Hippocrates wrote about hemorrhoids, therefore, of course, it is impossible to call this disease an acquisition of the modern way of life. Statistics assure that at least 20% of all people on the planet suffer from this disease, and if we add to this data those patients who do not see a doctor, the numbers will be at least twice as high.
Hemorrhoidal disease does not choose gender, age, status - even infants can get it. But more often the disease affects representatives of both sexes over forty. External hemorrhoids are varicose veins specifically located in the external hemorrhoidal plexus, located under the skin of the perineum next to the dentate line of the rectal canal.
Causes of pathology
In proctology, it is customary to differentiate between external (or subcutaneous) hemorrhoids and internal (or submucosal) hemorrhoids. In the entire structure of pathology, external hemorrhoids account for 35 to 42 percent of cases. The disease affects men more often: they develop hemorrhoids at about the age of 35+.
A common cause of external localization of venous deformation is impaired outflow of venous blood from the choroid plexuses through the so-called cochlear arteries.
This pathology can be explained by the congenital nature of the disease or acquired degeneration of the vein walls. If the outflow is disturbed, the blood stagnates, as a result of which the cavernous bodies expand and hyperplastic deformations begin in them.
If the cavernous bodies expand significantly, the mechanical aspect will work - weakening awaits the longitudinal muscle of the rectum itself. She will simply lose the ability to hold the nodular formations, and they protrude even more subcutaneously in the affected area.
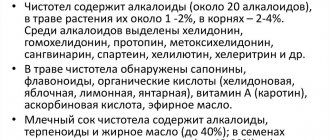
What contributes to this pathology:
- Heredity is the most important point in the development of the disease, but still not determining; with the correct lifestyle of a person, the genetic factor will not be dominant;
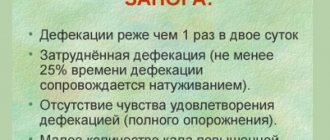
- Constant constipation is a really big problem; the longer you sit on the toilet, the more the blood flow in the pelvis worsens, and the intestinal mucosa becomes irritated;
- Pregnancy and difficult childbirth - hemorrhoids are often diagnosed due to these joyful circumstances, because if the expectant mother experiences symptoms of external hemorrhoids, she needs to be treated without delay;
- A lifestyle with a lack of physical activity also opposes the well-functioning functioning of the body with normal blood circulation;
- Poor nutrition - if you overuse foods that contain spicy, salty, smoked foods, then you also expose your digestive tract to irritation, which only increases the risk of developing hemorrhoids.
Heredity
Constant constipation
Pregnancy
Poor nutrition
It must be said that adherence to alcohol also increases the likelihood of developing vascular deformation.
It is no coincidence that the disease is called a professional diagnosis for loaders, weightlifters, office workers, and drivers.
Etiology
The pathogenesis of the disease is a violation of the outflow of blood from the veins of the external hemorrhoidal plexus against the background of congenital or acquired weakness of the venous walls. This entails stagnation of blood, causing the cavernous bodies to increase in size. With significant expansion of the cones, the weak rectum cannot hold them, so they protrude from the anus.
Clinicians have found that the main risk group is middle-aged people from twenty to fifty years old. A characteristic feature is that this type of hemorrhoids is diagnosed in men several times more often than in women. In females, the peak incidence occurs during pregnancy and breastfeeding.
The following factors can lead to the formation of external hemorrhoids:
- complicated heredity - the risk of such an unpleasant disease increases if a similar disease was diagnosed in close relatives;
- lack of physical activity in a person’s life or, conversely, excessively hard physical work;
- working conditions that require sitting at a desk or standing on your feet most of the time;
- lifting weights by a physically weak person;
- poor nutrition, namely abuse of spicy, fatty and salty foods;
- addiction to addictions, in particular drinking alcohol;
- the period of bearing a child is the main reason for the appearance of such a disease in female representatives. This happens due to compression of the intestines by the enlarged uterus and displacement of internal organs due to the active growth of the fetus;
- Varicose veins;
- chronic constipation;
- childbirth - the appearance of external hemorrhoidal cones is caused by a strong increase in intra-abdominal pressure during the birth of a baby;
- the course of infectious processes in the pelvic area;
- presence of excess body weight;
- formation of tumors or inflammation in the gastrointestinal tract;
- lack of fiber in the diet.
Causes of external hemorrhoids
Symptoms of externally localized hemorrhoids
If the problem is externally localized, the patient can notice it when discomfort appears in the anal ring. This may well be associated with intestinal emptying, but more often it still occurs spontaneously. Soreness can be caused by prolonged sitting, standing, sneezing, or physical activity. Negative sensations often intensify when sneezing or coughing, jumping or running. The intensity of this pain varies - either mild discomfort, or noticeable pain, or even unbearable sensations with thrombosed nodes.
In addition to pain, patients may complain of unbearable itching, burning, and distension in the anal area.
But the first symptom that the patient usually notices is blood:
- With external localization, rectal bleeding occurs less frequently than with internal localization, and it is not as voluminous;
- Blood is found not in feces, but on toilet paper, on underwear, on a towel;
- Blood streaks are sometimes noticed on top of the stool.
There may be no blood at all, but without any signs the disease does not develop. Usually the patient himself is able to feel the minimal formations in the anus area. These formations resemble lumps and are often painful. If the nodules are greatly enlarged, the patient may feel some foreign object in the anus (of course, there is nothing foreign there, but the nodes create such a misleading perception). Sometimes, with severe inflammation of the nodes, the pain increases, as does the temperature.
Stages of the disease
This pathology develops in stages: the disease has three stages in total (unless, of course, it was stopped in time). At the first stage, pain and discomfort are detected - in particular, this is noticeable after a bowel movement or a stormy feast. Upon examination, a dense enlarged nodule will be detected, and it happens that swelling is noted.
At the second stage, the symptoms become stronger - the skin in the area of the node turns red, the swelling also becomes more obvious. Due to the pain, the doctor is unable to perform a digital examination at this stage.
At the third stage of the disease, inflammation spreads to the subcutaneous tissue and neighboring areas. If the proctologist palpates the node, the patient is in great pain, the pain is shooting and sharp. The skin over the inflamed node becomes burgundy with noticeable cyanosis. The doctor probes a dense formation with a surrounding infiltrate, even necrotic zones are identified.
Internal hemorrhoids go through four stages, while external hemorrhoids are often differentiated into the three described above.
Diagnostic measures: external hemorrhoids
This diagnosis can be made by a doctor during a routine initial examination. Near the anus, he fixes small special seals: they sometimes fall out from the outside, very much like lumps. Sometimes they can only be felt under the skin. Bluish accumulations will sometimes be a marker of thrombosis, which already indicates complicated hemorrhoids. By pressing firmly on the knot itself, a person will feel pain. If the problem worsens, swelling forms around the perianal area and the skin turns red.
Diagnostic methods:
- Anoscopy and retromanoscopy - with the help of these devices, an instrumental examination of the rectum is carried out, it allows you to exclude the internal form of hemorrhoids with nodular expansion and subsequent loss of cones;
- Colonoscopy – studies the condition of the colon and provides more complete information than the above methods;
- Irrigoscopy – x-ray examination with a contrast enema;
- Angiography - it is performed when fixing bleeding in order to detect its source.
If the doctor sees a need, he will prescribe the patient an ultrasound of the rectal canal: this examination allows you to visualize deformations of the venous bodies and neighboring veins.
All laboratory methods for diagnosing external hemorrhoids will be uninformative.
The CBC will allow you to evaluate the existing inflammatory signs: the level of ESR and leukocyte count are increasing. If the medical history reaches the point of thrombosis, then the data in the coagulogram may change.
Treatment of external hemorrhoids: general principles
How to treat external hemorrhoids should be determined by a coloproctologist. Conservative methods are purely symptomatic. But medicinal methods do not lead to complete healing. Doctors usually prescribe non-steroidal ointments to the patient, sometimes they are combined with hormonal compounds (if the symptoms are severe). They can relieve swelling, reduce pain and negative sensations. Patients must also adhere to a special diet, change their lifestyle, and stop lifting heavy objects.
If the doctor detects thrombosis, the patient will have to take anticoagulants. If thrombosis is detected in a timely manner, thrombolytics will give results. But if such a program does not produce results, then the blood clot will have to be removed surgically. The doctor will cut the nodule with a scalpel and remove the blood clot. This manipulation is considered minimally invasive; there is no need for inpatient treatment.
Treatment with folk remedies
Many people ask how to cure external hemorrhoids with folk remedies. Before using traditional medicine methods, it is worth remembering that folk remedies can only be used in conjunction with drug treatment. Taking them helps relieve pain and reduce inflammation. The most effective are decoctions of sage, potato juice, onion peels and propolis, from which baths are prepared. Remember that folk remedies in the treatment of hemorrhoids are purely complementary and cannot replace drug therapy.
Ointments for external hemorrhoids
One of the remedies for external hemorrhoids is ointments. These are medications based on synthetic and natural fats. Ointments heal wounds quite quickly, stop bleeding, relieve swelling and create a special protective film on the skin. The remedies come with different effects - they relieve pain, regenerate, and relieve inflammation.
Popular ointments for external hemorrhoids:
- Levomekol. This is a cheap ointment with the antibiotic chloramphenicol, which actively helps with various types of inflammation. It also treats deep cracks, reduces swelling, and prevents suppuration. The product is used for both rubbing and applications. There are few contraindications for this treatment. Apply the ointment in five-day courses at intervals.
- Vishnevsky ointment. This is a simple natural medicine based on xeroform, birch tar and regular castor oil. It quickly heals abrasions and wounds, disinfects and may be known for its anti-inflammatory properties. The ointment will heal if you use it in the form of compresses: the composition is applied to the inflamed bumps, covering the affected area with plastic film. The compress usually lasts 2-3 hours, or is left on all night.
- Heparin ointment. This medication is relevant for severe swelling. It prevents inflammation from developing and also helps with internally localized hemorrhoids. The composition is rubbed into the anus, but it is not injected inside. The course of therapy is one and a half to two weeks.
- Hepatrombin G. This ointment is made from heparin and prednisolone. It allows you to reduce the diameter of protruding nodes. The ointment tones the blood vessels, makes their walls stronger, and improves blood flow. It reduces pain and prevents inflammation and microtraumas from forming. The drug is usually rubbed into the skin itself and into palpable bumps.
The drug should not be used if the patient has serious gastrointestinal pathologies.
Ointment is not the only remedy that can be used to treat external hemorrhoids. This is a local medicine, the components of which do not enter the systemic circulation. Therefore, ointments are often prescribed to pregnant women and those patients who cannot, for example, take pills. And they, by the way, also participate in the symptomatic correction of the condition of external hemorrhoids.
Effective prevention
If the doctor has identified external signs of hemorrhoids, treatment at home should begin with normalizing digestion.
You should avoid constipation, prolonged sitting in the toilet, and avoid spicy and fried foods. If the disease occurs due to a sedentary lifestyle, then you need to change your lifestyle.
Simple exercises to improve blood circulation can eliminate inflammation in the anus
And don’t forget about physical activity and gymnastic exercises.
Many people constantly put off visiting the doctor. Often due to the sensitivity of the problem or lack of understanding of the seriousness of the situation. Someone is hindered by lack of knowledge! For example, people are sure that hemorrhoids do not occur at a young age. This attitude towards yourself is very dangerous! One day you may discover that the disease not only arose, but has already developed with complications. Timely measures will help avoid such situations.
THERE ARE CONTRAINDICATIONS CONSULTATION WITH YOUR DOCTOR IS REQUIRED
Author of the article Alexey Alexandrovich Egorov, proctologist
- Nadia
Can anyone tell me a good remedy for external hemorrhoids? I used Fleming's ointment before. Now I can’t find it, is there something similar?
- Dinara
My external nodes are thickened, but do not come out. An exacerbation occurs more often in the fall, itching and itching. I take a course of Detralex and use Posterizan ointment, which seems to help. I forget about the problem for a year.
- Catherine
Fleming's ointment is very good, I bought it at the pharmacy and had it delivered to order.
Write your opinion
Pills and external hemorrhoids
The individual regimen includes tablets or capsules taken orally. These medications optimize blood flow, they have a preventative effect on inflammation and the growth of cones. The tablets are well compatible with local pharmaceuticals.
Doctors often prescribe to patients:
- Detralex. These tablets improve the condition of the vascular network and prevent its deformation. The product works gently, but also effectively. It is used at different stages of the disease. After a two-week course, the external hemorrhoidal nodule decreases slightly (and sometimes significantly). But such tablets should not be taken by people with diabetes, autoimmune diseases, or those with individual intolerance.
- Diclofenac. The product has a pronounced analgesic effect, reduces fever, and reduces inflammation. Tablets should not be taken if you have diseases of the digestive system or malignant tumors.
- Lachesis. This is a well-known homeopathic drug, which, no matter how scary it may sound, is based on rattlesnake extract. It effectively relieves inflammation and swelling, relieves fever, relieves pain and heals wounds. The patient uses 6-7 granules per day, dissolving them until dissolved. The course lasts about 3 weeks.
Detralex
Diclofenac
Lachesis
In the treatment of external hemorrhoids, suppositories are also effective.
More often they are still taken for the treatment of internal nodes, but in the external course of the disease they are also useful. The fact is that when dissolved in the rectum, fat-containing components leak from the anus and have a positive effect on the skin around it and, of course, on protruding lumps. To heal wounds, Prostopin suppositories (with honey and wax), as well as Olestezin suppositories (with sea buckthorn oil), may be suitable for the patient.
Treatment methods at home
Conservative treatment of uncomplicated external hemorrhoids can be done at home. It is carried out for the purpose of:
- reducing unpleasant symptoms;
- improving quality of life;
- prevention of exacerbations.
To carry out such therapy, the following are used:
- medicines;
- traditional methods;
- dietary nutrition;
- lifestyle correction;
- physiotherapy.
It is strictly prohibited:
- self-medication;
- heating of nodes;
- great physical activity.
Drugs
Pharmaceutical agents for the treatment of external varicose veins exist in the form of:
- ointment, cream, gel;
- pills;
- capsules;
- solution.
Suppositories are used to treat internal hemorrhoids.
Regardless of the volume of therapy, any medication for local use or general effects must be prescribed by a doctor. Self-medication is unacceptable for many reasons. Only a specialist will prescribe the complex of medications required in each individual case, taking into account the patient’s condition, existing chronic diseases, and side effects.
To quickly relieve inflammation, accompanying swelling, pain, as well as unpleasant symptoms such as itching and burning, topical agents are most often used:
- anti-inflammatory (NSAIDs and GCS);
- antithrombotics;
- anesthetics;
- painkillers;
- phlebotonics;
- enhancing regeneration.
Any local medicine is used in a course of 7-10 days, the duration and frequency of use is determined by the doctor. Usually used 2-3 times a day. The choice of local drug is made taking into account the main symptom of hemorrhoids.
Aurobin ointment has a good anti-inflammatory and analgesic effect. It consists of 4 components:
- prednisolone (GCS) is a steroid drug, quickly relieves inflammation, swelling, pain, has a number of contraindications, like any steroid drug;
- lidocaine is a local anesthetic that has an analgesic effect and reduces inflammation;
- triclosan is an antimicrobial drug;
- dexpanthenol is a reparant.
Is it possible to quickly cure external hemorrhoids?
Patients wonder how long it takes to treat external hemorrhoids. In fact, a quick solution to the problem only involves surgery. But if for some reason you have not yet decided on a radical intervention, in some cases the patient is given injections with anesthetics. If the patient is given an injection of novocaine or lidocaine, the acute attack will be stopped quickly.
In case of extensive inflammation, the patient will be recommended antibacterial therapy. But these measures do not answer the question of how to cure external hemorrhoids, they only help to urgently relieve symptoms. Nevertheless, symptomatic treatment works, as they say, for the time being. We will have to decide on drastic measures to correct the situation.
Why are hemorrhoids dangerous?
Can prolapse of nodes during hemorrhoids be dangerous? Today there are many ways to remove fallen cones. It is good to undertake treatment as quickly as possible, as serious complications may occur. Are external hemorrhoids dangerous? Yes, but the danger is this:
- Bleeding.
- Thrombosis of hemorrhoidal veins.
- Paraproctitis is purulent inflammation.
External hemorrhoids are a serious disease that brings terrible discomfort to the patient. If left untreated, it can lead to complications.
If conservative therapy does not give a positive result, then the patient is prescribed surgery. This is the only way to get rid of hemorrhoids forever.
Minimally invasive technologies for node removal
These techniques can be called non-surgical treatment. Classic surgery involves anesthesia, an operating table and long recovery. But minimally invasive techniques are comparable to going to the dentist. Local anesthesia is not always needed, the procedure does not take much time, and the patient recovers quickly.
Features of such mini-operations:
- They are done for minor damage to the tissues surrounding the nodes;
- The whole action takes no more than 30-35 minutes;
- Local anesthesia is possible, but it is not always necessary;
- Patients do not experience pain and find themselves at home literally a couple of hours after the mini-surgery;
- After such an intervention, the threat of scarring and deformation of the mucous tissue structures of the rectum is extremely small;
- The techniques have few limitations;
- Such techniques operate at stages 1-3 of the disease.
How to remove external hemorrhoids is decided by the doctor - he is the one who chooses the method of therapeutic correction. One of these methods is laser coagulation.
Forms of the disease
There are several types of external hemorrhoids. In clinical practice, a classification is most often used that distinguishes 2 forms of this pathology: acute and chronic. However, experienced proctologists believe that the sudden expansion of the veins of the hemorrhoidal node and their loss from the anal canal cavity is only the first symptom of a previously undetected disease.
According to the nature of the course, external hemorrhoids are classified into complicated and typical. In addition, there are isolated and combined forms of the disease (when the pathological process affects not only external, but also internal hemorrhoids).
Opinion of proctologists: how best to remove external nodules
Many patients are really surprised that suppositories and ointments relieve symptoms well, but still do not remove the external bumps themselves. But when they cause you inconvenience, there is only one way to lose them - to remove them surgically.
It is possible to remove external nodes:
- Laser;
- Surgitron (radio wave apparatus);
- Coagulator (special electrosurgical knife);
- Traditional scalpel;
- Surgical scissors.
These options are only a tool, using which doctors excise nodes. Whichever path you choose, after excision, a small wound will form at the site of the node. There will be no stitches, but the wound will still take about three weeks to heal.
Laser in proctological practice
Lasers are actually actively used in proctology. It is able to concentrate thermal energy to the smallest area of influence, and control the depth of this effect. The main method of laser operation is the influence of a high-temperature beam with unique precision on the required object.
What does laser treatment provide:
- Cutting effect - tissues are destroyed exactly in the right place;
- Aseptic burn;
- Scarring;
- Specially defined tissue necrosis with an increase in connective tissue in this area;
- Sealing the required vessels;
- Nerve root decay;
- Sterilization of the damaged area.
We can say that a laser beam in coloproctology is a truly precise modern scalpel; it anesthetizes, stops bleeding, and sterilizes. It also “evaporates” the cellular fluid, which leads to planned cell necrosis.
Removing nodes using Surgitron
This is a safe and very effective method of therapy. The essence of the action of this device lies in the production of high-frequency radio waves. The uniqueness of this technique is that the doctor can actually cut without a knife. Radio wave radiation promotes non-contact excision of tissue with subsequent soldering of blood vessels - this eliminates the threat of bleeding and other difficulties.
Once inside the tissues, radio waves work extremely delicately, without actually causing muscle spasms or touching nerve endings. That's why the pain is small. In the postoperative period, pain can be relieved with analgesics.
When there are indications for treatment with Surgitron:
- External deformed cones that need to be removed;
- Hemorrhoids at different stages;
- Excision of fistulas;
- Therapy of anal fissures;
- Destruction of polyps and non-malignant formations.
The radio wave method does not allow blood loss, because sometimes the vessels are sealed during surgery. This obviously reduces the chance of infection. Therefore, this method of dealing with nodes is often recommended to elderly patients, as well as weakened people, because their tissue regenerative capacity is reduced.
Description of the operation by Surgitron
Radio wave correction is carried out only after the patient undergoes the examination prescribed by the doctor and passes tests. The session itself is carried out on an outpatient basis, but local anesthesia is still used.
No special preliminary preparatory work is needed, i.e. for example, you can eat as usual, there are no significant restrictions. Two hours before the mini-operation, the patient is given a cleansing enema.
Before the session, the patient will be given special disposable underwear with a slit in the place where the doctor will work. During the operation, the patient will be either on the couch or on the operating table in the lateral decubitus position. The doctor injects the anal area with lidocaine or novocaine.
Features of the mini-operation:
- Excision of external nodes is carried out with a radio knife (this is a surgical electrode that emits radio waves of the required range);
- After the excision is completed, the wounds do not need to be sutured, since the device “seals” them, which prevents bleeding;
- During the manipulations, radio waves literally kill all pathogenic bacteria that can cause infection;
- In the postoperative period, the wound heals under a scab - a dense crust, which will reliably protect the wound from external harmful microorganisms.
What is the postoperative period?
The proctologist always emphasizes what should not be done for external hemorrhoids after surgery. Caring for the operated area is not difficult, but it is required. The patient will treat the wound surface daily with a healing ointment (for example, Levomekol). Additionally, he can use ointments and creams that work as regenerants.
It is imperative to ensure proper hygiene of the anorectal area and follow all medical recommendations. You need to care for the wounds daily until they disappear. Don’t expect scars and scars that disfigure the skin - everything will be as before.
In the first two days after the mini-operation, a person is not recommended to sit - only stand or lie down. Also, physical activity is unacceptable for at least a week; you need to give up baths and saunas, even hot baths, for a month. If you do everything correctly, postoperative wounds will heal very quickly and without problems.
Features during pregnancy
During pregnancy, there is a large load on the internal organs, including those localized in the pelvis. During pregnancy, external hemorrhoids may appear due to constant constipation, which can be avoided by drinking more than 2 liters of water per day. Superficial hemorrhoids are diagnosed less frequently during pregnancy if a woman moves a lot and performs special gymnastics. External hemorrhoids during pregnancy can be prevented in the early stages by following the following recommendations:
- do not lift heavy objects;
- maintain hygiene of the anal area and wash after each act of defecation;
- is not constantly in a sitting position;
- make ice compresses for a short time to prevent inflammation;
- carry out complex treatment of the initial stages of hemorrhoids in a timely manner, using suppositories, ointments and other local remedies permitted during pregnancy.
Special cases: external hemorrhoids after childbirth
This phenomenon is diagnosed quite often in young mothers. The women themselves blame themselves for making the wrong attempts, or they say that doctors allowed the disease to develop this way. But hemorrhoids usually develop not during childbirth, but during gestation. The disease goes through several stages, and in the initial stages it is asymptomatic. The reason for the development of the disease will be pregnancy itself - and an enlarged uterus, which puts pressure on the organs, disrupting normal blood flow, can also be the reason. Venous blood stagnates in the pelvis, and this is fraught with inflammation.
Causes of postpartum hemorrhoids:
- Physical inactivity;
- Long-term constipation;
- Hormonal imbalances;
- Excess weight;
- Complicated childbirth with problematic pushing period.
Physical inactivity
Long-term constipation
Excess weight
Complicated childbirth
A young mother cannot ignore the disease. You need to contact a proctologist, indicating special circumstances (breastfeeding). He will select mild medications for symptomatic therapy. But if external hemorrhoids still bother you, your doctor may indicate the need for surgical treatment. And then the young mother resorts to the same minimally invasive techniques as ordinary patients.
If the patient is prescribed antibacterial therapy during the postoperative period, she will have to temporarily stop breastfeeding.