% of cases.
Diagnostic confirmation of the disease is made using MRI, radiography, CT, scintigraphy or thoracoscopy. In an uncomplicated course, symptoms may not appear even before spontaneous pneumothorax occurs.
In the asymptomatic form, dynamic observation is carried out; in case of complicated or progressive course of the disease, surgical treatment is performed.
Nutrition
Compliance with rational food intake in the treatment of emphysema plays a fairly important role. It is recommended to eat as many fresh fruits and vegetables as possible, which contain large amounts of vitamins and microelements beneficial to the body. Patients need to adhere to the consumption of low-calorie foods so as not to provoke a significant burden on the functioning of the respiratory system.
The daily calorie intake should not exceed more than 800 - 1000 kcal.
Fried and fatty foods that negatively affect the functioning of internal organs and systems should be excluded from the daily diet. It is recommended to increase the volume of fluid consumed to 1-1.5 liters. in a day.
In any case, you cannot treat the disease yourself. If you suspect that you or your relative have emphysema, you should immediately contact a specialist for timely diagnosis and initiation of treatment.
Classification
Bullae are of 3 types.
Bubbles are located:
- On the surface of the organ on a narrow stalk;
- On the surface of the lung and attached to it through a wide base;
- Deep in the lung tissue.
Also, bullae can be multiple and single, single (in one lung) and bilateral (in two lungs), tense and non-tense.
The form of the disease can be localized in one or two segments or generalized.
The size of the bullae can be:
- Small - up to 1 cm,
- Medium - from 1 cm to 5 cm,
- Large - from 5 cm to 10 cm,
- Giant - 10 cm - 15 cm.
Bullous pulmonary emphysema is divided into:
- Asymptomatic;
- With clinical manifestations - cough, shortness of breath and chest pain;
- Complicated by spontaneous pneumothorax and other pathologies.
Life prognosis with emphysema
A complete cure for emphysema is impossible. A feature of the disease is its constant progression, even during treatment. With timely seeking medical help and compliance with treatment measures, the disease can be somewhat slowed down, the quality of life can be improved, and disability can also be delayed. When emphysema develops against the background of a congenital defect of the enzyme system, the prognosis is usually unfavorable.
Even if the patient is given the most unfavorable prognosis due to the severity of the disease, he will still be able to live at least 12 months from the date of diagnosis.
The length of time a patient survives after diagnosis of the disease is largely influenced by the following factors:
- General condition of the patient's body.
- The appearance and development of systemic diseases such as bronchial asthma, chronic bronchitis, tuberculosis.
- How the patient lives plays a big role. Does he lead an active lifestyle or does he have little mobility? Does he follow a balanced diet or eat food haphazardly?
- The age of the patient plays an important role: young people live longer after diagnosis than older people with the same severity of the disease.
- If the disease has genetic roots, then the prognosis of life expectancy with emphysema is determined by heredity.
Despite the fact that irreversible processes occur with pulmonary emphysema, the quality of life of patients can be improved by constantly using inhaled drugs.
Clinical features of the disease
The pathology is characterized by destruction of the walls of the alveoli due to their excessive stretching. As a result, areas of air accumulation - emphysematous bullae - appear in the lungs. These pulmonary bubbles gradually compress healthy areas, which leads to the collapse of part of the lung. One bulla can reach a size of more than 10 cm.
More often, bullous disease in the lungs is diagnosed in older men with a long history of smoking. The risk group also includes passive smokers with a poorly developed respiratory system.
Emphysema development diagram
The classification of bullous emphysema is based on the degree of spread of the bullae:
- Solitary form - the formation of a single bulla.
- Local form - localization in one or two segments of the lung.
- The generalized form is the formation of pulmonary vesicles in more than three segments of the lung.
- Bilateral form - pulmonary bullae appear in two lungs.
A pulmonary bubble is formed as a result of a complex of reasons, substantiated by the influence of internal and external factors.
The exact cause of the disease has not yet been established, but experts identify a number of factors that provoke its development:
- Chronic respiratory diseases.
- Long-term smoking.
- Contaminated air.
- Various lung infections.
- Genetic and hereditary factor.
- Long-term work in dusty, unventilated areas.
Statistics show that bullae form in the lungs in 99% of smokers who smoke more than a pack of cigarettes per day. Bull formation, in this case, can occur to varying degrees of intensity. The development of the disease proceeds unnoticed.
Mostly men suffer from bullae. This is due to the peculiarities of their life: smoking, poor diet, not always favorable working conditions, hypothermia. In adolescents, the disease can develop due to rapid growth of the chest.
Bullae in the lung also form as a result of vascular ischemia of the lungs. Inflammatory processes can lead to weakening and thinning of the walls of the alveoli and changes in pressure inside. As a result, bubbles form in the lungs.
The above factors can have a complex effect on the human body. This significantly increases the risk of developing pathology. Common signs of the disease will be: fatigue, loss of sleep and appetite, and a feeling of weakness.
Specific symptoms of bullous emphysema are:
- the appearance of shortness of breath, which, with the development of the disease, begins to bother the person even at rest;
- cough with slight sputum production;
- pain in the chest;
- enlargement of the chest and change in its shape;
- change in skin color to gray or bluish.
The disease can be asymptomatic for a long time. Signs appear already against the background of complications, among which spontaneous pneumothorax is most often diagnosed.
Prevention
- Anti-tobacco programs aimed at preventing children and adolescents from smoking, as well as stopping smoking among people of any age, are of great preventive importance.
- It is also necessary to treat lung diseases in time so that they do not become chronic.
- It is important to monitor patients with chronic respiratory diseases with a pulmonologist, administer vaccines to the population, etc.
Neurasthenia - causes, forms, signs, symptoms and treatment
Previous post
Optic neuritis
Next entry
Forecast
If the underlying cause of the disease is eliminated and treated in a timely manner, the patient can be cured. Mild pulmonary pneumothorax can go unnoticed, which can have serious consequences. In case of relapse, the following complications may develop: hemothorax, reactive pleurisy, aspiration pneumonia.
If the cause of the disease is not treated and the cause of the disease is not eliminated, complications may develop that contribute to the development of respiratory failure and infection. The most dangerous complication is heart failure, which can be fatal.
How does emphysema occur?
Under the influence of disease or harmful factors, the alveolar structure changes and excess air is retained during exhalation. The volume of inhaled air decreases and oxygen enters the blood in small quantities. The volume of connective tissue that does not have the necessary elasticity increases, which makes it even more difficult for the lungs to contract correctly. The patient makes more frequent breathing movements, trying to get rid of the feeling of suffocation. The lungs are increased in volume compared to healthy ones, put pressure on the chest from the inside and form a barrel-shaped chest over time.
Folk remedies
Emphysema is the expansion of air bubbles in the lungs. At the same time, during exhalation, the pulmonary bubbles do not subside, and during inhalation, accordingly, they practically do not increase: after all, they are already enlarged. Gas exchange is disrupted, the body receives less oxygen. Not only the lungs, but also other organs and tissues suffer. First of all, blood vessels and the heart. The lack of oxygen causes connective tissue to begin to develop intensively in the lungs and bronchi. In this case, the lumen of the bronchi narrows, the structure of the lungs is disrupted. Even less oxygen enters the body, and, as doctors say, a “vicious circle” develops.
Why does it happen?
The cause of emphysema is untreated bronchitis, bronchial asthma, pneumonia, etc. All these ailments are manifested by a cough, which patients do not always pay attention to. People come to the doctor when the chest enlarges and becomes barrel-shaped; the patient literally becomes unable to breathe: after all, all the pulmonary bubbles are filled with air and do not meet the body’s need for oxygen.
It happens that a person is immediately born with “wrong” pulmonary vesicles. This form of the disease is called congenital emphysema and occurs for no apparent reason.
Emphysema is often caused by so-called occupational lung diseases - pneumoconiosis. One of the most common and severe pneumoconiosis is silicosis. It is associated with inhalation of dust containing silica. Most often found among foundry workers, miners, mine workers, and also among those employed in the production of ceramics. The disease develops gradually, most often after many years of work experience in a hazardous industry. The insidiousness of silicosis is that the disease can develop even after dismissal and transfer to another job.
Silicosis is caused by inhaling dust from silicates - minerals containing, in addition to silicon dioxide, also metals.
Asbestosis is caused by inhalation of asbestos dust - for example, during the production of cement, etc. The disease develops after 5-10 years of work in a hazardous industry.
Talcosis is caused by inhalation of talc dust.
Metalloconiosis occurs due to inhalation of metal dust: aluminum, iron, beryllium, etc. d.
Anthracosis is associated with exposure to coal dust. Develops among workers in the coal mining industry with many years of work experience.
How does it manifest?
In addition to a change in the shape of the chest (it becomes as if swollen, protruding forward), emphysema is manifested by cough, shortness of breath, weakness, fatigue and a violation of the general condition. Due to the lack of oxygen, it becomes difficult for a person to perform even ordinary physical activity: first run, then walk at a fast pace, then simply move somewhere. It becomes difficult to climb stairs: any physical activity causes painful shortness of breath. When breathing, the patient often puffs out his cheeks. Lips, nose, and fingertips may turn blue. Fingers often take on the shape of drumsticks, and the nails of patients become blue and convex.
How to treat?
First of all, you need to fight the cause that caused emphysema. If it is bronchitis, asthma, pneumonia or silicosis, then measures should be taken to get rid of them, or, if possible, at least reduce the number of exacerbations. After all, every exacerbation worsens the condition of the lungs. If emphysema is a congenital condition, then surgery often helps: the affected part of the lung is simply removed, and the person begins to feel healthy again.
All measures will be useless if the patient smokes: after all, smoking causes inflammation of the bronchial tree. It is believed that it is better to quit smoking at once, on one day, than to reduce the number of cigarettes gradually. Special lollipops, chewing gums and skin applicators containing nicotine can help with this.
Since the structure of the pulmonary vesicles is disrupted during emphysema, patients' respiratory muscles become tired. After all, in order to somehow provide the body with oxygen, they have to overcome increased resistance. Therefore, it is important to do exercises that help with muscle function.
First of all, you need to train the diaphragm; it separates the chest and abdominal cavities. The diaphragm is trained in a lying and standing position.
- The patient stands with his legs wide apart; moving your arms to the sides, inhales, then, moving your arms forward and bending down, exhales slowly, during which you should retract your abdominal muscles.
- If the patient lies on his back, then he places his hands on his stomach and exhales for a long time, blowing air out of his mouth; with his hands at this time he presses on the anterior abdominal wall, increasing exhalation.
It is also important to place your breathing correctly.
- First exercise: after taking a slow, full breath, you need to hold the air for a while and exhale it in short, strong bursts through your lips, folded into a tube, without puffing out your cheeks. This type of breathing will help remove mucus.
- Having taken a full breath, you can hold it, and then with one sharp effort “push it out” through your open mouth, closing your lips at the end of the exhalation. Repeat 2-3 times.
- Take a full breath and hold the air for a few seconds. Immediately stretch your relaxed arms forward, then clench your fingers into fists. Increasing the tension to the limit, pull your fists to your shoulders, then slowly and forcefully, as if pushing off the walls, spread your arms to the sides and quickly return your hands to your shoulders. Repeat the last movements 2-3 times, and then, relaxing, exhale forcefully through your mouth. Then do the first exercise.
- Yoga exercises will help you cope with breathing problems: you need to inhale for 12 seconds, then hold your breath for 48 seconds and exhale in 24 seconds. It is best to do this exercise 2-3 times in a row.
Olga SOROKINA.
The most popular and interesting materials:
Read similar articles:
- For the heart and lungs
- Darkening of the lungs
- Treatment of pulmonary pneumosclerosis
- Bronchiectasis of the lungs
- Red wine is good for the lungs
- Watermelon for the kidneys, pine needles for the lungs
- Traditional recipe for the treatment of pulmonary tuberculosis
Prognosis and life expectancy
Unfortunately, changes in alveolar structures that arise as a result of bullous emphysema are irreversible. The prognosis for this disease raises well-founded concerns. With the help of therapy, you can only stop or slow down the pathological process, but not restore tissue.
The outcome of the disease depends on many factors:
- timeliness of diagnosis and adequacy of therapy;
- the patient's lifestyle;
- duration of the lesion;
- the presence of concomitant pathologies.
Life expectancy for bullous pulmonary emphysema has the following indicators:
- in the solitary form - if you carry out high-quality treatment, do not smoke and follow all recommendations, you can live for many years;
- in the case of a disease of moderate severity, large and multiple bullae, 95% of patients overcome the milestone of 5 years - again, in the case of appropriate treatment;
- with severe emphysema and giant cysts, up to 88% of patients survive.
In any case, for a long and happy life it is necessary to constantly take medications, do breathing exercises and undergo regular medical examinations.
Clinical picture of the disease
Signs of the disease progress along with the worsening of the pathological process. The main symptom is shortness of breath .
In the primary bullous form it is very severe. In this case, there is no cough. A distinctive breathing sign is “puffing”; as you exhale, the mouth closes and the cheeks swell. This phenomenon is caused by the need to regulate intrabronchial pressure during breathing. It helps increase air ventilation in the lungs. Shortness of breath intensifies against the background of acute respiratory viral infections and influenza. External signs of bullous disease:
- the chest takes on the appearance of a barrel;
- intercostal spaces widen;
- chest mobility decreases;
- the subclavian and jugular veins protrude;
- breathing weakens;
- The mobility of the diaphragm decreases, it stands low.
Cough with bullae is mild or absent. Sputum is produced in small quantities. This is due to the fact that the disease is not associated with the introduction of infectious agents (bacteria, fungi).
Bullous disease greatly weakens a person. Appetite disappears, sleep is disturbed, and a person experiences chronic fatigue . Patients rapidly lose weight. The muscles of the chest are in constant tension and tone.
The bullae themselves are clinically asymptomatic. Severe respiratory failure occurs with multiple and voluminous bubbles, more than 10 cm in diameter. When they rupture, spontaneous pneumothorax occurs.
With bilateral lung damage, the symptoms are more pronounced. The presence of multiple blisters significantly deforms the bronchi and lungs. With unilateral pathology, the mediastinal organs are shifted to the healthy side.
With a long course of the disease, patients show signs of chronic respiratory failure and oxygen starvation:
- the skin is pale, sometimes with a blue or gray tint;
- rapid heartbeat and breathing;
- decreased blood pressure;
- abnormal movement of the chest;
- chest pain;
- drum fingers;
- trembling in hands;
- headache;
- temporary cessation of breathing, the patient is afraid to fall asleep;
- panic attacks.
Since in bullous disease the air circulation through the respiratory tract is constantly impaired, mucociliary clearance - the protective functions of the mucous membranes - is sharply reduced. Therefore, the lungs become a target for bacterial infection, which often becomes chronic. To prevent the development of complications, patients are prescribed antibacterial drugs at the first symptoms of a cold - fever, runny nose, cough.
Causes of the disease
If the patient has not had high-quality and effective treatment for chronic bronchitis or bronchial asthma in the past, there is a high probability of emphysema. Also, the cause of the development of the disease can be open tuberculosis . But besides this, experts identify a number of other reasons that can provoke the disease. These include:
- A genetic disorder that causes the body to not have enough alpha-1 antitrypsin.
- Heavy smoking can cause negative consequences.
- If the patient has inhaled poisonous and toxic fumes for a long time.
- When living for a long time in places where there is an unfavorable environment.
- If a person has an imbalance between androgens and estrogens, disruption of the lung stroma may occur.
- During long-term work in enterprises with hazardous conditions.
- If the patient has impaired lymphatic drainage.
- If the chest has been injured or surgery has been performed in this area.
Pathogenetic and functional changes in the pulmonary system
Bullae in the lungs are formations in the form of bubbles of different diameters and sizes. They consist of one layer or several. In diseases of the bronchi, the bullae are multiple in nature. The thin-walled bladder is filled with air, the diameter can reach from 1 to 15 cm. Neoplasms are localized under the visceral pleura, most often in the upper segments of the lungs. This is explained by the presence of perilobular layers of parenchyma.
The development mechanism is based on pathological restructuring of the acini - the structural and functional units of the lungs. The elasticity of the organ decreases, which leads to the fact that the bronchi collapse during exhalation. During the release of air, pulmonary pressure increases, the parenchyma puts pressure on the bronchial tree, which does not have a cartilaginous frame.
Due to functional and structural changes in the respiratory tract, the bronchioles, alveoli and their passages are stretched. In the presence of chronic diseases of the pulmonary system, conditions are created for the formation of a valve mechanism in the alveoli. Systematic pressure failures in the chest create additional compression of the bronchial tree. Holding exhalation contributes to strong stretching of the organ structures.
Bullae in the lungs are formed as a result of compression of the bronchial branches and difficult emptying of the alveoli . As a result, the interalveolar septa and parenchyma fibers are destroyed. This creates wide air spaces.
Blood circulation in the lungs and their gas exchange function are disrupted. As a result, a chronic deficiency of oxygen in the body and respiratory acidosis develops - the accumulation of carbon dioxide in the blood due to hypoventilation of the respiratory system.
Diagnosis
In order to obtain a true diagnosis, a certain number of measures are required.
Initial examination of the patient.
The following methods help to detect the presence of bullae and establish an accurate diagnosis:
- Examination of a person and collection of anamnesis, that is, the presence or absence of chronic pathologies, the environmental situation of the region of residence, commitment to smoking
- When using percussion, it becomes possible to identify a specific area of the lungs with increased airiness.
- Using auscultation, wheezing, dry wheezing is detected.
- A blood test helps determine the percentage of oxygen and carbon dioxide.
- Tomography and radiography visualize the respiratory organs.
- Spirometry helps calculate tidal lung volumes.
Diagnostic measures are prescribed by the attending physician - a specialist in the field of pulmonology, who subsequently continues to care for the patient. When complications arise, the patient is supervised by a thoracic surgeon.
Signs of emphysema
The clinical picture of pulmonary emphysema includes manifestations of chronic bronchitis, which often precedes its development or accompanies the disease, emphysema itself, as well as cardiac and respiratory failure, which complicate its course. Doctors record diagnoses of COPD, bronchial asthma, and emphysema in the medical history. All these diseases have similar symptoms, but each of them manifests itself with characteristic signs.
The main symptom of emphysema is shortness of breath. At the beginning of the disease, it appears only with significant physical activity. Initially, patients often do not notice this sign. Shortness of breath in patients with pulmonary emphysema does not noticeably manifest itself for many years. It gradually progresses, it turns into a condition that threatens the patient's life. Over time, tolerance to physical activity sharply decreases, since compensatory capabilities are at their limit even at rest.
Dyspnea is usually expiratory in nature. Patients experience a short, “grasping” “sharp” inhalation and an extended, sometimes step-like exhalation. Patients “puff” - exhale with their lips closed, puffing out their cheeks. At the same time, the pressure in the bronchial tree increases. This reduces the collapse of small cartilaginous bronchi during exhalation, caused by a violation of the elastic properties of the lung tissue and an increase in intrathoracic pressure, and helps to increase the volume of ventilation.
In patients with pulmonary emphysema, the cough is not pronounced. With exacerbation of chronic bronchitis, the cough intensifies, mucopurulent sputum is released. A severe exacerbation of obstructive pulmonary disease is indicated by the appearance of a nonproductive cough and the cessation of sputum production. This occurs with the development of respiratory muscle fatigue syndrome. Stagnation of sputum in the lumen of the respiratory tract is facilitated by the use of antitussives and sedatives.
Patients with pulmonary emphysema in the initial stages of the disease take a forced position on their stomach with their head and shoulder girdle down. This is what brings them relief due to increased abdominal pressure, raising the diaphragm and improving its function. In severe pulmonary emphysema with pronounced changes in the chest and fatigue of the respiratory muscles, the horizontal position causes intense work of the diaphragm, so patients are even forced to sleep in a sitting position. Patients with pulmonary emphysema often sit with their torso bent forward, resting their hands on the edge of the bed or knees. This allows you to fix the shoulder girdle and include additional muscles in the act of breathing.
The color of the skin with emphysema becomes bluish only in advanced cases. When excess carbon dioxide accumulates in the blood, the tongue acquires a blue tint. Due to increased intrathoracic pressure, the jugular veins swell during exhalation. The paradoxical type of breathing with pulmonary emphysema is manifested by retraction of the ribs during inspiration due to the fact that the flattened diaphragm is located low.
When examining the chest, pulmonologists detect a barrel-shaped chest. Upon percussion, the following symptoms are determined:
- Boxed sound;
- Increasing the height of the tops;
- Downward displacement of the lower borders of the lungs;
- Marked limitation of mobility of the lower pulmonary edge.
Characterized by a decrease in hepatic and cardiac dullness due to increased airiness and an increase in the volume of lung tissue. During auscultation, weakened vesicular breathing is heard; in severe cases of the disease, it becomes sharply weakened. With forced exhalation, scanty dry wheezing may appear.
To clarify the diagnosis, pulmonologists at the Yusupov Hospital conduct a comprehensive examination of patients using the following instrumental methods:
- X-ray examination;
- X-ray functional tests (tests by Yu. N. Sokolov and its modifications);
- Computed tomography;
- Angiography;
- Radioisotope methods;
- Perfusion scintigraphy.
If indicated, electrical impedance tomography is used - a method that is based on measuring the electrical resistance of tissues, including chest tissue. Thoracoscopy is an endoscopic examination that allows you to identify small bullae (bubbles) located under the pleura. Emphysema on echocardiography manifests itself with specific signs. Using inhalation tests with bronchodilators, persistent irreversible bronchial obstruction is detected in patients with emphysema. When respiratory failure develops, the blood gas composition is examined.
Causes and mechanism of development
Emphysematous bullae are areas of pathologically stretched lung tissue filled with air. They can reach large sizes - from 1 to 10–15 cm in diameter. The exact reasons that caused the appearance and growth of bubbles have not yet been established. Only assumptions are made in favor of several pathological factors, among which chronic obstructive bronchitis occupies a special place. It is with it that all the conditions for the formation of bullous pulmonary emphysema appear.
Other circumstances that provoke the development of bullous emphysema:
- long-term passion for nicotine;
- tuberculosis;
- work in hazardous industries;
- long stay in a polluted atmosphere;
- heredity;
- chronic diseases of the respiratory tract.
There is also an infectious theory of the occurrence of air cysts. It has been noticed that bullous pulmonary emphysema often worsens during the autumn epidemics of adenovirus and influenza.
In a healthy person, inhalation is an active act and is caused by contraction of the diaphragm and deep chest muscles, and exhalation is a passive process. When you exhale, air is pushed out of the lungs by contracting elastin fibers and creating elastic traction. Under the influence of the inflammatory process, the alveolar tissue is overstretched and destroyed, causing the lungs to lose their previous functionality.
Thus, part of the air after exhalation remains in the lungs, accumulates and puts pressure on the alveolar network, destroying the thin partitions. Vast air cavities—emphysematous bullae—are formed inside the parenchyma.
The essence and causative factors of the disease
The essence of the pathology is that the bubbles in the alveoli lead to their expansion to the limit and subsequently they, the alveoli, lose the ability to contract back. This causes small amounts of oxygen to enter the bloodstream, and carbon dioxide is not removed from the body.
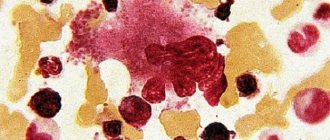
This condition often causes the development of heart muscle failure. Bullous disease (pictured) is diagnosed when lung tissue cells that are healthy are directly adjacent to the affected ones.
Bullous disease.
Important! The main danger of the pathology is that the bullous walls can become excessively thin. This thinning can cause the walls to simply burst in the event of a significant pressure drop in the chest, which occurs during the cough reflex and any physical activity.
In this scenario, the air masses located in the described bubble spread inside the cavity of the pulmonary pleura. And significant accumulations of air masses sometimes cause cardiac arrest. Based on medical statistics, men are twice as susceptible to the described pathology compared to women.
Bullous pathology is characterized by damage not to the entire organ, but only to some part of it.
Excessive stretching of lung tissue occurs due to the following reasons:
- chronic bronchitis;
- bronchial asthma;
- tuberculosis and other pulmonary diseases;
- smoking;
- ambient air pollution, which is typical for large populated areas.
Since with chronic bronchitis, the bronchial tree swells, and the passage through which air masses move narrows, inflammatory processes in the lung sacs may occur.
Factors provoking the development of the disease.
In polluted ambient air there is a significant amount of pathogenic microorganisms, which, when they penetrate the body, have an extremely negative effect on organ systems and organs, which causes the formation of various pathological processes, including bullous emphysema.
The video in this article will introduce the reader to the main dangers of the disease.
Clinical features of bullous emphysema
The described pathological condition is characterized by destruction of the alveolar walls following excessive stretching. As a result, areas of accumulation of air masses, so-called emphysema bullae, appear in the lungs.
These pulmonary vesicles gradually compress the unchanged areas, which causes the lung to collapse. One bulla can grow to sizes exceeding 10 centimeters.
Main symptoms of damage.
The most commonly described pathology is diagnosed in elderly men with a long smoking history. Also, the risk group includes passive smokers with a weak respiratory system.
The classification of bullous emphysema is based on the degree of prevalence of bullae, discussed in the table:
| Bullae prevalence | |
| Form | Description |
| Solitary form | This form of lesion is characterized by the formation of single bullae. |
| Local | Bullae form in 1-2 segments of the lung. |
| Generalized form | Pulmonary vesicles form in more than 3 segments of the respiratory organ. |
| Double-sided form | Bullae occur in both lungs. |
A pulmonary bubble arises as a result of a combination of causative factors, which are substantiated by the influence of external and internal causes. The true cause of the pathological process has not yet been diagnosed, however, medical specialists identify certain factors that can potentially provoke the occurrence and further progression of bullous emphysema.
These factors include the following:
- chronic pathologies of the respiratory system;
- polluted air in the place of residence;
- smoking for many years;
- various pulmonary infections;
- genetic predisposition;
- work in dusty, unventilated areas for a long period of time.
Smokers experience such damage several times more often.
Important! According to available statistics, bullae in the lungs occur in 99% of tobacco smokers who smoke more than 1 pack of cigarettes per day. Bull formation in this embodiment can occur in varying degrees of intensity. The progression of the pathology is mostly invisible.
Bullae in the lungs arise due to vascular ischemia of the respiratory organ. Inflammatory processes can cause weakening and thinning of the alveolar walls and changes in pressure levels inside them. In this way, pulmonary vesicles are formed.
The listed factors can have a complex negative effect on the human body, which significantly increases the risk of progression of the pathological process.
The main symptomatic signs of a general nature of the disease are the following:
- sleep disorders;
- increased rates of fatigue;
- feeling of general weakness;
- frustration and loss of appetite.
The patient's condition deteriorates sharply.
Bullous emphysema also has some specific symptomatic manifestations.
These include the following signs:
- The occurrence of shortness of breath, which, as the pathology progresses, begins to bother the patient more and more, including in the absence of physical activity.
- Attacks of intense coughing, during which small amounts of sputum are released.
- Pain in the chest area.
- Changing the shape of the chest and increasing its parameters.
- Change in skin color to bluish or grayish.
Bullous emphysema may not make itself felt for a long period of time.
Important! Symptomatic manifestations occur against the background of complications, among which spontaneous pneumothorax is most often diagnosed.
Spontaneous pneumothorax
Spontaneous bullous pneumothorax most often occurs as a complication of bullous emphysema. For spontaneous pneumothorax, the accumulation of air masses in the pleural cavity is standard. Most often, this complication is diagnosed in men under 40 years of age.
Pneumothorax.
Often, spontaneous pneumothorax affects the right lung. In a person who does not belong to the category of tobacco smokers, the course of the disease is mild and often goes away on its own. Surgical intervention and immediate hospitalization are required only by complicated pneumothorax, which can cause severe consequences.
With spontaneous pneumothorax, an increase in pulmonary pressure inside the bullae occurs and the wall of the cavity with air breaks through, which can cause lung collapse.
In most cases, such developments are facilitated by the following factors:
- excessively strained cough;
- changing the rhythm of life to an active one;
- lifting weights.
With spontaneous pneumothorax, both lungs are rarely affected; for the most part, it is detected only in 1 organ. When a complicated pneumothorax is detected in a person, serous exudate may be observed in the cavity of the pulmonary pleura.
Complicated spontaneous pneumothorax often causes the development of dangerous intrapleural bleeding.
Characteristic signs of a dangerous condition.
The pathological condition can make itself felt by the following number of symptomatic signs:
- In the area of the affected respiratory organ, the patient feels a stabbing pain, which often spreads to the neck, arm or peritoneum. The pain sometimes becomes more intense when coughing or when taking an extremely deep breath.
- The patient experiences shortness of breath, which gradually intensifies, as well as difficulty in breathing.
- There are attacks of coughing of a non-productive, that is, dry, nature. After coughing, the condition does not improve.
- When pneumothorax becomes severe, a person's condition rapidly deteriorates. Rupture of the pleura often causes loss of consciousness. Along with this, pallor of the skin and increased heart rate are determined.
Mild pneumothorax often passes without pronounced symptoms or with little severity. This condition can cause serious consequences because patients do not receive timely medical care. When the disease recurs, hemothorax, reactive pleurisy, or aspiration pneumonia may develop.
Causes and types of emphysema
Based on the cause and mechanism of development, primary and secondary pulmonary emphysema are distinguished. Primary pulmonary emphysema is an independent nosological form. It develops without previous bronchopulmonary pathology. In its development, great importance is attached to genetic factors (a1-antitrypsin deficiency). Secondary pulmonary emphysema occurs against the background of other respiratory diseases, primarily chronic obstructive bronchitis.
Based on the prevalence of the lesion, pulmonologists distinguish diffuse and local pulmonary emphysema. The diffuse form of the disease includes primary and secondary pulmonary emphysema, which developed against the background of chronic obstructive bronchitis. Local forms of pulmonary emphysema (bullous, irregular, peri-scar) develop for the following reasons:
- Cicatricial changes in the pleura and pulmonary parenchyma;
- Congenital changes in lung tissue;
- Local disorders of bronchial obstruction;
- Overextension of part of the lung due to shrinkage or surgical removal of other parts.
The following external factors play a great role in the development of pulmonary emphysema: air pollution, smoking, pulmonary infections. Pollutants (chemicals or compounds that are in the air in quantities that exceed background values) and occupational hazards, which lead to the formation of chronic processes in the respiratory tract and an imbalance in the proteolysis-antiproteolysis system, have a damaging effect on lung tissue. When air pollutants penetrate through inhalation, the membranes of the apical part of epithelial cells are damaged, inflammatory mediators, leukotrienes are released, and the balance in the oxidant-antioxidant system is disrupted. When the antioxidant system is depleted, inflammation of the mucous membrane of the respiratory tract continues. The development of emphysema is caused by exposure to particulate matter, suspended dust, and hydrocarbons. Fossil coal dust is especially dangerous.
The severity of the disease depends on the intensity and duration of smoking. The development of pulmonary emphysema is promoted by components of tobacco smoke - cadmium, sulfur, nitric oxide. They activate the work of alveolar macrophages and neutrophils. This helps to increase the level of metalloproteinases and neutrophil elastase. With prolonged smoking, the activity of proteolysis inhibitors decreases, and proteases, under conditions of the slightest deficiency of antienzyme function, cause significant damage to elastic fibers and destruction of the fine structures of the respiratory part of the lung. Tobacco smoke contains oxidants. They suppress the activity of anti-elastase inhibitors and inhibit recovery processes in the damaged elastic framework of the lung. Under the influence of smoking, the content of antioxidants in the blood plasma decreases, which together leads to the development of pulmonary emphysema.
One of the reasons for the development of pulmonary emphysema is a pulmonary infection. In the presence of infectious inflammation, the proteolytic activity of macrophages and neutrophils is stimulated. Bacteria and respiratory viruses can act as an additional source of proteolytic agents. Viruses themselves do not stimulate the production of neutrophils or macrophages, but due to their ability to suppress the immune system, they contribute to the exacerbation of inflammatory processes and the development of bacterial infection.
Symptoms
Patients with pulmonary emphysema are bothered by a feeling of lack of air, shortness of breath and an unproductive cough.
Patients with emphysema complain of shortness of breath and lack of air. In the early stages of the disease, shortness of breath occurs only after physical exertion, in the later stages it is felt constantly. The condition is accompanied by a cough with scanty sputum.
With primary emphysema, the breathing pattern changes. The inhalation becomes fast, the exhalation becomes longer. When exhaling, such patients open their mouths slightly and puff out their cheeks, as if puffing.
At moderate and severe stages, significant weight loss occurs due to high energy costs for the work of the respiratory muscles. The chest takes on a cylindrical (barrel) shape.
In severe respiratory failure, symptoms associated with oxygen starvation of tissues and organs are added:
- cyanosis of the skin and nails,
- swelling of the neck veins,
- puffiness of the face,
- irritability,
- insomnia.
With obvious damage to the lungs, the load on the diaphragm increases, so patients with emphysema are often forced to sleep in a sitting position.
Pathogenesis and classification of the disease
With emphysema, the air content in the lungs exceeds their normal volume, as a result of which the alveolar tissue stretches, loses its elasticity and ability to transport oxygen.
Because of this, respiratory failure occurs, the amount of oxygen in the blood is insufficient, and secondary disorders develop in the cardiovascular and nervous systems. The mechanism of disease development is as follows:
- Due to the disruption of air passage in the lungs, the alveoli increase in volume and their walls stretch.
- Behind them, the walls of blood vessels stretch, which provide pulmonary blood supply and gas exchange. Transport functions are disrupted, because the excess air occupying the alveoli is carbon dioxide (waste material).
- Following the damaged tissue, the function of healthy areas of the lungs is also impaired, because they experience pressure from pathologically expanded areas.
- Oxygen starvation is accompanied by an increase in intrapulmonary pressure, which also compresses the heart.
There are diffuse and bullous forms of pulmonary emphysema. In the diffuse form, the affected alveoli occupy the entire area of the lung, and in bullous emphysema, they are adjacent to healthy tissues.
The causes of pulmonary emphysema can be different - the main damaging factors are considered to be lung diseases (pneumonia, tuberculosis, bronchitis). Increasingly, experts are noticing an increase in the incidence of pulmonary emphysema among workers in hazardous production associated with mixtures and gases, as well as among heavy smokers.
Pulmonary emphysema
According to the nature of its course, acute and chronic pulmonary emphysema are divided. In addition, this disease can be primary or secondary in origin.
- Primary emphysema. It is called if it develops against the background of congenital characteristics of the body. This type of emphysema progresses rapidly and often ends in death in childhood.
- Secondary emphysema. It develops against the background of previous diseases and various harmful factors that act throughout life. Several other types of emphysema are also distinguished according to the anatomical features of the course.
Thus, pulmonary emphysema is a disease caused by a violation of the passage of air through the upper respiratory tract, and is accompanied by impaired breathing, circulation and secondary systemic disorders.
Centrilobular and paraseptal emphysema - what is it?
The pathology under consideration is divided into a primary (also called congenital) form, which acts as an independent disease, as well as a secondary form that develops with other pulmonary diseases.
If we base the classification of emphysema on the degree of prevalence of the process, then we can divide this painful condition into limited and diffuse types.
Depending on the extent to which the acinus is involved in the pathogenic process, several types of disease are distinguished.
If the alveoli are affected in the central region of the specified morpho-functional unit, then we can say with confidence that this is centrilobular emphysema (this disease occurs quite often). Emphysematous lesions of the distal acinar part are called perilobular. The panlobular variant of the pathology is characterized by damage to the entire acinus.
When bullae form, the form of the disease is called bullous. The development of an emphysematous process around foci of sarcoidosis, tuberculosis or pneumonia indicates an irregular (or peri-scar) variant of the disease in question.
There is also such a type of disease as paraseptal pulmonary emphysema, what it is can be described as follows: the focus of the pathology is adjacent to the septum between the alveoli, gradually destroying it.
Separately, it is worth mentioning congenital lobular emphysema, as well as McLeod syndrome, which is emphysematous pathological changes with a currently unclear etiology, and usually affects only one half of the respiratory organ.
How to cure emphysema
Treatment of emphysema is a complex task. Pulmonologists at the Yusupov Hospital provide complex therapy aimed at treating emphysema itself, chronic obstructive disease, and complications of the disease. Doctors carry out activities that are aimed at improving the quality of life of patients and slowing down the progression of the disease. Quitting smoking is of primary importance.
Methods of specific therapy for pulmonary emphysema itself, which would reduce the loss of lung elasticity, have not been fully developed. Doctors provide replacement therapy for a1-antitrypsin deficiency with the following drugs:
- Donor plasma;
- Native A1-AT from the serum of healthy donors;
- A1-AT, created by genetic engineering.
Patients are prescribed a1-AT aerosols. In order to increase the production of a1-AT, the synthetic anabolic steroid danazol is used. To correct the proteolysis-antiproteolysis system, antioxidants are prescribed (vitamin E, ascorbic acid, glutathione, b-carotene, trace elements zinc and selenium, sodium thiosulfate). Patients are prescribed drugs that affect the surfactant system of the lungs and restore the surface-active properties of the alveolar lining. For this purpose, the following substances are used for intratracheal administration:
- Eucalyptus oil;
- Menthol;
- Camphor;
- Fatty acid;
- Palmitic acid;
- Dipalmityl lecithin;
- Phospholipids.
Liposomes are injected intratracheally. Calcium antagonists have a positive effect on the surfactant system of the lungs when combined orally and inhaled (lazolvan, bromhexine, glycyram).
In most cases of bullous emphysema, surgical interventions are performed. The most promising are video-assisted thoracoscopic operations. Recently, surgeons have used surgical reduction of lung volume and lung transplantation as surgical methods for treating pulmonary emphysema.
For the treatment of COPD, which occurs in parallel with pulmonary emphysema, bronchodilating and mucoregulatory drugs, immunocorrective therapy, antibacterial agents, and glucocorticoids are used. When treating pulmonary emphysema, doctors at the Yusupov Hospital pay great attention to the correction of respiratory failure, which is achieved through oxygen therapy and respiratory muscle training. Preference is given to long-term (18 hours a day), low-flow (2–5 liters per minute) oxygen therapy. The presence of expert-class breathing equipment allows doctors in the intensive care unit to use helium-oxygen mixtures and non-invasive ventilation with two levels of positive pressure in case of severe respiratory failure.
Specialists at the rehabilitation clinic teach patients suffering from pulmonary emphysema special breathing exercises, including those aimed at passivizing exhalation, and use devices that create positive pressure at the end of exhalation. According to indications, transcutaneous electrical stimulation of the diaphragm is used.
In order to undergo an examination and a course of adequate treatment for pulmonary emphysema, make an appointment with a pulmonologist online or by calling. Contact center specialists will offer a consultation time convenient for you with leading specialists in the field of respiratory diseases. At the rehabilitation clinic, specialists will conduct a course of rehabilitation therapy aimed at strengthening the respiratory muscles.
Author
Sergey Borisovich Shornikov
Cardiologist
Folk recipes
The use of folk remedies is possible, but as an addition to the main therapy, carried out under the supervision of a doctor and herbalist. Dandelion, juniper, sage, marshmallow root, eucalyptus, spruce, pine, thyme, peppermint, lemon balm, anise, buckwheat, coltsfoot, plantain, sweet clover, cumin have expectorant and bronchodilator effects.
- Mix dried and crushed mint, sage and thyme in equal proportions. 1 tbsp. spoon. Pour the mixture into a thermos and pour 1 glass of boiling water overnight. Drink 70 ml after breakfast, lunch and dinner.
- 1 tbsp. Pour a spoonful of dry coltsfoot leaves into 2 cups of boiling water and leave for an hour. Drink 1 tbsp. spoon 4-6 times a day.
- Mix 1 part each of marshmallow and licorice roots, pine buds, sage leaves, and anise fruits. 1 tbsp. Pour 1 cup of boiling water over a spoonful of the mixture, leave for several hours and strain. Take a quarter glass with honey 3 times a day.
- 1 hour pour 500 ml of boiling water over a spoonful of dried and crushed wild rosemary and leave for 1 hour. Take 150 ml of warm infusion twice a day. Add 1 tbsp to a glass of warmed fat milk. spoon of carrot juice, drink on an empty stomach for three weeks.
- Pour 0.5 liters of boiling water over buckwheat flowers and leave for 1 hour. Drink 0.5 cups 3-4 times a day with honey.
- Chopped juniper, dandelion root, birch leaves are mixed in a ratio of 1:1:2. 1 tbsp. Pour 1 cup of boiling water over a spoonful of the mixture and leave for 1 hour. Drink 70 ml after meals 3 times a day.
Inhalations with a decoction of potato root vegetables “in their jacket” have an expectorant and relaxing effect on the bronchial muscles. The temperature of the liquid should not exceed 85°C to prevent burns to the mucous membrane. To carry out the procedure, take several potatoes, wash them, put them in a pan and cook until tender. Then remove the pan from the heat, place it on a stool, cover with a towel and breathe in the steam for 10 to 15 minutes.
Saturation of the air with medicinal components of essential oils of marjoram, dill, eucalyptus, oregano, wormwood, thyme, sage, chamomile, cypress, cedar improves the condition of patients suffering from emphysema.
Use a special device for fine spraying (diffuser) or a regular aroma diffuser (5-8 drops of ether per 15 square meters of room).
The same oils are used to rub the feet, palms, and chest. To do this, in 1 tbsp. a spoonful of jojoba oil, vegetable or olive, add 2-3 drops of ether or a mixture of several oils. Author: Victor Punga, professor, doctor of medical sciences
Causes
Emphysema can be either congenital (associated with genetic mutations) or acquired. The main prerequisites are:
- Congenital anomalies of lung development;
- Chronical bronchitis;
- tuberculosis;
- bronchial asthma;
- acute pneumonia;
- damage to lung tissue due to occupational hazards;
- long-term smoking;
- significant air pollution;
- removal of one of the lung lobes.
Doctors combine the diseases that cause emphysema into one group called COPD (chronic obstructive pulmonary disease ) .