Yeast is a type of fungal infection caused by the Candida species. It can affect a variety of areas of the human body: from intimate areas to the skin and nails. Under normal conditions, a small amount of spores of the disease is concentrated in the body, but the immune system allows you to cope with them. When the condition of a woman’s body worsens due to illness, infection (stress), the immune system can no longer contain fungal spores, an inflammatory algorithm begins, which is very important to treat – not only in the groin area, but in all the others.
Where does the fungus enter the female body?
Gynecological fungal diseases are caused by a fungus of the genus Candida. It is part of the microflora in women.
But if various unfavorable factors begin to put pressure on it, which weaken the immune system, then the fungus will begin to grow very quickly and uncontrollably. Gradually it will affect the genitals and mucous membranes of the gastrointestinal tract. Read also: How to get tested for fungus: types of fungi, how tests are taken.
Unfavorable factors that provoke the growth of fungus:
- Elderly age;
- Diabetes;
- Venereal diseases;
- Taking antibiotics, hormonal drugs;
- Injuries to the genital organs;
- Infectious diseases in chronic form;
- Surgical interventions.
The fungus can also be transmitted to a woman during sex with a man who has a fungal infection of the penis.
Gynecological fungal diseases
In women, the Candida fungus causes urogenital candidiasis or, to put it simply, thrush. But if a colony of fungi infects the vulva, then vulvovaginitis or vaginitis will occur. These gynecological fungal diseases cause a lot of trouble for women, as they occur with severe itching, burning and discharge.
Symptoms of urogenital candidiasis:
- Pain during sexual intercourse;
- Copious curdled vaginal discharge;
- Itching and burning in the vagina.
Thrush is an insidious disease. If it goes into a chronic stage, then before each menstruation a woman may experience an exacerbation.
Symptoms of vulvovaginal candidiasis and vaginitis
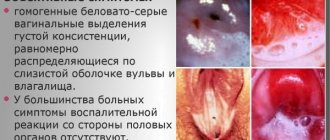
- The amount of vaginal discharge increases;
- An unpleasant odor appears, which tends to intensify after sex;
- The discharge is white and “plaque-like”;
- Itching intensifies after sex, as well as when exposed to heat;
- Burning of the external genitalia;
- The mucous membrane of the genital organs becomes more sensitive to urine and water.
Gynecological fungal diseases can cause various complications. In women, the fungus can easily penetrate the genitourinary system.
This can trigger the development of inflammatory diseases and also lead to infertility. Foci of inflammation usually form in the fallopian tubes, uterus and ovaries. Fungal infections can cause the development of colpitis, erosion, endometritis, and bartholinitis.
Vaginal smear - what infections does it show?
A vaginal smear allows you to identify pathogenic microflora in the vagina (bacteria, fungi). This is the simplest and most effective laboratory method for diagnosing the inflammatory process in the female genital organs. Based on the results of the analysis, the gynecologist makes a diagnosis (vaginal candidiasis, vaginitis or other gynecological disease).
A vaginal smear shows:
- number of leukocytes, lactobacilli, squamous epithelial cells;
- Is the ratio of “beneficial”, pathogenic and opportunistic microorganisms, the number of which must be balanced, disturbed?
Treatment of fungal diseases in women
In women, fungal diseases are quite difficult to completely cure. Treatment must be comprehensive. You need to start with the use of local and systemic antifungal drugs.
Doctors recommend taking Diflazon9raquo;, Flucostat9raquo;, Mycoflucan9raquo; orally. Locally prescribe vaginal suppositories - “Livarol9raquo;, “Iodoxide9raquo;. The use of Clotrimazole cream gives a good effect.
Next, you need to work on restoring the normal microflora of the vagina. As soon as antifungal therapy ends, you need to start taking medications that contain lactobacilli orally, and place tampons or suppositories with the same lactobacilli in the vagina.
It is imperative to take care of your immune system. After all, a fungal infection occurs when the body’s defenses have decreased. For this reason, it is recommended to use multivitamin complexes.
Prevention of gynecological fungal diseases
- Try to reduce douching to a minimum, or better yet, do not use this procedure at all;
- Avoid stressful situations;
- Do not wear underwear that is too tight;
- Do not wear synthetic underwear;
- Balanced diet;
- Visit your gynecologist every 6 months;
- Intimate hygiene must be at a very high level;
- Don't take baths that are too hot;
- Avoid casual sexual contacts;
- Do not use pads with strong fragrances.
Where does a fungal infection come from?
Fungi of the genus Candida are an integral part of the microflora of the female body. But under the influence of unfavorable factors that weaken the immune system, the fungus begins to multiply uncontrollably, infecting the mucous membranes of the gastrointestinal tract and the female genital organs.
Such unfavorable factors include:
- Endocrine system diseases (obesity, diabetes, hypothyroidism)
- Metabolic disease
- Taking medications (antibiotics, cytostatics, hormonal contraceptives)
- Pregnancy
- Elderly age
- Sexually transmitted diseases (trichomoniasis, ureaplasmosis, chlamydia)
- Chronic infectious diseases
- Injuries
- Surgical interventions
In some cases, the fungus can be transmitted through sexual contact with a man who has candidiasis of the penis.
Complex treatment of gynecological fungal diseases includes the following stages:
- The use of local, topical and systemic antifungal drugs, such as Polygynax. nystatin. candidate Fluconazole preparations for oral administration (flucostat, mycoflucan, diflazon, fluconazole, etc.) have a good effect. For local use, vaginal suppositories iodoxide, livarol, vaginal tablets or clotrimazole cream, etc. are used.
- Restoration of the natural microflora of the vagina. After the end of antifungal treatment, tampons or suppositories with lactobacilli are used to restore normal microflora, or oral preparations with lactobacilli are used.
- General strengthening measures. Since the appearance of a fungal infection indicates a decrease in the protective properties of the immune system, it is necessary to direct efforts to strengthen them. For this purpose, taking multivitamins with a high content of ascorbic acid, vitamins A and E is indicated.
Yeast on a smear: where to go
If yeast is detected in a smear, please contact our clinic. We have experienced doctors who will carry out the necessary additional examination and treatment.
Our services:
- determining the type of candida that caused inflammation for more effective treatment
- selection of antifungal therapy
- screening for concomitant infections
- examination to identify the causes of recurrent candidiasis (immunogram, blood glucose test, HIV test, etc.)
We offer treatment for recurrent candidiasis. If necessary, we conduct a culture to determine sensitivity to antifungal drugs.
If yeast is detected in a smear, contact the experienced specialists of our medical center.
According to statistics, candidiasis occurs in 9 out of 10 women during pregnancy. Most often, this disease manifests itself in the last trimester. But, despite the “harmless” symptoms, the infection can lead to serious consequences for both the expectant mother and the child.
Candidiasis or thrush develops due to excessive proliferation of the yeast-like fungus Candida albicans. In small quantities, its strains are present in the normal microflora of the vagina.
Prevention of fungal diseases
The following recommendations will help prevent the uncontrolled proliferation of Candida fungi, and, consequently, the development of gynecological fungal diseases:
- Avoid douching
- Do not wear tight underwear, especially those made from non-natural fabrics
- Use scented tampons and pads as little as possible
- Avoid taking hot baths
- Maintain intimate hygiene
- Do not be in a wet swimsuit
- Avoid casual sex
- Eat balanced
- Avoid stress
- Regularly undergo preventive examinations with a gynecologist.
Consequences of untreated candidiasis of the labia
If you start treating labia fungus in time, you can avoid unpleasant consequences and harm to health. However, the symptoms of the disease themselves are not at all pleasant; they can constantly cause discomfort that increases over time and disrupt the quality of life.
The fungus needs to be treated on time to prevent complications.
Usually, candidiasis takes a very long time to be treated, and in complicated forms it can affect the bladder, urethra and kidneys. When the disease is completely advanced, reproductive functions may be impaired, resulting in infertility. In case of pregnancy, candidiasis can threaten the development and life of the fetus.
What is the disease?
Fungal infection of the vagina (candidiasis) is a gynecological disease of an infectious-inflammatory nature that affects the mucous membranes. The pathology is widespread.
According to statistics, up to ninety percent of the fair sex encounters it. This is explained by the fact that Candida fungi, present in the body of every person, can remain there for a long time without manifesting themselves, however, under the influence of certain factors and under favorable circumstances, they begin their pathological activity.
Thus, every woman has a risk of contracting vaginal fungus. Therefore, it is especially important to know how to identify this disease in the early stages and how to treat it correctly.
How to take a yeast smear
To diagnose urogenital candidiasis, smears are taken from:
- vagina
- urethra
- head of the penis (smear-imprint)
Also, material can be collected from other parts of the body. For example, anus or mouth.
The research will be most informative if:
- no antimycotics were prescribed before the examination
- no topical medications were used for 3 days
- a smear was taken against the background of existing clinical symptoms, from an area of active inflammation
- in a woman, the study was carried out closer to the middle of the cycle
In women, a swab is taken from the urethra first.
Then a native smear is prepared from material obtained from the lateral vaginal vaults. After this, a sample is taken from the cervical canal.
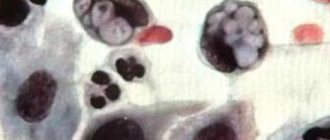
Vaginal samples are most often tested. The material is taken with a bacteriological loop. It is placed on a glass slide and diluted with saline solution.
Then they are covered with a coverslip and examined under a light microscope. If the doctor does not immediately plan to make a diagnosis, he places the taken material in a test tube with warm saline solution. In this form, the material is sent to the laboratory. In addition to the native smear, Gram stain, methylene blue stain, or potassium hydroxide stain can be used.
Causes
The main factor provoking the occurrence and development of the disease is a certain kind of fungal infection that enters the female body. However, there are a number of factors that provoke and stimulate this process. These include:
- Disturbances in the functioning of the immune system.
- Diabetes mellitus and other endocrine diseases. Hypothyroidism. Hormonal imbalances.
- Stressful situations. Mental and physical fatigue.
- Past severe infectious diseases.
- General intoxication of the body.
- General weakening of the immune system.
- Recent surgery.
- Excessive physical activity and psychological stress.
- Vaginal microflora disorders.
- Certain gynecological diseases.
- Long-term treatment with antibiotics, uncontrolled use of a number of medications that cause changes in the microflora and functioning of the body’s immune system.
- Long-term use of local external antibacterial agents.
- Prolonged and uncontrolled use of hormonal contraceptives, intrauterine contraceptives.
- Wearing tight, form-fitting, synthetic underwear.
- Tuberculosis.
- Neglect of intimate hygiene rules.
- Poor nutrition, alcohol abuse.
- Pregnancy.
- Tendency to allergic reactions.
- Presence of sexually transmitted diseases.
- Traumatic injuries to the vaginal mucosa.
- Frequent and prolonged douching (especially with the use of antibacterial solutions).
- Hypothermia of the body.
Signs of defeat
This disease is characterized by very specific signs and symptoms that make it possible to identify it even in the early stages of development. These include the following:
- Pain in the genital area.
- Feeling of itching and burning in the vaginal area.
- Thick, white vaginal discharge with an unpleasant, specific odor.
- Swelling of the mucous membrane.
- Frequent urge to urinate.
- Feeling of discomfort in the intimate area.
- Unpleasant sensations during sexual intercourse.
- Difficulty urinating, pain and burning sensation during this process.
- The appearance of a characteristic white coating on the vaginal mucosa.
- Sleep disorders, insomnia.
- Increased vaginal dryness.
- Irritation of the genital organs during contact with urine.
It should be emphasized that vaginal fungal infections not only significantly reduce a woman’s quality of life and cause a lot of discomfort, but can also lead to serious infectious lesions of the body.
This disease is especially dangerous during pregnancy, since the pathogenic fungus is quite capable of leading to miscarriage or intrauterine infection of the fetus.
Therefore, if you find at least a few of the above signs, you should consult a gynecologist. The earlier you start treating an infectious disease, the easier and faster it will be to get rid of it with the least damage to the body!
Myth No. 9: Thrush is not dangerous.
The danger itself is the delusion itself. The fact is that a yeast infection can have serious consequences and very unwanted complications.
- It weakens the immune system and opens the way for other pathogenic microorganisms. Thrush is often associated with other infectious diseases.
- A common complication of yeast infections is vaginal stenosis.
- Candidiasis of the urogenital area is especially dangerous for pregnant women. It can lead to spontaneous miscarriage, premature birth of a child, and cause low birth weight of the newborn.
- In addition, thrush can cause miscarriage.
Diagnostic methods
This disease is determined during a gynecological examination, based on a study of symptoms, the general clinical picture, and the results of the anamnesis. To clarify the diagnosis and determine the type of fungal pathogens, the patient is prescribed the following studies:
- Taking a smear of vaginal contents.
- Smear analysis.
- Bacteriological culture.
- Carrying out tests to determine sensitivity to the effects of antimycotic therapy.
- Analysis of urine.
- Conducting studies of the bacterial flora of vaginal discharge.
- Immunofluorescence.
- PCR – diagnostics.
- Conducting special testing with KOH to detect the presence of certain pathogenic bacteria, as well as mycelium and pseudomycelia.
- Cytological analysis.
Depending on the results of the research, the specialist will develop a course of treatment that will be as safe and effective as possible in each case. This takes into account the type of pathogen, stage of the disease, age and general health of the patient.
Treatment of thrush in women with drugs
It is necessary to improve the health of the vaginal microflora under the supervision of a doctor. Self-treatment can quickly remove the symptoms, but the Candida fungus lurks and will recur in the future.
If a connection between the disease and the use of antibiotics is established, they are canceled. Further actions are determined by the stage of the thrush.
For mild candidiasis, topical medications are prescribed - these are fungicidal suppositories and ointments:
The doctor may also recommend a single dose of Fluconazole tablets at a dosage of 150 mg. For chronic mycosis, Fluconazole and its analogues are taken weekly at 100 mg. Treatment lasts from several weeks to several months.
If fungi recur regularly, the woman is recommended to undergo examination by an endocrinologist and other specialists to make sure there are no chronic pathologies.
It is mandatory to take measures to strengthen the immune system, and develop a course of therapy for the sexual partner.
The choice of drugs remains with the attending physician, since cases of genital thrush are always individual. In addition to antifungal agents, courses of immunotherapy, herbal medicine and fortification of the body can be prescribed for the treatment of vaginal fungus.
During treatment, abstinence from intimate life (in any form) and increased hygiene will be useful.
To maintain intestinal microflora, women are prescribed B vitamins and prebiotics - Bon-Sante, Normaze, Lactusan, Duphalac, etc.
In terms of diet, the gynecologist may recommend avoiding spices, salty and pickled foods, sweets and fatty foods. Preference is given to fresh vegetables, fruits and herbs and dairy products. The daily menu should be rational.
Strengthening the immune system
With regular relapses of thrush, you need to draw the doctor’s attention to this in order to examine other organs for the presence of chronic diseases. In particular, it is necessary to evaluate the functioning of the endocrine system. Recurrent thrush requires complex treatment, the course of which can last 2 or more months. In particular, Fluconazole 100 mg is used orally once a week until recovery. Regular monitoring by a doctor will allow you to defeat the disease without harming the body.
If you have a regular sexual partner, it is important that both undergo treatment for a fungal infection to avoid re-infection. After treating acute candidiasis, you can take control tests a week later. If the course was aimed at treating chronic vaginal mycosis, then control tests are taken three times at intervals of a month. The analysis takes place immediately after menstruation.
Folk remedies against vaginal dysbiosis
You can remove Candida fungus from the vagina by creating conditions for it to die.
- Mycosis pathogens do not like an alkaline environment, so you can use 1 liter of boiled water, 50 drops of iodine and 1 spoon of baking soda. The solution is poured into a warm bath and the procedure is taken before bed. This treatment lasts 10 days.
- Alum works well as a medicine against thrush. 2 tablespoons of pharmaceutical alum are diluted with 1 liter of water and kept on the stove until it boils. A warm solution is used for washing and douching.
- In the treatment of vaginal fungus with folk remedies, medicinal herbs with antiseptic properties are widely used - calendula, sage, chamomile, etc. Decoctions are prepared from 1 spoon of any herb and 200 g of water.