Tablets for tachycardia are prescribed if necessary to stop an attack or to treat a disease. Drugs are divided into 2 groups: natural and synthetic. They have almost the same effect, but the former have fewer contraindications and side effects. Medicines of synthetic origin are more relevant when providing emergency care.
Tablets for tachycardia are natural and synthetic
Basic antiarrhythmic drugs
Tachycardia is a rapid heartbeat when the pulse reaches more than 90 beats/minute. During such an attack, due to the randomness of myocardial contractions, blood flows unevenly into the ventricles of the heart, which provokes ischemia, hypoxia, and the development of heart failure.
The situation is corrected with antiarrhythmic drugs of different pharmacological groups. The treatment regimen depends on the reasons that caused the tachycardia. Only a doctor prescribes medications. Self-medication is unacceptable, as it can lead to serious complications.
Group of myocardiocyte receptor blockers
The essence of the action of antiarrhythmics is the normalization of the transport of potassium, sodium, and calcium ions through cell membranes, which is disrupted during tachycardia. An imbalance in the flow of microelements into and out of the cell affects the speed of electrical impulses through the conduction system of the heart. Its duration and the time required to restore the sinus node are disrupted. Taking these points into account, all drugs for tachycardia are divided into 5 classes, which doctors use to correct different types of rapid heartbeat:
- Sodium channel blockers.
- Beta blockers.
- Potassium channel blockers.
- Calcium channel blockers.
- If-channel blockers.
| Class and individual representatives | Mechanism of action |
| Class I – sodium blockers: A-group: Quinidine, Novocainamide B-group: Lidocaine C-group: Ethacizin, Ethmosin, Propafenone, Flecainide, Allapinin | The essence of the action is to block the transport of sodium ions, which stabilizes the properties of the membrane, slows down excitation, and the heart begins to contract more slowly. The ability of the myocardium to independently generate electrical impulses for muscle contraction is lost |
| Class II - beta blockers: selective (act only on the myocardium): Betaxolol, Propranolol, Atenolol, Metoprolol, Bisoprolol, Egilok, Ritmilen; non-selective (also act on the bronchi and blood vessels): Pindolol, Oxprenolol; Vasodilators: Nebivolol, Labetalol, Carvedilol | The main mechanism is blockade of beta-adrenergic receptors of cardiomyocytes, slow conduction of electrical impulses through the myocardium, and decreased activity of the heart muscle. The point is that adrenaline and norepinephrine do not reach the myocardium, and the heart rate becomes lower. At the same time, the vascular wall relaxes, pressure drops, myocardial oxygen demand decreases, and the heart becomes more resilient. Read more about the mechanism of action of beta blockers |
| Class III - potassium blockers: Amiodarone, Sotalol, Dofetilide, Cordarone | Blockade of potassium transport into the cell inhibits the restoration of the original electrical potential, causing a slowdown in heart rate |
| Class IV - calcium blockers: Diltiazem, Verapamil, Corinfar, Foridon | The main action is to prevent the entry of calcium ions into angiocytes, which leads to their expansion, normalizes blood flow, and slows down the pulse. Read more about the mechanism of action of calcium channel blockers |
| Class V – if-channel blockers: Coraxan is a representative of the newest category of drugs with multi-vector effects, one of which is antiarrhythmic | The main effect is achieved by blocking the channels of the sinus node, which provides a negative chronotropic effect, reduces the frequency of ventricular contractions and myocardial ischemia |
Cardiac glycosides
Drugs from the group of cardiac glycosides are used in the treatment of tachycardia because they have ionotropic properties, that is, they are able to increase the duration of diastole, reducing the pulse. During systole, due to this, the release of blood volume increases, ischemia and hypoxia are stopped. Medicines are prescribed for tachyarrhythmias that accompany manifestations of coronary artery disease.
The most famous representative of cardiac glycosides is Digoxin, tablets of which are prescribed for tachycardia in patients with dystrophic changes in the myocardium. Reception is monitored by ECG.
Drugs in this category include Celanide and Digitalis. In emergency cases, use Strophanthin.
Sedatives
Tablets of the sedative group are included in drugs for the treatment of tachycardia due to their ability to relieve psycho-emotional stress. One of the reasons for rapid heartbeat is precisely psychosomatics.
Sedative drugs can be roughly divided into herbal remedies (Valerian extract, Deprim, Corvalol), synthetic (Afobazol, Adaptol) and combined (Novo-Passit, Persen).
All drugs are used in a complex therapy regimen for tachycardia of any origin. If the stress trigger of the pathology is precisely established, then it can be used as a monomedicine.
Antithrombotic agents
Drugs of the group of anticoagulants and antiplatelet agents are prescribed in case of development of tachycardia against the background of atrial fibrillation (atrial fibrillation). Unbalanced contractions of the myocardium create conditions for the formation of blood clots, which, when released into the bloodstream, can block the main vessels feeding one or another internal organ.
Antithrombotic drugs themselves do not reduce the pulse, but are prescribed to prevent possible complications. These include: Warfarin, Aspirin, Clopidogrel, Pradaxa, Eliquis, Xarelto. The drugs are prescribed by a doctor under the supervision of laboratory blood tests.
Blood thinners
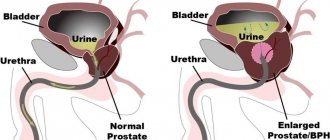
One of the complications of tachycardia is atrial fibrillation, which threatens to develop into atrial fibrillation. With a rapid heartbeat, patients begin to experience erratic contractions, which “knock down” the blood and stimulate the formation of clots. When detached from the arterial wall, a thrombus can clog the vessel, leading to stroke, pulmonary embolism, and internal bleeding.
For chronic hypertension and arrhythmia, doctors recommend taking special medications that improve blood composition:
- Warfarin;
- Pradaxa;
- Xarelto.
https://youtu.be/0RuMF3iIvLM
The listed tablets for the treatment of tachycardia are selected individually and have many side effects. After normalization of the condition, the drugs are changed to safer ones and the dosage is reduced.
Microelements for the heart with tachycardia
Vitamins and minerals have a strong impact on the functioning of the cardiovascular system. Micronutrient deficiency very often causes tachycardia and arrhythmia. Therefore, to prevent the development of such a situation, drugs for tachycardia are used in the form of vitamin and mineral complexes. Minerals are responsible for the functioning of the heart and blood vessels:
- magnesium, which prevent blood clots by normalizing metabolic processes and controlling blood viscosity;
- calcium, which normalizes myocardial contractile function;
- phosphorus – a conductor of nerve impulses;
- selenium, which increases local immunity, providing protection to heart cells and blood vessels;
- potassium that accompanies the generated electrical impulse through the myocardial conduction system.
Specific treatment for increased heart rate
A normal heartbeat is when the rhythm of the heart beats is from sixty to eighty units per minute. Minor fluctuations in these indicators are acceptable in the presence of complex physical loads or psycho-emotional oversaturation, however, in such situations, in a healthy person, the heart rate is restored no later than ten minutes after the start of the precedent, which is considered a standard physiological reaction of the body to external provocative factors.
If an increase in heart rate occurs without provoking reasons, and the precedents are systematic, this indicates the presence of pathological processes in the body of the cardiac or vascular class and requires mandatory medical therapy.
Tachycardia is treated by a cardiologist who, based on the history of the disease, its type and cause of development, the individual characteristics of the human body, and the specific nature of the problem, prescribes effective drugs that can stop attacks. In this case, treatment can be either aimed at eliminating exclusively tachycardia, or complex, as part of the treatment of the pathology provocateur.
The incentive to visit a doctor is often negative symptoms indicating tachycardia, which is expressed by a rapid heart rate, with the parallel occurrence of shortness of breath, discomfort in the chest area, headache or dizziness, which is a serious reason for examining the body and taking appropriate tests. Based on the results of the examination, the doctor decides on the specifics of therapeutic measures.
In situations where examination results indicate irregular heart rhythm, the cardiologist diagnoses “arrhythmia” and prescribes appropriate medications. To treat tachycardia, drugs on a natural or synthetic base can be used, while the former are prescribed mainly for preventive purposes, in the absence of pathological problems of a cardiac nature, the latter are prescribed in the presence of cardiac provocateurs of the disease.
Arrhythmia, in the absence of adequate therapy, can be the primary source of stroke progression, therefore, only the treating doctor should choose a medicine for tachycardia. In order for the drug’s effect on the disease to be as effective as possible, the prescribed drug should not only allow regulating the heart rhythm, but also help eliminate possible associated problems, prevent the formation of blood clots, help stabilize blood pressure and improve the general condition of the patient.
Features of treatment of tachycardia
Attacks of tachycardia lead to deterioration of heart function, high blood pressure, brain hypoxia, and the development of encephalopathy.
Hypoxia is especially dangerous for pregnant women, so timely antiarrhythmic therapy is extremely important to prevent such conditions and correct heart rate. In each specific case, the treatment of tachycardia has its own characteristics.
Emergency help at home
Sometimes it is necessary to urgently stop an attack of tachycardia in order to avoid serious consequences. This happens if palpitations do not occur for the first time, develop against the background of long-existing somatic pathologies, or there is an already developed scheme for relieving the condition.
Stopping a rapid pulse that is gaining momentum at home is not so difficult. The algorithm of actions before the doctors arrive is as follows:
- call an ambulance;
- the patient is laid horizontally, with a pillow under his head so that it is higher than the level of his legs;
- the neck should be in a relaxed state, you should not bend your head too much, as the blood flow to the brain is disrupted;
- provide an influx of fresh air to prevent increasing hypoxia;
- a damp, cool towel is placed on the forehead, which reflexively slows down the pulse;
- free a person from tight accessories so that breathing is free;
- give 30 drops of sedatives dissolved in water to drink: Corvalol, Valocordin, Motherwort;
- you can press on the patient’s eyeballs with his eyes closed – the heart rate slowing reflex will work (take out the contact lenses!);
- you need to ask the person to hold their breath and cough;
- give a tablet for tachycardia, subject to a developed medication regimen.
If the attack passes before the doctors arrive, the doctors take a cardiogram and write out a referral for a consultation with a cardiologist. If the situation does not resolve, the patient is hospitalized (he always has the right to refuse this).
Drugs for tachycardia at normal blood pressure
Tachycardia with normal blood pressure is most often physiological in nature. Heart rate returns to normal when the provoking factor is eliminated: stress, physical activity.
But if the palpitations do not go away after this, the doctor and the patient are faced with the task of finding adequate pills for palpitations that do not lead to hypotension by reducing the pulse. This is especially true for sinus tachycardia, which is treated with beta blockers, which cause a drop in blood pressure.
Until recently, there was no alternative to these drugs. Today there is a new pharmaceutical group that can replace beta blockers in this case. The representative of innovation on the Russian market is Koraksan. Its foreign analogues are Bravadin, Vivaroxan, Raenom, which are used for the treatment of coronary artery disease.
The essence of the action is to slow down the heart rate without hypoxia due to stress or physical activity. In other words, the drug slows down the pulse without affecting blood vessels, and therefore blood pressure.
For hypertension
A difficult option is the selection of medications for tachycardia against the background of arterial hypertension. In this case, the main task is to reduce the tension of the vascular wall, relieve vasospasm, in order to prevent possible rupture with cerebral hemorrhage or ischemia with necrosis in AMI.
Taking such drugs for heart palpitations is lifelong. Although attacks of rapid pulse are rarely combined with an increase in blood pressure, they pose a great danger. They help to cope with it: Diroton, Corinfar, Enap, Verapamil.
For hypotension
Low blood pressure when combined with a rapid pulse threatens the development of cerebral edema. The essence of selecting drugs for tachycardia in this case is to increase vascular tone. The difficulty is that antiarrhythmic drugs, as a rule, reduce blood pressure. When such a scenario develops, doctors use:
- Grandaxin, as a drug that has a sedative effect;
- Mazepam – relieves nervous excitement, anxiety, aggression;
- Phenazepam is an anticonvulsant.
During pregnancy
The body of a pregnant woman experiences excessive stress on the heart and blood vessels. It is enough to remember that at this time, two circulatory systems work as a single whole, the volume of circulating blood doubles.
Tachycardia during pregnancy is a common occurrence. The problem of its relief is that medications, in principle, are not indicated during pregnancy, especially antiarrhythmic drugs that affect blood vessels and the heart.
But frequent heart contractions are dangerous for the fetus, so attacks should be removed. To do this, use anti-tachycardia drugs with the maximum degree of safety:
- Magne B6 (Magnelis B6) – cardiomyocyte regenerant;
- Valerian, Motherwort – herbal-based sedatives;
- Propranolol, Verapamil, which reduce the pulse - from the second trimester, after the formation of the placenta.
During menopause
For elderly patients, in addition to tablets for tachycardia, pine baths, reflexology, and bromine electrophoresis on the collar area are recommended.
Paroxysms are usually relieved with beta-blockers: Trazikor, Propranolol, Atenolol, Metoprolol, Bisoprolol, calcium blockers: Corinfar, Verapamil, Diltiazem.
Sedatives are prescribed in the form of tinctures of peony, hawthorn, motherwort, mineral complexes: Panangin, Asparkam, Doppel Hertz-active, metabolic drugs: Riboxin, for example.
Drugs that can reduce the frequency of contractions without changing blood pressure
Sometimes an attack is diagnosed against the background of stable blood pressure with values within the normal range. Symptoms are characteristic of sinus tachycardia and the initial stage of the pathology. Many drugs that block the production of adrenaline also lower blood pressure. Therefore, the doctor must select a medicine with minimal side effects.
https://youtu.be/bLf7SnB4uBI
A new drug for sinus tachycardia without a sharp decrease in pressure is Ivabradine. Its analogues are: Coraxan, Bravadin, Vivaroxan. The main active ingredient gently slows down the heart rate, relaxes muscles, and does not affect the speed of blood flow. Doctors recommend taking it in small doses daily to prevent oxygen starvation of internal organs.
Important! Many patients must take medications for palpitations throughout their lives to prevent stroke or heart attack.
Risk of complications, side effects
Drugs that slow the heartbeat and restore heart rhythm are prescribed after at least Holter monitoring of ECG and blood pressure. In some cases, a complex manipulation is indicated - transesophageal electrophysiological study (TEPE).
This is necessary in order to avoid serious complications if antiarrhythmics are prescribed not once, to stop an attack, but for life. In this case, it becomes necessary to take into account their interaction with other drugs, otherwise the following may develop:
- arterial thrombosis, causing a heart attack or stroke;
- heart failure (impaired myocardial contractility);
- presyncope and fainting;
- sudden death (possibly due to ventricular tachycardia).
Causes of rapid heartbeat
For a healthy person, it is considered natural to increase the heart rate after a run, exercise, or fear. If the problem appears at rest, doctors warn about tachycardia - a pathological process with a high heartbeat. The diagnosis is made when rates exceed 100 beats per minute, which are accompanied by unpleasant sensations and changes in blood pressure.
Tachycardia is in first place among heart rhythm dysfunctions. It develops when the transmission of impulses from the sinus node is disrupted. In the heart, there is an increase in activity in one of the departments: the ventricles, atria, and bundles of His. The organ works under increased load, the heartbeat and pulse increase.
The main causes of tachycardia:
- chronic anemia;
- hypothyroidism;
- cardiac ischemia;
- chronic failure;
- congenital and acquired defects;
- cardiomyopathy;
- myocarditis.
Factors that increase heart rate are side effects of hormonal or diuretic drugs, alcohol abuse, smoking, stress, heavy physical work.
Drugs that provoke tachycardia
To avoid an accidental attack of tachycardia, you should know everything about the drugs that can provoke it. The list is quite long:
| Name | When to use |
| Anagrelide | Bone marrow diseases |
| Aspirin and Oxycodone | Pain syndrome |
| Chlordiazepoxide | Tranquilizer |
| Clidinium bromide | Relieving bronchospasm |
| Dosulepin | Antidepressant |
| Ephedrine | Vasoconstrictor effect (including nasal drops) |
| Epinephrine | Non-glycoside cardiotonic |
| Epoprostenol | Relieves pulmonary hypertension |
| Moclobemide | Relieves an attack of angina |
| Nalmefene | Treats alcohol addiction |
| Niacin, Lovastatin and Simvastatin | Correctors of lipid metabolism, involved in the treatment of atherosclerosis |
| Nicardipine | Reduces blood pressure |
| Oprelvekin | Treats thrombocytopenia |
| Paliperidone | Antipsychotic drug |
| Phenoxybenzamine | Participates in the treatment of pheochromocytoma |
| Folotin | Antitumor agent |
| Pralidoxime | Used to treat poisoning by organophosphate and carbamate insecticides |
| Voriconazole | Antifungal drug |
Methods for lowering heart rate
You can reduce myocardial strokes using several methods. The selection of certain methods is carried out only by the supervising doctor based on the patient’s age category, the general course of the disease, as well as the blood pressure indicator with increased heartbeats.
Important! It is recommended to carry out procedures to reduce the pulse rate regardless of how often this pathology occurs or whether it develops once. Such actions can be carried out in several ways.
Medicines
To bring the patient’s well-being to normal levels, it is worth taking pills when the pulse is elevated. Dragees are divided into groups. Medicines are taken after consultation with a doctor and prescribing for each patient a certain dosage necessary to achieve a low heart rate.
Natural and synthetic medicines eliminate symptoms that increase heart rate. And antiarrhythmic drugs normalize blood pressure, while a high pulse with high blood pressure will help lower it.
Psychological techniques
In addition to medications that slow down the heartbeat, you can additionally use psychological methods developed specifically for these purposes. Calming programs are used that have a positive effect on the functioning of blood vessels and myocardium, as well as calm the psyche.
As a treatment, it is recommended for patients suffering from increased heartbeat and who do not want to take blood pressure pills to have special consultations with psychotherapists. It is worth developing yourself and attending trainings and group sessions of psychologists.
Literature
- Shubitidze I.Z., Tregubov V.G., Pokrovsky V.M. Comparison of the effectiveness of nebivolol and sotalol in patients with hypertension and ventricular arrhythmias. Eurasian Cardiology Journal. 2019.
- Fomina I.G. Cardiac RI disorders, 2003.
- Bunin Yu.A. Treatment of cardiac tachyarrhythmias. M. 2003.
- Almendral J., Castellanos E., Ortiz M. Update: Arrhythmias (V). Paroxysmal supraventricular tachycardias and preexcitation syndromes. Rev Esp Cardiol (Engl Ed). 2012.
- Camm CF, James CA, Tichnell C. et al. Prevalence of atrial arrhythmias in arrhythmogenic right ventricular dysplasia/cardiomyopathy. Heart Rhythm. 2013
Lyudmila Zhavoronkova
Higher medical education. 30 years of working experience in practical medicine. More about the author
All articles by the author
Emergency help
If a person who is having an attack does not know which pills to treat a high heart rate are recommended to take, then the following emergency measures should be taken to bring the patient’s well-being to a normal level:
- Ambulance doctors must be called;
- it is recommended to induce vomiting;
- wash your face and hands with cool water;
- rub the limbs until red;
- tighten your abdominal area.
It would be a good idea to breathe in aromatic oils that are aimed at calming the excited nervous system or drink weak tea, preferably green.
Thus, various techniques are used to reduce the increased beats of the heart muscle. It is recommended to know the basic recommendations that can help in difficult times before the medical team arrives. In addition, it is always worth having the simplest medicines at home. But if recommended by a doctor, do not refuse treatment.
Blood thinners for heart problems
Separately, it is worth considering blood thinners, which are prescribed to prevent the formation of dangerous blood clots. These medications include antiplatelet agents and anticoagulants, which have the side effect of increasing the risk of bleeding. If a doctor prescribes one of these drugs to a patient, this means that great care must be taken with any injury, surgery, or even dental procedures.
Antiplatelet agents
These drugs work by directly affecting the function of platelets in the blood. Platelets are special cells that help stop bleeding by sticking together and forming a clot.
List of drugs with antiplatelet action:
- clopidogrel (Plavix);
- prasugrel;
- tirofiban (aggrastat);
- dipyridamole.
https://youtu.be/9fu8TSusSds
Anticoagulants
These drugs work by increasing the time it takes for blood to clot. If your doctor prescribes drugs from this group, this means that you will have to take a blood clotting time test several times. Such routine tests are necessary to ensure that the prescribed medications are only beneficial.
List of drugs with anticoagulating effect:
- warfarin;
- dabigatran (pradaxa);
- rivaroxaban (xalerto).
Anticoagulants are prescribed in the form of tablets or injections. The injection form of administration is prescribed for those who need an increased dosage of anticoagulants. Injections are most often prohibited from being given at home, so doctors suggest that the patient come to the outpatient clinic to receive professional medical services. Some nurses conduct mini-courses on self-administration of the drug subcutaneously, and then you can give injections at home.
List of injection anticoagulants:
- enoxaparin (Clexane);
- dalteparin sodium;
- arixtra.
https://youtu.be/ucbtBAiKFJM
So, there are many drugs used to get rid of cardiac problems. But not all heart pills are suitable for treating tachycardia and arrhythmia. Each subtype of drug works differently. The choice of cardiologist will depend on the patient's medical history, side effects, and other medications the patient is currently taking. Only an experienced doctor will be able to find a medicine that will have the best effects for each individual patient.
Antiarrhythmic drugs
Arrhythmia and tachycardia cannot be treated independently. Medicines that help reduce rapid heart rate are used only as prescribed by a doctor. An examination and correct diagnosis are required. It is necessary to identify contraindications to the use of drugs. For each case, it is important to use your own tablets for tachycardia and palpitations. The task of antiarrhythmic drugs when affecting the patient’s body is to restore the rhythm. It can be solved using:
- beta blockers;
- calcium channel inhibitors;
- potassium blockers;
- membrane stabilizing drugs.
Beta blockers
Among tablets for tachycardia and palpitations, beta-blockers occupy a special place, and all thanks to their active effect on the patient’s body. The drugs Egilok, Anaprilin, Ritmilen are taken in a course. In case of illness they help:
- reduce the strength and frequency of heart contractions;
- relax the walls of blood vessels;
- reduce blood pressure;
- reduce oxygen consumption by heart muscle cells;
- improve exercise tolerance;
- reduce the risk of developing arrhythmia.
Calcium channel inhibitors
Drugs used for increased heart rate that prevent calcium from entering the vascular cells, dilating them - calcium channel inhibitors. When using these tablets, blood flow improves, muscle tone decreases, and normal heart rate is restored. The drugs are taken under the strict supervision of a cardiologist, because a sharp decrease in heart rate is possible, which can cause heart failure. Recommended drugs:
Potassium blockers
Pills to lower the pulse - potassium blockers - provide great help with an increased heart rate. They slow down the electrical processes that occur in the heart. Medicines have a slow effect on the body and have many contraindications. Drugs that affect the heartbeat, prescribed by a doctor:
- reduces pulse in case of ventricular tachycardia - Amiodarone;
- for periodic occurrences of pulse disturbances - Sotalol;
- in case of atrial flutter - Dofetilide;
- for gastric and atrial fibrillation - Cordarone.
How to lower blood pressure and pulse
Most drugs used for tachycardia simultaneously lower blood pressure and pulse:
- beta blockers – Nebil, Atenolol;
- calcium antagonists – Isoptin, Verapamil.
If your heart rate periodically increases, you can lower your blood pressure and heart rate with sedatives. The most proven option is a mixture of tinctures of motherwort, mint, hawthorn, and valerian in equal parts. Take 20-30 drops of the mixture with a small amount of water 3-4 times a day.
High heart pressure (systolic, upper reading) is effectively reduced by a Nifedipine tablet placed under the tongue. At the same time, the heart rate slows down. In all cases of high heart rate and blood pressure, a doctor’s consultation is required.
Video: how to reduce heart rate
An increase in pulse most often indicates the development of tachycardia, which can be observed in various conditions, physiological and pathological. Also, this symptom can act as an independent disease, in which case sinus, orthostatic tachycardia, or even atrial fibrillation can be diagnosed.
If normally in an adult the heart rate can be determined from 60 to 90 beats/min, then with tachycardia the heart rate is 100 beats/min and higher.
Depending on the cause of the increase in heart rate, medications may or may not be prescribed at all. In the latter case, it is enough to adjust your lifestyle, diet, and physical activity so that your general condition returns to normal. If you are still prescribed medications to lower your heart rate, they must be taken strictly as prescribed by your doctor to avoid serious complications.
Video: Medications for tachycardia
https://youtu.be/IBJJ3FCifA4
Causes and types of tachycardia
There can be many factors causing pathology. It is divided into two types. Tachycardia is a sign of some diseases, and physiological tachycardia appears for natural reasons - due to excessive stress or strong emotions. If the heartbeat is irregular, this is a manifestation of atrial fibrillation, which is very dangerous to health and can lead to cardiac arrest.
| Types of tachycardia | Peculiarities |
| Sinus | Occurs due to a heavy load on the heart or against the background of its diseases. Usually the disease goes away on its own, and the symptoms are mild. There is no need to treat temporary tachycardia. |
| Paroxysmal | It appears suddenly and stops unexpectedly. These attacks occur due to damage to the heart or when it develops abnormally. During therapy, medications are prescribed - beta blockers, glycosides and maintenance drugs. |
| Chronic | Why does such a rapid heartbeat occur? It occurs against the background of congenital anomalies and diseases. Here, in addition to treatment, the patient must strictly follow a daily routine, proper nutrition, and get enough sleep. He needs to do gymnastics every day, but only moderately, without much physical activity. |
Basic principles of treatment with tablets
Medicines for tachycardia are prescribed depending on the reasons that caused it. Pregnant women should take medications to lower their heart rate with extreme caution. Medicines always have contraindications and can harm the fetus and the health of the expectant mother.
Medications that reduce heart rate have the following positive effects on the body:
- calm and relax;
- strengthen the heart muscle;
- reduce the risk of a recurrent attack;
It is unacceptable to take pills uncontrollably, even natural ones, although they are considered the safest.
You cannot be treated constantly with the same medications to lower your heart rate. The body begins to get used to the active substance, and the drug becomes less effective.
What should you take?
If such a problem occurs, the person often does not have enough air. A pounding heart causes panic and fear.
Important! Tachycardia can occur due to excessive physical exertion, consumption of drinks containing caffeine, excess weight, and other factors.
When tachycardia appears, a person should loosen constricting clothing, open air access to the room, put validol under the tongue and call a doctor.
You can give the patient 40 drops of motherwort or valerian for a calming effect. Their price is low, they are in every home medicine cabinet. If tachycardia appears due to physical factors, then medications for palpitations will not be required. The pulsation will return to normal on its own in a few minutes.
You should not take any medications without consulting a doctor. All medications have their contraindications. For example, calcium and potassium channel blockers are not prescribed in the presence of arterial hypotension, bradycardia and a number of other diseases. Not all drugs are indicated during pregnancy and lactation.
What drugs reduce heart rate?
Heart rate pills are the fastest way to reduce your heart rate. With an increased pulse, they work by affecting the nervous system and dilating blood vessels. The amount of blood passing through the vessels can increase sharply and cause an attack of angina. Therefore, before taking the medicine, you must carefully read the instructions and the list of side effects. The most popular medications to lower heart rate:
- Validol;
- Panangin;
- Lidocaine;
- Nitroglycerine;
- Corvalol;
- Mexiletine;
- valerian extract;
- Diazpam;
- Persen;
- Verapamil.
If you have an increased heart rate, what should you do in this case, besides taking pills?
- Check the room, put on light clothing, try to normalize your breathing.
- You can try stimulating the vagus nerve by inhaling deeply and then exhaling with your nose and mouth closed. This will lead to a decrease in heart rate.
- For 20-30 seconds, lightly press your fingers on your closed eyeballs.
- Lie on a flat surface on your stomach for half an hour.
- Another unusual method is to induce vomiting, which will stimulate the parasympathetic nervous system and cause a decrease in heart rate.
https://youtu.be/qz0xZzpzBZk
If these simple methods do not help, and there are no tablets at hand, you can use folk remedies. Honey and black currant, rosehip tea, and calendula infusion are excellent for lowering heart rate. In addition, you can prepare a decoction of mint, St. John's wort, oregano and valerian. Various soothing teas and herbal infusions will also have a positive effect.
Traditional recipes that reduce heart rate:
- Hawthorn tincture: drink 20 drops mixed with 1/3 glass of water for 3 weeks, 2-3 times a day.
- Motherwort decoction: pour 1 tbsp of boiling water over a glass. l. dry motherwort. Then add 1 tsp to the liquid. honey and 3-4 drops of mint oil. Drink in small sips every day for 1 month.
- Another effective remedy is an infusion of calendula and motherwort: brew 1 tbsp in 200 ml of boiling water. l. herbal collection. Strain and drink after meals for 2-3 weeks.
In emergency situations, when the pulse exceeds 200 beats per minute, you should immediately call an ambulance!
Symptoms of the condition
There are no warning signs of tachycardia. The condition can be detected already at the moment when the number of heart beats becomes quite frequent.
When the myocardial contraction frequency reaches 110 beats/min, a person develops symptoms characteristic of this condition:
- there is a feeling that the heart may jump out of the chest;
- there is headache and dizziness;
- the person often sweats, shortness of breath appears;
- Often a person feels sick;
- it gets dark in the eyes;
- the mouth becomes dry, the skin becomes pale.
Attention! In severe cases, fainting and increased blood pressure may occur. There is a feeling of panic and fear.
An attack of tachycardia, in which the pathological centers of the conduction system are located in the atria, is manifested by sweating, frequent urination, increased temperature, and gas formation.
Sinus tachycardia is characterized by a doubling of the heart rate. The person is excited and cannot sleep at night. At the beginning of a nocturnal episode of a seizure, the person immediately wakes up.
Also, with sinus tachycardia, the patient loses his appetite. After the attack ends, on the contrary, he really wants to eat. Although the heart rate is increased, blood pressure decreases.
How to lower your heart rate without pills using psychological techniques
Without pills or any other medications, you can lower your heart rate if it is caused by nervous tension, excessive coffee or energy drinks; relaxation techniques are used for this:
- concentrate on breathing - count the duration of inhalation and exhalation, inhale for 3 counts and exhale for 4-6 counts (according to sensations), try to use only the stomach without the participation of the chest;
- listen to melodic music;
- lie on your back and alternately relax the muscles of the foot, lower leg, thigh of the right leg, then the left, arms, torso and face;
- look at the candle flame.
Watch the video on how to lower your heart rate:
https://youtu.be/KPY1-Z_R85Q
Prevention of tachycardia (high heart rate)
In order not to have to think about how to quickly reduce a high heart rate and not experience attacks of tachycardia, you should follow some simple rules of a healthy lifestyle:
- Reduce the amount of coffee and tea in your diet. Chicory is a great substitute for coffee.
- Quit cigarettes and alcohol.
- Limit the consumption of salty and fatty foods, as they negatively affect the cardiovascular system.
- Play sports, but do not overdo it with the amount of physical activity. Cardio exercises and walking are suitable for strengthening the heart muscle.
- Lose excess weight by maintaining proper nutrition.
- Try to reduce the number of stressful situations, take soothing herbal infusions.
https://youtu.be/SfxfnxqZqWg
What else can you do to lower your heart rate at home in emergency situations?
If your heart rate suddenly increases, the following actions will help reduce your pulse at home:
- open windows for fresh air;
- unfasten all constricting clothing;
- wash with ice water;
- take 15-20 drops of any tincture that quickly calms down (hawthorn, motherwort), or Corvalol;
- lie on a high pillow, applying a cold compress or ice to your head;
- close your eyes and massage them gently for 3 minutes (10 seconds massage and 10 seconds break), relax;
- cough, take a deep breath, hold your breath and try to “push” it down your stomach;
- perform vagal tests.
Watch the video about ways to lower your heart rate at home:
https://youtu.be/n6U30ejZmb8
If you cannot stop your pulse, dizziness, darkening of the eyes, and rapid heartbeat persist, then it is important to call emergency medical help as quickly as possible. In case of a serious condition, this should be done at the very beginning, before performing any actions.
Causes of the disease
Cardiac causes can provoke the development of this disease:
- myocardial infarction;
- heart failure (congestive, acute);
- cardiosclerosis;
- heart defects;
- bacterial endocarditis;
- angina pectoris occurring in acute form;
- pulmonary embolism;
- pericarditis (exudative, adhesive);
- myocardium (various etiologies);
- carliomyopathy.
In some cases, tachycardia is provoked by non-cardiac causes, which include:
- adrenal insufficiency;
- diabetic ketosis;
- pheochromocytoma (this is a hormonally active tumor);
- various endocrine disorders;
- disruptions in the functioning of the autonomic nervous system;
- withdrawal syndrome (manifests itself in alcoholism);
- low blood sugar is the main cause of the disease;
- certain medications;
- lack of sodium in the blood;
- hypoxia causes the development of this heart disease;
- anemia;
- hypertensive crisis;
- pneumothorax (air accumulates in the pleural cavity);
- various infectious and inflammatory diseases that are accompanied by fever;
- bronchial asthma;
- Allergies can also cause the symptom of increased heart rate.
Tablets "Concor": instructions for use
The main active ingredient is bisoprolol fumarate. Sold in packs of thirty or fifty tablets. Effectively normalizes heartbeat, reduces the myocardium's need for the required amount of oxygen. Improves the course of heart diseases. Most effective for angina pectoris, arterial hypertension and chronic heart failure. It has a number of contraindications, so you should consult your doctor before use. As a rule, it is the specialist who, in each individual case, must prescribe the dosage in which Concor tablets should be taken. Instructions for use recommend taking one tablet in the morning (regardless of meals) with clean water.