Damage to the cervix: forms
Damage to the cervix (rupture) occurs both spontaneously and due to surgical intervention (violent).
Spontaneous ruptures can be caused by:
- excessive stretching of the cervix;
- rigidity of the cervix, that is, loss of its elasticity. Often observed in primiparous women over 30 years of age;
- large fruit when its weight exceeds 4 kg;
- advancement of the fetus with an extended cervical spine along the birth canal;
- a woman’s narrow pelvis, the consequence of which is prolonged compression of the cervix and further disruption of the nutrition of its tissues with a decrease in their strength;
Forced ruptures occur during operations that accelerate labor, namely:
- vacuum extraction of the fetus;
- application of obstetric forceps;
- extracting the fetus by the pelvic end.
There are three degrees of cervical rupture:
- Grade 1: tears no more than 2 cm on one or both sides;
- 2nd degree: tears larger than 2 cm, not reaching the vaginal vaults;
- 3rd degree: ruptures reaching and extending to the vaginal vaults.
Complicated and uncomplicated cervical ruptures are also distinguished.
Uncomplicated tears include grade 1-2 tears.
Complicated ones include:
- ruptures reaching and extending to the vaginal vaults;
- ruptures ascending the cervical canal and reaching the uterine internal os;
- ruptures involving the parametrium or peritoneum.
Treatment
The basis of treatment is surgical correction. If there is no bleeding, doctors close the rupture with self-absorbing sutures. The operation is performed under general anesthesia; the cervix is brought closer to the vaginal outlet using bullet forceps and retracted in the opposite direction. After this, the doctor places stitches just above the tear through all layers of the cervix except the mucous membrane. If the lesion is extensive, it may be necessary to open the abdominal cavity, in which case the operation is called transection. It is usually indicated when the parametrium is ruptured and hematomas form there.
Complications and consequences
In most cases, cervical rupture does not lead to serious consequences. After complete healing, the woman returns to her usual lifestyle. If the rupture was discovered late or was not completely sutured, the woman may experience a number of complications. Among them are:
- Rupture of the uterus or disruption of the integrity of its walls.
- Formation of a hematoma in the fatty tissue around the uterus.
- Inflammatory processes in the cervix.
- Hemorrhagic shock due to loss of blood.
- Disturbances in the reproductive system.
- Cervical inversion, which increases the likelihood of cancer and erosion.
An incompletely sutured cervical rupture can cause complications. This leads to future miscarriage and isthmic-cervical insufficiency. Pathology also provokes the formation of inflammatory and precancerous diseases. Due to the formation of scars at the site of the rupture, a woman may experience problems with the reproductive system, and the quality of sexual life decreases.
Prevention
Prevention consists of proper management of labor, timely and careful delivery, which should be carried out in obstetric conditions. It is strictly forbidden to extract the fetus if the throat is not open enough. If the doctor sees that it is impossible to do without applying forceps due to incomplete opening of the pharynx, then it is necessary to cut it in both directions using surgical scissors.
To prevent recurrent cervical rupture, a woman should abstain from sex for 2 months.
Ignoring this recommendation leads to rupture of the applied sutures, resulting in bleeding and the formation of erosion. You can plan a pregnancy only after you have completely gotten rid of the consequences of the breakup. Doctors recommend that at least 2 years pass from the moment of uterine surgery to conception. Otherwise, there is a high risk of ectopic pregnancy or other complications.
Cervical ruptures
arise mainly during childbirth, so the question of fresh cervical ruptures relates to the field of obstetrics.
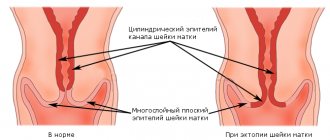
Here we will only talk about old breaks. Cervical ruptures never heal by primary intention; if the rupture was not sutured in a timely manner, the wound becomes filled with granulations, undergoes scarring and leaves behind a gaping gap. Ruptures are often lateral, one- or two-sided. With a bilateral rupture, the external pharynx turns into a wide gap, and the anterior and posterior lips are presented in the form of separate semilunar flaps. The deeper the gap, the more the uterine pharynx gapes and the more the mucous membrane of the cervical canal protrudes outward (ectropion).
Treatment of old cervical ruptures can only be surgical.
Contraindications to surgery are: 1) suspicion of pregnancy; 2) suspicion of malignant degeneration of the everted mucous membrane of the cervix or specific syphilitic and tuberculous ulcers (at the slightest suspicion of such, a biopsy should be done first); 3) the presence of acute or subacute inflammation of the genital organs, as well as chronic inflammation of the uterine appendages, pelvic peritoneum, pelvic tissue; 4) intercurrent diseases with increased temperature.
Method of surgical treatment
depends on the size and shape of the gap.
For one- or two-sided lateral ruptures of the vaginal part of the uterus that do not extend to the vaginal vault, if the cervix is not excessively hypertrophied and not severely deformed, plastic surgery is used to restore the previous shape of the external uterine os. As always before vaginal surgery, vaginal discharge should be brought to I or II degree of purity, i.e. lactic acid bacilli should predominate in smears taken from the vagina (at II degree of purity, along with vaginal bacilli, colibacillus and gram-positive diplococci may be found and a small number of staphylococci; in addition to the indicated bacterial flora, in smears, along with cells of the vaginal squamous epithelium, leukocytes may also be found in small quantities). In the presence of purulent discharge and contaminated vaginal flora, surgery should be postponed and vigorous conservative treatment of pathological discharge should be carried out first.
Anesthesia
during plastic surgery on the cervix, despite the fact that the tissue of the uterine cervix is not very sensitive, it is still necessary, since the strong reduction of the cervix, required for this operation according to technical conditions, is very painful. This operation does not last long, and if there are no contraindications to short general ether anesthesia, we willingly resort to it.
Among the plastic methods of surgery for an old cervical rupture, plastic surgery using the method of refreshing the edges of the rupture has become widespread.
Technique of operation using the refreshing method
. Preparation for surgery, usual for vaginal operations. The external genitalia, after the hair on them is shaved, is disinfected with alcohol and iodine tincture; The vagina, the vaginal part of the uterus and the cervical canal are wiped in a mirror with alcohol and lubricated with iodine tincture. The surgical field is covered with sterile linen; vaginal specula are replaced with fresh ones and the cervix is again exposed; using bullet forceps, grab the anterior and separately posterior lips of the uterine pharynx; the anterior spoon of the vaginal speculum (lift) is removed, and the rear one is replaced with a short operating speculum, which allows the cervix to be brought down to the entrance to the vagina. After this, using zero forceps, the anterior lip of the uterine pharynx is retracted anteriorly (towards the womb), and the posterior lip is retracted posteriorly (towards the anus); thus, the angle of the rupture is exposed (for a unilateral lateral rupture) or alternately both angles (for a bilateral rupture).
In order to reconnect the edges of the old gap, they need to be refreshed. During the Emmettian refreshment operation, the scar is excised. First, the boundaries of the refreshment are outlined with a sharp scalpel. On the inside, the refreshment border should pass at the very edge of the mucous membrane of the cervical canal so that the mucous membrane remains intact. When cutting off a piece of scar with a sharp knife, you need to make sure that the entire surface is refreshed; if an unrefreshed area remains, then fusion with the opposite side will not occur in this place. For good fusion, the cut flap should not be too thin. A flap of the same thickness is cut on the opposite surface of the tear.
After the flaps are excised on the lower and upper surfaces of the tear, sutures begin. To avoid bleeding in the postoperative period, some plastic surgery operators use silk ligatures. During these operations, we invariably use catgut (No. 3), and we always sew with interrupted sutures, and not with a continuous suture. Some gynecologists do not pass sutures through the mucous membrane of the cervical canal, but make injections and punctures slightly away from the edge of the mucous membrane of the cervical canal. If there is a bilateral cervical rupture, then it is advisable to perform a refresh on both sides, and only after that apply sutures first on one and then on the other side of the rupture.
The described operation is associated with tissue loss. The flaps to be removed, as we have already indicated, should not be very thin, otherwise there will be no good fusion of the refreshed surfaces. If the rupture occurs in a woman with a narrow infantile cervix, the loss of tissue during Emmett's surgery can sometimes lead to an even narrower cervix after the rupture has been successfully repaired. Therefore, we personally prefer to perform cervical plastic surgery using the “flap method”.
Flap technique for old neck rupture surgery
. The principle of this method is not to excise the scar that has formed at the site of the rupture in the mucous membrane of the cervical canal, the muscular wall and the mucous membrane covering the vaginal part of the uterus, but to split it. By splitting this scar, we separate the edge of the mucous membrane of the cervical canal and the underlying scar tissue from the scar tissue adjacent to the covering of the vaginal part of the uterus. Therefore, we reproduce the same thing that happens when a tear is scarred, but in reverse order. When a scar formed at the site of the rupture, the outer edge of the rupture, covered with the mucous membrane of the vaginal part, gradually merged in a sealing scar with the edge of the mucous membrane of the cervical canal, but during plastic surgery we separate them again, and split “refreshed” surfaces are formed in the scar, which grow together after connecting them to each other.
The indications, conditions, and preparation for surgery for pain relief with the flap method of surgery are the same as for the operation with the refreshment method.
Progress of the operation
: using bullet forceps, pull the anterior lip of the uterine call away from the posterior one. An incision is made along the scar, at the site of the former rupture. The scar is split with a sharp knife, which is drawn parallel to the mucous membrane of the cervical canal. When the splitting of the scar along the upper and lower edges of the tear is completed, four refreshed surfaces are obtained: two at the top and two at the bottom. After this, they begin to apply sutures. First, the freshened edges of the mucous membrane of the cervical canal are sewn together with separate catgut ligatures so that the knots of the tied ligatures lie inside the cervical canal. Then, using separate ligatures (catgut No. 3 or thin silk), the refreshed surfaces of the thickness of the cervical wall are sewn together; the nodes of these sutures lie on the outer surface of the vaginal part of the uterus. If the patient, as is often observed with old cervical ruptures, suffers from menorrhagia, then before plastic surgery begins (after probing the uterine cavity and a slight expansion of the cervical canal), the uterine cavity is scraped out with a narrow curette. In the postoperative period, no special measures are required. But we must remember that healing of refreshed scar tissue in one way or another is sluggish, and any excessive physical stress can disrupt healing and lead to postoperative bleeding. That is why, despite the insignificance of the surgical trauma accompanying plastic surgery on the cervix, we still keep the patient in bed for 7-8 days and discharge her from the clinic no earlier than the 10th day. Sexual activity is permitted 3 weeks after discharge from the clinic and not earlier than the end of the first week after discharge
Rupture of the cervix during childbirth complicates the course of labor in 6 women out of a hundred, while during the first birth this happens 4 times more often.
The consequences can be very serious if healing is poor or for some reason the wound is not sutured. The causes of cervical rupture are varied:
1. Inadequate management of the second stage of labor, often due to the fault of the woman in labor herself. At the end of the first stage of labor, when the genital organ is not yet fully dilated, the moment comes when the first attempts come, an irresistible, acute desire to push down appears, however, since the cervix has opened only 8 cm, attempts can lead to damage to it, you cannot push, You need to breathe through this period. If a woman in labor is allowed to push ahead of time or does not listen to the medical staff, rupture becomes a very possible complication.
2. A decrease in the elasticity of the cervix, which leads to its incomplete dilatation, sufficient for the birth of a child, but not sufficient for this to happen without complications. The reasons for this may be the late age of the woman in labor for the first birth, or other conditions that reduce the elasticity of tissues, for example, the presence of scars after abortions and previous births, operations on the cervix, and other traumatic and infectious injuries.
3. Features of childbirth. Problems occur during childbirth with a large fetus, during breech birth, and during the provision of obstetric care (operative childbirth). Discoordination of labor activity contributes to pathologies, or, on the contrary, labor occurs too quickly.
Classification of cervical ruptures.
There are three degrees of damage. Usually the damage is localized on the sides of the hollow muscular organ on both sides.
1st degree - occurs most often, while the cervix has damage not exceeding 2 cm in length. 2nd degree - the wound is deeper than 2 cm, but does not extend to the vaginal wall. Grade 3 - tissue damage extends to the vaginal vaults.
Damage to the cervix is manifested by the development of usually minor bleeding immediately after the birth of the child, and without examination of the soft birth canal it is not diagnosed. With 3rd degree ruptures, blood can accumulate in the soft tissues and tissue around the uterus, this is dangerous. A parametric hematoma is formed, its symptoms are pain and a feeling of fullness in the pelvic area and perineum.
If the wound is left unsutured, the consequences can be quite serious. The female genital organs are capable of healing on their own, but the edges of the rupture may be everted or incorrectly aligned, this is called ectropion of the cervix. By and large, this is an erosion that will bother you until it is removed surgically. In this case, childbirth may be complicated by repeated ruptures, pregnancy may be complicated by isthmicocervical insufficiency and miscarriage. All these are the consequences of unsutured ruptures after childbirth and poor healing.
With timely treatment to the required extent, any internal damage during childbirth results in complete restoration of the shape and function of the cervix.
“Old wounds,” if not treated correctly, can manifest themselves as erosion, or even ectropion. These are contact bleeding (bloody discharge after sex), recurrent colpitis and inflammatory diseases (cervicitis). Long-term ectropion cannot be treated conservatively and may even lead to cancer; reconstructive surgery on the cervix is required. “Old wounds” and pregnancy repeatedly create the risk of miscarriage, since the ability of the reproductive organ to hold the fetus is impaired, under load it begins to open ahead of time, and at the same time, due to the scar and decreased elasticity, it can rupture again during childbirth, since will not be able to fully open up.
All women are examined by a doctor immediately after the birth of the child and the separation of the placenta, and the degree of damage to the soft birth canal is assessed. At that point you won’t care; the procedure is easy to bear. Injuries of the 1st degree, and often the second, are sutured without any anesthesia at all; it is not necessary, since there are no nerve receptors in this area. It can only be unpleasant because the birth canal is painfully stretched; treatment comes down to careful comparison of the edges of the tear and suturing with restoration of the anatomy of the cervix; catgut sutures are placed that do not require further removal from the vaginal vault to the internal os.
Cervical rupture is one of the complications of childbirth. A woman may not feel pain if the damage is not too significant, but this does not mean that this situation is unworthy of attention. Immediately after the birth of the child, the doctor conducts a gynecological examination, and if any tears are found during childbirth, they are stitched up.
If the stitches are not carefully applied, this can lead to a number of problems in the future:
- ectropion (eversion of the mucous membrane of the cervix), which will be a constant source of inflammation, bleeding when touched, including during sexual intercourse;
- there will be a threat of tissue tearing during subsequent births; in principle, such a possibility already exists with a serious degree of cervical rupture;
- isthmic-cervical insufficiency - a severely damaged cervix will not be able to remain closed until the end of the pregnancy, there will be a threat of spontaneous miscarriage in the later stages and premature birth.
Such complications of cervical rupture during childbirth are very common. In order to carry a child to term, women are given stitches and the cervix is sutured, as it begins to smooth out and open ahead of time. True, this does not always help... But one way or another, childbirth after a cervical rupture can and should be natural, if there are no indications for a cesarean section. And the stitches are removed at approximately 37-38 weeks. Or earlier, if contractions begin, or amniotic fluid breaks.
The causes of cervical rupture during childbirth vary, sometimes they can be prevented and sometimes they cannot. Sometimes this may be due to unprofessional actions of doctors and midwives. Thus, doctors often try to manually “re-open” the cervix to the required 10 centimeters and injure the tissue.
Other reasons:
- cervicitis, colpitis are infectious processes;
- damage to the cervix, scars resulting from abortions, diagnostic procedures, treatment of erosion and dysplasia, especially in the case of conization and diathermoelectrocoagulation - “cauterization” of erosion with electric current;
- narrow maternal pelvis;
- the fetus is large, which is why perineal ruptures occur during childbirth;
- fast, rapid labor, especially if the baby comes out in the wrong position;
- rigidity (inelasticity, poor extensibility) of the cervix - occurs in both young girls and mature women;
- early pushing, a woman begins to push when the preparation of the cervix for childbirth has not been completed, there is no necessary dilation;
- the use of obstetric forceps, bullet forceps, vacuum extraction of the fetus and similar manipulations;
- fetal hydrocephalus.
As you can see, childbirth without ruptures is not always possible. But a woman can still do something to reduce the risk of a pathological birth. This means paying attention to vaginal discharge - after all, it is they that are the main symptom of the inflammatory process, which can become one of the provocateurs of ruptures. Naturally, regular monitoring by a gynecologist is mandatory. Or even better, attend a school for young mothers, where they will tell you about cervical ruptures during childbirth and how to prevent them. It is necessary to learn in advance proper breathing, which will help curb untimely attempts. Rarely does anyone succeed in learning this quickly while already in labor.
If a woman has had complicated cervical ruptures, that is, extending to the vaginal walls, which have a large area, she should undergo a thorough examination by a gynecologist before a new pregnancy. Often in such cases, you first need to make a surgical correction, this is a treatment for cervical rupture, and only then, after some time, plan conception. In this case, colposcopy should be normal. It would be useful to do an ultrasound, where the doctor can examine the scars and suggest the likelihood of problems during pregnancy.
Almost always, cervical ruptures during childbirth have some consequences. But there is no need to be upset. The main thing is to follow all the instructions of your doctor. And give birth to a trusted specialist.
| 04/13/2019 11:55:00 Losing weight quickly: the best tips and methods Of course, healthy weight loss requires patience and discipline, and crash diets do not bring long-term results. But sometimes there is no time for a long program. To lose weight as quickly as possible, but without hunger, you need to follow the tips and methods in our article! |
| 04/13/2019 11:43:00 TOP 10 products against cellulite The complete absence of cellulite remains a pipe dream for many women. But this does not mean that we should give up. The following 10 foods tighten and strengthen connective tissue—eat them as often as possible! |
| 04/11/2019 20:55:00 These 7 foods are making us fat The food we eat greatly affects our weight. Sports and physical activity are also important, but secondary. Therefore, you need to be careful when choosing products. Which ones make us fat? Find out in our article! |
The onset of labor ahead of schedule, an abnormally narrow pelvis in a woman in labor, the breaking of water without the development of labor and other pathologies of delivery cause rupture of the cervix. This is a very dangerous injury that requires treatment.
To understand why ruptures occur, you need to understand what is the basis for the pathology. The main reason for the occurrence of cracks in the cervix is its incomplete dilatation before childbirth. The abnormal condition provokes difficulties in childbirth.
Why does the cervix rupture during childbirth?
- weak elasticity or its decrease with age, after 30 years;
- a large number of abortions performed;
- the presence of birth scars;
- child is too large – more than 4 kg;
- pathological opening during delivery;
- obstetrician errors;
- pelvic position of the fetus;
- rapid labor;
- abnormally narrow pelvis;
- age over 35 years;
- excessively long period of contractions, over 20 hours;
- organ rigidity;
- early discharge of amniotic fluid.
Non-violent cervical ruptures are caused by factors that the woman in labor cannot spontaneously influence. But there are also those that become the result of improper medical care; they are considered to be violent. This is the use of obstetric forceps (they are prohibited for use), a vacuum extractor, and also pulling the child by the pelvic end.
Deep cracks can also involve the vagina, and a rupture of the perineum is possible as a complication. The most common are lateral tears, which soon scar, but make themselves felt in subsequent births.
The cause of cervical rupture often lies in the unprofessionalism of obstetricians. The presence of two or more factors that provoke pathology increases the likelihood of a problem occurring.
Damage to the cervix: causes
There are a number of reasons leading to cervical ruptures:
1. Dystrophic and inflammatory diseases of the cervix:
- cervicitis;
- true cervical erosion;
- cervical scars;
- consequences of treatment of dysplasia and true erosion of the cervix: cauterization with laser, liquid nitrogen, exposure to electric current or high temperatures;
- consequences of cervical conization.
2. Prolonged compression of the cervix between the woman’s pelvic bone ring and the fetal head;
3. Strong stretching of the edges of the uterine os with:
- fetal hydrocephalus;
- extension position of the fetus;
- large fruit (weight over 4 kg);
Complicated forms of cervical injury occur in the following cases:
- rapid labor: for primiparous women it lasts up to 6 hours, for multiparous women – up to 4 hours;
- long labor: for primiparous women – more than 20 hours, for multiparous women – more than 15 hours;
- cervical rigidity;
- history of vaginal delivery operations;
- surgeries that speed up labor;
- premature rupture of amniotic fluid;
- large fruit, weighing more than 4 kg.
Are there any consequences for the pathology?
Rupture of the cervix during childbirth has extremely unpleasant consequences. Of course, most women manage to avoid this phenomenon. To do this, you need to listen to the doctor during the process. However, a representative of the fairer sex who is preparing to become a mother should know what a cervical rupture during childbirth can lead to. The consequences will be described below.
Signs of pathology largely depend on the causes of this phenomenon and its degree. This often occurs while a woman is giving birth, but can also occur after labor.
Signs of a rupture include:
- The first sign is the development of bleeding. Based on the size of the uterine damage, bleeding can be small or heavy - especially often, a woman experiences blood discharge with clots. In addition, the patient may complain of pallor, weakness and profuse sweating. With minor injuries to the uterus, there are often no symptoms.
- If the damage occurs during childbirth, the woman will behave too restlessly, and labor will be characterized by excessive activity and painful contractions.
- The uterus becomes like an hourglass, and swelling also appears on it, which also spreads to the vaginal cavity.
- If the rupture has just begun, the clinical picture is accompanied by convulsive contractions, blood in the urine, as well as discharge mixed with blood.
- After a violation of integrity has occurred, which is accompanied by a sudden burning sensation and severe pain, the contractions stop.
As a result of painful shock, the patient may experience:
- nausea turning into vomiting;
- heavy sweating;
- pale skin;
- rapid pulse;
- decrease in blood pressure.
After the integrity of the cervix is violated, the fetus can be palpated in the peritoneum. This complication often leads to the death of the baby, since his heartbeat in this position cannot be heard.
Many women ask the same question - is it possible to give birth again and how successful will childbirth be after a cervical rupture. However, we must remember that only proper treatment will avoid problems, as well as normalize the health of the genital organs.
The consequences of this pathology depend primarily on the severity of the rupture and the assistance provided. Diagnosing a cervical rupture is quite simple. Usually, if it occurs, the woman begins to bleed, but not always. In modern maternity hospitals, every woman is examined; with the help of mirrors, doctors detect postpartum pathologies on the cervix.
If the sutures are applied incorrectly (or a cervical rupture is not detected), then the woman faces very unpleasant consequences. The vaginal and uterine area may become inflamed; a damaged and improperly healed cervix may not be able to withstand subsequent births or even pregnancies, resulting in miscarriages or premature births.
Well, the most dangerous complication of an unsutured rupture is cervical inversion, which in the future can even cause cancer.
Damage to the cervix: treatment
The main treatment for cervical injuries is surgery. Suturing of cervical ruptures is carried out in all cases, except superficial ones, not accompanied by bleeding cracks. In case of severe bleeding, squeeze out the placenta and proceed to suturing. Suture of ruptures is performed under strict asepsis. The doctor exposes the cervix using vaginal speculum, then grabs it with special forceps by the front and back lips, moves it outward and pulls it in the direction opposite to the location of the existing gaps. The doctor places the first suture on the upper corner of the wound, while the suture captures the entire thickness of the tissue of the vaginal part of the cervix, excluding the mucous membrane of the cervical canal. When it is impossible to apply the first suture to the upper corner of the wound, apply one or two sutures closer to the upper corner in the area of the rupture, then tighten the threads and begin suturing the uppermost corner of the injury. The seam on each side is made at a distance of 0.5-1 cm from the edge to avoid cutting through the seam while tightening it.
Suturing the rupture stops the bleeding and also prevents the occurrence of parametritis. Unsutured ruptures can lead to the development of erosions, endocervicitis and ectropions of the cervix.
In case of a complicated rupture that extends to the parametrium and is accompanied by the formation of hematomas, transection is used to stop bleeding, remove the hematoma and suturing the rupture.
Types of uterine injuries
Uterine contusion
Hemorrhoids kill the patient in 79% of cases
The risk of such uterine injuries increases in pregnant women in proportion to the increase in gestational age. Isolated uterine bruises can provoke spontaneous abortion at any stage, premature placental abruption or premature birth. These complications are usually indicated by bloody discharge from the genital tract, abdominal pain, and increased uterine tone. In case of damage to the chorionic villi, feto-maternal transfusion may develop, in which fetal blood enters the bloodstream of the pregnant woman. This condition is dangerous due to the development of fetal anemia, fetal hypoxia, and intrauterine death. With severe blunt trauma to the abdomen, ruptures of the liver, spleen, and uterus are also possible, resulting in massive intra-abdominal bleeding.
To determine the severity of the injury, the condition of the pregnant woman and the fetus, in addition to traditional physical and laboratory tests, a gynecological examination, ultrasound of the uterus and fetus, and CTG are performed. To detect blood in the pelvic cavity, culdocentesis or peritoneal lavage is performed.
Treatment of uterine injuries and their consequences is carried out taking into account the severity of the injury and gestational age. For mild bruises and early gestation, dynamic observation with ultrasound control and CTG monitoring can be carried out. When the pregnancy is close to full-term, the question of early delivery is raised. If blood is detected in the abdominal cavity, an emergency laparotomy is performed, stopping the bleeding and suturing the damaged organs. Feto-maternal transfusion may require intrauterine blood transfusion.
Uterine ruptures
Minor cervical ruptures may be asymptomatic. With extensive and deep defects, bright red bloody discharge appears: blood can flow out in a stream or be released with clots. Cervical ruptures are usually recognized clinically or by examining the cervix in a speculum. For such injuries, catgut sutures are placed on the cervix. If such uterine injuries were not detected in a timely manner or properly sutured, they may later be complicated by the formation of a hematoma in the parametrium, cervicitis, postpartum endometritis, ectropion and cervical erosion.
Uterine rupture is accompanied by acute cutting pain in the abdomen, pallor of the skin and mucous membranes, a drop in blood pressure, and cold sweat. If the rupture occurs during the active phase of labor, labor ceases. Signs of intra-abdominal bleeding and bleeding from the genital tract appear. Parts of the fetus are identified directly under the anterior abdominal wall. The general condition of the patient is extremely serious. Damage to the uterus by type of rupture is diagnosed on the basis of a general objective and external obstetric examination, ultrasound, and cardiotocography. In this case, immediate delivery by cesarean section and inspection of the uterus and abdominal cavity are indicated. Possible surgical treatment options are suturing the rupture, supravaginal amputation, or radical removal of the uterus.
Perforation of the uterus
When the uterine wall is perforated by a surgical instrument, intra-abdominal or mixed bleeding develops. Patients experience sharp pain in the lower abdomen, complain of bleeding, dizziness and weakness. With massive internal bleeding, arterial hypotension, tachycardia, and pale skin are noted. Along with damage to the uterus, injury to the bladder or intestines may occur. The most common complication of uterine perforation is peritonitis.
Perforation of the uterine wall can be recognized during intrauterine manipulation by characteristic signs (a feeling of “failure” of the instrument, visualization of intestinal loops, etc.). The diagnosis in this case is confirmed by hysteroscopy and transvaginal ultrasound of the pelvic organs. The main method of treating penetrating uterine injuries is surgical (suturing the rupture, subtotal or total hysterectomy).
Uterine fistulas
Abdominal-uterine fistulas connect the uterine cavity with the anterior abdominal wall and are classified as external. The outlet of the fistula often opens in the area of the suture or postoperative scar. The presence of a fistula is supported by inflammatory infiltration of the fistula tract. It manifests itself as periodic discharge of blood and pus through the skin opening of the fistula. Fistulas are detected during examination and hysteroscopy. Treatment is excision of the fistulous tract and suturing of the uterus.
The main signs of a vesicouterine fistula are cyclic menouria (Yussif's symptom), urine discharge from the vagina, a symptom of “stacking” a stream of urine when blood clots form in the bladder, and secondary amenorrhea. Ureteral-uterine fistulas are manifested by urine leakage from the vagina, lower back pain, and fever caused by hydroureteronephrosis. Genitourinary fistulas are detected during examination of the vagina in speculums, cystoscopy, and hysterography. Treatment is surgical closure of fistulas (fistuloplasty), ureteroplasty.
Uterointestinal fistulas can be a consequence of perforation of the uterus with damage to the intestine, or a breakthrough of an abscess into the intestine that developed after a conservative myomectomy or cesarean section. The course of intestinal-uterine fistulas of inflammatory origin is recurrent. Before the abscess breaks into the large intestine, pain in the lower abdomen, hyperthermia, chills, and tenesmus increase. Mucus and pus appear in the stool. After the abscess empties, the patient's condition improves. However, due to the fact that the fistula opening quickly undergoes obliteration, pus soon accumulates again in the abscess cavity, which causes a new exacerbation of the disease.
For diagnosis, examination of the vagina using speculum, combined gynecological ultrasound, rectovaginal examination, sigmoidoscopy, fistulography, CT and MRI of the pelvis are used. Tactics for pathology of this kind are only surgical; includes “intestinal” and “gynecological” stages. The details of the intervention are determined by the operating gynecologist and proctologist. Excision of necrotic tissue and restoration of intestinal integrity is usually combined with supravaginal amputation or hysterectomy.
Chemical and thermal damage to the uterus
In the acute period after damage to the uterus of this kind, the clinical picture of endomyometritis develops. Worries include an increase in body temperature, pain in the lower abdomen, and sometimes bloody discharge caused by rejection of the necrotically altered uterine mucosa. Such injuries can be complicated by peritonitis and sepsis. After healing of thermal and chemical damage, cicatricial changes in the cervix, atresia of the cervical canal, and intrauterine synechiae can form. In the long term, the development of hypomenstrual syndrome or amenorrhea and infertility is likely.
Diagnosis is based on clarifying the medical history (detecting the fact of insertion of hot solutions or chemicals into the vagina), examination of the cervix in speculum, and gynecological ultrasound. Treatment is detoxification and antibacterial therapy. With the development of peritonitis, laparotomy, sanitation and drainage of the abdominal cavity are performed; in case of extensive necrotic damage to the uterus - extirpation of the organ. Subsequently, to restore the patency of the cervical canal, it is bougienage. In Asherman's syndrome, hysteroscopic division of synechiae is indicated.
Prevention
The main prevention of cervical ruptures is the correct course of labor, which largely depends on the woman in labor. Doctors strongly recommend listening to your body and the advice of obstetricians. At the beginning of labor, it is important to withstand the first periods of pushing until full dilation (that is, do not push) and breathe correctly.
Also, for prevention, it is recommended to use antispasmodic drugs that will promote dilatation of the cervix, if necessary, anesthetize labor, and most importantly, try to foresee possible infringement of the cervix.
Have an easy birth without any ruptures!
Preventive measures to prevent injury to the cervix include both the professional actions of the doctor and the attentive attitude of the mother to her health. When planning a pregnancy, it is necessary to carefully examine and treat all chronic diseases.
To prevent cervical ruptures during childbirth, you should do special gymnastics to strengthen the vaginal muscles, take vitamins and minerals, eat right and get proper rest. It is recommended to enroll in courses for expectant mothers.
Proper breathing plays an important role. Timely breathing movements of sufficient depth and rhythm reduce pain and allow you to concentrate on labor.
To reduce pain and prevent premature pushing, painkillers are used. In order to ensure normal dilatation of the uterus, antispasmodics are prescribed.
The obstetrician leading the birth should not make sudden movements when using medical instruments or removing the fetus during breech presentation, since injury in such situations is almost inevitable.
It should be taken into account that in patients with a history of damage to the reproductive organs, the risk of recurrence of the situation increases significantly.
To ensure that subsequent births after cervical rupture occur without serious consequences, the woman should follow all the recommendations of the obstetrician-gynecologist. Coherence in the team of doctors and women in labor is the key to a natural birth with a favorable outcome.