Recently, there has been a rejuvenation of cardiovascular disease. Just a few decades ago, heart muscle diseases were considered exclusively among older people. Today, the age group of sick men and women is from 20 to 45 years. Tricuspid valve regurgitation in children and adults is no exception. This heart disease is congenital in nature and can be diagnosed before the birth of a child by performing an ultrasound (ultrasound) on a pregnant woman.
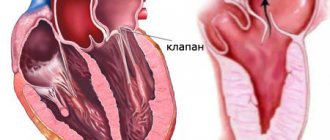
Development mechanism
The essence of the pathological process is the disruption of hemodynamics at the local level and the formation of a persistent anatomical defect.
In the normal state of affairs, blood in the cardiac structures moves strictly in one direction, ending the cycle in the left ventricle and being transported to the aorta, and from there to its branches in a large circle.
The heart is represented by a group of chambers, each separated from the other by valves, which does not allow fluid connective tissue to move in the opposite direction.
The tricuspid structure closes the gap between the right atrium and ventricle. In case of weakness, insufficiency, or defects of the connective tissue, a reverse flow of blood or regurgitation occurs, which is called according to the name of the valve that causes the condition.
The result of the deviation is, firstly, a disruption in the transport of blood in the small circle, and secondly, an insufficient amount of it, which is released into the aorta.
This leads to generalized hemodynamic deviations, tissue hypoxia, and multiple organ failure in the future.
Prognostic assessments
Predictions vary from one case to another. The five-year survival rate is 45%, and in men it is almost one and a half times lower, what is causing this - it is not known exactly.
Young people cope better with the pathological process. During treatment, recovery is observed in every third person; approximately half of those treated have a sufficient quality of life.
Only 3-8% remain in serious condition or become deeply disabled. The ischemic type is easier to treat than the rheumatoid type.
Mitral valve regurgitation is the reverse flow of blood from the left ventricle into the left atrium, due to incomplete closure of its valves. The condition is potentially fatal. Treatment is surgical, urgently or planned. Specialized doctor - cardiologist.
Forms of violation
Typification of the pathological process is carried out on two grounds.
Based on the origin of the anatomical defect, they talk about:
- Primary form. It develops spontaneously, against the background of cardiac problems themselves. Including aortic insufficiency, previous inflammatory, infectious conditions and others.
It is characterized by greater complexity from the point of view of cure and prospects for recovery, since correction requires not only the symptomatic component, but also the acquired defect.
This group also includes congenital factors caused by genetic defects and spontaneous deformations of the tricuspid valve.
- Secondary variety. Against the background of current pathologies of distant organs and systems.
Causes of pathology
The main factor that provokes the development of an abnormal process in the heart valves is valvular insufficiency against the background of heart dilatation. In some cases, the disease occurs against the background of developing rheumatism, endocarditis, or due to the regular use of certain medications.
Causes provoking primary cardiac valve regurgitation:
- The inflammatory process of connective tissues is rheumatism.
- Cardiac endocarditis of an infectious nature (in most cases occurs in people with drug addiction).
- Deflection of the valve leaflet (prolapse).
- A genetic disease of connective tissue is Marfan disease.
- A congenital heart valve defect in which the valve leaflets are displaced or absent altogether.
- Thoracic injury.
- Long-term use of medications.
Causes of secondary regurgitation:
- High pressure in the circulatory system of the lungs (hypertension).
- Ventricular dilatation.
- Ventricular dysfunction.
- Valve pathology.
- Insufficiency of the cardiac ventricles.
- Cardiopathy.
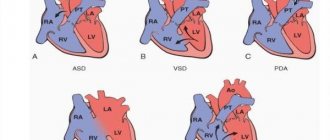
- Congenital defect of the interatrial septum.
- Obstruction of the pulmonary artery.
Degrees of regurgitation
Another basis for classification is the degree of deviation from the norm. Also called stages of the pathological process.
Accordingly, they distinguish:
- Weakly expressed type. 1st degree. The amount of blood returning is not known exactly. The volumes of the jet do not exceed 1 cm in diameter. The intensity of manifestations with minimal tricuspid regurgitation is insignificant or completely absent, which makes early diagnosis a matter of luck. This is the best time to start therapy under the supervision of cardiac surgeons.
- Moderate type. 2nd degree. Characterized by disruption of normal blood flow in a volume of 2 cm, no more. Recovery is carried out surgically. The clinical picture is minimal, characterized by chest pain, shortness of breath during intense physical activity. There is a chance for a complete cure, the likelihood of the formation of persistent cardiac and extracardiac defects is present, but it is not yet great. Even if these occur, the likelihood of a high-quality, long life is maximum.
- Expressed type. 3rd degree. A stream of blood more than 2 cm in diameter. Chronic heart failure of congestive type develops. There are prospects for recovery, but they are not complete, and long-term, lifelong maintenance therapy is required.
- Terminal phase. 4th degree. Surgical assistance does not make much sense, since the heart, kidneys, liver, and brain are significantly changed. Recovery is impossible; palliative care is required to ensure an acceptable quality of life for the short remaining period of life. Death occurs from acute heart failure.
Classifications are used to accurately assess the patient’s condition, prospects for treatment, and determine diagnostic and therapeutic tactics.
Causes and degrees of the disease
This pathology occurs to a small extent in absolutely healthy people. But pronounced, ranging from moderate to severe, is already a rare phenomenon and is provoked by the following reasons:
- congenital and acquired defects of the main “motor” of the body;
- mitral valve prolapse;
- previous endocarditis of an infectious nature;
- previous myocardial infarction;
- injuries.
In this case, several degrees of valvular pathology are distinguished. First-degree mitral regurgitation, in which the backflow appears as a vortex on the valve. In medicine, it is considered practically the norm and does not require correction with medications, but only observation.
In second-degree pathology, the flow penetrates the atrium to a distance not exceeding half its length. With the third degree, this distance increases by more than half, and with the fourth, the flow reaches the back wall, penetrates behind the ear or into the veins of the lung.
In addition, mitral valve regurgitation can be acute or chronic. Acute disease is caused by dysfunction of the papillary muscles or their rupture, acute rheumatic fever, etc. Chronic disease develops for the same reasons. Less commonly, it is caused by atrial myxoma, calcification of the mitral annulus, characteristic of older women, etc.
DETAILS: Acute heart failure in children emergency care
The first degree of regurgitation is considered a physiological condition and does not require treatment. The patient must undergo the necessary examination once a year to avoid the development of complications. The patient must come for control at the time prescribed by the doctor.
Young men are interested in the question: are they recruited into the army with such a problem? In the first degree of valve malfunction, when the refluxed blood flow is no longer than two centimeters, no pathological changes occur. The person is completely healthy and can be taken into the army.
The diagnosis of tricuspid regurgitation must be confirmed by echocardiography, cardiogram, stress test results and other clinical tests.
Persistent arrhythmia, conduction disturbances and severe heart failure lead to dismissal from service.
Patients with this form of the disease are prescribed physical therapy, swimming, race walking, and skiing. Sports involving lifting heavy objects are prohibited. The following procedures lead to improvement of the condition: massage, herbal medicine, acupuncture.
Patients are advised to follow the necessary diet. It is not recommended to overuse fatty, fried and salty foods. Doctors advise keeping weight under control, as quickly gaining kilograms leads to a sharp deterioration in a person’s condition.
Preventive measures are divided into primary and secondary. Primary activities are carried out for healthy people and include:
- Timely diagnosis and adequate treatment of viral and infectious diseases leading to cardiac dysfunction (rheumatism, infectious endocarditis, influenza).
- Fighting foci of infection in the body (chronic tonsillitis, caries).
- Hardening children and raising the overall tone of the body.
Secondary preventive measures are intended for patients with diagnosed regurgitation of the second and third degrees, complicated by progressive valve damage.
Secondary preventive measures:
- Drug therapy necessary to strengthen general tone and reduce the risk of complications (diuretics, nitrates, potassium, glycosides, vitamins, immunomodulators).
- Antibiotic therapy.
- Hardening procedures, physiotherapy, physical therapy.
- Removing foci of infection such as tonsils and caries.
- Special diet.
The menu for patients must include lean meat, nuts, bananas, fresh herbs, vegetables and fruits.
It is recommended to limit store-bought foods, artificial fats, salt, sugar, and fast food products in your diet.
How dangerous is the disease?
Complications arise starting from the third, less often the second stage of the pathological process. Tricuspid valve regurgitation determines the following consequences for health and life:
- Acute heart failure. Disruption of the normal functioning of cardiac structures. It is characterized by a triad of signs: a decrease in blood output, a drop in local and generalized hemodynamics, and arrhythmic processes. It has a short period of development in an acute case; in a latent course, the duration of formation of a full-fledged picture is 2-4 weeks; death occurs as a result of stopping the work of a muscular organ.
- Cardiogenic shock. The condition is lethal in almost 100% of cases. There is no prospect of cure. Even with partial recovery, there is a guarantee of a repeat episode.
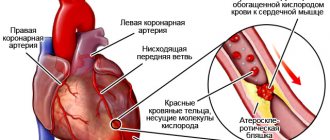
- Heart attack. Myocardial nutritional disturbances, acute tissue necrosis and, as a result, decreased functional activity. Heart failure develops with all its consequences.
- Stroke. Cerebral ischemia.
- Dangerous forms of arrhythmia leading to cardiac arrest.
Minor regurgitation provokes fatal complications in 0.3-2% of cases, often the result of a random coincidence.
Hemodynamically significant forms determine the risk of death in a wide range: from 10 to 70% and higher.
The main cause of death is not regurgitation, but organic defects of the heart and systems developing against its background.
Why is this happening?
The valve apparatus of the heart is designed to maintain blood flow in the desired direction during heart contraction.
But as a result of valve damage (primary regurgitation), or expansion of the heart (secondary regurgitation), reverse outflow develops, leading after some time to heart failure.
The main causes of tricuspid insufficiency are:
- septic endocarditis;
- rheumatic valve disease (most often in combination with aortic and mitral disease);
- cardiomyopathy;
- mechanical injury;
- carcinoid syndrome (with the production of serotonin-like substances from a metabolically active tumor);
- myxomatous deneration;
- Marfan syndrome;
- tricuspid valve prolapse;
- long-term use of certain medications;
- congenital pathologies (Ebstein's anomaly).
In addition, the following conditions act as secondary causes:
- pulmonary hypertension with pancreatic hypertrophy;
- atrial septal defect;
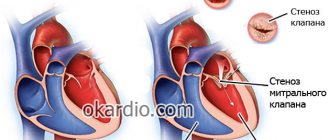
- mitral valve stenosis;
- severe left ventricular failure;
- obstructive changes in the pulmonary artery.
Thus, the causes of tricuspid regurgitation are either diseases associated with damage to the heart muscle or a violation of the valve structure.
Causes
Factors of formation are divided into primary and secondary, according to the main forms of the pathological process.
Primary factors
- Burdened heredity. Leads to the development of tricuspid valve insufficiency. Problems arise during the prenatal period. In this case, there is a genetic predisposition. The exact mechanism, however, is not known.
One thing has been proven: in the presence of a sick parent, children are born with the defect in question and regurgitation in 12-15% of cases. Spontaneous defects of the perinatal period are possible, caused by internal and external factors.
- Spikes in the heart. These are small fibrin strands that disrupt the normal anatomical structure of the organ. They develop as a result of inflammatory processes of any type, especially infectious. This is a kind of protective mechanism, as well as further deposition of calcium salts to isolate the affected area.
- Previous heart attack. It ends with the replacement of functionally active tissues with weak, scarred ones, incapable of contraction, signal transmission, or spontaneous excitation.
If the process affects the tricuspid valve, the following options are possible: its complete fusion, stenosis, or functional failure, immediately leading to severe regurgitation. Recovery is urgent, surgical.
- Inflammatory pathologies of the heart (myocarditis and others). Accompanied by rapid destruction of tissue of cardiac structures. Treatment is urgent, in a hospital, with the use of antibiotics and NSAIDs, as well as steroids and diuretics.
- Rheumatism. Inflammatory pathology of a chronic nature, with frequent relapses and short periods of remission. Therapy is lifelong, using supportive tactics. If necessary, surgical correction of the consequences is performed.
Secondary factors
The secondary pathological process is caused by cardiac problems and extracardiac issues:
- Pulmonary hypertension and the development of specific abnormalities in the anatomical development of the heart. Requires urgent treatment in the early stages, since in the later stages there is no longer any sense. The main risks are smokers, alcoholics, asthmatics and patients with long-term COPD.
- Cardiomyopathy.
- Endocrine pathologies: hyperthyroidism, excess of adrenal hormones, their deficiency, diabetes mellitus and others.
Risk factors
They do not directly cause tricuspid regurgitation, but lead to the onset of the pathological process:
- Long-term smoking.
- Consuming alcohol in immoderate quantities.
- A long period of immobilization, without the possibility of vigorous activity. Development takes a long time, from six months or more.
- Drug addict.
- Excessive use of “dangerous” drugs: glycosides, antiarrhythmics, progestin agents, also hormonal medications, broad-spectrum antibiotics.
- Harmful working conditions affect chemical, hot production, and mines.
The reasons are considered as a whole; a system of development factors is possible.
Types of disease
Tricuspid valve regurgitation can be congenital or acquired. In a child, the phenomenon is registered in the first few months. It happens that the valves work themselves into place. Congenital anomalies are much easier to control, especially if exacerbation of the disease is prevented.
The acquired type of regurgitation develops together with other diseases of the heart or blood vessels.
Based on the reasons that entail the development of the anomaly, the disease can be primary or secondary:
- The primary type of tricuspid valve regurgitation is associated with diseases of the heart muscle. The cause is pulmonary hypertension. This means that blood flows through the pulmonary artery under very high pressure.
- The secondary form is associated directly with the valve, which has a malfunction.
Considering the fact that regurgitation is always directly related to heart valve insufficiency, it can be absolute and functional. Absolute regurgitation occurs when the valve leaflets are affected. It is a congenital form of the disease. The functional form occurs against the background of severe stretching of the valve walls, which is a consequence of diseases or pathological processes in the pulmonary circulatory system, or due to lesions occurring in the tissues of the heart.
Characteristic symptoms
Manifestations depend on the stage of the pathological process. A hemodynamically insignificant variety has no signs at all.
Typical signs in other situations include:
- Liver lesions. They make themselves known in the later stages. They are determined by pain in the right hypochondrium, an increase in the size of the organ, and yellowness of the skin due to excess bilirubin. A gradual formation of insufficiency is possible.
- Abdominal pain of unknown localization. Wandering, radiating to the iliac regions. Acute discomfort is not typical, therefore it is impossible to confuse it with the clinical picture of appendicitis.
- Shortness of breath for no apparent reason. It develops first against the background of intense physical activity, then occurs in a state of complete rest. Significantly reduces quality of life.
- Polyuria. As a result of developing renal failure. At later stages (3-4), with primary damage to the excretory system, it is replaced by a reverse process. Daily diuresis is 500 ml or less.
- Tachycardia. The heart rate reaches 120-150 beats. They are full-fledged, regular. Type - sinus. Less often paroxysmal.
- Weakness, lack of ability to work.
- Feeling of constant cold. The patient freezes because the intensity of peripheral circulation decreases.
- Increased pressure in the veins. Objectively, the symptom is manifested by swelling of the cervical vessels, their intense pulsation, and visible tension. Not only the doctor, but also the patient himself or the people around him can determine the sign. However, blood pressure drops in most cases. Not significant, however, clinical significance is present.
- Swelling of the lower extremities. As a logical continuation of increasing renal failure.
- Breathing problems.
As a result, the patient has a whole range of symptoms from both distant organs and systems, and the cardiac structures themselves. The reason for all the sensations lies in the disruption of blood circulation, both in the large and in the small circle.
Pulmonary valve regurgitation
Damage to the pulmonary valve leaflets can be congenital, manifesting itself in childhood, or acquired as a result of atherosclerosis, syphilitic lesions, or changes in the leaflets due to septic endocarditis. Often, damage to the pulmonary valve with insufficiency and regurgitation occurs with existing pulmonary hypertension, lung diseases, and damage to other heart valves (mitral stenosis).
Minimal regurgitation on the pulmonary valve does not lead to significant hemodynamic disorders, while a significant return of blood to the right ventricle, and then to the atrium, causes hypertrophy and subsequent dilatation (expansion) of the cavities of the right half of the heart. Such changes are manifested by severe heart failure in the systemic circle and venous stagnation.
Pulmonary regurgitation is manifested by all kinds of arrhythmias, shortness of breath, cyanosis, severe edema, accumulation of fluid in the abdominal cavity, changes in the liver up to cirrhosis and other signs. With congenital valve pathology, symptoms of circulatory disorders occur already in early childhood and are often irreversible and severe.
Diagnostics
The examination is carried out under the guidance of a cardiologist, and if the process is proven, the specialized surgeon continues to work. He is also responsible for prescribing treatment.
Scheme of events in the correct order:
- Oral questioning of the patient regarding complaints, their duration, as well as collecting anamnesis. This way the doctor understands the direction of further examination.
- Blood pressure measurement. Usually it is slightly reduced. Heart rate is higher than normal. The rhythm is correct; as it progresses, spontaneous premature beats (extrasystoles) occur.
- Listening to sound (auscultation). A sinus noise of reverse blood flow is detected. Tones can be either normal or dull.
- Daily monitoring. To record cardiac performance indicators over 24 hours in dynamics. It is most often used as the first method, after a routine examination. Provides comprehensive information about the movement of blood pressure and heart rate during the day.
- Electrocardiography. Assessment of the functional state of the heart.
- Echocardiography. Method of visualization of cardiac structures. It is carried out as a matter of priority, since it allows one to detect organic abnormalities on the part of the tricuspid valve.
- MRI or CR (much less often). It is carried out to detail the image of the heart and surrounding tissues.
- Pulmonary artery pressure measurement.
- Load tests. At an early stage, later not used due to significant danger.
The methods are aimed both at establishing the fact of an anatomical defect and at verifying the alleged diagnosis.
Diagnosis of tricuspid regurgitation
To diagnose tricuspid regurgitation, in addition to the history, physical examination and auscultation, the following studies are performed:
- ECG. The dimensions of the right ventricle and atrium, heart rhythm disturbances are determined;
- Phonocardiogram. The presence of systolic murmur is detected;
- Ultrasound of the heart. Signs of compaction of the valve walls, the area of the atrioventricular orifice, and the degree of regurgitation are determined;
- Chest X-ray. The location of the heart and its size, signs of pulmonary hypertension are revealed;
- Catheterization of the heart cavities. The method is based on the introduction of catheters to determine the pressure in the cavities of the heart.
In addition, coronary angiocardiography can be used before surgery. It is based on the introduction of a contrast agent into the vessels and cavities of the heart to assess the movement of blood flow.
Treatment methods
Therapy is carried out under the full supervision of a cardiac surgeon. Methods of exposure depend on the stage of the pathological process.
Grade 1 tricuspid regurgitation is the best time to start therapy. But there are no symptoms yet, identification is incidental (random), and does not pose any difficulties during a targeted search.
At this stage, dynamic observation for 3-5 years is indicated. In the absence of progression, with stagnation of the process, there is no need for treatment. Sometimes patients can live a quality life without knowing about their condition, without major restrictions.
Tricuspid regurgitation of grade 2 and higher is corrected strictly surgically. There are several intervention options.
But before the treatment stage, it is necessary to stabilize the patient’s condition, if there is time for that (planned operations).
Drugs used:
- Antiarrhythmics in the minimum dosage to restore an acceptable heart rate (Amiodarone, Hindin).
- Beta blockers (Metoprolol).
- Glycosides. In order to normalize myocardial contractility.
- Cardioprotectors.
- Anticoagulants. To prevent the formation of blood clots, which cause frequent premature death of patients.
- Diuretics in the treatment of early manifestations of renal conditions.
The duration of the preparatory period varies from 2 to 4 months, possibly more.
By the time of surgery, the rhythm should be stable, correct, blood pressure within the reference value or close to it.
Depending on the stage of the pathological process and the nature of the changes, plasty or prosthetics of the tricuspid valve is indicated. Both methods are generally equivalent.
Correction of pathologies and defects of distant organs is carried out under the supervision of specialized specialists. The list of techniques is wide and is determined based on the severity of the process.
Attention:
The use of folk remedies is impossible. Since the effect of them in case of organic deviation on the part of the cardiac structures is zero.
Changing your lifestyle will also not play a key role. It makes sense to give up smoking, alcohol and drugs. When carrying out severe therapy for third-party pathologies, correction by a treating specialist is recommended.
Therapy tactics
At the initial stage of the pathology, treatment is carried out by a therapist or cardiologist; in the future, a consultation with a cardiac surgeon may be required. Treatment of mitral valve regurgitation is carried out in strict accordance with modern medical and economic standards.
Radical treatment
In severe cases of mitral regurgitation, surgery is not necessary. Restoring the valve leaflets or completely replacing the valve is the main goal of the intervention. It is best to perform surgery before ventricular decompensation occurs. Otherwise, radical treatment will be ineffective.
The main methods of surgical intervention to eliminate regurgitation:
- Valve replacement (prosthetics). Heart valve replacement is indicated in cases of serious structural changes leading to circulatory problems. Prostheses can be mechanical or biological.
- Valve plastic surgery. Reconstruction of the valve allows you to restore all its functions, prevent heart failure, and save the patient’s life. During the operation, plastic structures are used to completely rehabilitate the heart and avoid repeated problems with the valve.
Plastic surgery and prosthetics are performed under general anesthesia using a heart-lung machine. The operation carries a risk of complications, so long-term rehabilitation will be required after it.
Conservative treatment
Minimal regurgitation does not require therapy. It is enough for the patient to monitor his condition by regularly visiting a cardiologist. In the second and third degrees, drug treatment is indicated. The main task is to eliminate the signs and causes that led to valvular regurgitation.
The treatment regimen may include the following groups of drugs:
- beta-blockers are a group of pharmaceuticals with a pronounced ability to inhibit the effect of adrenaline on special receptors, which, when excited, cause stenosis (narrowing) of blood vessels, acceleration of cardiac activity, and an increase in blood pressure indirectly;
- diuretics – remove fluid from the body, help eliminate swelling and reduce the load on the heart;
- antibiotics – stop the growth and spread of pathogens and are prescribed to eliminate infection;
- anticoagulants - inhibit the activity of the blood coagulation system and prevent the formation of blood clots.
Attention! Often taking medications does not bring a positive effect, which patients should be aware of.
Patients with chronic MR are prescribed vasodilators, as well as drugs that reduce the load on the heart. Corticosteroids, non-steroidal anti-inflammatory drugs, immunosuppressants, TNF inhibitors are indicated in the presence of systemic diseases. In chronic conditions, the most commonly used agents are ACE inhibitors and hydralazine.
Forecast
Depends on the stage and nature of therapy.
- At the first stage, the survival rate is 100%, especially if there is no progression of the condition.
- The second is associated with a probability of 85%.
- Third - 45%.
- The fourth or terminal puts an end to the patient, giving no chance. The median is 1-2 years, often even less.
When carrying out complex therapy, it is possible to stabilize the conditions of even the most severe patients, prolonging life for several years.
Favorable prognostic factors:
- Period of youth.
- Absence of somatic pathologies, bad habits, complications after the operation.
- Good family history.
- Response to treatment.
- Reduction of symptoms.
Determining the possible outcome falls on the shoulders of the cardiologist. In order to say anything concrete, you need to at least carry out a full diagnosis.
Features of pediatric regurgitation
Regurgitation of the tricuspid valve in the fetus can be recorded in the early stages of development using ultrasound. In most cases, this pathology is associated with a deviation in the DNA chain chromosomes (Down syndrome). Although a completely healthy child may experience regurgitation. The presence of this phenomenon does not indicate a developmental disorder.
In the absence of other diseases of the cardiovascular system, the function of the valve levels out independently with age. However, if the phenomenon has been registered, it is necessary to regularly visit a cardiologist to monitor the possible development process.
Methods of correction and recovery of the patient
Types of surgical interventions:
applying clips and rings (correction of the shape of the leaflets and the width of the fibrous base of the valve);
- installation of a prosthesis (complete replacement of the mitral valve).
Principles of patient recovery after surgery:
- support of blood rheology (thinning drugs);
- preventing blood clots (antiplatelet agents);
- exclusion of significant physical activity;
- long-term follow-up.
conclusions
Regurgitation in the bicuspid valve occurs due to the inability of its leaflets to close tightly during systole. The danger of reverse blood flow is the expansion of the cavities of the heart and their excessive filling with blood. To support the pumping function, the myocardium hypertrophies compensatoryly. The heart muscle is not adapted for long-term stress of this degree, so decompensation occurs, expressed in characteristic clinical symptoms, the earliest of which is shortness of breath.
The gold standard for diagnosing regurgitation is Doppler ultrasound of the heart. Stages 3 and 4 of mitral regurgitation are subject to surgical treatment.
The following sources of information were used to prepare the material.
The concept of regurgitation refers to the reverse movement of fluid or gases in hollow muscle organs during contractions.
Doctors of many specialties encounter this phenomenon, but cardiologists deal with this problem more often.
Specialists involved in the pathology of the cardiovascular system speak of this phenomenon as the reverse movement of blood from one chamber of the heart to another.
Complications of mitral regurgitation
Complications without treatment
In cases where the patient is not bothered by complaints, and the degree of the defect, determined by ultrasound of the heart, is not severe, the absence of medications or surgical treatment does not affect the hemodynamic state. If the patient comes with active complaints, and the diagnosis of mitral regurgitation is confirmed or its severe degree is diagnosed, the lack of treatment leads to disruption of blood circulation in the body and the functions of the cardiovascular system. Without correction of the work of the heart muscle, complications can develop, including life-threatening ones - cardiogenic shock, pulmonary edema, systemic thromboembolism, paroxysms of atrial fibrillation, also with the risk of blood clots forming and settling in the vessels of the brain, lungs, intestines, heart, and femoral artery. Complications are more rare than with mitral stenosis.
Complications of the operation
As with any operation, there is a certain operational risk when replacing or replacing the mitral valve. Mortality after such operations, according to various authors, reaches 8–20%. The patient may also develop postoperative complications, for example, the formation of blood clots in the cavities of the heart due to the operation of mechanical prostheses, the development of bacterial inflammation on the valve leaflets, including artificial biological ones, the formation of adhesions between the leaflets with the development of narrowing of the valve opening (stenosis). Prevention of the development of complications is the adequate prescription of anticoagulant drugs, antibiotic therapy in the early postoperative period, as well as during various diagnostic and therapeutic measures in other areas of medicine (catheterization of the bladder, extraction - tooth extraction and other dental procedures, gynecological operations, etc.) .
General information about regurgitation
During regurgitation, some volume of biological fluid (blood) returns to the original chamber. The reverse course may be due to various provoking factors. A pathological return occurs when the heart muscle contracts.
The term applies to violations in all four chambers. The degree of deviation is set based on the volume of biological fluid that is returned.
The heart is a hollow muscular organ. It has four full cameras. Consists of 2 atria and the same number of ventricles. Normally, biological fluid moves in one direction.
The mitral valve is located between the left atrium and the ventricle. Consists of several doors. It is he who undergoes changes more often. It is worth noting that the left side of the heart performs a large number of functions, and pathologies affecting the valve between the atrium and the ventricle occur quite often. In this case, the patient may be diagnosed with mitral regurgitation.
The heart consists of four chambers, pathology can affect any of them
Tricuspid regurgitation of 1-2 degrees affects the valve located between the atrium and the ventricle. The pathology is usually secondary. Aortic regurgitation affects valves that have 3 leaflets. They are located at the junction of certain vessels with a hollow muscular organ.
It is important to understand what regurgitation is in cardiology. If there is a lesion, the valve flaps are unable to close tightly. A certain amount of biological fluid returns back.
Minor aortic regurgitation or minor deviation of any other valve is called physiological. Characterized by a small change in blood circulation through the valves. The pathology is not considered dangerous and does not cause discomfort, which means there is no need for therapy.
Tricuspid regurgitation of the 1st degree is quite often diagnosed in extremely thin people. Patients who are tall are also susceptible to deviation. Doctors say that the diagnosis is made in 70 out of 100 applicants.
People who are thin and tall are most susceptible to pathology.
Tricuspid regurgitation of 0 or 1 degree in a child or adult is considered physiological. Accordingly, there is no need for drug treatment.
Mitral valve regurgitation 2nd degree: causes, symptoms and classification
One type of heart defect is mitral valve prolapse. This disease is accompanied by reverse blood flow - rugurgitation.
The essence and classification of the defect
With MVP at the stage of LV systole, the valve leaflets bend into the cavity of the left ventricle.
Normally, at the stage of atrial systole, the mitral valve leaflets are in an open state.
When left ventricular systole occurs, the halves of the valve close, thereby pushing blood from the ventricle into the aorta.
Due to the fact that the valve leaflets are in a state of prolapse, part of the blood returns back to the atrium.
In modern medicine, the classification of RMC according to its severity is practiced:
- 1st degree – mitral regurgitation 1st degree. is considered minor and is the norm. It can be found in both young and old people. The simplest method used for diagnosis is auscultation. As a rule, in this situation the pathology does not require special treatment. It is enough that the patient will be examined by specialists several times throughout the year. This is necessary in order to avoid the possibility of developing concomitant diseases or any complications;
- Grade 2 – moderate MR – is characterized by the development of circulatory disorders, as well as heart contractions. Pathology of this severity can be diagnosed through the use of examination methods such as an electrocardiogram or an electrophysiological examination of the heart and system. When listening to a patient's heart contraction, specialists are able to hear a specific click that is formed while the heart is in the systole phase;
- Grade 3 – regurgitation of this severity is considered the most complex and dangerous. Among the symptoms that may appear in patients are the presence of edema of the upper and lower extremities, an increase in liver volume, and a significant increase in venous pressure. Patients diagnosed with stage 3 cervical cancer. receive group 1 disability.
I would also like to note that 2nd degree MV regurgitation is classified due to its development into the following groups:
- Primary. The main reason for its development is disturbances in the structure of connective tissue, which have a negative impact on the structure of the mitral valve leaflets. These disorders develop during the intrauterine development of the child. As a result of such disturbances, the valve becomes more elastic and pliable.
- Secondary. This defect develops as a result of myocardial dystrophy, which has a rheumatic origin. Often the cause of secondary regurgitation of the 2nd degree is also mechanical damage to the integrity of the chest, which entails a violation of the integrity of the heart.
The most accurate determination of the degree of regurgitation and the causes of its origin will help to choose an effective treatment method.
Causes and consequences
I would also like to note that grade 2 mitral valve regurgitation can be chronic or acute. This is facilitated by the following factors:
- disruption of the functioning or structure of the papillary muscles of the myocardium;
- damage to the endoderm of the heart wall caused by the development of infection (endocarditis);
- increase in left ventricular volume;
- mechanical damage to the mitral valve;
- cardiac ischemia;
- development of rheumatism in the patient, which leads to myocardial damage.
Often, grade 2 MV regurgitation can be diagnosed in a newborn. This is due to the following reasons:
- development of myocardial inflammation;
- proteins accumulate in the area near the heart valve or on the inside of the lining of the heart;
- congenital heart defect.
If second-degree cervical cancer is diagnosed in patients, the likelihood of complications increases:
- atrial fibrillation;
- blood clot formation.
This degree of regurgitation is one of the main reasons for the development of cerebral stroke in those patients aged 40 years or more.
It is also worth noting that changes in the structure of the mitral valve leaflets can become a site for the formation of blood clots (which in turn leads to the development of vascular thromboembolism), an increase in the volume of the cavity of the left atrium, atrial fibrillation, and changes in the structure of blood cells that are responsible for the coagulation process.
With age, the likelihood of complications increases.
In approximately 15–40% of patients, the intensity and frequency of manifestation of pathological symptoms increases with age. In patients, stage 2 RCC transforms into a more significant and dangerous disease of the cardiovascular system.
However, regurgitation stage 2. does not always entail the development of complications. As a rule, this is typical for 60% of cases.
If you notice any symptoms characteristic of stage 2 mitral valve regurgitation, you should immediately contact a specialist for a thorough examination. This is necessary in order to exclude the presence of a more serious concomitant disease or the development of complications.
What is regurgitation? Its types
The heart constantly pumps blood, which enters the vessels and arteries. As you know, the heart consists of two ventricles, two atria and 4 valves (mitral, aortic, tricuspid, pulmonary valve). Valves allow blood to flow in only one direction. If they cease to perform their function, the functioning of the heart is disrupted, which is life-threatening.
Mitral and tricuspid regurgitation are quite common and are sometimes physiological in nature. That is, a person lives with this pathology and does not realize its presence.
The term “regurgitation” itself is not a diagnosis or a separate disease.
This is a condition that occurs against the background of an existing serious disorder. Regurgitation can have several degrees (usually from 0 to 4), each degree having its own level of severity and consequences.
There are 4 types of regurgitation corresponding to the 4 heart valves:
- Mitral. This is a weakening of the mitral valve, located between the left ventricle and the left atrium. This type of regurgitation occurs most often, since it is the left side of the heart that experiences the greatest stress.
- Tricuspid. When the tricuspid valve malfunctions between the right ventricle and the right atrium, tricuspid regurgitation occurs. It is secondary and often associated with serious heart disease.
- Aortic. The aortic valve is located between the aorta and the left ventricle. With pathological dilatation of the aorta, the valve weakens and blood from the aorta flows back into the left ventricle.
- Pulmonary artery regurgitation. The pulmonary valve is located at the border of the pulmonary trunk and the right ventricle. This pathology is often accompanied by various pulmonary diseases.
The type of regurgitation and its stage can be determined using various diagnostic methods. The severity is determined depending on the volume of blood that comes back.
Causes and signs of mitral regurgitation
When the left atrium contracts, the mitral valve opens and blood enters the left ventricle, after which the valve closes to prevent blood from flowing back. When the left ventricle contracts, blood is pushed into the aorta. If the mitral valve does not close completely, some blood flows back into the ventricle, which is called mitral regurgitation.
This type of regurgitation occurs in 70% of people. It occurs to a mild degree even in healthy people. In most cases, this disorder does not have pronounced symptoms, except for a heart murmur, which can only be determined during an ultrasound. Symptoms in the form of fatigue, shortness of breath, and chest pain appear as a result of complications of mitral regurgitation.
Mitral regurgitation can occur for the following reasons:
- Mitral valve prolapse. This is a fairly common heart disease in which the valve leaflets protrude into the atrium. Its causes can be both heredity and inflammatory heart diseases. Symptoms of mitral valve prolapse include dizziness and weakness, chest pain, fainting, and tachycardia.
- Congenital or acquired heart defect. This is a pathological condition in which the valve apparatus is disrupted to one degree or another. Some congenital heart defects may be incompatible with life. Acquired defects can occur as a result of injury or infection.
- Myocardial infarction. During a heart attack, blood flow to the myocardium is disrupted, resulting in necrotic processes. One of the consequences of a heart attack is mitral regurgitation.
- Infectious endocarditis. This is damage to the inner lining of the heart by pathogenic microorganisms. Complications may include valve dysfunction, embolism, and glomerulonephritis.
Mitral regurgitation can range from mild to severe. Its consequences include heart failure and pulmonary hypertension.
Causes and signs of tricuspid regurgitation
With tricuspid regurgitation, the function of the tricuspid valve is disrupted. Most often it is secondary and occurs against the background of an existing disease (usually pulmonary hypertension). There are also congenital and acquired tricuspid regurgitation.
At the initial stages, this pathology does not manifest itself in any way. In rare cases, pulsation of the neck veins appears due to increased blood pressure. If tricuspid regurgitation occurs for a long time, it leads to heart failure and a number of characteristic symptoms: swelling of the legs, weakness, accumulation of fluid in the abdominal cavity, impaired kidney function, shortness of breath.
Also, tricuspid regurgitation leads to disruption of the liver.
There may be several reasons for this disease:
- Pulmonary hypertension. This concept may hide a number of pathologies that are united by increased pressure in the pulmonary artery. In this condition, the load on the right ventricle increases significantly. Symptoms include increased fatigue, shortness of breath, tachycardia, chest pain, and swelling.
- Myocardial infarction. During a heart attack, part of the myocardial tissue is replaced by connective tissue. The functioning of the heart is disrupted, which often affects the condition of the valves. As a rule, the post-infarction state requires long-term rehabilitation.
- Mitral stenosis. With this disease, the walls of the mitral valve narrow or fuse together. As a result, blood cannot pass from one chamber to another. All this leads to the fact that the load on all other valves increases. Left ventricular failure begins.
- Dilatation of the right ventricle. With dilatation, the right ventricle increases in volume. Tricuspid insufficiency can be both a cause and a consequence of this disease.
At stages 1 and 2 of the disease, a person may not realize that he has tricuspid regurgitation. It is most often detected during a preventive examination or already at the stage of complications.
Mitral valve prolapse
Mitral valve prolapse is a bulging, protrusion of one or both leaflets of the mitral valve of the heart into the cavity of the left atrium during contraction of the left ventricle.
Mitral valve prolapse with regurgitation of the 1st degree (MVP) is one of the types of pathology when regurgitation is caused by sagging (prolapse) of the mitral valve leaflets in side of the left atrium in the systole phase. However, grade 1 mitral valve prolapse can occur without regurgitation, which is typical for congenital forms of the pathology.
We suggest you familiarize yourself with: What is the name of a human blood pressure meter • How to cure hypertension
Aortic valve regurgitation
Have you been struggling with CHOLESTEROL for many years without success?
Head of the Institute: “You will be amazed at how easy it is to lower your cholesterol just by taking it every day...
Read more "
Aortic regurgitation is mistakenly taken to be the name of the disease. Some are even trying to find an analogue in the ICD due to lesions of the aortic valves of various natures. Regurgitation is a physical phenomenon caused by the return of fluid flow. When applied to the aorta, it is the reverse flow of blood into the left ventricle. This is the meaning given to the term in functional diagnostics.
If previously experienced doctors could indicate this process only from a subjective point of view (as a result of auscultation and determination of the characteristic noise on the aorta), then with the introduction of ultrasound examination of the heart into practice, it became possible to see the movement of blood in the opposite direction. And the Doppler ultrasound method made it possible to assess the degree of return and connect this diagnostic sign to solving the problem of choosing a treatment method.
Prevalence
Patients with aortic regurgitation are recorded only in functional diagnostic rooms.
Therefore, prevalence can be judged in relation to the number of Doppler-examined patients rather than in relation to the total population. Various degrees and signs of reverse blood flow through the aortic opening are found in 8.5% of examined women and 13% of men. Among all heart defects in adults, chronic aortic regurgitation is detected in every tenth patient. Most often in old age in men.
What anatomical structures are involved in the formation of regurgitation?
The structure of the four chambers of the heart ensures normal filling of the ventricles (blood flows from the atria) and active ejection into the aorta from the left ventricle, and into the pulmonary artery from the right. The valve system between the cavities and main vessels forms a natural barrier to the return flow.
The physiology of valves, their structure, and muscle bundles for tension react to blood pressure and obey nerve impulses that control the functions of the heart. Any violations of the structure and structure contribute to incomplete closure of the valves. The blood, having passed through the hole, is directed back.
The heart has 4 types of valves between:
- atria and ventricles on the left and right;
- left ventricle and aorta;
- right ventricle and pulmonary artery.
Accordingly, depending on the location of the lesion, mitral regurgitation, return through the tricuspid valve, and incompetence of the valves in the pulmonary artery are possible.
Aortic regurgitation seems to be a special case of dysfunction of the valve apparatus.
The mechanism of regurgitation in normal and pathological conditions
Cardiologists identify minor physiological regurgitation, which is possible under normal conditions. For example, 70% of tall adults have incomplete closure of the tricuspid valve, which the person is not aware of. Ultrasound reveals slight swirling flows when the valves are completely closed. This does not affect general blood circulation.
Pathology occurs during inflammatory processes:
- rheumatism,
- infective endocarditis.
The formation of scars after an acute heart attack, against the background of cardiosclerosis, in the area approaching the valve leaflets and threads, leads to breakdown of the necessary tension mechanism and changes the shape of the leaflets. Therefore, they do not completely close.
In a pathological process, an equally significant role is played by the diameter of the outlet, which must be blocked. Significant enlargement due to left ventricular dilatation or hypertrophy prevents the tight junction of the aortic valve leaflets.
Cholesterol will drop to normal! Will help on…
A tricky recipe for cleaning blood vessels from bad cholesterol! 4 drops and all plaques will disappear...
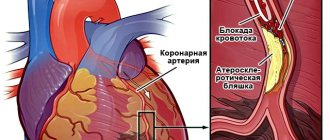
Main valvular causes of aortic regurgitation
The causes of damage to the aortic valves, the diameter of the hole between the left ventricle and the initial part of the aorta, are:
- rheumatic inflammation localized along the line of valve closure - tissue infiltration at the initial stage leads to wrinkling of the valves, forming a hole in the center for the passage of blood during systole into the cavity of the left ventricle;
- bacterial sepsis with damage to the endocardium and aortic arch;
- warty and ulcerative endocarditis in severe forms of infection (typhoid fever, influenza, measles, scarlet fever), pneumonia, cancer intoxication (myxoma) - the valves are completely destroyed;
- congenital defects (formation of two leaflets instead of three) involving the aorta, large ventricular septal defect;
- specific autoimmune processes in the ascending aorta in chronic syphilis, ankylosing spondylitis, rheumatoid polyarthritis;
- hypertension, atherosclerosis - the process of compaction of the valves with the deposition of calcium salts, expansion of the ring due to dilatation of the aorta;
- consequences of myocardial infarction;
- cardiomyopathy;
- chest injuries with rupture of the muscles that contract the valves.
The reasons include complications of treatment of heart diseases using catheter radiofrequency ablation, as well as cases of destruction of the biological valve prosthesis.
Causes associated with aortic damage
The portion of the aortic arch closest to the heart is called the aortic root. It is its structure that influences the “health of the valves” and the width of the gate ring from the left ventricle. Root lesions include:
- age-related or degenerative changes causing dilatation;
- cystic necrosis of the middle layer of the aorta in Marfan syndrome;
- dissection of the aneurysm wall;
- inflammation (aortitis) with syphilis, psoriatic arthritis, ankylosing spondylitis, ulcerative colitis;
- giant cell arteritis;
- malignant hypertension.
Among the reasons, a negative effect of drugs used to reduce appetite in obesity was found.
Consequences of aortic regurgitation
The return of blood to the left ventricle inevitably leads to its expansion and increase in volume. Possible expansion of the mitral annulus and further enlargement of the left atrium.
At the point of contact of the blood flow, “pockets” are formed on the endocardium. The greater the degree of regurgitation, the faster the left ventricular overload develops.
Studies have shown the meaning of heart rate:
- bradycardia increases the volume of return flow and promotes decompensation;
- tachycardia reduces regurgitation and causes greater adaptation.
Forms of aortic regurgitation
It is customary to distinguish between acute and chronic aortic regurgitation.
Features of the acute form
Typical causes of acute aortic regurgitation are:
- injuries;
- dissecting aneurysm;
- infective endocarditis.
The volume of blood entering the left ventricle during diastole increases suddenly. Adaptation mechanisms do not have time to develop. The load on the left side of the heart and myocardial weakness increases sharply. Insufficient blood volume is released into the aorta to support general circulation.
Features of chronic aortic regurgitation
A distinctive feature of the chronic form is sufficient time for the full activation of compensatory mechanisms and adaptation of the left ventricle. This causes a period of compensation for circulatory disorders. Myocardial hypertrophy helps compensate for the reduced output.
When reserve energy reserves are depleted, a stage of decompensation occurs with severe heart failure.
Clinical manifestations
In the acute form of aortic regurgitation, the patient suddenly exhibits signs of cardiogenic shock:
- severe weakness;
- pale skin;
- severe hypotension;
- dyspnea.
For pulmonary edema:
- the patient is suffocating;
- breathing is noisy and hoarse;
- when coughing, foamy sputum mixed with blood is released;
- face, lips, limbs are cyanotic;
- heart sounds are sharply muffled;
- A lot of moist rales are heard in the lungs.
With chronic aortic regurgitation, a long asymptomatic period is possible. Symptoms appear only with the development of myocardial ischemia and severe cardiac decompensation. The patient notes:
- shortness of breath on exertion;
- strong heartbeats;
- extrasystoles;
- angina attacks at night;
- a “cardiac asthma” clinic is possible.
During the examination, the doctor notes:
- shaking the head in rhythm with the pulsation of the heart;
- a typical pulse on the radial artery is a sharp shock wave and an immediate fall;
- trembling when palpating the chest at the base of the heart;
- expansion of the left cardiac border;
- pulsating carotid arteries;
- diastolic murmur on the aorta, along the left edge of the sternum in the third and fourth intercostal spaces, is better heard in a sitting position with a slight bend forward, the first sound is clapping.
Diagnostic methods
Indirect signs of aortic regurgitation are noted in:
- chest x-ray - the left contour of the cardiac shadow is expanded to the side and down, the expansion of the aortic arch is similar to an aneurysm, there are clear signs of enlargement of the left atrium, calcifications may be detected in the aortic arch;
- electrocardiogram - overload of the left chambers of the heart is revealed.
Echocardiographic method
In the diagnosis of regurgitation, echocardiography serves as the main objective method; it allows one to determine the cause, the degree of regurgitation, the sufficiency of compensatory reserves, and circulatory disorders even in the asymptomatic stage of the disease with minimal disturbances. It is recommended for patients in the initial stage annually, and twice a year when clinical symptoms appear.
The calculations take into account the surface area of the patient's body, due to the lack of pronounced expansion of the ventricular chamber in short people.
The most commonly used mode is color Doppler scanning. The sensors are installed in such a way as to measure the area of blood flow at the aortic valves, in the initial part of the aorta, and compare it with the width of the passage. In severe cases, it exceeds 60% of the ring diameter.
In the practice of cardiologists, a division of the return jet into 4 degrees is used in relation to its length to the size and internal formations of the left ventricle:
- 1 - does not extend beyond half the length of the anterior leaflet at the mitral valve;
- 2 - reaches or crosses the gate;
- 3 - the flow value approaches half the length of the ventricle;
- 4 - the jet touches the top.
If information from Doppler sonography is not enough, the following is carried out:
- magnetic resonance imaging;
- radionuclide angiography;
- cardiac catheterization.
Treatment options
Treatment of aortic regurgitation depends entirely on the underlying disease and the completeness of elimination of the causes.
Drug therapy uses drugs that can lower systolic blood pressure and reduce reflux volume.
A group of vasodilators is used (Nifedipine, Hydralazine, ACE inhibitors). They are not indicated for patients with asymptomatic or mild or moderate forms of regurgitation.
Who is indicated for surgical treatment?
The only form of surgery is aortic valve replacement. The operation is indicated for:
- severe form of regurgitation with impaired left ventricular function;
- if the course is asymptomatic, with preserved ventricular function, but pronounced expansion (dilatation).
Forecast
The prognosis for the patient’s life depends on the underlying disease, the degree of regurgitation, and the form. An early mortality rate is typical for the acute development of pathology. In the chronic form, 75% of patients live more than 5 years, and half live 10 years or longer.
In the absence of timely surgical intervention, the development of heart failure is noted in the next 2 years.
Treatment of moderate clinical symptoms is accompanied by positive results in 90% of patients. This reinforces the importance of evaluating and monitoring patients with aortic regurgitation.
Forms of aortic regurgitation
It is customary to distinguish between acute and chronic aortic regurgitation.
Features of the acute form
Typical causes of acute aortic regurgitation are:
- injuries;
- dissecting aneurysm;
- infective endocarditis.
The volume of blood entering the left ventricle during diastole increases suddenly. Adaptation mechanisms do not have time to develop. The load on the left side of the heart and myocardial weakness increases sharply. Insufficient blood volume is released into the aorta to support general circulation.
Features of chronic aortic regurgitation
A distinctive feature of the chronic form is sufficient time for the full activation of compensatory mechanisms and adaptation of the left ventricle. This causes a period of compensation for circulatory disorders. Myocardial hypertrophy helps compensate for the reduced output.
When reserve energy reserves are depleted, a stage of decompensation occurs with severe heart failure.
General manifestations
Patients become apathetic and their thinking productivity decreases. Possible cognitive impairment.
Without proper treatment, the atrium stretches, which leads to an increase in pressure in the pulmonary vein and then the artery.
Chronic heart failure sets in and is accompanied by a host of phenomena. From ascites, fluid accumulation in the abdominal cavity, to liver enlargement, generalized dysfunction of cerebral structures.
Edema and hemoptysis crown the picture. Differential diagnosis is required. Usually, at the stage of the appearance of such symptoms, it does not present any difficulties.
If at least one symptom occurs, you need to consult a doctor for help.
If there is paralysis, paresis or numbness of the limbs, one side of the body, problems with vision, hearing, speech, facial distortions, severe headaches, vertigo, spatial orientation problems, fainting, you need to call an ambulance. Possibly an emergency such as a heart attack or stroke.
Treatment of mitral regurgitation
Treatment of this heart defect involves the prescription of medications and a radical method of curing the defect - surgical correction of the valve.
The following groups of drugs are used in drug treatment:
- to reduce the total peripheral resistance of the vessels into which the enlarged left ventricle has to push blood, ACE inhibitors and beta-blockers are prescribed: perindopril 2 - 4 mg once a day, fosinopril 10 - 40 mg once a day; carvedilol 12.5 – 25 mg once a day, bisoprolol 5 – 10 mg once a day. - to reduce blood flow to the distended right atrium, nitrates are prescribed - nitroglycerin preparations and its analogues: nitrospray under the tongue 1 - 3 doses for attacks of shortness of breath or chest pain, Cardiquet 20 - 40 mg 20 minutes before physical activity in the early stages and daily from one up to five times a day in the later stages (with severe shortness of breath and frequent episodes of pulmonary edema). - to reduce the total volume of circulating blood and, as a result, avoid volume overload of the heart, diuretics (diuretics) are prescribed: indapamide 2.5 mg in the morning, veroshpiron 100 - 200 mg in the morning, etc. - to reduce thrombus formation and increased blood clotting, antiplatelet agents and anticoagulants are prescribed: thrombo Ass 50 – 100 mg at lunch after meals; warfarin 2.5 mg, plavix 75 mg - the dose is calculated individually under strict monitoring of blood coagulation parameters. - in the presence of atrial fibrillation, antiarrhythmic drugs are used to help restore the correct rhythm (in the paroxysmal form) - a polarizing mixture intravenously, amiodarone, procainamide intravenously. For persistent atrial fibrillation, cardiac glycosides (corglycone, strophanthin) and beta-blockers are prescribed. — to prevent repeated rheumatic attacks, as well as during invasive (introducing into body tissues) interventions, antibiotics are used (bicillin, amoxicillin with clavulanic acid, etc.).
The treatment regimen is established individually for each patient by the attending physician.
Surgical treatment methods include valve plasty (suturing valve leaflets, chordae tendineae) and prosthetics.
The figure shows valve replacement with a mechanical prosthesis.
The operation is indicated for the second degree of defect (severe insufficiency) and for the second - third stages of the process (sub- and decompensation). In the stage of severe decompensation, the use of surgical treatment remains controversial due to the severe general condition, and in the terminal stage, surgery is strictly contraindicated.
Combination of mitral and tricuspid insufficiency
Often, mitral and tricuspid regurgitation are diagnosed simultaneously in one patient. After a detailed examination and receipt of test results, the cardiologist will decide on the treatment tactics for such a patient. If valve insufficiency is mild, no treatment may be needed, but you will need to be periodically observed by a cardiologist and undergo the necessary examinations.
If the cause of valve insufficiency is determined, therapeutic treatment will be prescribed aimed at eliminating the provoking disease. In the absence of positive dynamics, surgical treatment of regurgitation is indicated. This usually happens when the disease is severe and severe.
Patients who have undergone surgical treatment of valve insufficiency are usually prescribed indirect anticoagulants.
Diagnostics of the process and detailing of complaints
The disease can only be diagnosed after the patient seeks help. Mitral valve regurgitation of the 1st degree (up to 5 ml) is not clinically manifested. Symptoms occur with more significant hemodynamic disturbances.
Long-term concealment of mitral insufficiency is ensured by thickening of the left ventricular myocardium. However, when the reserves of this mechanism are depleted, the patient’s condition sharply worsens.
There are 5 stages of mitral insufficiency.
| Stage | Complaints | Hemodynamic disorders | Treatment |
| Compensation | None | Clinically insignificant regurgitation, up to 1+ (no more than 5 ml) | Not required |
| Subcompensations | Shortness of breath when walking long distances or running | Regurgitation within 2+ (about 10 ml). Left heart: ventricular hypertrophy, atrial dilatation | Surgical treatment is not indicated |
| Right ventricular decompensation | Breathing problems with minor exercise | Significant regurgitation, 3+. Dilatation of the left ventricle, enlargement of the right sections. | Surgical treatments are recommended |
| Dystrophic | Shortness of breath without external causes, cough, swelling, fatigue | Deterioration of the pumping function of the heart, relative insufficiency of the tricuspid valve | Surgical treatment indicated |
| Terminal | The patient's condition is serious. Hemoptysis, cough, swelling, poorly healing ulcers. | Decompensation of the circulatory system | Treatment not indicated |
The army will not accept for military service a person with regurgitation of the second degree or higher!
Typical complaints with mitral insufficiency:
shortness of breath (initially with significant physical activity, in the terminal stages - on an ongoing basis);
- palpitations (during physical activity);
- acrocyanosis (blue discoloration of fingertips);
- “mitral butterfly” (blue blush on the cheeks);
- cardialgia (pain in the heart of an aching or pressing, sometimes stabbing nature, not necessarily associated with stress);
- swelling in the legs (appears in the afternoon, in the evening, in the initial stages disappears overnight);
- pain in the right hypochondrium (appears as a result of blood stagnation, with pronounced swelling);
- cough (with stagnation of blood in the pulmonary circulation, often unproductive);
- hemoptysis (with decompensation of the patient’s condition).
Hemodynamic disorders can be diagnosed using the following instrumental methods:
- electrocardiography (left ventricular hypertrophy, arrhythmias, after the third stage - right ventricular hypertrophy);
- phonocardiography (the first tone is weakened, a systolic murmur is determined at the apex of the heart);
- echocardiography (enlargement of the heart cavities and thickening of the myocardium, changes in the movements of the interventricular septum, calcifications in the mitral valve leaflets);
- Doppler echocardiography (detection of the return of part of the blood to the atrium during ventricular systole).
Possible complications
The likely consequences are:
- Heart failure. Considered the leader in frequency. The cause of death in patients with mitral regurgitation in 80% of cases is acute suspension of the muscular organ.
- Myocardial infarction. As a result of malnutrition of cardiac structures. If the process continues for a long time, but does not reach a critical mass, insufficiency and dysfunctional disorder are likely.
- Coronary heart disease (CHD).
- Stroke. Acute deviation of blood supply to brain structures.
- Arrhythmias of various kinds. Fibrillation, paired or group extrasystoles.
Symptoms in children
Congenital tricuspid regurgitation in infants in 25% of cases manifests itself as supraventricular tachycardia or atrial fibrillation; severe heart failure may later appear.
In older children, even with minimal exertion, shortness of breath and palpitations appear. The child may complain of heart pain. Dyspeptic disorders (nausea, vomiting, flatulence) and pain or a feeling of heaviness in the right hypochondrium may be observed. If stagnation occurs in the systemic circulation, peripheral edema, ascites, hydrothorax or hepatomegaly appear. All these are very serious conditions.
Consequences of aortic regurgitation
The return of blood to the left ventricle inevitably leads to its expansion and increase in volume. Possible expansion of the mitral annulus and further enlargement of the left atrium.
At the point of contact of the blood flow, “pockets” are formed on the endocardium. The greater the degree of regurgitation, the faster the left ventricular overload develops.
Studies have shown the meaning of heart rate:
- bradycardia increases the volume of return flow and promotes decompensation;
- tachycardia reduces regurgitation and causes greater adaptation.
Lifestyle with mitral regurgitation
The patient must follow the general principles of maintaining a healthy lifestyle, as well as follow the doctor’s recommendations used for many cardiac diseases - avoid alcohol, smoking, fatty, fried, spicy foods; limit the amount of liquid and salt consumed; sleep a lot and walk outdoors more often.
When pregnancy occurs, a woman should be observed by a cardiac surgeon together with an obstetrician and a cardiologist. In the early stages and in cases where the defect is not severe, pregnancy can be maintained, but in case of severe hemodynamic disturbances, it is strictly contraindicated. Delivery will most likely be by caesarean section.
Prevalence
Patients with aortic regurgitation are recorded only in functional diagnostic rooms. Therefore, prevalence can be judged in relation to the number of Doppler-examined patients rather than in relation to the total population.
Various degrees and signs of reverse blood flow through the aortic opening are found in 8.5% of examined women and 13% of men. Among all heart defects in adults, chronic aortic regurgitation is detected in every tenth patient. Most often in old age in men.
Types of pathology
Detection of reverse systolic blood flow in the right half of the heart is possible even in healthy people. Among acquired defects, regurgitation through the tricuspid valve accounts for about 25 percent. According to the mechanism of development, it can be primary or secondary; isolated or combined forms are found.
Sagging of the valve leaflet or its pathological protrusion is most often found after infective endocarditis. Prolapse also appears with a congenital anomaly in the structure of connective tissue, against the background of rheumatism. The sagging part does not allow complete closure of the hole during contraction of the right ventricle; part of the blood passes back into the atrium.
The degree of regurgitation may vary depending on the increase in pressure in the pulmonary artery system.
With a congenital anomaly in the structure or location of the pulmonary artery trunk, increased pressure occurs in the vessels of the lungs. The right ventricle works harder to push blood into the pulmonary bloodstream. At first, its muscle layer thickens (hypertrophy), then, as compensatory capabilities decrease, the cavity expands.
Patients develop relative valve insufficiency with blood regurgitation.
Blood reflux can occur with a normal valve structure due to mitral stenosis. This complication occurs in 90% of patients due to difficulty in the passage of blood from the left atrium. High pressure in this part of the heart inhibits the outflow of blood from the pulmonary veins and causes overflow of the pulmonary circulation. The development of right ventricular failure and weakness of the heart muscle impair the functioning of the tricuspid valve.
Less common than combined heart defects. Leads to insufficient emptying of the right sections and stagnation of blood in the systemic venous network. Overload of the right atrium, and especially the expansion of its cavity, causes a type of rhythm disturbance and is accompanied by a high risk.
There are several types of tricuspid valve insufficiency:
- Absolute or organic failure. The pathology is caused by damage to the valve leaflets, such as valve prolapse (sagging leaflets), due to a congenital disease - connective tissue dysplasia, also causes include rheumatism, infective endocarditis, carcinoid syndrome and others;
- Relative or functional deficiency. Occurs when the valve is stretched due to resistance to the outflow of blood from the right ventricle, with pronounced dilatation of the ventricular cavity caused by high pulmonary hypertension or diffuse myocardial damage.
Based on the severity of reverse blood flow, tricuspid regurgitation is divided into four degrees:
- 1st degree. Barely detectable backflow of blood;
- 2nd degree. Regurgitation is determined at a distance of 2 cm from the tricuspid valve;
- 3rd degree. Reverse flow of blood from the right ventricle is detected at a distance of more than 2 cm from the valve;
- 4th degree. Regurgitation is characterized by a large extent in the cavity of the right atrium.
The severity of blood return is determined using echocardiographic examination.
Features of treatment
Treatment of mitral or any other regurgitation of the 1st degree is not carried out. The patient is registered with a cardiologist. He must undergo regular diagnostics to prevent the development of complications. In addition, you need to give up all bad habits.
With 3-4 degrees of pathology, the patient may be referred for prosthetics. The operation is considered difficult and often provokes the development of complications.
There is no specific set of medications for the treatment of regurgitation. Medicines are selected based on the main diagnosis.
If the patient has no complaints, it is enough to follow the doctor’s general recommendations. They consist of moderate physical activity and maintaining a healthy lifestyle.
You can learn in detail about the causes and mechanisms of development of mitral regurgitation by watching the video below:
Heart valve regurgitation: symptoms, degrees, diagnosis, treatment
The term “regurgitation” is quite often used by doctors of various specialties - cardiologists, therapists, functional diagnosticians. Many patients have heard it more than once, but have little idea what it means and what it threatens. Should we be afraid of having regurgitation and how to treat it, what consequences to expect and how to identify it? Let's try to find out these and many other questions.
Regurgitation is nothing more than the reverse flow of blood from one chamber of the heart to another. In other words, during contraction of the heart muscle, a certain volume of blood, for various reasons, returns to the cavity of the heart from which it came. Regurgitation is not an independent disease and therefore is not considered a diagnosis, but it characterizes other pathological conditions and changes (heart defects, for example).
Since blood continuously moves from one part of the heart to another, coming from the vessels of the lungs and leaving for the systemic circulation, the term “regurgitation” applies to all four valves on which reverse flow may occur. Depending on the volume of blood that returns, it is customary to distinguish the degrees of regurgitation that determine the clinical manifestations of this phenomenon.
A detailed description of regurgitation, identification of its degrees and detection in a large number of people became possible with the use of ultrasound examination of the heart (echocardiography), although the concept itself has been known for quite a long time. Listening to the heart provides subjective information, and therefore does not allow one to judge the severity of the return of blood, while the presence of regurgitation is not in doubt except in severe cases. The use of ultrasound with Doppler makes it possible to see in real time the contractions of the heart, how the valve flaps move and where the blood stream rushes.
Briefly about anatomy...
In order to better understand the essence of regurgitation, it is necessary to recall some aspects of the structure of the heart, which most of us conveniently forgot, having once studied in biology lessons at school.
The heart is a hollow muscular organ with four chambers (two atria and two ventricles). Between the chambers of the heart and the vascular bed there are valves that function as “gates”, allowing blood to pass in only one direction. This mechanism ensures adequate blood flow from one circle to another due to the rhythmic contraction of the heart muscle, which pushes blood inside the heart and into the vessels.
The mitral valve is located between the left atrium and the ventricle and consists of two leaflets. Since the left half of the heart is the most functionally burdened, works under heavy load and under high pressure, it is often here that various malfunctions and pathological changes occur, and the mitral valve is often involved in this process.
The tricuspid, or tricuspid, valve lies on the path from the right atrium to the right ventricle. It is already clear from its name that anatomically it consists of three interlocking valves. Most often, its damage is secondary in nature to an existing pathology of the left side of the heart.
The valves of the pulmonary artery and aorta each have three valves and are located at the junction of these vessels with the cavities of the heart. The aortic valve is located on the path of blood flow from the left ventricle to the aorta, and the pulmonary artery - from the right ventricle to the pulmonary trunk.
In the normal state of the valve apparatus and myocardium, at the moment of contraction of one or another cavity, the valve leaflets close tightly, preventing the reverse flow of blood. With various heart lesions, this mechanism may be disrupted.
Sometimes in the literature and in doctors’ reports you can find references to the so-called physiological regurgation, which means a slight change in blood flow at the valve leaflets. In fact, in this case, a “swirl” of blood occurs at the valve opening, and the leaflets and myocardium are completely healthy. This change does not affect blood circulation in general and does not cause clinical manifestations.
Physiological can be considered 0-1 degree regurgitation on the tricuspid valve, at the mitral valve leaflets, which is often diagnosed in thin, tall people, and according to some data, is present in 70% of healthy people. This feature of blood flow in the heart does not in any way affect your well-being and can be detected by chance during an examination for other diseases.
As a rule, pathological reverse blood flow through the valves occurs when their valves do not close tightly at the moment of myocardial contraction. The reasons may be not only damage to the leaflets themselves, but also to the papillary muscles, chordae tendineae involved in the mechanism of valve movement, stretching of the valve ring, and pathology of the myocardium itself.
Mitral regurgitation
Mitral regurgitation is clearly observed with valve insufficiency or prolapse. At the moment of contraction of the left ventricular muscle, a certain volume of blood returns to the left atrium through an insufficiently closed mitral valve (MV). At the same moment, the left atrium fills with blood flowing from the lungs through the pulmonary veins. This flooding of the atrium with excess blood leads to overdistension and increased pressure (volume overload). Excess blood during contraction of the atria enters the left ventricle, which is forced to push more blood into the aorta with greater force, as a result of which it thickens and then expands (dilatation).
For some time, disturbances in intracardiac hemodynamics may remain invisible to the patient, since the heart, as best it can, compensates for blood flow due to the expansion and hypertrophy of its cavities.
With mitral regurgitation of the 1st degree, there are no clinical signs for many years, and with a significant volume of blood returning to the atrium, it expands, the pulmonary veins become filled with excess blood and signs of pulmonary hypertension appear.
Among the causes of mitral regurgitation, which is the second most common acquired heart defect after changes in the aortic valve, we can highlight:
- Rheumatism;
- Prolapse;
- Atherosclerosis, deposition of calcium salts on the valves of the mitral valve;
- Some connective tissue diseases, autoimmune processes, metabolic disorders (Marfan syndrome, rheumatoid arthritis, amyloidosis);
- Coronary heart disease (especially infarction with damage to the papillary muscles and chordae tendineae).
With mitral regurgitation of the 1st degree, the only sign may be the presence of a murmur in the area of the apex of the heart, detected by auscultation, while the patient has no complaints, and there are no manifestations of circulatory disorders. Echocardiography (ultrasound) can detect slight divergence of the leaflets with minimal disruption of blood flow.
Mitral valve regurgitation of the 2nd degree accompanies a more pronounced degree of insufficiency, and the stream of blood returning back to the atrium reaches its middle. If the amount of blood return exceeds a quarter of the total amount located in the cavity of the left ventricle, then signs of stagnation in the small circle and characteristic symptoms are detected.
The third degree of regurgitation is said to occur when, in the case of significant defects of the mitral valve, the blood flowing back reaches the posterior wall of the left atrium.
When the myocardium cannot cope with the excess volume of contents in the cavities, pulmonary hypertension develops, leading, in turn, to overload of the right half of the heart, resulting in circulatory failure in the systemic circle.
With grade 4 regurgitation, characteristic symptoms of severe disturbances in blood flow inside the heart and increased pressure in the pulmonary circulation are shortness of breath, arrhythmias, and the possible occurrence of cardiac asthma and even pulmonary edema. In advanced cases of heart failure, signs of damage to the pulmonary bloodstream include swelling, cyanosis of the skin, weakness, fatigue, a tendency to arrhythmias (atrial fibrillation), and pain in the heart. In many ways, the manifestations of severe mitral regurgitation are determined by the disease that led to damage to the valve or myocardium.
Separately, it is worth mentioning about mitral valve prolapse (MVP), quite often accompanied by regurgitation of varying degrees. In recent years, prolapse has begun to appear in diagnoses, although previously such a concept was quite rare. This state of affairs is largely due to the advent of imaging methods - ultrasound examination of the heart, which makes it possible to trace the movement of the valves of the MV during cardiac contractions. With the use of Doppler, it became possible to determine the exact degree of blood return to the left atrium.
MVP is typical for tall, thin people; it is often discovered accidentally in adolescents during examination before conscription into the army or undergoing other medical examinations. Most often, this phenomenon is not accompanied by any disturbances and does not in any way affect the lifestyle and well-being, so you should not be alarmed right away.
Mitral valve prolapse with regurgitation is not always detected; its degree in most cases is limited to the first or even zero, but at the same time, this feature of the functioning of the heart can be accompanied by extrasystole and disturbances in the conduction of nerve impulses through the myocardium.
If low-grade MVP is detected, you can limit yourself to observation by a cardiologist, and treatment is not required at all.
Aortic regurgitation
Reverse blood flow on the aortic valve occurs when it is insufficient or the initial part of the aorta is damaged, when, in the presence of an inflammatory process, its lumen and the diameter of the valve ring expand. The most common reasons for such changes are:
- Rheumatic lesions;
- Infectious endocarditis with inflammation of the leaflets, perforation;
- Congenital malformations;
- Inflammatory processes of the ascending aorta (syphilis, aortitis with rheumatoid arthritis, ankylosing spondylitis, etc.).
Such common and well-known diseases as arterial hypertension and atherosclerosis can also lead to changes in the valve leaflets, aorta, and left ventricle of the heart.
Aortic regurgitation is accompanied by the return of blood to the left ventricle, which becomes overfilled with excess volume, while the amount of blood entering the aorta and further into the systemic circulation may decrease. The heart, trying to compensate for the lack of blood flow and pushing excess blood into the aorta, increases in volume. For a long time, especially with stage 1 regurgitation, such an adaptive mechanism allows maintaining normal hemodynamics, and symptoms of disorders do not occur for many years.
As the mass of the left ventricle increases, its need for oxygen and nutrients, which the coronary arteries are unable to provide, also increases. In addition, the amount of arterial blood pushed into the aorta becomes less and less, and, therefore, it will not flow enough into the vessels of the heart. All this creates the preconditions for hypoxia and ischemia, resulting in cardiosclerosis (overgrowth of connective tissue).
As aortic regurgitation progresses, the load on the left half of the heart reaches its maximum degree, the myocardial wall cannot hypertrophy indefinitely and it stretches. Subsequently, events develop in the same way as with damage to the mitral valve (pulmonary hypertension, congestion in the small and large circles, heart failure).
Patients may complain of palpitations, shortness of breath, weakness, and pallor. A characteristic feature of this defect is the appearance of angina attacks associated with inadequacy of coronary circulation.
Tricuspid regurgitation
Isolated lesions of the tricuspid valve (TC) are quite rare. As a rule, its insufficiency with regurgitation is a consequence of pronounced changes in the left half of the heart (relative TC insufficiency), when high pressure in the pulmonary circulation prevents adequate cardiac output into the pulmonary artery, which carries blood for oxygenation into the lungs.
Tricuspid regurgitation leads to disruption of complete emptying of the right half of the heart, adequate venous return through the vena cava and, accordingly, congestion appears in the venous part of the systemic circulation.
For tricuspid valve insufficiency with regurgitation, the occurrence of atrial fibrillation, cyanosis of the skin, edematous syndrome, swelling of the neck veins, enlarged liver and other signs of chronic circulatory failure are quite typical.
Pulmonary valve regurgitation
Damage to the pulmonary valve leaflets can be congenital, manifesting itself in childhood, or acquired as a result of atherosclerosis, syphilitic lesions, or changes in the leaflets due to septic endocarditis. Often, damage to the pulmonary valve with insufficiency and regurgitation occurs with existing pulmonary hypertension, lung diseases, and damage to other heart valves (mitral stenosis).
Minimal regurgitation on the pulmonary valve does not lead to significant hemodynamic disorders, while a significant return of blood to the right ventricle, and then to the atrium, causes hypertrophy and subsequent dilatation (expansion) of the cavities of the right half of the heart. Such changes are manifested by severe heart failure in the systemic circle and venous stagnation.
Pulmonary regurgitation is manifested by all kinds of arrhythmias, shortness of breath, cyanosis, severe edema, accumulation of fluid in the abdominal cavity, changes in the liver up to cirrhosis and other signs. With congenital valve pathology, symptoms of circulatory disorders occur already in early childhood and are often irreversible and severe.
Features of regurgitation in children
In childhood, the proper development and functioning of the heart and circulatory system is very important, but disorders, unfortunately, are not uncommon. Most often, valve defects with insufficiency and return of blood in children are caused by congenital developmental anomalies (tetralogy of Fallot, hypoplasia of the pulmonary valve, defects of the septa between the atria and ventricles, etc.).
Severe regurgitation with an abnormal structure of the heart manifests itself almost immediately after the birth of a child with symptoms of respiratory distress, cyanosis, and right ventricular failure. Often, significant violations end fatally, so every expectant mother needs to not only take care of her health before the intended pregnancy, but also promptly visit an ultrasound diagnostic specialist during pregnancy.
Possibilities of modern diagnostics
Medicine does not stand still, and the diagnosis of diseases is becoming more reliable and of high quality. The use of ultrasound has made significant progress in detecting a number of diseases. The addition of ultrasound examination of the heart (EchoCG) with Dopplerography makes it possible to assess the nature of blood flow through the vessels and cavities of the heart, the movement of valve leaflets at the time of myocardial contractions, establish the degree of regurgitation, etc. Perhaps EchoCG is the most reliable and informative method for diagnosing cardiac pathology in the mode real time and at the same time being accessible and inexpensive.
In addition to ultrasound, indirect signs of regurgitation can be detected on an ECG, with careful auscultation of the heart and assessment of symptoms.
It is extremely important to identify disorders of the heart valve apparatus with regurgitation not only in adults, but also during fetal development. The practice of ultrasound examination of pregnant women at different stages makes it possible to detect the presence of defects that are beyond doubt even during the initial examination, as well as to diagnose regurgitation, which is an indirect sign of possible chromosomal abnormalities or developing valve defects. Dynamic observation of women at risk makes it possible to timely establish the presence of serious pathology in the fetus and resolve the issue of the advisability of continuing pregnancy.
Treatment
The treatment tactics for regurgitation are determined by the cause that caused it, the degree of severity, the presence of heart failure and concomitant pathology.
Both surgical correction of structural abnormalities of the valves (various types of plastic surgery, prosthetics) and medical conservative therapy aimed at normalizing blood flow in the organs, combating arrhythmia and circulatory failure are possible. Most patients with severe regurgitation and damage to both circulation circles require constant monitoring by a cardiologist, the prescription of diuretics, beta-blockers, antihypertensive and antiarrhythmic drugs, which will be selected by a specialist.
In case of low-grade mitral prolapse or prevalvular regurgitation of another localization, dynamic observation by a doctor and timely examination in case of worsening of the condition are sufficient.
The prognosis of valvular regurgitation depends on many factors: its degree, cause, age of the patient, the presence of diseases of other organs, etc. With a caring attitude towards your health and regular visits to the doctor, minor regurgitation does not threaten complications, and with pronounced changes, their correction, including including surgical, allows you to prolong the life of patients.
Step 2: after payment, ask your question in the form below ↓ Step 3: You can additionally thank the specialist with another payment for an arbitrary amount ↑
Diagnostic methods
Indirect signs of aortic regurgitation are noted in:
- chest x-ray - the left contour of the cardiac shadow is expanded to the side and down, the expansion of the aortic arch is similar to an aneurysm, there are clear signs of enlargement of the left atrium, calcifications may be detected in the aortic arch;
- electrocardiogram - overload of the left chambers of the heart is revealed.
Echocardiographic method
In the diagnosis of regurgitation, echocardiography serves as the main objective method; it allows one to determine the cause, the degree of regurgitation, the sufficiency of compensatory reserves, and circulatory disorders even in the asymptomatic stage of the disease with minimal disturbances. It is recommended for patients in the initial stage annually, and twice a year when clinical symptoms appear.
The calculations take into account the surface area of the patient's body, due to the lack of pronounced expansion of the ventricular chamber in short people.
The most commonly used mode is color Doppler scanning. The sensors are installed in such a way as to measure the area of blood flow at the aortic valves, in the initial part of the aorta, and compare it with the width of the passage. In severe cases, it exceeds 60% of the ring diameter.
In the practice of cardiologists, a division of the return jet into 4 degrees is used in relation to its length to the size and internal formations of the left ventricle:
- 1 - does not extend beyond half the length of the anterior leaflet at the mitral valve;
- 2 - reaches or crosses the gate;
- 3 - the flow value approaches half the length of the ventricle;
- 4 - the jet touches the top.
If information from Doppler sonography is not enough, the following is carried out:
- magnetic resonance imaging;
- radionuclide angiography;
- cardiac catheterization.
Why does backflow of blood into the MV occur?
The pumping function of the heart is provided by the left ventricle.
When it relaxes, blood from the atrium flows through the mitral orifice into its cavity. This is the diastole phase. During systole, the ventricle contracts, pushing the blood it contains into the vascular bed. Tightly closed fibrous plates, the mitral valve leaflets, prevent blood from refluxing into the atrium. If their edges do not touch during systole, part of the fluid volume moves back, and regurgitation occurs.
This condition is called mitral regurgitation.
The causes of backflow of blood may be degenerative processes in the valves. A change in the structure of the valve disrupts the shape of its edges and negatively affects the range of motion.
- systemic connective tissue lesions (for example, scleroderma);
- congenital hereditary diseases (Ehlers-Danlos syndrome);
- rheumatism;
- endocarditis of infectious etiology;
- rupture of the chordae (thin strings that connect the edge of the valve and the bottom of the left ventricle; the main function is to prevent eversion (prolapse) of the leaflets towards the atrium);
- dysfunction of the papillary muscles (located at the base of the chordae);
Valvular mitral regurgitation can be caused by changes in the myocardium with a normal leaflet structure:
- expansion of the mitral ring;
- pathological enlargement of the left ventricular cavity (with heart failure);
- hypertrophic cardiomyopathy (typical for hypertension stages 2, 3).
The atrioventricular orifice has a round shape. The basis for the valves is a fibrous ring fused to the myocardium. If the heart muscle stretches, the shape of the hole will change . In this case, the unchanged leaflets will not be able to perform their function (tightly block this outlet for blood during systole) and regurgitation will occur.
If the bicuspid valve does not close completely, this triggers a cascade of pathological processes:
The return of part of the blood volume to the left atrium causes stretching of its walls (dilatation) and overflow with blood.
- The myocardium has to push out a larger volume, the muscle fibers hypertrophy compensatoryly and contract more strongly.
- Since blood enters the left atrium from the pulmonary circulation, the pressure in the lungs increases ( the first characteristic symptom appears here - shortness of breath ).
- The right ventricle pumps blood into the lungs, and to overcome the increased resistance it also hypertrophies, but to a lesser extent.
- The left ventricle is gradually stretched by the increased incoming volume of blood.
As long as he is able to cope with the increased workload, there will be no clinical symptoms.
Classification
We found that tricuspid valve regurgitation can be congenital or acquired, primary (organic) or secondary (functional) by etiology. Organic failure is expressed by deformation of the valve apparatus: thickening and wrinkling of the valve leaflets or their calcification. Functional failure occurs when valve dysfunction is caused by other diseases and is manifested by rupture of the papillary muscles or chordae tendineae, as well as disruption of the annulus fibrosus.
Etiology
Aortic regurgitation can be caused either by primary damage to the aortic valve leaflets or by damage to the aortic root, which currently accounts for more than 50% of all cases of isolated AR (Table 1).
Valve damage
- Rheumatic fever is one of the main valvular causes of AR. Wrinkling of the leaflets due to infiltration by connective tissue prevents their closure during diastole, thereby forming a “defect” in the center of the valve, which is a window for regurgitation of blood into the LV cavity. Concomitant fusion of the commissures limits the opening of the aortic valve, which leads to the appearance of concomitant aortic stenosis (AS).
- Infectious endocarditis. AR may be caused by valve destruction, perforation of its leaflets, or the presence of growing vegetations that prevent the leaflets from closing in diastole.
- Calcified AS in elderly people leads to the development of AR in 75% of cases, both due to age-related expansion of the fibrous ring of the aortic valve and as a result of aortic dilatation.
- Other primary valvular causes of AR are:
- trauma leading to rupture of the ascending aorta. In this case, the attachment of the commissures is disrupted, which leads to prolapse of the aortic cusp into the LV cavity;
- congenital bicuspid valve due to incomplete closure or prolapse of its valves;
- large septal defect of the interventricular septum;
- membranous subaortic stenosis;
- complication of radiofrequency catheter ablation;
- myxomatous degeneration of the aortic valve;
- destruction of the biological valve prosthesis.
Aortic root damage
Diseases that can cause aortic root damage include: age-related (degenerative) dilatation of the aorta, cystic necrosis of the aortic media (isolated or as a component of Marfan syndrome), aortic dissection, osteogenesis imperfecta (osteopsatyrosis), syphilitic aortitis, ankylosing spondylitis, Behçet's syndrome, psoriatic arthritis, ulcerative colitis arthritis, relapsing polychondritis, Reiter's syndrome, giant cell arteritis, systemic hypertension, and the use of certain appetite suppressants.
AR in these cases is formed due to pronounced expansion of the aortic valve ring and aortic root with subsequent separation of the leaflets. Subsequent dilatation of the root is inevitably accompanied by excessive tension and bending of the valves, which then thicken, wrinkle and become unable to completely cover the aortic opening. This, in turn, aggravates AR, leads to further expansion of the aorta and closes the vicious circle of pathogenesis (“regurgitation increases regurgitation”).
Regardless of the cause, AR always causes dilatation and hypertrophy of the left ventricle, with subsequent dilation of the mitral annulus and the possible development of left atrium dilatation. Often, “pockets” form on the endocardium at the site of contact between the regurgitant flow and the LV wall.
Treatment
The basis of treatment measures is taking medications aimed at removing the causes and signs of the disease. In addition, this method of therapy is recommended for the development of complications. Mitral valve insufficiency of the two initial stages of development does not require medical intervention. A more complex course involves performing surgical operations, of which there are several. The first type of intervention, plastic surgery, is used for diseases in the second and third stages. There are three ways to do this:
- plasty of the valves - a support ring is sewn in at the base of the valves;
- decrease in chord length;
- elimination of the elongated part of the rear sash.
The second type of operation is based on valve replacement. Prostheses can be made from biological material, such as an animal's aorta. They are often used to treat mitral regurgitation in children and women who want to have a child in the future. In addition, there are mechanical valve prostheses that are made from medical alloys. In the postoperative period, patients need to take anticoagulants, which are aimed at reducing blood clotting. In cases of implantation of a mechanical valve, it is necessary to take medications throughout life; in case of implantation of a biological valve, drug therapy lasts no more than three months. With valve repair, the use of drug therapy is not required.
Carrying out any type of operation is strictly prohibited in the presence of serious illnesses that will inevitably lead to death, as well as in cases of heart failure that cannot be treated with drugs.