Parkinson's disease is a chronic, steadily progressing brain disease in which neurodegenerative changes are observed in the structures of the substantia nigra.
Parkinson's disease is diagnosed in 5% of people over 60 years of age
This pathology is one of the leading in the group of neurodegenerative diseases, manifested by the death of nerve cells in the brain, disruption of the production of neurotransmitters and instability of the interaction of various structural parts of the central nervous system.
The first mention of the disease as an independent nosology is presented in the essay “An Essay on the Shaking Palsy”, written by James Parkinson (1817), although in ancient India more than 4500 years ago a disease was described that has manifestations similar to Parkinson’s disease - kampa vata.
The disease occurs everywhere, on all continents, in all ethnic groups, with an average prevalence of 60–160 cases per 100,000 population. The average incidence is 20 episodes per 100,000 population per year, and it increases significantly with age: for example, in 70-year-olds the rate is 55 cases per 100,000, and in 85-year-olds it is already 220 cases per 100,000 population per year. In recent decades, there has been a trend toward rejuvenation of the pathology (onset before the age of 40).
According to statistics, Parkinson's disease is diagnosed in 1% of the population under 60 years of age and in 5% of older people. The incidence among men is slightly higher.
According to the World Health Organization, at the end of the twentieth century there were more than 4,000,000 people in the world diagnosed with Parkinson's disease.
Synonyms: idiopathic parkinsonism, shaking palsy.
Parkinson's disease - what is it?
The development of this disease is most often observed in older people. If the disease has an early onset, disability may soon occur. Despite the fact that Parkinson's disease was described more than 100 years ago, the exact mechanism of development of this pathological condition has not yet been established. The problem lies in the gradual death of cells in the brain and spinal cord.
Damaged neurons cannot perform their function. In addition, there is a destruction of connections between nerve cells. This leads to the fact that the brain ceases to control the functioning of all body systems, but the functioning of the musculoskeletal system is especially affected.
Given that nerve cells do not regenerate, there is no question of whether Parkinson's disease is curable.
The functioning of the human body is regulated by many interconnected reflexes that determine the reaction to stimuli. This complex system has the functions of irritation and inhibition. If the central nervous system did not have well-functioning mechanisms for recognizing external and internal stimuli, the human body would be in constant tension.
With this disease, the inhibition function is weakened, so the patient’s body has a heightened reaction to any irritants. An involuntary response may be the appearance of grimaces, twitching, tremors, etc.
With this disease, there is a decrease in dopamine production. This hormone performs the function of transmitting impulses to one or another part of the brain, which causes the appearance of one or another reaction to the stimulus. Thus, decreased dopamine production negatively affects the ability to carry out planned actions.
Characteristic mental disorders and movement disorders increase as degenerative processes in the brain progress. Viral and bacterial infections, the influence of other unfavorable factors can contribute to the acceleration of the development of symptoms.
In reality, the nature of the course of the pathology and the rate of increase in its symptoms are almost impossible to predict. For some patients, disability occurs several years after the onset of symptoms. In others, motor functions and normal neurological status may persist for decades.
Symptoms of the disease
The course of the disease is characterized by a gradual increase in symptoms. The development of the clinical picture may take up to a year. The first signs of the disease in young people rarely occur. However, several years before the development of the pathology itself, phenomena appear that warn a person about a possible illness.
Early symptoms
Symptoms in the early stages of Parkinson's disease may include:
- impaired sense of smell;
- depression;
- anxiety states;
- chronic constipation;
- restless sleep, movements of limbs, screaming;
- malfunctions of the genitourinary system;
- general apathy;
- low performance.
Such disorders are associated with the fact that the pathological process has already started, but before the neurons responsible for motor activity begin to die, the extranigral parts of the brain will suffer.
Important! Many patients, shortly before the development of Parkinson's disease, experienced changes in their handwriting, which became smaller and more illegible.
Some patients develop Parkinson's mask syndrome. There is a feeling that the face has become less mobile. And indeed it is. A person blinks less, speaks more slowly, and emotions are less expressed. His speech becomes unintelligible at times, making it difficult for others to understand him. These symptoms intensify during moments of anxiety or stress.
Making an accurate diagnosis at an early stage of the disease can be difficult, since many people consider all these phenomena to be normal signs of aging, unaware of the development of pathology.
Symptoms of Parkinsonism
Symptoms of Parkinson's disease are mainly expressed in movement disorders. Let's consider the most pronounced ones.
In a person suffering from Parkinsonism, the muscles are in constant tension. At the last stage, muscle rigidity is especially pronounced. A “supplicant pose” develops (can be seen in the photo), that is, the back is tilted forward, the arms and legs are also bent at the joints. Due to constant being in such an uncomfortable position, muscle and joint pain appears.
It is impossible not to notice the trembling of the limbs, especially the tremor of the hands, which is present both at rest and when trying to make some kind of movement. Hand actions seem rough.
As Parkinson's disease progresses, twitching of the eyelids, jaw, and tongue occurs. At the same time, normal body movements become slower. Facial expressions and gestures worsen, the amplitude of any actions decreases. This phenomenon is called oligobradykinesia.
Postural instability is expressed in changes in the patient's posture and gait. It is increasingly difficult for him to control the center of gravity, which is why the patient often falls. Before changing the direction of movement, a person marks time, and the gait as a whole becomes uncertain, shuffling and mincing.
Due to impaired motor function, the process of swallowing saliva is also disrupted. It is secreted profusely, resulting in drooling and slurred speech.
Symptoms of dementia are observed only in the final stages. In patients with Parkinsonism, the ability to remember information and fully learn worsens. Logical thinking and the ability to concentrate are reduced. In some patients, dementia does not occur at all, but if the symptom does appear, it will steadily progress.
Note! If parkinsonism develops in a man, one of the symptoms is impotence.
People with Parkinson's disease constantly suffer from depression. A chronic form develops and the condition becomes a constant companion of the sick person.
Symptoms and signs
Given that this disease is genetic in nature, it is almost impossible to predict when the first symptoms will appear. At the same time, it is believed that the development of pathology can be stopped if detected at the 1st stage of development.
Clinical signs of the disease and the degree of their severity largely depend on the form of the disease.
The most common signs of this pathology in women and men include:
- tremor;
- slowing down movements;
- postural disturbances;
- muscle stiffness;
- sharp decreases in blood pressure;
- deterioration of balance, unsteadiness of gait.
The most distinct manifestation of Parkinson's pathology is tremor. Patients experience tremors of the upper or lower extremity. In the future, the tremor can spread to the facial muscles and tongue. This manifestation in the early stages of the disease is especially well detected immediately after waking up and after prolonged physical activity. A nervous tic causes not only physical but also emotional discomfort.
Rigidity or muscle stiffness is accompanied by intense pain. The disease already in the early stages of development leads to a decrease in the swing movements produced by the hand. In addition to pain, the patient has constant muscle fatigue.
Often, already in the early stages of the disease, pronounced signs of imbalance appear.
Difficulties arise during sharp turns. The gait becomes shuffling. At the same time, the person begins to take small steps, which increases the risk of falls. Often there are feelings of weakness and spasms of the throat muscles. This leads to problems with swallowing.
An early manifestation of pathology is postural disturbances. If the patient extends his arms forward, asymmetrical position may be noted. Other manifestations are also possible.
Signs of Parkinson's disease
The most obvious sign of Parkinson's disease is tremors. This disorder occurs in 100% of patients. Patients present with rhythmic twitching of the limbs, muscles of the lower jaw, face and tongue. There are characteristic movements of the fingers, reminiscent of an attempt to count out money. Trembling occurs spontaneously, and the patient cannot control it.
Often the development of the disease is accompanied by the appearance of a number of additional symptomatic manifestations caused by damage to neurons.
Common signs of pathology include:
- increased salivation;
- depression;
- disturbances in the process of urination and defecation;
- sleep disorders;
- restless legs syndrome;
- constipation;
- change in voice timbre;
- “freezing” when performing actions;
- muscle cramps;
- joint pain;
- oily skin;
- dandruff;
- increased irritability.
Approximately 20% of people suffering from this disease develop psychosis. This condition is accompanied by the appearance of hallucinations, unmotivated feelings of confusion, fear and disorientation.
As the disease progresses, the appearance of dementia—acquired senile dementia—is noted. This condition is accompanied by a decrease in intelligence, impaired coordination in space and loss of self-care skills.
Prevention
A specific disease prevention program has not been developed. Considering the serious consequences of Parkinson's disease, it is important to consult a doctor at the first signs of pathology for early diagnosis and prescribing the correct treatment.
Parkinson's disease occurs against the background of neurodegenerative processes and is manifested by tremors at rest, postural instability, muscle rigidity, slowing and limitation of the range of purposeful movements while maintaining asymmetry in the manifestation of symptoms. Early diagnosis and correct therapy are favorable prognostic factors.
Causes
It is believed that the main cause of Parkinson's syndrome lies in a genetic disorder. Even if a person has a hereditary predisposition to the development of pathology, it is not necessary that pronounced manifestations of the disease will appear in the future.
A number of factors can be identified that can contribute to the activation of the pathological process. These include:
- individual characteristics of the aging body;
- living in environmentally unfavorable areas;
- lack of vitamins and minerals;
- poor nutrition;
- presence of bad habits;
- brain injuries;
- vascular pathologies;
- increased mental activity throughout life;
- taking certain medications;
- infectious diseases complicated by inflammatory brain damage;
- poisoning with toxic substances.
Tumors of a benign and malignant nature that form in the tissues of the brain can provoke the development of pathology.
Causes
Scientists have not yet been able to identify the exact causes of Parkinson's disease, but there is a certain group of factors that can trigger the development of this disease.
According to statistics, Parkinson's disease is diagnosed in 1% of the population under 60 years of age and in 5% of older people. The incidence among men is slightly higher.
The causes of Parkinson's disease can be identified as follows:
- aging of the body, in which the number of neurons naturally decreases, which leads to a decrease in the production of dopamine;
- hereditary predisposition;
- permanent residence near highways, industrial enterprises or railways;
- lack of vitamin D, which is formed when exposed to ultraviolet rays in the body and protects brain cellular formations from the destructive effects of free radicals and various toxins;
- poisoning with certain chemical compounds;
- the appearance of defective mitochondria due to mutation, which often leads to neuronal degeneration;
- neuroinfections (tick-borne encephalitis);
- tumor processes occurring in the brain or its trauma.
Parkinson's disease can also develop, according to some statements, against the background of drug intoxication associated with long-term use of phenothiazine medications by patients, as well as with certain narcotic drugs.
Scientists come to the conclusion that most often a combination of several of the listed reasons leads to the development of the disease.
The causes of the disease also depend on the type:
- Primary parkinsonism is caused by a genetic predisposition in 80% of cases.
- Secondary parkinsonism occurs against the background of various pathologies and existing diseases.
Risk groups include people 60-65 years old, most often the male population. It also occurs in young people. In this case, it proceeds more slowly than in people of the older age group.
It is worth noting that the signs of Parkinson’s disease in women and men do not have obvious differences, since cell damage occurs regardless of a person’s gender.
Petitioner pose and puppet walk
Characteristic manifestations of the development of Parkinson's syndrome include 4 types of motor symptoms, combined with disturbances in mental activity and functioning of the autonomic nervous system. Due to the increase in these signs of pathology, patients experience such characteristic symptoms of pathology as the “petitioner” pose and “doll gait”.
Increased muscle tone and movement disorders
Due to progressive hypokinesia, which leads to the appearance of a characteristic “petitioner” pose, people suffering from Parkinson’s syndrome can be recognized even from afar. This is the most common and severe manifestation of the disease.
Due to increased muscle tone, the front part of the patient’s body moves forward, but at the same time the limbs are bent at the elbows and knees. The patient experiences stiffness of movement. A person can freeze in one position for a long time. The patient cannot stop independently after starting to move.
Increased muscle tone leads to the fact that if you raise the head of a person who is in a supine position, it will remain in that position for some time. When moving, people suffering from Parkinson's syndrome press their arms to their body. Patients move in small steps, shuffling along the floor. This manner of movement is called the “doll gait.” The presence of the disease is also indicated by poor facial expressions, rare blinking and a frozen gaze.
Symptoms
Parkinson's disease is characterized by movement disorders (hypokinesia, muscle rigidity, tremor, postural disorders) and concomitant dysfunctions of the autonomic and cognitive spheres.
Hypokinesia implies difficulty initiating and slowness of movements, while the amplitude and speed of repeated movements decrease while muscle strength is preserved. The main manifestations of hypokinesia:
- poor facial expressions, rare blinking;
- slow, monotonous and quiet speech, fading towards the end of the phrase;
- difficulty swallowing and resulting drooling;
- respiratory disorders;
- loss of friendly movements (hand movements when walking, wrinkling of the forehead when looking up, etc.);
- shuffling gait in small steps with feet parallel to each other (“doll gait”);
- spontaneous freezing in a static position;
- small “shaky” handwriting with letters decreasing towards the end of the line;
- difficulty changing body position;
- slowness in daily activities.
Manifestations of Parkinson's disease
Rigidity refers to a feeling of stiffness or tightness. The muscle tone in patients is plastic, “sticky”: after flexion or extension of the limb during the examination, it freezes in this position (“wax doll symptom”). The tone in the limbs prevails over the tone of the axial muscles, which leads to the appearance of a characteristic “petitioner pose” (“mannequin pose”) - a hunched, bent forward back, arms pressed to the body, half-bent at the elbow joints, bowed head, legs also half-bent at the knees and hips joints.
When studying the muscle tone of the limbs, flexion and extension do not occur smoothly, but stepwise, intermittently, in the form of uniform pushes.
The most characteristic symptom is tremor, that is, trembling, however, in approximately 15% of patients this symptom is absent throughout the entire course of the disease. The specificity of tremor in Parkinson's disease is its maximum severity at rest (including during sleep), when stretching the arms or during movement, the tremor significantly decreases or completely disappears, and intensifies with excitement, emotional and physical stress.
Hand tremors are the most characteristic sign of Parkinson's disease
Trembling begins in the early stages of the disease from the fingertips of one hand, subsequently spreading to the entire limb, and then to other parts of the body (sometimes there is a trembling of the tongue, lower jaw, eyelids, head like “yes-yes” or “no-no” , stop).
Characterized by multidirectional rhythmic small movements in the 1st, 2nd and 3rd fingers, similar to counting coins or rolling pills.
Postural instability is the loss of the ability to maintain body balance when walking or changing body position, turning in place, getting out of a chair or bed, which provokes the patient to frequent falls (more often forward, less often backward). This phenomenon usually appears in the later stages of the disease.
According to the World Health Organization, at the end of the twentieth century there were more than 4,000,000 people in the world diagnosed with Parkinson's disease.
A patient with postural instability has difficulty both initiating movement and completing it. For example, having started walking, the patient cannot stop on his own; the body, as it were, continues to move forward by inertia, ahead of the limbs, which leads to a shift in the center of gravity and a fall.
Autonomic disorders most characteristic of Parkinson's disease:
- orthostatic hypotension (sharp decrease in blood pressure when body position changes);
- urinary and fecal incontinence;
- erectile disfunction;
- lacrimation;
- thermoregulation disorder;
- impaired sweating (hypo- or hyperhidrosis);
- sensory disorders in the form of tingling sensations, numbness, burning, itching (50% of patients);
- impaired sense of smell (90% of patients).
Cognitive disorders of mild and moderate severity in the first 5 years are observed in the majority of patients. Signs of dementia appear after 5 or more years, extremely rarely at the onset of the disease.
In the advanced stage, mental disorders are possible (depression and anxiety, the development of obsessive-compulsive syndrome, delusions, hallucinations, impaired identification, delirium).
Consequences for humans
The development of this pathology is accompanied by an increase in physical and mental disorders. Over time, it becomes difficult for the patient to perform the simplest everyday tasks. As the disease progresses, patients find it difficult to sit down, wash dishes, brush their teeth, and dress themselves. Life expectancy is decreasing.
If the manifestations of pathology begin to increase at a young age, the consequences are even more unfavorable. The patient quickly loses his ability to work and becomes completely dependent on relatives. As the disease progresses, mental disorders increase. The patient loses the ability to critically evaluate his appearance and actions.
As the disease progresses, pronounced intellectual impairments appear. Both short-term and long-term memory deteriorate. A person loses previously acquired knowledge and skills. In the future, the development of paralysis and complete loss of the ability to verbal communication is possible.
If signs of pathology appear at an early age, the patient is doomed to premature death due to a critical disruption of the functioning of brain structures.
Autonomic disorders and mental disorders
The development of the disease can be easily determined by the increasing disorders of the autonomic nervous system in a person. Due to metabolic disorders, the patient rapidly gains weight or loses weight to the point of exhaustion. Other autonomic disorders may be present.
As brain tissue is destroyed, the patient's psyche suffers greatly. Signs of mental disorders may vary depending on the extent of neuronal damage. The patient becomes uninitiated and passive, and the desire to communicate with people is sharply limited. Switching from one type of activity to another is difficult for the patient.
Video: Early signs of Parkinson's disease, Live Healthy program
The early manifestations of Parkinson’s pathology are well described in Elena Malysheva’s “Live Healthy” program. Experts are analyzing the relationship between disruption of the neural network in the human brain and symptoms characteristic of this pathological condition.
Forecast
The prognosis for Parkinson's disease is conditionally unfavorable, which is associated with its steady progression. In the absence of treatment, patients lose the ability to self-care for approximately 8 years; after 10 years, complete immobility often occurs. Patients receiving pharmacotherapy become dependent on their caregivers after an average of 15 years.
Life expectancy with Parkinson's disease is reduced; as symptoms progress, the quality of life irreversibly deteriorates, and the ability to work is lost.
Video from YouTube on the topic of the article:
Forms and stages of Parkinson's
There are several types of pathology depending on the predominance of certain symptoms. There are the following forms of Parkinson's disease:
- rigid-bradykinetic;
- trembling-rigid;
- trembling.
Each option has its own flow characteristics.
In the rigid-bradykinetic form, there is a pronounced increase in muscle tone, leading to impaired motor activity. Patients in this case quickly lose the ability to move normally.
The trembling-rigid form is accompanied by the appearance of stiffness in movements and tremors of varying degrees of intensity.
The mildest form is considered to be the trembling form , in which muscle rigidity is weakly expressed, so motor activity is almost not affected. A characteristic manifestation of this variant of the course of the disease is the presence of tremor.
The development of the disease is accompanied by a steady increase in manifestations.
As this pathology progresses, it goes through 5 main stages of development.
- At stage 1 of the disease, characteristic symptoms are observed on one limb. In this case, it is possible for the disorders to transfer to the body.
- At stage 2 of the pathological condition, signs of postural disturbances appear on both sides.
- At stage 3, there is a characteristic worsening of postural instability. Patients can already overcome the inertia of movement with great difficulty. The patient is still able to care for himself.
- At stage 4 of the disease, the patient’s motor functions and psyche are so impaired that he cannot move independently and needs constant assistance.
- The last stage of the pathology is characterized by complete immobilization of the patient. There is not only a complete loss of motor ability, but also critical mental disorders.
Stages of the disease
The generally accepted gradation of stages of the disease, reflecting the degree of severity, is as follows:
- stage 0 – absence of motor disorders;
- stage 1 – unilateral nature of the manifestations of the disease;
- stage 2 – bilateral manifestations of the disease, the ability to maintain balance is not affected;
- stage 3 – moderately severe postural instability, the patient is able to move independently;
- stage 4 – severe loss of motor activity, the ability to move is preserved;
- stage 5 - the patient is bedridden or wheelchair-bound, and movement without assistance is impossible.
Stages of Parkinson's disease according to the Zen and Yahr scale
The modified Hoehn and Yarh scale (Hoehn and Yarh, 1967) suggests the following division into stages:
- stage 0.0 – no signs of parkinsonism;
- stage 1.0 – unilateral manifestations;
- stage 1.5 – unilateral manifestations involving the axial muscles (neck muscles and muscles located along the spine);
- stage 2.0 – bilateral manifestations without signs of imbalance;
- stage 2.5 – mild bilateral manifestations, the patient is able to overcome the caused retropulsion (the patient accelerates backward when pushed from the front);
- stage 3.0 – moderate or moderate bilateral manifestations, slight postural instability, the patient does not need outside assistance;
- stage 4.0 – severe immobility, the patient’s ability to walk or stand without support is preserved;
- stage 5.0 – the patient is confined to a chair or bed without assistance.
In the absence of treatment, patients lose the ability to self-care for approximately 8 years; after 10 years, complete immobility often occurs.
Diagnostics
Elderly people need to undergo regular examinations by a neurologist. This will allow pathology to be recognized at an early stage. When signs of the disease appear, a more thorough examination is required using magnetic resonance imaging and other research methods. The entire diagnostic process can be divided into several stages.
Stage 1
First, an external examination of the patient is performed to identify symptoms characteristic of Parkinson's syndrome. Anamnesis is collected to assess the patient's complaints. If possible, the presence in the family history of cases of the development of this pathological condition is clarified.
Stage 2
At this stage of diagnosis, the neurologist needs to exclude other diseases that may have similar symptoms, including strokes, traumatic brain injuries, poisoning, brain tumors, etc.
Stage 3 - confirmation of the presence of the disease
Stage 4 of diagnosis involves identifying signs such as:
- the duration of the disease is at least 10 years;
- gradual deterioration of the condition;
- asymmetry of symptoms.
To make an accurate diagnosis, the results obtained from studies such as CT, EEG, MRI and rheoencephalography are taken into account.
Description of parkinsonism
Parkinsonism is a term used to describe a syndrome of movement disorders resulting from damage to neurons (nerve cells) in the basal ganglia (nuclei) of the brain. The cause of such damage can be various external and internal factors.
The basal ganglia regulate motor and autonomic functions
Most often, the syndrome develops in older people (over 60 years old), and its connection with heredity and natural aging processes is noted. In this case, we are talking about Parkinson's disease, which accounts for about 70% of all clinical episodes of parkinsonism. In other cases (only about 30%), a diagnosis of secondary parkinsonism is made. In this case, postural disorders (disorders of gait, posture, statics) are associated with the damaging effects on the central nervous system of various external factors (toxins, drugs, certain medications, traumatic brain injuries) or are a consequence of some primary pathologies (infectious diseases, atherosclerosis, etc.). d.).
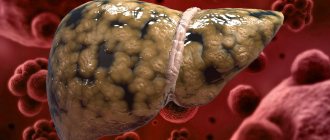
Parkinsonism occurs due to damage and death of neurons in certain areas of the brain.
Motor disorders in parkinsonism are associated with dysfunction of certain parts of the midbrain and impaired control of the basal ganglia over the transmission of impulses from the spinal cord to the muscles, which leads to increased tone of the latter. The syndrome, having a neurochemical nature, is characterized by a disorder of cerebral catecholamine metabolism. Catecholamines are substances that act as “mediators” in intercellular processes occurring in the brain.
Postural disturbances (lack of coordinated movements, inability to maintain the body in a certain position) in parkinsonism are also associated with insufficient production of the neurotransmitter dopamine in the damaged basal ganglia and substantia nigra (the substance of the midbrain). This neurotransmitter is designed to inhibit the excess of muscle-stimulating nerve impulses emanating from the cerebral cortex, thereby achieving precision of movements and normal tone of muscle tissue. With a lack of dopamine, nerve impulses are sent directly to the muscles without delay, which leads to their excessive tension and contraction. This explains the main symptoms of the pathology - trembling of the arms and legs at rest (tremor), excessive muscle tension (rigidity), and disorder of voluntary movements.
Damage to the substantia nigra (a substance located in the midbrain) leads to dopamine deficiency, which leads to the development of parkinsonism syndrome
Despite similar manifestations, parkinsonism has certain differences from the disease of the same name. The difference between the syndrome and Parkinson's disease is as follows:
- the syndrome does not develop independently and is directly associated with a brain-damaging agent;
- it begins acutely under the influence of an etiological factor (root cause);
- Initially, with parkinsonism, there is a symmetry of symptoms, while there are other manifestations of damage to the nervous system;
- the syndrome is more malignant in nature and can therefore lead to disability for several years;
- traditional antiparkinsonian drugs (for example, Levodopa) do not have a pronounced therapeutic effect in the syndrome;
- in certain cases, stopping the damaging factor leads to a complete regression of the manifestations of the syndrome.
Degenerative changes in the central nervous system, manifested by parkinsonism, can be observed at any age. And although classically the syndrome is considered in neurology as characteristic primarily of adults, pediatric neurologists have to deal with varieties of parkinsonism in children and adolescents. Most often, the disorder develops as a complication of whooping cough, viral encephalitis, other infections, and also as a result of hereditary disorders.
Treatment
Despite the fact that the disease cannot be cured, with an individual approach it is possible to slow down its development. The patient can remain active longer and lead a full life.
The latest treatment methods make it possible to delay the onset of severe complications. Therapy should be aimed at maintaining the patient’s normal motor activity and developing a special physical therapy program. The doctor selects medications for the patient individually.
Drug treatment
Medicines are selected taking into account the degree of neglect of the pathological process. Medications that stimulate dopamine production may be prescribed first. These drugs include Amantadine. In the future, drugs belonging to the category of dopamine receptor antagonists can be introduced into the treatment regimen.
Such drugs include:
- Pramipexole;
- Mirapex.
In the later stages, in addition to previously used drugs, Levodopa is prescribed. Patients with Parkinson's syndrome are prescribed symptomatic treatment. In the presence of severe psychoses, neuroleptics and psychoanaleptics are selected.
Drugs of this type include:
- Exelon;
- Seroquel;
- Reminyl;
- Azaleptin;
- Clozapine;
- Leponek.
Drugs are selected to relieve autonomic disorders. Depending on the symptoms, patients are often prescribed antispasmodics, gastrointestinal motility stimulants and laxatives.
For severe pain, sleep disturbances, depression and increased anxiety, antidepressants and intoxicants are prescribed.
Such drugs include:
- Cipramil;
- Paxil;
- Amitriptyline;
- Ixel;
- Zolpidem.
Drugs are often prescribed to improve memory and increase concentration. Medication dosages should be adjusted periodically.
Exercise therapy
People suffering from this pathological condition need to do special physical exercises daily to maintain muscle tone and normal motor activity. A specialist should select a complex of exercise therapy. All movements must be learned under the supervision of an instructor. Therapeutic exercise allows you to remove existing symptoms and slow down the progression of the disease.
Surgical intervention
If drug therapy is ineffective, surgery may be indicated. There are several surgical treatment options. Pallidotomy is often performed. Such an intervention allows you to eliminate hyperkinesia.
In addition, the method of neurostimulation is widely used. This intervention involves the installation of a special device with electrodes that are connected to the desired areas of the brain. The effect of electric current allows eliminating existing motor disorders in patients.
Treatment of pathology
Treatment of Parkinson's disease is also carried out using a complex of medications. It is important to understand that complete rehabilitation is impossible.
Note! It is better to start using medications for treatment as late as possible, since most of them are addictive, you have to increase the dosage, and side effects increase.
In the early stages of the pathology, feasible physical activity, laughter therapy, and therapeutic prophylaxis are recommended. Next, symptomatic treatment is used:
- neuroleptics (for mental disorders);
- antispasmodics;
- antidepressants;
- sedatives;
- drugs that improve blood flow to the brain.
Important! Levodopa drugs should be prescribed as late as possible and the dosage should be increased as slowly as possible.
Surgeries for illness are rarely performed. Surgery is indicated only if drug therapy is ineffective. Neurostimulation is effective, in which selective electric current is applied to certain areas of the brain.
The prognosis for early treatment is favorable and people live to a ripe old age. In 25% of patients, the pathology is severe and ends in death.
Treatment of the disease with folk remedies can only be carried out as prescribed by a doctor and in combination with the main therapy. Most often, such recipes are used for the symptomatic treatment of sleep disorders and normalization of the psycho-emotional state.
Ineffective treatments for Parkinson's disease
Antioxidant therapies have been attempted in the past , but studies have shown them to be ineffective.
The same can be said about the introduction of stem cells into the body, when the effect was short-lived and a massive deterioration in the condition occurred. However, genetically engineered stem cells have not yet completely discredited themselves, but a lot of effort is still required to bring this method to a reliable and effective level.
Currently existing stem cell techniques can be used
How does the syndrome manifest?
The main clinical manifestations include a triad of symptoms:
- Bradykinesia. It represents a decrease in the number and speed of voluntary movements, a person becomes slow, gestures lose expressiveness, and over time disappear completely, facial expressions become impoverished.
- Muscle rigidity (hypertonicity) - is expressed in persistent tension in the motor muscles. At the beginning of the disease, tone can be observed during passive (performed by a neurologist) movements of the arms and legs, then rigidity can be noted by the fact that the limbs are constantly in a semi-bent state.
- Trembling hyperkinesis, or postural tremor, is manifested by trembling of the hands and head when the patient is at rest. The tremor goes away as soon as the person begins voluntary movements.
Damage to certain parts of the midbrain leads to the appearance of certain symptoms of parkinsonism.
Over time, postural disturbances can lead to immobility of the patient, the person loses self-care skills, significant personality changes occur, and there is a decrease in memory and intellectual abilities.
Depending on the form of the pathology, some of the three main symptoms may be more pronounced than others. Thus, the akinetic form is manifested by a decrease in general motor activity and gestures. Facial expressions become difficult, the patient has a frozen, mask-like expression on his face. At the same time, he rarely blinks (Marie’s symptom), his speech becomes muffled, inexpressive, and monotonous. When walking, there are no accompanying movements of the arms, the step becomes small (“mincing gait”), and the patient often cannot stop immediately.
In the akinetic-rigid form, along with the above-described signs, muscle hypertonicity is observed, which can be general or selective. Rigidity causes the patient to remain in a specific position (the supplicant position): the body is tilted forward, the head is to the chest, the arms are pressed to the sides and bent at the elbows and hands.
The supplicant pose is a characteristic sign of the akinetic-rigid form of parkinsonism
The rigid-tremor form, in addition to muscle tension, is manifested by fine-rhythmic tremor at rest, noticeable especially in the upper extremities. Sometimes the tremor spreads to some of the neck and head muscles.
The trembling form is always characterized by pronounced tremor, while bradykinesia (slowing of voluntary movements) and hypertonicity are less pronounced and may be completely absent.
The syndrome is characterized by rapid progression of symptoms, while the features of the clinical picture depend on the etiological forms of parkinsonism:
- post-infectious parkinsonism is characterized by significant rigidity, vegetative manifestations (tendency to constipation, increased greasiness of the skin and hair, sweating), sleep disorders, decreased intellectual abilities, oculogyric crises (episodic strabismus). In this case, tremor is often absent;
- in the posthypoxic form of the syndrome, trembling, on the contrary, is clearly expressed;
- Vascular parkinsonism is manifested by severe motor and cognitive disorders, minor tremor. In this case, postural disturbances predominate in the lower part of the body;
- hydrocephalic parkinsonism is characterized by the rapid development of dementia (dementia), ataxia (disorder of coordination of movements), urinary incontinence, and can be combined with apraxia (inability to perform consistent actions), sensitivity disorders (the sensation of “foreign” limbs);
- with the syndrome that has arisen against the background of dementia with Lewy bodies, mental disorders occur (hallucinations, psychoses);
- drug-induced parkinsonism develops acutely, with pronounced hypertonicity, akinesia (impossibility of voluntary movements), hyperkinesis (involuntary contractions of different muscle groups).
Video - manifestations of parkinsonism
Is Parkinson's disease inherited?
Scientists studied identical twins who carry exactly the same genotype, but only one of the twins gets sick, while the other is spared the disease.
A genetic connection can be traced, but cases of inheritance of Parkinson's disease from parents to children do not exceed 10%, and even this figure, as practice shows, is clearly overestimated.
Some symptoms of Parkinson's disease.
The course and prognosis of Parkinson's disease and parkinsonism.
The disease is steadily progressing. The exception is some forms caused by drug intoxication (if the drugs are discontinued, the condition may improve). It is generally accepted that treatment at the initial stage can reduce the severity of symptoms and slow down the progression of the disease. In later stages, treatment measures are less effective. The disease leads to disability for several years. Even treatment with levodopa currently slows the progression for a short period of time. This confirms the position that the basis of the disease is not only a primary biochemical defect, but also an as yet unstudied neuropathological process.
Surgical methods for treating parkinsonism
The earliest are the so-called destructive operations: destruction of certain nuclei on one side of the brain led to the disappearance of dyskinesia and tremor on the opposite side, attempts at bilateral destruction led to extremely unpleasant consequences - impaired swallowing, loss of voice and often severe depression; subsequently, the techniques of destructive operations were improved , a non-invasive method of operations has appeared - the gamma knife, based on the radiological focus of the target point in the brain.
A less dangerous and more effective surgical method is deep brain stimulation (DBS). But this expensive intervention can also lead to a number of side effects.
It should be added that any surgical intervention does not allow the abolition of antiparkinsonian drugs and has its own strict indications and contraindications.
What it is
The disease “inherited” its name from the name of the doctor who first described it in detail - the Englishman James Parkinson, who described the disorder as “shaking” paralysis. This neurological pathology is multifactorial (affects various body systems) and extensive damage to the central nervous system.
PD progresses slowly and steadily, interferes with the functioning of the human brain, leading to the death of dopaminergic neurons of the substantia nigra (located in the midbrain), which is responsible for regulating the motor function of the body, muscle tone, and is involved in the implementation of many autonomic functions.
In addition, the disease initiates a number of non-motor :
- sensory (pain, burning, numbness, tingling, impaired sense of smell);
- mental (apathy, depression);
- vegetative (tone of blood vessels, breathing, heart activity).
PD is characterized by age-related characteristics. As a rule, the first signs of the disease may appear as early as 50-55 years of age . In the age subgroup under 65 years, the prevalence of the disease increases to 1%; at 65-75 years old – already up to 2%; and the incidence of the disease from 3 to 4% is observed at the age of 75+ .
WHO records the figure for patients with PD at 3.7 million, with 300 thousand cases per year. The incidence of Parkinson's disease per 100 thousand population, according to various studies, averages from 60 to 180 cases.
Symptoms of Parkinson's disease and parkinsonism
Symptoms of Parkinsonism are disorders of movement and muscle tone and their combinations. Stiffness of movements, increased tone, tremors of the hands and head, chewing-type movements of the lower jaw, disturbances in handwriting and precision of movements, gait “bent over”, small steps, “shuffling”, poverty of facial movements - “frozen face”, decreased emotionality of behavior , depression. Symptoms of the disease, initially one-sided, further progress, in severe cases leading to disability, immobility, and cognitive impairment.
Symptoms of Parkinsonism
The main clinical syndrome in Parkinson's disease and parkinsonism is akinetic-rigid or hypertensive-hypokinetic. Shaking paralysis and parkinsonism are characterized by hypo- and akinesia. A peculiar flexion posture appears: the head and torso are tilted forward, the arms are half-bent at the elbow, wrist and phalangeal joints, often tightly brought to the lateral surfaces of the chest and torso, the legs are half-bent at the knee joints. Poor facial expressions are noted. The rate of voluntary movements gradually slows down with the development of the disease, sometimes complete immobility can occur quite early. The gait is characterized by small shuffling steps. There is often a tendency to involuntary run forward (propulsion). If you push the patient forward, he runs to avoid falling, as if “catching up with his center of gravity.” Often a push to the chest leads to running backwards (retropulsion) or to the side (lateropulsion). These movements are also observed when trying to sit down, stand up, or throw your head back. Often, with pronounced parkinsonism syndrome, the patient’s postures resemble cataleptic ones. Akinesis and plastic hypertension are especially pronounced in the muscles of the face, masticatory and occipital muscles, and muscles of the limbs. When walking, there are no friendly movements of the arms (acheirokinesis). Speech is quiet, monotonous, without modulation, with a tendency to fade at the end of the phrase.
During passive movement of the limb, a kind of muscle resistance is noted due to an increase in the tone of the antagonist muscles, the “gear wheel” phenomenon (the impression arises that the articular surface consists of the clutch of two gear wheels). An increase in the tone of antagonist muscles during passive movements can be determined by the following technique: if you raise the head of a person lying down, and then suddenly release your hand, the head will not fall on the pillow, but will fall relatively smoothly. Sometimes the head is slightly elevated when lying down - the “imaginary pillow” phenomenon.
Tremor is a characteristic, although not obligatory, symptom of parkinsonism syndrome. This is a rhythmic, regular, involuntary trembling of the limbs, facial muscles, head, lower jaw, tongue, more pronounced at rest, decreasing with active movements. Oscillation frequency is 4-8 per second. Sometimes finger movements in the form of “rolling pills” or “counting coins” are noted. The tremor intensifies with excitement and practically disappears in sleep.
Mental disorders are manifested by loss of initiative, activity, narrowing of horizons and interests, a sharp decrease in various emotional reactions and affects, as well as some superficiality and slowness of thinking (bradyphrenia). Bradypsychia is observed - difficult active switching from one thought to another, acairia - stickiness, viscosity, egocentrism. Sometimes paroxysms of mental excitement occur.
Autonomic disorders manifest themselves in the form of greasiness of the skin of the face and scalp, seborrhea, hypersalivation, hyperhidrosis, trophic disorders in the distal parts of the extremities. A violation of postural reflexes is detected. Sometimes special research methods are used to determine breathing that is irregular in frequency and depth. Tendon reflexes are usually without deviations. In atherosclerotic and postencephalitic parkinsonism, increased tendon reflexes and other signs of pyramidal insufficiency can be detected. With postencephalitic parkinsonism, so-called oculogyric crises occur - fixation of gaze upward for several minutes or hours; sometimes the head is thrown back. Crises can be combined with a violation of convergence and accommodation (progressive supranuclear palsy).
It is customary to distinguish several clinical forms of shaking palsy and parkinsonism; rigid-bradykinetic, tremulous-rigid and tremulous. The rigid-bradykinetic form is characterized by an increase in muscle tone according to the plastic type, a progressive slowdown of active movements up to immobility; muscle contractures and flexor posture of patients appear. This form of parkinsonism, the most unfavorable in its course, is more often observed in atherosclerotic and less often in postencephalitic parkinsonism. The trembling-rigid form is characterized by tremor of the extremities, mainly their distal parts, which is accompanied by stiffness of voluntary movements as the disease develops. The trembling form of parkinsonism is characterized by the presence of constant or almost constant medium- and large-amplitude tremor of the limbs, tongue, head, and lower jaw. Muscle tone is normal or slightly increased. The tempo of voluntary movements is maintained. This form is more common in postencephalitic and posttraumatic parkinsonism.
A person's movements, muscle control and balance of the body in space are impaired. This condition is formed precisely due to the destruction of the accumulation of part of the nerve cells (substantia nigra) of the brain stem. These nerve cells are connected by their fibers to both hemispheres of the brain. They produce and release special substances (neurotransmitters) that help control the movements and coordination of the body in space. Their absence leads to the appearance of such outwardly noticeable signs of parkinsonism as a decrease in the range of movements with an increase in muscle tone, trembling of the limbs, a mask-like facial expression, walking in small steps and similar symptoms.
Data from laboratory and functional studies.
In post-traumatic parkinsonism, an increase in cerebrospinal fluid pressure is detected with normal cellular and protein composition. In parkinsonism, which occurs as a result of carbon monoxide poisoning, carboxyhemoglobin is found in the blood; in manganese parkinsonism, traces of manganese are found in the blood, urine, and cerebrospinal fluid. Global electromyography in shaking paralysis and parkinsonism reveals a violation of muscle electrogenesis - an increase in the bioelectrical activity of muscles at rest and the presence of rhythmic group potential discharges. Electroencephalography reveals predominantly diffuse, rough changes in the bioelectrical activity of the brain.
Diagnosis and differential diagnosis of parkinsonism.
First of all, the doctor examines the patient and, based on this data, can make a preliminary diagnosis. It is necessary to differentiate Parkinson's disease from parkinsonism syndrome. Postencephalitic parkinsonism is characterized by oculomotor symptoms; Torticollis and torsion dystonia phenomena may be observed, which are never observed with shaking paralysis. There are sleep disturbances, respiratory dyskinesias with bouts of yawning, coughing, adiposogenital disorders, and vegetative paroxysms. Post-traumatic parkinsonism can be reliably diagnosed in young and middle-aged patients. The disease develops after severe, sometimes repeated traumatic brain injury. Post-traumatic parkinsonism is not characterized by antetropulsions, gaze convulsions, disorders of chewing, swallowing, breathing, and cataleptoid phenomena. At the same time, vestibular disorders, impaired intelligence and memory, and visual hallucinations (due to damage to the cerebral cortex) are common. A regressive course or stabilization of the pathological process is often observed. For the diagnosis of manganese parkinsonism, anamnesis (information about work in contact with manganese or its oxides) and the detection of manganese in biological fluids are important. Diagnosis of oxycarbon parkinsonism is based on the determination of carboxyhemoglobin in the blood.
In atherosclerotic parkinsonism, trembling and rigidity are combined with signs of cerebral atherosclerosis or occur after acute cerebrovascular accidents. Focal neurological symptoms are detected in the form of pyramidal insufficiency and severe pseudobulbar symptoms. The unilaterality of rigidity and stiffness is often determined. Dyslipidemia, characteristic of atherosclerosis, is detected in the blood. Certain changes in the REG are recorded in the form of flattening of pulse waves.
A clinical picture reminiscent of Parkinson's disease can be observed in senile atherosclerotic dementia, which is most characterized by severe mental disorders up to dementia. Rigidity and stiffness are moderate, tremor is usually absent. Individual clinical manifestations of parkinsonism can be detected in other hereditary degenerative diseases of the nervous system: Friedreich's ataxia, olivopontocerebellar atrophy, orthostatic hypokinesia, Creutzfeldt-Jakob disease. In these diseases, along with akinetic-rigid symptoms, there are progressive phenomena of cerebellar ataxia.
If a neurological examination is insufficient, the following methods can be used to clarify the diagnosis:
- REG, USDG of vessels of the neck and brain
- X-ray of the cervical spine with functional tests
- MRI of the brain and its vessels
- MRI of the cervical spine, etc.
Parkinsonism begins at 45-52 years of age, when the activity of dopaminergic structures decreases significantly. This is a disease of neurotransmitter metabolism - there is insufficient production of dopamine in the basal ganglia and with the loss of 70% of dopamine in the striatum (caudate nucleus and putamen), clinical signs of parkinsonism appear. The only reliable diagnostic criterion is positron emission tomography. In practice, a specific reaction to levodopa is used, the administration of which leads to the disappearance of the symptoms of the disease.
In young people
Symptoms and signs in young or young patients with PD are in most cases similar to the classic version of the disease.
- Early (juvenile) parkinsonism tends to manifest itself in the age period of 20-40 years . As the disease progresses, secondary symptoms that are not related to motor activity begin to appear - the disease does not affect the substantia nigra (as in older patients), but other areas of the brain.
- Motor manifestations are reduced to involuntary and painful contraction of the muscles of the shoulder girdle and feet, as well as involuntary motor activity in the limbs or body in general.
In general, the disease at a young age occurs in a mild form, because There are no presence of many disorders of the body’s physiology inherent in older patients.
What care do patients with Parkinson's syndrome require?
Parkinson's disease in older people is accompanied by movement disorders. Intelligence can also be affected, but this does not always happen. Therefore, when caring for patients, they should be trusted as much as possible. They should perform the movements independently whenever possible so as not to increase the progression of movement disorders. In the patient's room it is worth leaving a minimum of furniture and other objects that would interfere with his movement.
Take care in advance of special devices to help the patient move safely. These are various rubber mats (especially needed in the bathroom), handrails, etc.
Caring for elderly people with Parkinson's syndrome should also include monitoring the patient's medication intake. This should be done unobtrusively, remembering that in most patients the intellect does not suffer.
In this case, it is necessary to monitor the mental state of patients: their mood, night sleep, etc. The appearance of tearfulness, aggressiveness, irritability, and depression should not be ignored by the caregiver. This should be reported to the doctor in order to prescribe appropriate treatment.
The life expectancy and quality of life of patients with Parkinson's syndrome largely depend on timely treatment and proper care.