In the 21st century, the main cause of death is considered to be vascular accidents - heart attacks and strokes, which are largely a consequence of hypercholesterolemia, atherosclerosis and hypertension. It would seem that liver cirrhosis almost never appears in large-scale surveys devoted to public health, but it only seems so. If we take the mortality rate of the active population, aged 35 to 65 years, then liver cirrhosis will be in sixth place. Thus, in the United States it is the fourth leading cause of death in the population over 40 years of age.
To imagine the global scale, it is enough to say that every year on our planet 40 million people die from cirrhosis - that’s three Moscows along with their suburbs! At the same time, mortality is constantly increasing. What is this insidious disease, what are its causes, how does it manifest itself and how is it treated?
Some historical data
Since ancient times, the liver has been considered as important an organ as the heart. According to the inhabitants of Mesopotamia, the liver produces blood and the soul lives. Hippocrates also described the connection between liver diseases and jaundice, as well as ascites. He argued that jaundice and hard liver were a bad combination of symptoms. This was the first judgment about liver cirrhosis and its symptoms.
Cirrhosis of the liver and its causes were described in 1793 by Matthew Baillie in his treatise Morbid Anatomy. In his work, he clearly linked the consumption of alcoholic beverages with the occurrence of symptoms of liver cirrhosis. In his opinion, middle-aged and older men were more likely to get sick. The British dubbed cirrhosis the “gin plague” or “gin liver.”
The term cirrhosis comes from the Greek “kirrhos”, which means yellow and belongs to René Théophile Hyacinthe Laennec, a French physician and anatomist. Many scientists have worked and continue to work on the study of liver cirrhosis to this day. Virchow, Kuehne, Botkin, Tatarinov, Abelov and others proposed many theories about what liver cirrhosis is, its symptoms, causes, methods of diagnosis and treatment.
Treatment
The doctor always decides how to treat cirrhosis on an individual basis. There is no universal remedy for getting rid of this pathology. Maintenance therapy is used, the goals of which are:
- eliminate signs of intoxication;
- relieve pain;
- normalize and support the functions of healthy liver cells that have not yet been replaced by connective tissue.
Patients are necessarily prescribed a special diet to reduce the load on the damaged organ and medications. These measures are aimed at maintaining long-term remission. Treatment of concomitant diseases is also often required, because cirrhosis can provoke complications from the gastrointestinal tract, kidneys, heart, blood vessels, and central nervous system.
Reasons for the development of cirrhosis
Among the main reasons leading to the development of the disease are:
- Viral hepatitis, which, according to various estimates, leads to the formation of liver pathology in 10-24% of cases. The disease results in such types of hepatitis as , , D and the recently discovered hepatitis G;
- Various diseases of the biliary tract, including extrahepatic obstruction, cholelithiasis and primary sclerosing cholangitis;
- Disturbances in the functioning of the immune system. Many autoimmune diseases lead to the development of cirrhosis;
- Portal hypertension;
- Venous congestion in the liver or Budd-Chiari syndrome;
- Poisoning with chemicals that have a toxic effect on the body. Among such substances, industrial poisons, salts of heavy metals, aflatoxins and mushroom poisons are especially harmful to the liver;
- Diseases transmitted by inheritance, in particular, genetically determined metabolic disorders (anomalies of glycogen accumulation, Wilson-Konovalov disease, deficiency of α1-antitrypsin and galactose-1-phosphate-uridyltransferase);
- Long-term use of medications, including Iprazide, anabolic steroids, Isoniazid, androgens, Methyldopa, Inderal, Methotrexate and some others;
- Drinking large doses of alcohol for 10 years or more. There is no dependence on a specific type of drink; the fundamental factor is the presence of ethyl alcohol in it and its regular intake into the body;
- The rare Osler-Rendu disease can also cause cirrhosis.
In addition, it is worth mentioning separately about cryptogenic cirrhosis, the causes of which remain unclear. It occurs in the range from 12 to 40% of cases. Provoking factors for the formation of scar tissue can be systematic malnutrition, infectious diseases, syphilis (which can cause cirrhosis in newborns). The combined influence of etiological factors, for example, a combination of hepatitis and alcoholism, significantly increases the risk of developing the disease.
Cirrhosis - what is it?
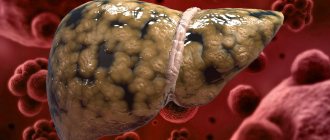
Gradual replacement of hepatocytes with fibrous tissue
Eight thousand years ago, a supernova exploded in the constellation Cygnus, and a nebula appeared in its place. It is poetically called “veil”, “fishing net”, or simply cirrus, cirrus. Cirrhosis and cirrus are the same root words. Cirrhosis is the growth of a mesh structure in the liver.
Normally, the liver consists of cells - hepatocytes, which are penetrated by blood capillaries, and at the exit from them bile is formed, which also collects in the bile ducts. These cells are arranged in tiers, in orderly rows, which are clearly visible under a microscope. These rows are called hepatic lobules, which are strictly organized. Larger segments, lobes of the liver, and the organ itself are made up of lobules.
Hepatocytes make up the liver parenchyma. Parenchyma is a specific tissue of an organ, which constitutes its “meaning”, distinguishing it from others. For example, the parenchyma of the liver and pancreas differ from each other because the functions of these organs are different.
In addition to the intensively working liver cells, there is a supporting (framework) tissue, or stroma - it looks like a network, or a veil. Consists of connective or fibrous tissue. And this framework in any organ is the same in cellular composition. The main role of the stroma is to be a “skeleton” for glandular tissue. With cirrhosis of the liver, all working tissue (parenchyma) gradually dies, and instead there is a proliferation of fibrous tissue. She does not “know how” to do anything, and cannot replace dead hepatocytes. Essentially, with cirrhosis, the entire liver is a rigid mesh, a “washcloth,” of overgrown stroma, interspersed with remnants of working tissue.
Since the liver is a vital organ, cirrhosis of the liver leads to irreversible chronic liver failure and death of the patient. The only chance to survive is a liver transplant.
Causes of cirrhosis
Of course, as with any disease in general, the causes of liver cirrhosis can be hidden even after a thorough and comprehensive examination. In this case, a diagnosis of cryptogenic cirrhosis is made. But this happens very rarely. Much more often, the causes of cirrhosis are more prosaic, both in men and women. Here are the most likely “candidates”:
- The presence of viral hepatitis, including B, C, D. Very rarely, acute hepatitis can transform into cirrhosis, but still the main role belongs to the chronic course, with medium or high activity. In women with hepatitis B and C, with such activity in 25% of cases, the outcome of hepatitis in cirrhosis is possible;
- Regular consumption of alcoholic beverages, alcoholism. If women's daily alcohol intake in terms of ethyl alcohol is 60 - 110 g, then 10% of patients will develop cirrhosis after many years of alcohol consumption. This corresponds to approximately 1.5 liters of strong beer per day (100 g of 96% alcohol). It is important that among female alcoholics, the number of patients with liver cirrhosis at a young age has recently increased;
- Hereditary metabolic diseases (antitrypsin deficiency, hemochromatosis, Wilson-Konovalov disease and others);
- As a side effect on medications (methotrexate, anti-tuberculosis drugs);
- Hepatotoxic poisons (carbon tetrachloride);
- Processes that lead to obstruction of the bile ducts (in this case, women develop secondary biliary cirrhosis). This is cholelithiasis, duct strictures, cholangitis, as well as incomplete obstruction, with partial patency. Usually, under such conditions, cirrhosis of the liver forms within a year;
- In the presence of venous stagnation in the liver tissue (with Budd-Chiari syndrome). The cause may lie far beyond the organ - for example, with valvular defects of the tricuspid valve, with adhesive and constrictive pericarditis.
Cirrhosis can also be caused by parasitic infections (schistosomiasis), autoimmune hepatitis, and other causes.
Classification
The modern classification of the disease in question is based on taking into account etiological, morphogenetic and morphological criteria, as well as clinical and functional criteria. Based on the reasons behind the influence of which cirrhosis of the liver developed, the following variants are determined:
- biliary cirrhosis (primary, secondary) (cholestasis, cholangitis);
- circulatory cirrhosis (arising against the background of chronic venous stagnation);
- metabolic and nutritional cirrhosis (lack of vitamins, proteins, accumulation cirrhosis resulting from hereditary metabolic disorders);
- infectious (viral) cirrhosis (hepatitis, biliary tract infections, parasitic liver diseases);
- toxic cirrhosis, toxic-allergic cirrhosis (food and industrial poisons, medications, allergens, alcohol);
- cryptogenic cirrhosis.
Depending on the clinical and functional characteristics, liver cirrhosis is characterized by a number of the following features:
- level of hepatic cell failure;
- general nature of the disease (progressive, stable or regressive);
- the degree of portal hypertension relevant to the disease (bleeding, ascites);
- general activity of the disease process (active cirrhosis, moderately active cirrhosis, as well as inactive cirrhosis).
Causes that trigger the mechanism of cirrhosis of the liver
The most common causes of liver damage are:
- viral hepatitis (B, C, D, G), the most dangerous are hepatitis C and D;
- autoimmune hepatitis, in which the human defense system begins to mistake its own cells for foreign ones and destroys them;
- abnormalities of the biliary tract - decreased patency of the bile ducts (liver disease progresses after 3-18 months);
- stagnation of venous blood in the liver for a long period (constrictive pericarditis, veno-occlusive disease, heart failure);
- hereditary diseases (Wilson-Konovalov).
In cases where it is impossible to determine the cause of the pathology, cryptogenic cirrhosis is diagnosed, characterized by accelerated pathogenesis and destruction of liver tissue.
Alcoholic liver damage
Alcoholic liver damage occurs due to prolonged consumption of alcohol-containing drinks, that is, in alcoholics. In alcoholic cirrhosis of the liver, symptoms are expressed by weight loss, fever, enlarged salivary glands, and Dupiutren's contracture.
Portal cirrhosis of the liver
The most common form of the disease, which is characterized by damage to liver tissue and death of hepatocytes. Changes occur due to poor nutrition and alcohol abuse. In 20%, portal cirrhosis can cause Botkin's disease. First, the patient complains of disorders of the digestive tract. Then external signs of the disease develop: yellowing of the skin, the appearance of spider veins on the face. The last stage is characterized by the development of ascites (abdominal dropsy).
Causes of complications of cirrhosis
Complications are a consequence of irreversible changes in the liver tissue. In turn, irreversible changes in hepatocytes are a consequence of chronic liver diseases.
The main reason for the development of complications of cirrhosis is the patient’s late visit to the doctor. After all, at the initial stage of the pathology there are no pronounced symptoms. Regular medical examinations help identify liver pathology at an early stage. The treatment that has begun will allow you to preserve hepatocytes, because they have great capabilities for self-healing.
Another, no less serious reason due to which complications develop is prolonged consumption of alcoholic beverages. Other reasons for the deterioration of the patient’s condition:
- obstruction of the biliary tract;
- cystic fibrosis;
- autoimmune diseases;
- hepatitis type B or C;
- iron metabolism disorder;
- non-alcoholic fatty liver disease.
First signs
Early symptoms indicating cirrhosis include the following:
- A feeling of bitterness and dryness appears in the mouth, especially often in the morning;
- The patient loses some weight, becomes irritable, and gets tired faster;
- A person may be bothered by periodic stool disorders, increased flatulence;
- Periodically occurring pain localized in the right hypochondrium. They tend to increase after intense physical activity or after taking fatty and fried foods, alcoholic beverages;
- Some forms of the disease, for example, postnecrotic cirrhosis, manifest themselves in the form of jaundice already in the early stages of development.
In some cases, the disease manifests itself acutely and there are no early signs.
Similar pathologies
Cirrhosis in women at the compensation stage has similar symptoms to:
- gastritis;
- cholecystitis;
- stomach ulcer.
If the diagnosis is made incorrectly (an illiterate diagnosis can lead to this), then the therapy will be ineffective and the disease will continue to progress. There are no external manifestations at the initial stage of the disease, since healthy cells of the organ can still work in an enhanced mode, replacing damaged areas.
If cirrhosis is detected in a woman at the compensation stage, she strictly follows medical recommendations, then the prognosis is relatively favorable. Thanks to modern medicines and technologies, pathological changes in the organ can be stopped for a long time.
Symptoms of cirrhosis
Cirrhosis is characterized by general symptoms: weakness, decreased ability to work, discomfort in the abdomen, dyspeptic disorders, increased body temperature, joint pain, flatulence, pain and a feeling of heaviness in the upper abdomen, weight loss, asthenia. Upon examination, an enlargement of the liver, compaction and deformation of its surface, and sharpening of the edge are revealed. At first, there is a uniform moderate increase in both lobes of the liver; later, as a rule, the increase in the left lobe predominates. Portal hypertension is manifested by a moderate enlargement of the spleen.
The detailed clinical picture is manifested by the syndromes of hepatic cell failure and portal hypertension. There is bloating, poor tolerance to fatty foods and alcohol, nausea, vomiting, diarrhea, a feeling of heaviness or abdominal pain (mainly in the right hypochondrium). In 70% of cases, hepatomegaly is detected, the liver is compacted, and the edge is sharpened. In 30% of patients, palpation reveals a nodular surface of the liver. Splenomegaly in 50% of patients.
Low-grade fever may be associated with the passage of intestinal bacterial pyrogens through the liver, which it is unable to neutralize. The fever is resistant to antibiotics and resolves only when liver function improves. There may also be external signs - palmar or plantar erythema, spider veins, scanty hair in the axillary and pubic area, white nails, gynecomastia in men due to hyperestrogenemia. In some cases, the fingers take on the appearance of “drum sticks.”
In the terminal stage of the disease, in 25% of cases there is a decrease in liver size. Jaundice, ascites, peripheral edema due to overhydration (primarily swelling of the legs), external venous collaterals (varicose veins of the esophagus, stomach, intestines) also occur. Bleeding from veins is often fatal. Hemorrhoidal bleeding occurs less frequently and is less intense.
General symptoms
Complications of liver cirrhosis are manifested by the following symptoms:
- weakness and fatigue;
- loss of appetite and weight loss;
- jaundice;
- redness of the palms and feet;
- nausea;
- bloating;
- pain in the right hypochondrium;
- dropsy;
- hernias;
- decreased sex drive;
- testicular atrophy in men, enlarged mammary glands;
- dilation of veins around the navel;
- swelling of the legs;
- bleeding;
- enlarged liver, spleen.
Patients also complain of memory loss, insomnia, and daytime sleepiness. Long-lasting headaches are typical. Convulsions, lethargy, decreased and complete absence of reflexes are observed.
Consequences
Liver cirrhosis, in principle, alone does not cause death; its complications in the decompensation stage are deadly. Among them:
- Ascites in cirrhosis is an accumulation of fluid in the abdominal cavity. A diet with limited protein (up to 0.5 grams per kg of body weight) and salt, diuretics, and intravenous administration of albumin (a protein drug) are prescribed. If necessary, resort to paracentesis - removal of excess fluid from the abdominal cavity.
- Spontaneous bacterial peritonitis is inflammation of the peritoneum due to infection of the fluid in the abdominal cavity (ascites). Patients have a fever of up to 40 degrees, chills, and intense abdominal pain. Long-term broad-spectrum antibiotics are prescribed. Treatment is carried out in the intensive care unit.
- Hepatic encephalopathy. Manifests itself from minor neurological disorders (headache, increased fatigue, lethargy) to severe coma. Since it is associated with the accumulation of protein metabolism products (ammonia) in the blood, protein is limited or excluded from the diet, and a prebiotic is prescribed - lactulose. It has a laxative effect and the ability to bind and reduce the formation of ammonia in the intestines. For severe neurological disorders, treatment is carried out in the intensive care unit.
- Hepatorenal syndrome is the development of acute renal failure in patients with liver cirrhosis. Stop the use of diuretics and prescribe intravenous albumin. Treatment is carried out in the intensive care unit.
- Acute variceal bleeding. Arises from varicose veins of the esophagus and stomach. The patient becomes increasingly weak, blood pressure drops, pulse quickens, and vomiting appears mixed with blood (the color of coffee grounds). Treatment is carried out in the intensive care unit; if ineffective, surgical treatment methods are used. To stop bleeding, intravenous administration of octropide is used (to reduce pressure in the blood flow of the abdominal vessels), endoscopic treatment (ligation of varicose veins, sclerotherapy). Transfusion of solutions and blood components is carried out carefully to maintain the required level of hemoglobin.
- The development of hepatocellular carcinoma is a malignant neoplasm of the liver.
The definitive treatment for hepatocellular carcinoma and decompensated liver cirrhosis is liver transplantation. Replacing a patient's liver with a donor's liver.
Course and clinical manifestations of cirrhosis
The insidiousness of cirrhosis lies in the fact that in the early stages, in 70-80% of cases there is an asymptomatic course, or the signs are disguised as other diseases - stomach problems, colds, respiratory infections.
At the beginning of the development of the disease, hepatocytes successfully cope with the functionality of dead liver cells, which slows down the process of the appearance of the clinic.
Over time, as more and more hepatocytes are destroyed, certain symptoms appear.
Early signs
The initial symptoms of liver cirrhosis in women are characteristic of many diseases, so even a highly qualified medical specialist with extensive practice experience will not immediately suspect the disease.
The first signs of cirrhosis in humans include:
- Decreased performance.
- Chronic fatigue without cause.
- Disorders of the digestive system.
- Unpleasant odor from the mouth.
- Emotional instability - apathy gives way to irritability, etc.
- Loss of body weight. The symptom is associated with a deterioration in appetite or its complete loss.
- Dry mouth, bitterness - most often in the morning, immediately after sleep.
- Discomfort or distension in the liver projection area.
- Swelling of the lower extremities.
- Excessive dryness of the skin.
After physical activity, consumption of alcohol or fatty foods, or a stressful situation, pain in the side increases. Symptoms increase gradually, become permanent, and new signs appear that aggravate the picture.
Symptoms as the disease progresses
In all people, the process of transformation of full-fledged liver cells into connective non-functional tissue develops at an excellent speed. This is due to lifestyle, concomitant diseases, diet, and age.
There are 4 stages of the disease.
If at the first stage there are practically no symptoms, then at the 2nd stage they begin to increase and cause a lot of concern. On the 3rd, the following signs appear:
- Yellowing of the skin, visible mucous membranes and whites of the eyes. Color - different - varies from slightly yellow to bright orange.
- Itching of the skin, intensifies mainly at night.
- Increase in abdominal volume.
- The liver palms symptom is characterized by redness of the surface of the skin on the hands and sometimes feet.
- The “head of Medusa” symptom is manifested by a venous pattern on the abdomen.
- Severe digestive dysfunction.
- Nausea, frequent vomiting (with an admixture of bile, blood streaks).
- The wounds do not heal well, and the nose bleeds periodically.
- Changes in behavior – tearfulness, apathy, irritability.
- Constant pain in the right side area.
Cirrhosis of the liver in women leads to disruption of the menstrual cycle, so diagnosis often goes the wrong way. Doctors suspect pathologies of the genitourinary system, although tests of its functionality show normality.
In women with destructive processes in the liver, problems with reproductive function are identified, and pregnancy often ends in premature birth.
Specific clinic of cirrhosis
In the early stages, it is difficult to suspect cirrhosis, since no specific symptoms are observed. In the later stages, the patient’s appearance and his complaints will “tell” the doctor about the disease:
- Heavy menstruation or its complete absence, which is not associated with female menopause.
- Hemorrhoidal bleeding.
- Severe hepatomegaly - the liver is significantly larger than normal size.
- The edge of the liver protrudes to the right side.
- The color of the tongue is crimson and shiny.
- The urine is dark brown and the stool is discolored.
- Swelling of the arms and legs, puffiness of the face.
- Tremor of the limbs (if the cause is alcoholic cirrhosis).
The listed symptoms are a direct indication for immediate examination and subsequent treatment.
Diagnostics
Determining the diagnosis of liver cirrhosis takes place in several stages. The diagnosis itself is made on the basis of instrumental research data:
- Magnetic resonance or computed tomography is the most accurate diagnostic method.
- Biopsy is a method of histological examination of material taken from the liver, which makes it possible to establish the type of large- or small-nodular cirrhosis and the cause of the development of the disease.
- Ultrasound – as a screening. Allows you to establish only a preliminary diagnosis, but is indispensable when diagnosing ascites and portal hypertension.
If, upon diagnosis, histological examination does not allow determining the cause of the disease, the search for it continues. To do this, perform a blood test to determine the presence of:
- antimitochondrial antibodies;
- Hepatitis C virus RNA and hepatitis B virus DNA using the PCR method;
- alpha-fetoprotein – in order to exclude blood cancer;
- copper and cerruloplasmin levels;
- level of immunoglobulins A and G, level of T-lymphocytes.
At the next stage, the degree of damage to the body due to liver damage is determined. For this use:
- liver scintigraphy - radionuclide study to determine working liver cells;
- biochemical blood test to determine indicators such as sodium and potassium levels, coagulogram, cholesterol, alkaline phosphatase, total and fractional bilirubin, AST, ALT, lipidogram, proteinogram;
- degree of kidney damage – creatinine, urea.
Absence or presence of complications:
- Ultrasound to exclude ascites;
- eliminating internal bleeding in the digestive tract by examining stool for the presence of hidden blood;
- FEGDS - to exclude varicose veins of the stomach and esophagus;
- sigmoidoscopy to exclude varicose veins in the rectum.
In cirrhosis, the liver can be palpated through the anterior wall of the peritoneum. On palpation, the tuberosity and density of the organ are noticeable, but this is only possible at the stage of decompensation.
Ultrasound examination clearly identifies foci of fibrosis in the organ, and they are classified into small ones - less than 3 mm, and large ones - over 3 mm. With the alcoholic nature of cirrhosis, initially small nodes develop; a biopsy determines specific changes in liver cells and fatty hepatosis. In later stages of the disease, the nodes enlarge and become mixed, and fatty hepatosis disappears. Primary biliary cirrhosis is characterized by an enlarged liver while maintaining the structure of the biliary tract. In secondary biliary cirrhosis, the liver becomes enlarged due to obstructions in the bile ducts.
Treatment of cirrhosis
Doctors do not have specific treatments that can cure cirrhosis specifically. However, they can treat many of the diseases that cause cirrhosis (and the main therapy is aimed at this). Some of the diseases that cause cirrhosis can be cured. Treating the underlying causes can prevent the disease from getting worse and prevent liver failure. Successful treatment may gradually improve some scarring in the liver.
The causes of cirrhosis are treated mainly with medications. The doctor will recommend stopping drinking alcohol and taking certain medications that may have caused the cirrhosis or may make it worse.
Alcoholic liver disease.
If the patient suffers from alcoholic liver disease, the doctor will recommend stopping drinking alcohol completely.
Non-alcoholic fatty liver disease.
If the cause is non-alcoholic fatty liver disease, your doctor may recommend weight loss. Losing weight through a healthy diet and regular exercise can reduce liver fat, inflammation, and scarring.
Chronic hepatitis C.
If a person has chronic hepatitis C, a doctor may prescribe one or more medications that have been approved to treat hepatitis C since 2013. Studies have shown that these medications can cure chronic hepatitis C in 80 to 95 percent of people with the disease.
Chronic hepatitis B.
For chronic hepatitis B, your doctor may prescribe antiviral drugs that slow or prevent further damage from the virus to your liver.
Autoimmune hepatitis.
Autoimmune hepatitis is treated with medications that suppress or reduce the activity of the immune system.
Diseases that damage, destroy, or block the bile ducts.
Doctors usually treat conditions that damage, destroy, or block the bile ducts with medications such as ursodeoxycholic acid (Ursosan, Exchol). Doctors may also use surgical procedures to open bile ducts that are narrowed or blocked.
Diseases that damage, destroy, or block the bile ducts include primary biliary cholangitis and primary sclerosing cholangitis.
Hereditary liver diseases.
Treatment for hereditary liver diseases depends on the disease. Treatment is most often aimed at eliminating symptoms and complications.
Long-term use of certain medications.
The only specific treatment for most cases of cirrhosis caused by certain medications is to stop taking the drug that caused the problem. Talk to your doctor before starting or stopping any medications.
Treatment of complications of cirrhosis
Treatment for complications of liver cirrhosis includes the following.
Portal hypertension.
Doctors treat portal hypertension with medications to reduce high blood pressure in the portal vein. Treatment for complications of portal hypertension includes:
- Varicose veins. Your doctor may prescribe medications to reduce pressure in the veins in your esophagus or stomach. This reduces the chance that veins will dilate and burst, causing internal bleeding. If you are vomiting blood or have bloody or black stools, go to the hospital immediately. Doctors may perform procedures during an upper gastrointestinal endoscopy or use surgical procedures to stop internal bleeding.
- Swelling in the legs, ankles, or feet. Your doctor may prescribe medications to remove fluid from your body. It is also recommended to limit the amount of salt in your diet.
- Ascites. The doctor will also prescribe medications that remove fluid from the body. Recommends limiting salt intake. If there is a large amount of fluid in the abdomen, the doctor may use needles or tubes to drain the fluid. He or she will check the fluid for signs of infection and prescribe medications to treat the infection.
- Problems with thinking, memory loss, personality changes or sleep disturbances resulting from hepatic encephalopathy. Your doctor may prescribe medications that reduce toxins in the brain and improve brain function.
Stages of liver cirrhosis
The course of the disease, as a rule, is characterized by its own duration, with the following main stages being distinguished:
- Compensation stage. It is characterized by the absence of symptoms of cirrhosis, which is explained by increased work of the remaining liver cells.
- Subcompensation stage. At this stage, the first signs of liver cirrhosis are noted (in the form of weakness and discomfort in the right hypochondrium, decreased appetite and weight loss). The functions inherent in the liver are performed in an incomplete manner, which occurs due to the gradual loss of resources of the remaining cells.
- Stage of decompensation. Here we are already talking about liver failure, manifested by severe conditions (jaundice, portal hypertension, coma).
Degrees of cirrhosis
The disease goes through several stages of development, each of which has certain clinical symptoms. Not only the person’s condition, but also the therapy he requires will depend on how much the pathology has progressed.
Liver cirrhosis of any etiology develops according to a single mechanism, which includes 3 stages of the disease:
- Stage 1 (initial or latent), which is not accompanied by biochemical disorders;
- Stage 2 of subcompensation, in which all clinical manifestations indicating functional liver disorders are observed;
- Stage 3 of decompensation or stage of development of hepatic cellular failure with progressive portal hypertension.
Last 4th degree of cirrhosis
Liver cirrhosis of the 4th degree is characterized by an exacerbation of all kinds of signs and symptoms of the disease, severe pain, which can only be relieved by strong drugs, sometimes of a narcotic nature.
Patients with cirrhosis at this stage have a characteristic appearance:
- pale yellow loose skin;
- with combs;
- yellow eyes;
- red and purple “spiders” of blood vessels are visible on the skin of the face and body;
- thin and thin arms and legs;
- bruises on arms and legs;
- large belly with a protruding navel;
- on the stomach - a network of dilated veins;
- red palms with reddened and thickened terminal phalanges, dull nails;
- swelling in the legs;
- enlarged breasts, small testicles in men.
Why do these signs appear at stage 4?
- Firstly, due to the fact that ammonia compounds, which are extremely toxic, accumulate in the blood, the patient is diagnosed with encephalopathy. Subsequently, hepatic coma develops. After a short period of euphoria, consciousness is depressed and orientation is completely lost. Problems arise with sleep and speech. Then a depressive state occurs and the patient loses consciousness.
- Secondly, the presence of ascites, in which there is a significant accumulation of fluid, provokes bacterial peritonitis. The eyelids and legs swell.
- Thirdly, it is because of heavy bleeding that patients most often die.
How to treat liver cirrhosis?
In general, the treatment of liver cirrhosis is selected on a strictly individual basis - therapeutic tactics depend on the stage of development of the disease, the type of pathology, the general health of the patient, and concomitant diseases. But there are also general principles for prescribing treatment.
These include:
- The compensated stage of liver cirrhosis always begins with eliminating the cause of the pathology - in this case, the liver is still able to function normally.
- The patient needs to adhere to a strict diet - even a slight violation can trigger the progression of liver cirrhosis.
- It is impossible to carry out physiotherapy or heat treatment for the disease in question. Physical activity is also excluded.
- If the disease is at the stage of decompensation, the patient is placed in a medical institution. The fact is that with this course of the disease, the risk of developing severe complications is very high and only medical workers will be able to promptly pay attention to even a slight deterioration in the condition and prevent the development of complications that lead to the death of the patient.
- Most often, hepatoprotectors, beta-blockers, sodium and ursodeoxycholic acid preparations are prescribed for treatment.
General advice for patients with liver cirrhosis:
- Rest as soon as you feel tired.
- To improve digestion, patients are prescribed multienzyme drugs.
- Avoid heavy lifting (this may cause gastrointestinal bleeding)
- Measure your body weight and abdominal volume at the navel level daily (an increase in abdominal volume and body weight indicates fluid retention);
- If there is fluid retention in the body (edema, ascites), it is necessary to limit the intake of table salt to 0.5 g per day, liquid intake to 1000-1500 ml per day.
- To monitor the extent of damage to the nervous system, it is recommended to use a simple handwriting test: write a short phrase, for example, “Good morning,” in a special notebook every day. Show your notebook to your relatives - if your handwriting changes, contact your doctor.
- Every day, count the fluid balance for the day (diuresis): count the volume of all liquid taken orally (tea, coffee, water, soup, fruit, etc.) and count all the liquid released during urination. The amount of fluid released should be approximately 200-300 ml more than the amount of fluid taken.
- Aim for stool frequency 1-2 times a day. Patients with liver cirrhosis are recommended to take lactulose (Duphalac) to normalize intestinal function and the composition of the intestinal flora in favor of “good” bacteria. Duphalac is prescribed in a dose that causes soft, semi-formed stools 1-2 times a day. The dose ranges from 1-3 teaspoons to 1-3 tablespoons per day, selected individually. The drug has no contraindications; it can be taken even by small children and pregnant women.
Treatment of pathological manifestations and complications of cirrhosis means:
- Reducing ascites using conservative (diuretic drugs according to the regimen) and surgical (removal of fluid through drains) methods.
- Treatment of encephalopathy (nootropics, sorbents).
- Relief of manifestations of portal hypertension - from the use of non-selective beta-blockers (propranolol, nadolol) to ligation of dilated veins during surgery.
- Preventive antibiotic therapy to prevent infectious complications during planned visits to the dentist, before instrumental procedures.
- Treatment of dyspepsia through nutritional correction and the use of enzyme preparations without bile acids (pancreatin). In such cases, it is also possible to use eubiotics - bactisubtil, enterol, bifidumbacterin and lactobacterin.
- To relieve skin itching, antihistamines are used, as well as drugs containing ursodeoxycholic acid.
- Prescription of androgens for men with severe manifestations of hypogonadism and correction of the hormonal levels of women to prevent dysfunctional uterine bleeding - under the supervision of an endocrinologist.
- The use of drugs containing zinc is indicated for the prevention of cramps during normal muscle activity and in the complex treatment of liver failure to reduce hyperammonemia.
- Prevention of osteoporosis in patients with chronic cholestasis and primary biliary cirrhosis, in the presence of autoimmune hepatitis with the use of corticosteroids. To do this, calcium is additionally introduced in combination with vitamin D.
- Surgical correction of portal hypertension for the prevention of gastrointestinal bleeding includes the application of vascular anastomoses (mesentericocaval and splenorenal) as well as sclerotherapy of existing dilated veins.
- In the presence of single foci of degeneration into hepatocellular carcinoma and the severity of the disease of class A, patients are advised to undergo surgical removal of the affected liver segments. In case of clinical class B and C disease and massive lesions, while awaiting transplantation, antitumor treatment is prescribed to prevent progression. To do this, they use both the effects of currents and temperatures (percutaneous radiofrequency thermal ablation) and chemotherapy by targeted injection of oil solutions of cytostatics into the vessels supplying the corresponding segments of the liver (chemoembolization).
Treatment of such a serious and fatal complication as acute massive bleeding from the veins of the esophagus includes:
- Local application of a Blackmore probe, with the help of which an air cuff is inflated in the lumen of the esophagus, compresses the dilated bleeding veins.
- Targeted injection of the esophageal wall with sclerosing substances.
- Blood replacement therapy.
Unfortunately, this condition becomes the main cause of death in patients with cirrhosis of the liver.
What are the complications?
Patients with liver cirrhosis and their loved ones should know everything about cirrhosis, incl. about its consequences. Preservation of the patient's life depends on the provision of medical care. With complications of cirrhosis, life-threatening symptoms occur.
Hepatic encephalopathy
This is damage to brain tissue by toxic products that accumulate in the body due to gradual liver damage. Characteristic disorders of cognitive activity and behavior. Neuromuscular disorders are common. The danger of encephalopathy is that at the initial stage of development it can only be detected using special liver tests.
Encephalopathy is caused by:
- uncontrolled use of diuretics;
- prolonged vomiting and diarrhea;
- bleeding from the digestive tract;
- infectious pathologies of the urinary system and respiratory tract;
- constipation;
- eating protein-rich foods (the breakdown of proteins produces ammonia, which is very harmful to brain cells);
- consumption of alcoholic beverages;
- taking sleeping pills and other drugs that depress brain activity.
Infectious pathologies
Patients with cirrhosis are more susceptible to bacterial and viral diseases than other people. Most often they have infections of the respiratory and urinary system. Sometimes the body temperature in cirrhosis can rise for no apparent reason.
Infectious diseases are difficult to cure, since drugs against them change their effect when they are among toxins that are not processed by the liver. Patients need to monitor their health, avoid hypothermia and take medications to boost immunity.
Bleeding from the veins of the esophagus
With cirrhosis of the liver, redistribution of blood flow in the abdominal cavity occurs. The liver vessels are compressed, which leads to overload and dilation of the esophageal veins. At the same time, the vascular walls become thinner, which leads to an increased risk of bleeding. It can occur during increased pressure inside the arteries, vomiting, or physical exertion.
When bleeding from varicose veins, the following symptoms are observed:
- vomiting of scarlet contents;
- severe weakness;
- dizziness;
- liquid stool with a tarry consistency.
Ascites
This is a pathological accumulation of fluid in the abdominal cavity due to portal hypertension and increased sodium concentration in the body. The amount of liquid can vary from 1 to 25 liters. It compresses the organs, aggravating the patient’s condition with gastroesophageal disease and atrophic gastritis.
Ascites as a complication of cirrhosis significantly worsens the prognosis. More than 40% of patients die within 24 months after being diagnosed with ascites. Only treatment by highly qualified specialists using the latest equipment helps achieve a positive result.
The development of this complication of liver cirrhosis can be gradual and rapid. With a rapidly developing disease, the patient’s stomach is inflated and his skin is stretched. A huge belly prevents normal breathing and movement.
With transient ascites, as the patient's condition improves, the amount of fluid decreases. The stationary form of ascites is dangerous because, despite treatment, the volume of fluid in the abdominal cavity does not decrease.
Ascites in cirrhosis is an alarming signal. It indicates that the disease is transforming into the terminal stage. When the abdominal organs are compressed, intestinal paralysis occurs. A large amount of fluid displaces the heart, causing the development of heart failure.
Normalization of fluid accumulation is associated with the treatment of cirrhosis. The diet completely excludes table salt. Diuretics are prescribed, and if necessary, fluid is removed from the abdominal cavity.
Peritonitis
As a result of cirrhosis, inflammation of the peritoneum occurs in the body. Peritonitis occurs in patients with high portal vein pressure. This type of complication in liver cirrhosis occurs in 8-32% of cases. The inflammatory process is often preceded by ascites.
Streptococci, enterobacteria, enterococci, and pneumococci are found in ascitic fluid.
Peritonitis is characterized by the appearance of acute pain, which intensifies when trying to change body position. Other symptoms:
- nausea and vomiting;
- a sharp increase in temperature;
- chills;
- heavy sweating;
- loss of appetite;
- increased heart rate;
- increase in leukocytes in the blood;
- pain after pressing on the anterior abdominal wall.
In older people, the severity of symptoms of peritonitis may be insignificant. This is due to a decrease in the body's reactivity.
Treatment of peritonitis depends on the type of pathogen. Until the results of the clinical analysis are obtained, Ampicillin, gentamicin, and third-generation cephalosprin antibiotics are prescribed. The latter should be combined with beta-lactamase inhibitors.
Hepatic coma
This condition is caused by decreased liver function. The cause of coma is decompensation of liver and body functions against the background of cirrhosis. It is also the end stage of encephalopathy.
The main mechanism for the development of hepatic coma is damage to brain cells by toxic substances produced as a result of metabolism. These are phenol, fatty acids, ammonia.
- At the initial stage of coma, the patient's consciousness is clear, and there is a pronounced reaction to pain. The pharyngeal and corneal reflexes are preserved.
- In the shallow stage of hepatic coma, involuntary release of urine and feces, dilated pupils and the appearance of pathological reflexes are observed. The patient makes repeated stereotypical movements - chewing, grasping objects.
- In a deep coma there is no reaction to stimuli. Reflexes are lost and paralysis is observed. Sometimes widespread clonic convulsions occur; in severe cases, breathing stops.
Hepatocellular failure is also manifested by yellowish skin and a liver odor.
Treatment of hepatic coma consists of prescribing vitamin preparations. Detoxification therapy is carried out using plasma substitute drugs. If necessary, antibiotics, diuretics and glucocorticosteroids are administered.
Liver cancer
In cirrhosis, primary cancer most often occurs. The tumor progresses rapidly and has a poor prognosis.
Clinical symptoms appear in the later stages of cancer. Characteristic:
- pain in the right hypochondrium;
- nausea;
- accumulation of intestinal gases;
- loss of appetite;
- weight loss;
- increased fatigue;
- yellowing of the skin;
- nosebleeds;
- dropsy;
- skin itching;
- the appearance of spider veins on the surface of the skin.
As the tumor increases significantly, the pain increases. At the fourth stage, it becomes unbearable, which makes it necessary to administer narcotic painkillers.
The success of liver cancer treatment depends on the stage of development. Radical treatment is organ transplantation.
Diet for liver cirrhosis
Following a diet for liver cirrhosis involves, first of all, avoiding foods that have a high protein content. After all, in patients with liver cirrhosis, the digestion of protein foods is disrupted, and as a result, the intensity of putrefaction processes in the intestines increases. The diet for liver cirrhosis involves periodic fasting days, during which the patient does not eat food containing protein at all. In addition, an important point is to limit the use of table salt with the main meal.
The diet for liver cirrhosis involves the exclusion of all products that contain baking soda and baking powder. You should not eat pickles, bacon, ham, seafood, corned beef, canned food, sausage, sauces with salt, cheeses, or ice cream. To improve the taste of products, you can use spices and lemon juice instead of salt.
The diet for liver cirrhosis allows the consumption of small amounts of dietary meat - rabbit, veal, poultry. You can eat one egg once a day.
Causes of cirrhosis and risk factors
Most people associate liver disease with alcoholism. However, everything that your body cannot break down and use for energy goes straight to the liver for detoxification. Thanks to this, your liver is constantly in need of any help. When you overindulge in alcohol, chemicals, medications, fried foods, and processed or refined foods (such as white flour, regular store-bought dairy, sugar, and low-quality meats), your liver is stressed and unable to function properly.
Risk factors for developing liver cirrhosis:
- History of fatty liver disease.
- Drinking too much alcohol
- Drug use and smoking
- Poor diet (low in vegetables, leafy greens and fruits, high in processed foods, sugar, salt and saturated fat)
- Advanced diabetes mellitus or metabolic syndrome
- Obesity
- High cholesterol and triglycerides
- Chronic viruses and various infections
- High exposure to toxins and pollutants from the environment
- Genetic factors
- Various diseases that damage, destroy and block the bile ducts and interfere with digestion processes
You have two risk factors that you can change quite simply and effectively: eating processed foods (fast food) and drinking alcohol. Various vegetables, including vegetable juices, are very beneficial for your liver because they contain important electrolytes, phytonutrients, enzymes and antioxidants. Vegetables and some fruits (especially citrus fruits like lemons and limes) also help lower acid levels in the body, which creates a friendlier balance and can prevent low potassium levels , which are associated with liver damage.
Plus, all of these plant-based foods contain much-needed dietary fiber, which helps maintain a healthy gastrointestinal tract and gut flora. Regulating your digestive system is critical to liver health, so it is important to achieve daily bowel movements to help eliminate toxins from your body once the liver has eliminated them.
Disease prognosis
Cirrhosis of the liver is incurable unless a liver transplant is performed. With the help of the above drugs you can only maintain a more or less decent quality of life.
How long people with liver cirrhosis live depends on the cause of the disease, the stage at which it was discovered and the complications that had appeared at the time of treatment:
- with the development of ascites they live 3-5 years;
- if gastrointestinal bleeding develops for the first time, from 1/3 to half of people will survive it;
- if hepatic coma develops, this means almost 100% mortality.
There is also a scale that allows you to predict life expectancy. It takes into account test results and the degree of encephalopathy:
| Parameter | Points | ||
| 1 | 2 | 3 | |
| Ascites | No | The abdomen is soft, goes away under the influence of diuretics | The abdomen is tense, its volume does not decrease well when taking diuretics |
| Changes in personality, memory, sleepiness | No | Mild degree | Strongly expressed |
| Total bilirubin | Less than 34 µmol/l | 31-51 µmol/l | More than 51 µmol/l |
| Albumen | 3.5 g/l or more | 2.8-3.5 g/l | Less than 2.8 g/l |
| Prothrombin index | More than 60% | 40-60% | Less than 40% |
| Sum of points | 5-6 | 7-9 | 10-15 |
| How long do they live? | 15-20 years | It is necessary to transplant the liver, but postoperative mortality is 30% | 1-3 years. If a transplant is performed at this stage, the probability of dying after the operation is 82 out of 100 |
Decompensated cirrhosis in women
The stage of decompensation manifests itself by the deterioration of almost all indicators considered vital. Inflammatory liver damage begins to negatively affect neighboring organs, which causes disruptions in the functioning of the central nervous system.
A woman experiences:
- yellowing of the sclera;
- spider veins on the skin of the body;
- severe skin itching;
- hematomas and bruises;
- expansion of internal veins;
- thickening and enlargement of the liver (it can be easily felt with your fingers);
- enlarged spleen;
- frequent vomiting.
Some patients fall into a coma and suffer from hepatic encephalopathy. They may become passive, hallucinate, or speak too slowly and slurred.
Prevention
Liver cirrhosis is a rather long-term process that can be stopped and treated. The main key to success is to go to the doctor on time. However, it is one of those diseases that can be easily avoided by following certain preventive measures, including:
- vaccination against hepatitis B in childhood;
- rational and proper nutrition;
- avoiding starvation and overeating;
- giving up alcohol and smoking to exclude alcoholic cirrhosis and toxic liver damage;
- annual ultrasound and endoscopic examination;
- timely seeking medical attention from a doctor;
- adequate intake of vitamin and mineral complexes;
- strict suppression and treatment of drug addiction.
Preventive measures to prevent viral hepatitis will also help avoid the development of cirrhosis.
What can be done to prevent cirrhosis from getting worse?
To prevent cirrhosis from getting worse, you can do the following:
- Do not drink alcohol or use illegal substances.
- Talk to your doctor before taking: prescription medications;
- prescription and over-the-counter sleeping pills;
- over-the-counter medications, including nonsteroidal anti-inflammatory drugs (NSAIDs) and acetaminophen;
- Dietary supplements, including herbal supplements.
Talk to your doctor about your risk of liver cancer and how often you should get tested.
Classification and stages
Classification is used to determine the severity of the disease and to predict life expectancy in cirrhosis. It is based on several factors that consistently develop at different stages of the disease. Depending on the presence of complications and symptoms, 4 stages of cirrhosis are distinguished, the first of which is considered relatively favorable, the fourth threatens death in a short time.
One of the methods for predicting cirrhosis is the international Child-Pugh classification. The table shows the parameters by which the severity of the patient is assessed and possible indicators (in columns A, B and C). For each parameter a certain number of points is assigned, from 1 to 3. Then they are summed up, and the total number is used to determine the forecast:
- up to 5–6 – one-year survival rate is 100%, two-year survival rate is 85% (class A);
- 7–9 – up to 81% of patients survive in the first year, 57% in the second year;
- 10–10 – during the first year, 45% of patients have a chance of survival, in the second year – up to 35%.
The result can be determined only after all tests have been completed and instrumental research has been carried out. Of primary importance are blood counts, ultrasound data and the body’s response to drug treatment of symptoms.
The photo shows a schematic representation of the generally accepted Child-Pugh classification of liver cirrhosis, which is used by doctors around the world when making a diagnosis
Stage 1
At the initial stage, liver cirrhosis occurs with virtually no clinical signs. Stage 1 is called compensated, since the body uses all possible mechanisms to compensate for liver failure. Symptoms that may indicate liver damage are periodic pain and heaviness in the right hypochondrium. They mainly occur when the diet is violated (eating large amounts of fatty foods), drinking alcohol or exercising. The prognosis is favorable; the patient’s condition can be maintained with proper nutrition and hepatoprotective medications.
Stage 2
The second stage is subcompensated cirrhosis. With the help of medications, the disease can be returned to the compensation stage, but the liver damage is more extensive. The patient is concerned about constant pain in the area of the right hypochondrium, digestive disorders, and there may be a slight accumulation of fluid in the abdominal cavity. Blood tests indicate decreased levels of bilirubin and albumin.
How to avoid occurrence
It is necessary to adhere to basic preventive measures:
- Drink alcohol in reasonable quantities, or better yet, abstain from it altogether.
- If there is a genetic predisposition, regularly check the liver if suspected.
- Stick to proper nutrition.
- Provide protection against hepatitis viruses.
- Maintain body and household hygiene.
- Minimize exposure to toxic substances.
- Prevent cardiovascular pathologies.
Thus, cryptogenic cirrhosis of the liver:
- can be cured completely by removing the diseased organ and performing a donor transplant;
- maintain the condition of the liver with the help of medications, folk remedies and diet;
- prevent with timely and constant prevention. This will provide reliable protection against the disease.
Hepatologist, Gastroenterologist, Proctologist
Alexey has been practicing medicine since 1996. Provides therapy for all diseases of the liver, gall bladder and gastrointestinal tract as a whole. Among them: hepatitis, pancreatitis, duodenal ulcer, colitis.
See what cryptogenic cirrhosis of the liver is in other dictionaries:
Cirrhosis
— liver Cirrhosis of the liver leading to hepatocellular carcinoma (macrodrug) ICD 10 K74.3 K ... Wikipedia
CIRRHOSIS
— (cirrhosis) is an irreversible diffuse process that is characterized by fibrosis, restructuring of the normal architecture and vascular system of the liver with nodular transformation and intrahepatic vascular anastomoses. With cirrhosis, the liver has a color#8230; ... Explanatory dictionary of medicine
Circumcision
- surgical removal of the foreskin of the penis. This operation is usually performed for religious or ethnic reasons, but in some cases it is also necessary for medical reasons, for example, #8230; ... Medical terms
DIFFUSE INTERSTITIAL LUNG DISEASE
- honey Diffuse interstitial lung disease (DILD) is a general term for a group of diseases characterized by diffuse inflammatory infiltration and fibrosis of the small bronchi and alveoli. Etyaodognya. risk factors. Inhalation of various substances.#8230; ... Directory of diseases
Treatment regimen
Liver cirrhosis is a dangerous disease that cannot be completely cured. However, patients are prescribed a set of medications to maintain the condition. A balanced diet is also necessary, the violation of which can quickly lead to an exacerbation of the disease. Therapeutic methods target several factors.
- Cell restoration. For this purpose, drugs from the hepatoprotector group are used. They protect intact hepatocytes and promote their regeneration. There are products on sale of natural and synthetic origin with a similar mechanism of action.
- Normalization of the balance of bile acids. For this purpose, cholic acid compounds are prescribed in tablet form. These can be preparations of ursodeoxycholic acid, chenodeoxycholic acid and combination drugs.
- Strengthening the immune system. Immunomodulators contain components that stimulate the formation of specific protective cells.
- Removal of excess fluid during ascites. To do this, you can take diuretics.
- Additional remedies are aimed at eliminating the cause or symptoms of cirrhosis. Thus, the treatment regimen may include antiviral agents, as well as medications against nausea and vomiting, skin itching and other manifestations.
Ultrasound of the liver is not a particularly informative diagnostic method due to the location of the organ
It is equally important to follow a gentle diet. The diet of a patient with cirrhosis should not contain fatty, fried foods, spices, sauces, semi-finished products, salt and sugar in large quantities. Alcohol should be avoided. The basis of nutrition should be boiled meat and fish, first courses, vegetables and fruits. It is useful to adhere to fractional meals, eating food at least 5-6 times a day in small quantities.
Causes
The reasons that provoke the occurrence of cryptogenic cirrhosis of the liver are not fully understood to date. There are a number of hypotheses and assumptions that the appearance of this pathology is influenced by nutritional factors, as well as autoimmune processes and heredity. True, none of these theories has found final confirmation.
Despite the increasing growth of diagnostic capabilities, in our time, doctors, unfortunately, often fail to establish the causes of the development of cirrhosis of this organ. Very often, cirrhosis can be directly related to a person’s past alcoholism or to the fact that the patient is hiding his addiction to alcohol. True, very often cryptogenic cirrhosis of the liver (ICD 10 code K74.3.) also has a non-alcoholic nature. It is also very difficult to determine the causes of the disease based on symptoms or external signs.
External signs of illness
The development of liver cirrhosis also affects the appearance of the patient. The first thing that catches your eye is excessive thinness. Also talking about what external signs are characteristic of this disease, the following should be highlighted:
- Fingers. They thicken and take on the shape of drumsticks. In addition, changes in the nail plates are observed. They become reddish in color.
- Stomach. On the surface of the abdomen there is an increase in the venous network.
- Telangiectasia. Characterized by the appearance of spider veins on the upper body. As the disease worsens and complications arise, the number of spider veins becomes much larger.
- Angiomas. They are benign formations consisting of lymphatic and blood vessels. With cirrhosis of the liver, they are localized in the area of the corners of the eyes and the edge of the nose.
- Language. It acquires a bright color and increases in size (its swelling is noted).
- Face. A person with cirrhosis of the liver has an unhealthy complexion, the cheekbones become pronounced, the salivary glands enlarge, and the capillaries dilate.
Manifestations of telangiectasia
Classification of cirrhosis
Of the numerous diseases of the body's hepatobiliary system, liver cirrhosis is the most dangerous. This is a pathological process during which an irreversible transformation of the main functioning cells of an organ into auxiliary (connective) tissue occurs. As a result of the degeneration of exocrine iron (liver), it becomes inoperable.
Cirrhotic liver lesions are classified according to the following parameters:
- the nature of the disease;
- changes in structure, shape and structure (organ morphology);
- degree of damage.
The last two parameters evaluate all types of disease, regardless of the cause, including cryptogenic cirrhosis.
Gradation of cirrhosis by etiological types:
- Viral. Develops as a result of viral hepatitis A, B, C.
- Pharmacological or medicinal. Occurs against the background of long-term use or sudden withdrawal of medications.
- Toxic (usually alcoholic). Manifests itself under the systematic influence of alcoholic beverages.
- Congenital. It is formed during the period of embryonic development, can be of a hereditary nature or develop under the influence of teratogenic (external, harmful to the fetus) factors.
- Metabolic and nutritional. The cause is chronic progressive pathologies of the endocrine system (diabetes mellitus), metabolic disorders, and obesity.
- Secondary biliary. It develops due to disruption of the adjacent organs of the hypatobiliary system, in particular, severe pathologies of the biliary tract.
- Autoimmune. Refers to diseases in which the destructive process is caused by improper functioning of the body's own immune system.
- Cryptogenic. With unknown etiology. In general practice, this diagnosis accounts for about 30% of all types of cirrhosis.
Cirrhosis has no age or gender criteria. In the absence of timely medical care, the disease quickly progresses and ends in the death of the patient.
Ultrasound diagnostics
The following manifestations can be recorded as part of an ultrasound examination:
- Change in organ size.
- The presence of an uneven contour of the liver with a round lower edge.
- Lack of homogeneous structure due to the presence of multiple nodes.
The presence of an increased ability to absorb ultrasound indicates an increase in liver density, which is typical for the initial and subcompensated stages of the pathology. In the decompensated stage of the disease, hypoechogenicity is observed, that is, compression of the organ. This feature is directly related to the fact that in the first two stages of the disease, the reflection of the ultrasonic wave comes from dense connective tissues that replace liver cells. At the final stage, this organ atrophies, not fully reflecting ultrasound.
Treatment options
One of the most effective ways to treat cirrhosis of this class is a donor liver transplant. It is this operation that guarantees recovery, but is expensive and requires significant financial investments from the patient. Another difficulty is finding an organ compatible with the diseased body for transplantation. A large number of patients simply do not have time to wait for their turn for a transplant or are unable to pay for the operation, so alternative ways to eliminate the disease are being developed.
Drug treatment methods can contain cryptogenic cirrhosis and prolong the patient’s life. For this use:
- diuretics - used to prevent ascites to remove excess fluid collected in the abdominal cavity. Courses usually consist of short but frequent use of drugs;
- hepatoprotectors - used in long courses;
- useful substances are better absorbed in the form of mono injections;
- solutions with a detoxifying effect - used for progressive intoxication;
- albumin solution - prescribed in courses for the entire period of treatment. Effectively slows down progressive cell inflammation.
In case of rapidly occurring ascites and low effectiveness of drugs, specialists use the so-called drainage of the abdominal cavity. This is a procedure during which a tube is inserted through the abdominal wall into the patient's abdomen under close ultrasound guidance to remove excess fluid. If more than 5 liters have accumulated, the operation is divided into several stages.
Prevention and prognosis
It is impossible to say that liver cirrhosis is curable. However, with the proper selection of medications, maintaining a healthy lifestyle and giving up bad habits, the patient’s life can be extended to 10–15 years or more. The presence of complications in the form of HIV infection or specific forms of viral hepatitis (B or combined) the prognosis is less favorable - up to 2-3 years.
It is impossible to completely guarantee the prevention of the disease. However, there are several recommendations that will reduce the likelihood of its development:
- give up bad habits - alcohol is dangerous for the liver even in small doses;
- exercise caution during any manipulations with blood (injections, in manicure and tattoo parlors) - this is how viral hepatitis is transmitted;
- periodically donate blood for diagnosis - in the early stages the likelihood of recovery is much higher.
Cirrhosis in women occurs as a complication of other liver diseases. This is a complex condition in which the liver tissue is destroyed and cannot perform its function. There are several reasons why cirrhosis occurs, among which one should distinguish between congenital and acquired pathologies. Treatment is aimed at eliminating pain and preserving the functional areas of the organ. If all recommendations are followed and there are no complications, you can live up to 10 years or more with this diagnosis.
Signs of the disease depending on the stage of its development
The symptomatic picture in children and adults with the development of liver cirrhosis is the same. Its intensity and nature directly depend on the stage of development of the disease.
Stage 1
This stage of liver cirrhosis is asymptomatic. It can only be detected through laboratory blood tests. At this stage, billiard, alcoholic and primary cirrhosis is manifested only by hepatocyte failure. This can be corrected by taking special medications. Doctors call this stage of the disease development compensatory. But unfortunately, it is detected very rarely.
Stage 2
This stage of development of cirrhosis is called subcompensated and is characterized by a significant decrease in liver functionality. The patient experiences changes in his condition. He begins to worry about weakness, nausea, itchy skin, etc. A laboratory blood test reveals a significant decrease in albumin, the prothrombin index is at 40.
The prothrombin index should normally be 80–90 units.
Stage 3
At this stage (decompensated) of the development of liver cirrhosis, a critical number of functioning hepatocytes is noted. As a result, renal failure begins to actively progress and an increase in symptoms is observed, which are supplemented by obstructive jaundice and pain. Most often, it is at this stage of cirrhosis that complications begin to develop. Among them is ascites. It is characterized by the accumulation of fluid in the abdominal cavity and an increase in the volume of the abdomen. It is also possible to develop hepatic coma, peritonitis and sepsis. Laboratory tests show a critical decrease in albumin levels and prothrombin index.
Stage 4
This stage of liver cirrhosis is called total. With its development, the functionality of the organ is completely disrupted. A person begins to suffer from constant pain, which is not completely eliminated even when taking strong painkillers. The patient's condition becomes critical and requires constant medical supervision.
It is believed that liver cirrhosis is a disease of alcoholics. But this is far from true. Its development can be diagnosed in both an adult and a small child. Yes, with alcoholism, cirrhosis develops much more often, since constant exposure to ethyl alcohol on the body causes the death of liver cells. But besides alcohol, biliary, toxic, viral, portal or any other type of cirrhosis can also be provoked by:
- viral infections (hepatitis A, B, C, chickenpox, whooping cough, chickenpox, etc.);
- autoimmune diseases;
- oncology;
- chemical and drug poisoning;
- thrombophlebitis;
- heart failure;
- diabetes;
- impaired fat metabolism, etc.
Poor diet can also cause liver cirrhosis.
The causes of liver cirrhosis are varied. And to install them, you will need to undergo a thorough diagnosis. As for the treatment of this disease, it is carried out mainly through the use of special medications and diet therapy.
It is difficult to say how long a person can live after being diagnosed with liver cirrhosis, since everything depends on the severity and degree of development of the disease, whether the patient has complications and his age. But as statistics show, the average life expectancy after diagnosis is approximately 5 years, but this is only if all the doctor’s recommendations are followed.
Childhood Indian cirrhosis
Liver dysfunction in children can occur from an early age, developing quickly and leading to death.
It is observed in children aged 1−3 years, is characterized by lightning-fast rates of development and is predominantly fatal. With this type of cirrhosis, symptoms develop quickly, and the small patient dies within 1 year. A child with illness has a high level of copper in the liver. It is believed that cirrhosis is caused by living conditions, drinking and food consumed by children affected by the disease. But experts are inclined to think that this disease is purely genetic.
Assessment of pathology by morphology and severity
Pathological changes in liver tissues and cells lead to the formation of thin septa (septa). As a result, the nodular portion of the organ, surrounded by septa, dies. Based on the size of the nodes, the morphological stage of gland damage is classified into micronodular, macronodular and mixed. In the first case, the lesions do not exceed 3 mm in size, in the second the nodes reach 5 mm. In the mixed type, both large and small lesions are recognized.
The severity of the disease is classified according to the Child-Turcotte-Pugh assessment method, according to which three classes of disease development are established:
- class A (initial or compensated stage);
- class B (subcompensation stage);
- class C (severe or decompensated stage).
Analysis of pathological changes and assignment of classification to cryptogenic liver damage is carried out according to five parameters, each of which corresponds to a certain number of points. The total score indicates the stage of the disease.
Score table
According to statistics, the survival rate of patients operated on in the compensated stage is 90%. It is possible to extend the life cycle of these patients by an average of 17.5 years. When assigning a disease class B, these figures correspond to 70% and ten years of life. In the stage of decompensation – 18% and no more than three years.
One of the features of cryptogenic cirrhosis is the forced transition from the first stage to the third.
Other signs of illness
Speaking about what symptoms are characteristic of liver cirrhosis, the following should be highlighted:
Ascites in cirrhosis
- Pain in the right side. As the disease progresses, the liver capsule expands, which causes increased pain. It manifests itself as colic. In the case of concomitant hypokinetic dyskinesia, the painful sensations become even more pronounced, constant and are accompanied by a feeling of heaviness in the right side.
- Nausea and vomiting. Attacks of nausea may bother the patient frequently. They become especially pronounced after consuming heavy food and alcohol. Nausea is often accompanied by vomiting. There may be blood in the vomit, which indicates bleeding from the dilated veins of the stomach and esophagus. Also, bile may be present in the vomit, which indicates destruction of the bile ducts and stagnation of bile.
- Loss of body weight. Initially, a person’s appetite worsens. After eating even a small amount of food, he begins to feel full. The patient begins to eat less and less, the processes of digestion and absorption of nutrients are disrupted, and active weight loss occurs. As a rule, when liver cirrhosis reaches the decompensated stage, the patient experiences anorexia. Against the background of exhaustion of the body, other symptoms appear - weakness, drowsiness, etc.
- Muscle tone decreases and muscle atrophy occurs.
- Mechanical jaundice. It occurs against the background of a decrease in the ability of hepatocytes to metabolize bilirubin. At the initial stages of the development of cirrhosis, jaundice is not very pronounced; only a slight yellowing of the sclera of the eyes and mucous membranes is noted. But as the disease develops and the bile ducts are destroyed, jaundice becomes pronounced and is characterized by yellowing of all skin and strengthening of the venous network.
- Xanthelasm. This condition is characterized by the appearance of spots with a lipid component. They are localized mainly in the area of the upper eyelids, but can also appear on other parts of the body.
- Joint pain. Accompanied by swelling, redness and other signs of joint diseases.
- Enlarged spleen. This phenomenon is detected by palpation.
- Nosebleeds. In the early stages of development, the disease occurs rarely, then it is observed almost every day.
The photo shows the external signs of xanthelasma
Carrying out prevention
Since the causes of cryptogenic cirrhosis have not yet been identified, there is no prevention of this disease. It is recommended to follow the following general rules:
- Eat a balanced and regular diet.
- Avoid any contact with people who are sick with viral hepatitis.
- Regularly observe all the rules of personal hygiene (wash your hands, do not eat dirty foods, etc.).
- Do not under any circumstances abuse alcoholic beverages.
- Don't use drugs.
The prognosis for survival of patients suffering from cryptogenic cirrhosis is usually five to ten years after the development of ascites. True, most often these numbers turn out to be somewhat lower, since this disease progresses quickly. Immediately after transplantation, patient survival is about ninety-five percent.
Here is the prognosis for the treatment of liver cirrhosis.