Why does itching occur?
Currently, there are different theories among specialists that explain the origin of itching. Of these, the most popular are the following:
- 1This is a type of pain. It is believed that it appears as a result of mild irritation of normal pain receptors.
- 2This is an independent sensation. Some experts believe that there are specific receptors in the body, the irritation of which prompts a person to itch. Receptors can be irritated by chemicals and nerve impulses.
As observations have shown, there are a number of substances, with an increase in the concentration of which, itching may appear or intensify - histamine, serotonin, adrenaline, kallikrein, substance P, opioids, cytokines, growth factors, eicosanoids and others. Heredity is also believed to play a role.
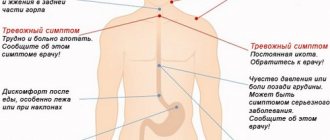
Sometimes itching is one of the symptoms of diseases of the internal organs or stress. He can be:
- 1Acute/chronic.
- 2Limited (local)/generalized (affects different parts of the body).
- 3Continuous/periodic.
- 4Weak/moderate/strong.
- 5With a known cause/idiopathic (the cause of which has not been established).
- 6Occurs in isolation/together with other symptoms: discharge, pain and cutting, rash, and so on.
https://youtu.be/lvYqB7tLauk
Internal predisposing factors
Endogenous causes that provoke the appearance of painful and tickling sensations in the intimate area of women are divided into two main groups - diseases of a gynecological nature and pathologies not related to the female reproductive system. Each of them contains a fairly large number of subparagraphs. Ailments associated with the gynecological sphere occupy a major place in the development of this scourge.
Almost any infection that develops in this area causes an itching effect in the vagina or outside the labia. The outer cover of the intimate area is populated by a large number of opportunistic microorganisms, which under normal conditions are completely safe, but under certain circumstances can provoke the development of an unpleasant disease. As soon as factors appear that lead to their increased reproduction, women develop the following diseases that cause the genitals to itch incredibly:
- Candidiasis caused by yeast-like microorganisms. More often, representatives of the fair sex call this pathological phenomenon thrush due to the abundance of white thick discharge that accompanies unpleasant vaginal itching.
- Colpitis, vaginitis and vulvovaginitis, which are bacterial in nature. With these ailments, tickling and painful sensations in the intimate area occur simultaneously with the appearance of thick grayish discharge from the vagina with a fishy odor. These gynecological pathologies are caused by opportunistic coccal microorganisms that have entered the active phase.
- Vaginal dysbiosis. This pathological disease, which always causes quite severe or mild itching, if adequate treatment is not carried out, eventually develops into bacterial vaginosis, which is caused by a pathogenic microorganism such as gardnerella. A characteristic sign of misfortune is grayish discharge.
- Hormonal fluctuations that occur in women carrying a child or approaching menopause can also lead to a pathological phenomenon. Here is even more about dryness in the intimate area during menopause and treatment.
- Among the pathologies that are not related to the female reproductive system, but can cause night itching in girls, lichen sclerosus of the vulva is sometimes noted. This attack is caused by certain autoimmune diseases and is characterized by the appearance of a thickened area of skin in the genital area. This disease is accompanied not only by itching and burning of the affected area, but also by the appearance of acute pain in it, as well as excessive dryness.
This piquant symptom also appears in diseases that are not related to the intimate sphere, such as diabetes mellitus, leukemia, iron deficiency anemia, malignant tumors, and lymphogranulomatosis. All these diseases are very serious and pose a direct threat not only to the health, but in some cases to the life of the patient. That is why experts strongly recommend that if itching appears in a woman’s intimate organs, do not try to get rid of it on your own, but seek help from a doctor.
Itching in the intimate area
The intimate zone is a fairly broad concept, including the area of the vulva, perineum and vagina of a woman. Unpleasant sensations can be concentrated in only one of these zones or affect them all. Their localization is one of the main points in gynecology, allowing the doctor to establish the correct diagnosis.
2.1. Vagina
The intensity of vaginal itching depends on the cause that caused it. It can be quite weak, moderate with cervical erosions, age-related changes, and vaginitis.
Itching of moderate intensity is observed with allergies to latex, spermicidal creams, vaginal tablets and suppositories, severe itching with infectious diseases (thrush, trichomoniasis and other STDs, bacterial vaginitis).
In combination with a feeling of burning, dryness and discomfort in the absence of heavy discharge, it is characteristic of menopausal changes in the vagina, atrophic vaginitis. Against the background of white cheesy discharge it occurs with candidiasis, and against the background of creamy, watery, white-gray, green or foamy discharge - with gynecological inflammatory diseases (vaginitis, bakvaginosis, cervicitis, etc.) and STIs.
2.2. Vulva
Vulva is a collective term that includes the external female genitalia. These include the vestibule of the vagina with the Bartholin glands, the clitoris, the labia majora and minora, and the pubis. The vulva area also contains the external opening of the urethra (urethra).
Itching can be limited only to the vestibule of the vagina, and also spread to the lips small and large. The mucous membranes of the vulva can be very itchy with genital herpes, trichomoniasis, gonorrhea and thrush, and psychosexual disorders.
Moderate itching is observed with inflammatory diseases of the vulva (vulvitis), allergic reactions to underwear and hygiene products, urethritis, as well as with enterobiasis (pinworms). A special category consists of benign and malignant tumors, kraurosis of the vulva.
The skin of the pubis, inguinal folds and labia majora is very itchy due to the appearance of pubic lice and scabies, eczema, athlete's foot and other fungal infections (dermatomycosis). In this case, redness, weeping erosions and characteristic rashes are also observed.
Sometimes persistent, difficult-to-treat itching, extending far beyond the intimate area, is caused by the accumulation of metabolic products and bile acids in the body against the background of kidney or liver failure or oncology. This condition is painful for a woman.
2.3. Crotch
This is the area of the intimate zone located between the genitals and the anus. Itching in the perineum can be caused by fungal and allergic skin diseases, general somatic pathology (for example, diabetes mellitus, liver disease, kidney disease), benign and malignant tumors of the rectum and pelvic organs, helminths (pinworms), scabies mites.
“Bumps” due to hemorrhoids, anal fissures, and healing wounds can itch in the anus area.
Combined itching, covering the entire intimate area, is characteristic of helminthic infestations, herpetic and fungal infections, skin diseases and advanced forms of STIs.
Factors contributing to the occurrence of genital itching and burning
The most common causes of itching in the intimate area are:
- STDs, including gonorrhea, trichomoniasis and chlamydia, ureaplasmosis, genital herpes;
- Fungal infection (candidiasis, mycoses);
- Parasitic diseases: pubic lice (pediculosis), scabies, helminths;
- General, infectious diseases, hepatitis and pyelonephritis;
- Disorders of the endocrine glands - diabetes mellitus, obesity, menopause;
- Diseases of the ovaries, prostate;
- Atrophy of the vaginal walls in old age, as well as in cases of local blood supply disorder;
- Disturbances of the normal anatomical structure of the vagina - prolapse of the walls, gaping of the vulva, damage to the mucous membrane (careless medical manipulations during douching, examination, abortion);
- Allergy to latex condoms, medications, vaginal preparations, intimate hygiene products, scented pads;
- Violation of sexual hygiene;
- Hypothermia and stress.
All factors lead to changes in the biocenosis (the ratio of beneficial and pathogenic microflora) of the genitals and to the development of inflammatory processes.
Women complain of itching and burning in the perineum with inflammation of the vagina (vaginitis or colpitis), clitoris and labia (vulvitis), as well as with vulvovaginitis, which combines symptoms of both diseases. Problems appear at any age, but are more common in women 18-45 years old.
Main reasons
The appearance of itching in women and men indicates some kind of malfunction in the body. There are more than a hundred reasons responsible for its occurrence: for example, it could be a reaction to washing powder or new underwear, as well as an undiagnosed infection or diabetes.
In addition, itching in intimate places can occur due to insect bites, natural changes during pregnancy, the menstrual cycle or climate change.
However, usually itching still indicates the presence of some kind of disease, problems with hygiene, or a change in usual lifestyle. Therefore, it is important to promptly consult a gynecologist for medical help.
Treatment with folk remedies
When burning and itching is observed in the intimate area in women, treatment can be done at home using unconventional methods.
However, they can only relieve the symptoms of inflammation and improve the patient’s well-being. Non-traditional methods cannot get rid of the main disease. Their use will bring results only when they are used as part of complex therapy, after consulting a doctor. How to get rid of itching in an intimate place in unconventional ways:
- using douching, tampons soaked in the product;
- if you make compresses;
- take medications orally;
- make baths.
The following alternative medicines help well:
- herbal decoctions and infusions;
- solution of soda with fir oil;
- carrot juice;
- milk with garlic;
- aloe vera pulp;
- sea buckthorn oil;
- tandem of salt and iodine;
- propolis ointment.
A couple of useful recipes:
- Douching is done before bed with a soda solution. To prepare it, 1 tsp. sodium carbonate is diluted in 1 liter of water. After this, a tampon is applied, lubricated in a mixture of butter and fir oil. To prepare the product, take 50 g of the first ingredient and 5 g of the second. Everything is mixed until smooth and heated in a water bath. The product can only be used after it has cooled. Several days should pass between applications.
- Sea buckthorn, thyme, and tea tree oils help well in the fight against the pathological condition of the genitals. You need to prepare a mixture from them. Take 1 part of thyme oil, tea tree oil and 5 parts of sea buckthorn raw materials. Mix everything thoroughly and add a few drops of sage. A tampon is moistened in the resulting product and inserted for 3 hours.
To prevent the occurrence of unpleasant phenomena, you need to carefully observe hygiene. Wash yourself and change your panties daily. Avoid sex without condoms. Treat concomitant diseases in a timely manner. Eat healthy foods and give up alcohol, nicotine, and drugs. The stronger your immunity, the lower the risk of difficult-to-treat pathologies.
Changes
4.1. Contact allergy
Quite often there is an allergic reaction from the genital organs to intimate hygiene products or the material from which underwear is made. In this case, the mucous membrane of the vulva and vagina is itchy and itchy, there may be redness and slight swelling.
Another case is intolerance to the powder used in washing. Sometimes women notice the appearance of symptoms when using scented sanitary pads and tampons.
4.2. Irritation after shaving
The main source of itching in this case is growing hard hairs that resemble stubble. As a rule, itching occurs mainly in the pubis, the skin of the labia majora and the inguinal folds in contact with them.
The sensation intensifies when wearing tight, waterproof underwear, increased humidity and infection. A careful examination may reveal irritation, moderate redness of the skin, and ingrown hairs.
4.3. Low level of hygiene
Even physiological secretions from the genital tract under the influence of the environment can become a good environment for the proliferation of microorganisms. The situation is aggravated by dirt or dust, as well as exfoliating epithelial cells.
As a result, inflammation develops, leading to tissue damage. It is accompanied by burning, pain and itching. In this case, the symptoms are localized in the area of the vaginal vestibule, labia minora, and clitoris. The discharge changes color and smell.
You can avoid such feelings by following these simple rules:
- 1Change underwear daily.
- 2Wash yourself at least once a day, using special hypoallergenic intimate hygiene products or running clean water.
- 3It is important not to scratch the skin and mucous membranes (it is better to simply wash with cool water and consult a doctor).
- 4During menstruation, pads should be changed as often as possible.
- 5Make sure that the fabrics from which the underwear is made absorb moisture well and allow the skin to “breathe”. It is optimal to use white, cotton panties.
What to do at home
How to treat itching and burning in the intimate area in women? You can eliminate the negative effects of itching and burning itself by following some simple tips.
- When washing the problem area, you can add a small amount of furatsilin to the water.
- It is important to change your underwear several times a day.
- If it's summer outside, you need to minimize your time in the sun.
- Follow your diet and review your diet. It is necessary to exclude from your menu all spicy dishes, as well as various pickled foods. Eat more dairy products, vegetables and fruits.
- When choosing underwear, you should give preference to cotton options.
- During the itching, you should limit yourself in your sexual life. You should also not visit public places - swimming pools, saunas and others.
- Protect yourself from stress and psycho-emotional stress. They can only increase itching and discomfort in the female area.
Timely diagnosis of itching and proper treatment contribute to a quick end to the discomfort. If self-treatment does not produce a positive effect, you should immediately consult a doctor, who will examine the itching in more detail and prescribe all the necessary manipulations.
Physiological conditions
5.1. Pregnancy
Slight itching during pregnancy may occur due to changes in hormonal levels, leading to a decrease in the sensitivity threshold. However, the most common causes of its occurrence are thrush (candidiasis) and bacterial vaginosis. It usually itches the vagina and vulva area.
5.2. During your period
Discharge during menstruation is sometimes accompanied by moderate itching in the vagina and its vestibule. This is due to their irritating effect, especially when sanitary pads and tampons are rarely changed.
In addition, during this period, existing gynecological and venereal diseases worsen, so the entire intimate area may “itch” (this depends on the nature of the lesion and the intensity of the symptoms of a particular disease). To understand the nature of the itching and rule out possible infections, consult a doctor.
5.3. Ovulation
During ovulation, the discharge becomes most abundant and watery. They increase moisture in the area of the groin folds and labia and can cause itching, and tight underwear and shaving further aggravate the situation. Normally, symptoms should be short-lived and disappear at the end of the cycle.
5.4. After intercourse
After unprotected sex, a common cause of discomfort in the vagina, vulva and inguinal folds are STIs, as well as the reaction of the mucous membranes and skin to the partner’s sperm and microtrauma (during anal sex, itching can be in the anus and perineum).
Less commonly, symptoms after intimacy occur due to allergies to sperm proteins, barrier contraceptives, including condom latex.
5.5. Climax
Vulvovaginal itching during menopause is caused by the extinction of ovarian activity and corresponding hormonal changes.
A woman develops dry mucous membranes, soreness and increased vulnerability of the mucous membranes of the genital tract.
Preliminary diagnosis depending on the color of the discharge
It will not be difficult for an experienced doctor to make a preliminary diagnosis based on the patient’s complaints, if the woman’s discharge is not transparent and is accompanied by itching, and there is an unpleasant odor. The gynecologist conducts an examination and evaluates the nature of the vaginal secretion - its color, consistency, thickness.
White
The patient should be wary if she suddenly experiences itching in the intimate area and discharge with a sour odor - these are the first signs of infection with thrush.
The released secretion particles have the following characteristics and are accompanied by symptoms:
- curdled consistency;
- pungent aroma of sour milk;
- the intimate area is very itchy, the feeling of discomfort increases when going to the toilet and having sexual intercourse;
- the skin of the external genitalia is red and swollen.
You should be wary of discharge that contains inclusions in the form of foam, mucus, lumps and scales, as well as their sharp unpleasant odor. If vaginal secretions acquire a pronounced aroma of rotten fish or missing eggs, this may signal the development of bacterial vaginosis and trichomoniasis.
Leucorrhoea, accompanied by itching and burning, often begins to bother women who do not follow the rules of personal hygiene. In the absence of regular washing (twice a day) with warm water and soap, active reproduction of pathogenic flora begins and erosion of the mucosal epithelium by droplets of remaining urine.
Yellow
In cases where a woman experiences strong pathological discharge and intense itching, this phenomenon is not normal - the symptoms indicate a pathology that needs to be treated urgently.
The most common causes of yellow discharge and a constant desire to scratch the skin in the intimate area:
- disruption of the normal balance of vaginal microflora;
- inflammation of the appendages (salpingoophoritis);
- vaginosis of bacterial nature;
- one of the sexually transmitted diseases - chlamydia, trichomonas;
- large cervical erosion.
Different types of pathologies are accompanied by their own varied symptoms, from discharge of an unusual color with an unpleasant odor to pain in the lower abdomen, fever and a sharp deterioration in general well-being.
Brown
Patients who regularly experience itching and brown discharge even after menstruation are advised to undergo an urgent examination - the causes of the symptoms can be either an incorrectly installed coil or cancerous tumors.
The coloring of the secretion in a brown tint indicates that bleeding is occurring in the organs of the reproductive system. Due to the small volume of its secretion, blood has time to coagulate inside the vagina before coming out.
These symptoms may indicate pathologies:
- Damage to the vaginal epithelium or internal uterine layer as a result of violation of surgical technique, careless insertion of a tampon. The symptoms of discomfort disappear on their own after a couple of days, if the damage is not severe. When the injury to the mucous membrane is severe, itching and infection are added to the blood secretion.
- Inflammation of the uterus and vaginal walls - the infectious process makes the mucous tissue very sensitive, which is why it can bleed even without touching sharp objects.
- Violations in the technique of installing the coil - excessive bleeding indicate an actively developing inflammatory process that requires urgent antibacterial therapy.
- Dysbacteriosis of the vaginal environment.
- Growth of condylomas on the labia.
- Cancerous tumors - vulva, cervix, vagina.
- Gonorrhea.
Pubic lice may be to blame for the appearance of itching and severe redness in the intimate area in women without any discharge - due to constant scratching of the skin, bleeding wounds appear.
Greens
A green tint to vaginal mucus appears when an acute inflammatory process is actively developing in the organs of the reproductive system - it is imparted by leukocytes present in large numbers in the microflora. They die trying to suppress infectious agents on their own, which is why such a secretion is called leukorrhea.
If, in the presence of green discharge mixed with pus, a woman does not immediately consult a doctor, there is a high risk of death due to blood poisoning. The symptom indicates the following pathologies:
- acute inflammation of the appendages and uterus - occurs against a background of elevated temperature, fever and pain;
- chronic bacterial vaginosis;
- long-term and indolent trichomonas infection.
Itching in the genital area forces a woman to scratch the skin, as a result of which the process of reproduction of pathogenic microbes only worsens. Treatment of severe infection often requires hospitalization due to the high risk of complications and sepsis.
Diseases
6.1. Thrush (candidiasis)
The main symptoms of the disease are severe itching in the vagina, vulva area and white, crumbly, cheesy discharge with or without a slight sour odor.
Often occurs during pregnancy, decreased immunity, after antibiotics, or taking systemic glucocorticosteroids. Sometimes the process involves the inguinal folds, anus, and urethra, and additional symptoms include burning and pain.
6.2. Bacterial vulvovaginitis
Itching in the genital area, unpleasant odor and purulent, mucous discharge are characteristic signs of inflammation caused by cocci, gardnerella, E. coli and other enterobacteria. A woman may also experience a burning sensation, pain during sexual intercourse, and discomfort.
6.3. Urethritis
With urethritis, during urination, urine provokes irritation of the mucous membrane of the urethra, resulting in pain, burning or itching. A similar situation occurs when fistulas occur connecting the vagina to the bladder or ureter.
6.4. Sexually transmitted infections (STIs)
This is one of the most common causes of itching in the intimate area. The symptom is characteristic of gonorrhea, donovanosis, trichomoniasis, syphilis and other similar infections. As a rule, typical discharge and other signs are observed.
The classic symptoms of genital herpes are the formation of transparent blisters, which open after a few days, leaving weeping erosions in their place. All this is accompanied by a burning sensation and severe pain.
However, there is also an atypical “itchy” form of the disease, when, against the background of slight redness of the genital organs, severe local itching and burning occurs. As a rule, with a herpetic infection, the vagina, vulva area, and perineum may itch.
6.5. Parasitoses
The pubis and skin of the labia majora can be affected by pubic lice (phthiriasis) or scabies mites (scabies). Another common cause of itching in the genital area is helminthic infestations, in particular pinworms (enterobiasis).
6.6. Neuroses and psychogenic diseases
Sometimes unpleasant symptoms occur due to stress or nervous shock. As a rule, in this case, during a gynecological examination, no signs of any pathology are detected (itching without discharge, changes in their color and smell).
A special category is neurosexual disorders, in which case sensations occur in any area: in the vagina, perineum, and throughout the intimate area.
6.7. Endocrine disorders
Itching in the labia area, in the vagina and its vestibule occurs with diabetes mellitus, ovarian hypofunction, and thyroid diseases.
6.8. Eczema
Unpleasant sensations with eczema are very pronounced, localized in the area of the pubis, labia, inguinal folds, perineum and spread to other areas. You can also see redness, painful cracks, merging and weeping wounds on the skin.
6.9. Fungal skin infections
In the intimate area, dermatitis can be caused by fungi such as Candida, Microsporum, Trichophyton and Epidermophyton floccosum. They are the cause of inguinal candidiasis, athlete's foot and ringworm. Their characteristic symptoms:
- 1Ringworm is an intensely itchy reddish-brown rash in the form of rings with scales and blisters that spreads to the buttocks and genital area.
- 2 Candidiasis - occurs in the area of the inguinal folds, where skin friction and damage occurs. It becomes covered with weeping cracks with a white coating and redness of the surrounding tissues. As the disease progresses, the itching becomes obsessive and unbearable.
- 3 Athlete's foot - pink spots and blisters with exudate form in the area of the perineum and inguinal folds. Severe itching and pain occurs.
Common causes of itching in the genital area in women
Gynecologists say that burning and itching in the intimate area in women without discharge rarely appears, for physiological reasons that do not require treatment; in other cases, there is vaginal secretion with a changed color and smell. Many pathologies that manifest themselves against the background of itching and unusual discharge can be dangerous to women’s health and lead to a number of complications:
- obstruction of the fallopian tubes;
- formation of adhesions in pipes;
- infertility;
- severe hormonal imbalances.
As a result of ignoring the symptoms, when the skin in the external genital area becomes red and itchy, chronic inflammation develops. Even when symptoms subside over time, you should not assume that the disease has gone away on its own. At this time, if there is a sexually transmitted infection, the woman is its source and can infect her partner the first time.
Thrush
The main symptoms of a fungal infection or thrush are itching in the intimate area and a white, curd-like discharge. If candidiasis affects only the vagina, vaginitis occurs; if the vulva is involved in the process, a diagnosis of vulvovaginal candidiasis will be made.
Reasons for the development of thrush:
- uncontrolled use of antibacterial drugs (a month or longer);
- a sharp decrease in the body’s protective function due to stress, colds, local or general hypothermia;
- infection from a partner;
- abuse of baked goods, baked goods, carbonated drinks - a sweet environment is favorable for the growth of fungi;
- hormonal disorders.
When girls ignore this condition and do not turn to specialists for a long time, the symptoms are supplemented by nagging pain in the lower abdomen and discomfort during sexual intercourse.
Bacterial vaginosis
As a result of this pathology, the natural balance of the microflora of the vaginal mucosa is disrupted - beneficial lactic acid bacteria become scarce, and pathogenic ones begin to actively multiply. With bacterial vaginosis, a woman begins to experience itching in intimate places, there is a discharge that smells unpleasant and changes color.
Normally, leucorrhoea is transparent and has a slight sour odor.
The discharge becomes dirty gray, greenish, may foam, and takes on the smell of rotten fish if vaginosis is diagnosed. The skin in the vaginal area becomes swollen, and diffuse redness is observed. Chronic inflammation leads to damage to the appendages, cervix and uterus, which is why it is important to start treating the disease in time by consulting a doctor.
Sexually transmitted diseases
The main reason for contracting a sexually transmitted infection is promiscuity. Adult women are recommended to be examined by a gynecologist twice a year, take blood tests for STDs and a smear to determine the degree of purity. If itching and redness against a background of suspicious discharge are found in a 14–15 year old girl, parents should urgently show her to a dermatovenerologist, since the transition of a venereal disease to a chronic form is fraught with infertility.
Severe itching and leakage of copious amounts of vaginal mucus are signs that occur with sexually transmitted infections:
- Ureaplasmosis, chlamydia - the secretion becomes thick and viscous, acquires a cloudy white tint, lumps and flakes may be present.
- Gonorrhea - the uterus secretes yellow or green mucus with purulent patches, itching of the skin, redness of the mucous membrane, and pain in the urethra when going to the toilet appear.
- Trichomoniasis - a flow of liquid, foamy mucus of a dirty gray color with a sharp, unpleasant smell of rotten meat is recorded.
It is forbidden to try to eliminate itching and leakage of mucus on your own, at home, if you suspect a sexually transmitted infection.
It is necessary to take blood tests using the PCR method to accurately identify the causative agent of the disease and follow the doctor’s instructions in therapy. STDs are especially dangerous during pregnancy because they can cause abnormal fetal development and miscarriage.
Cervical erosion
Changes in the structure of the uterine cervix begin with constant leucorrhoea, if the girl does not pay attention to them and does not visit a gynecologist for preventive purposes. Regular irritation of the sensitive mucous membrane leads to erosion of the cervix and the formation of ulceration on it - erosion.
Similar phenomena are observed with bacterial vaginosis and chronic thrush. If the diagnosis of erosive cervix is complemented by an inflammatory process, the woman experiences severe itching, but the secretion coming out of the vagina does not smell or change color. The amount of discharge increases before the onset of menstruation.
Diseases of the pelvic organs
Important factors in why a girl’s intimate area itches and white discharge bothers her are systemic diseases accompanied by similar symptoms:
- diabetes;
- cancerous tumors;
- leukemia.
The course of these diseases affects the general condition of the body, and the reproductive system is no exception. If a woman constantly complains to the doctor about severe itching in the groin and unclear vaginal secretions, the specialist should recommend that she undergo examination for the listed pathologies.
The first signs of the growth of a malignant tumor in the pelvis, in addition to the desire to scratch the skin in the groin, are increased fatigue, acute inflammation in the body for no specific reason, and changes in blood tests.
Endocrine system disorders
Often itching and uncharacteristic vaginal discharge are provoked by hormonal imbalance in the premenopausal period or during menopause itself. The adrenal glands and thyroid gland disrupt their functions, and a simultaneous lack of estrogen affects the normal hydration of the vaginal mucosa. Itching and burning occur. The same symptom is observed in women with an unstable monthly cycle.
Hormonal levels can be affected by constant stress, autoimmune diseases, due to a sharp decrease in immunity, and also if there are hereditary pathologies. A rare disease is lichen sclerosus of the vulva - the patient experiences intense itching in the groin without leakage of mucus and swelling of the skin of the labia minora.
Allergy
Severe itching in a woman’s perineum and leakage of watery secretions may be associated with an allergic reaction to the following irritants:
- intimate hygiene product;
- pads with aromatic fragrances;
- poor quality underwear material;
- vaginal suppositories.
An allergy can even develop to the sperm of a sexual partner. Sensitization can be distinguished from other pelvic diseases by pronounced redness and dryness of the skin on the labia minora and majora, which disappear only after taking antihistamines.
Cystitis
The inflammatory process in the bladder is manifested by the following symptoms:
- acute pain in the lower abdomen;
- increased urge to urinate;
- pain in the urethra when going to the toilet;
- white, yellow-green discharge mixed with pus.
The secreted mucus dries on the skin; in the absence of regular hygiene, it accumulates in the folds of the groin, causing unbearable itching.
Diagnostic methods
Due to the variety of causes of itching and gynecological diseases, a whole team of doctors is often involved in the examination:
- 1Gynecologist.
- 2Endocrinologist.
- 3Allergist.
- 4Dermatovenerologist.
- 5Neurologist.
- 6Therapist.
If necessary, consultations with an oncologist, hepatologist, nephrologist, hematologist, psychotherapist, infectious disease specialist and other highly specialized specialists are also scheduled. For in-depth laboratory and instrumental diagnostics, the following is prescribed:
- smear on flora and GN;
- STI tests using PCR;
- smear for oncocytology and colposcopy;
- Ultrasound of the pelvic organs;
- blood tests (general, biochemical), urine;
- stool examination for the presence of hidden blood, helminth eggs, coprogram, scraping for enterobiasis;
- study of hormonal profile and immunological status;
- allergy tests and other studies as indicated.
Drugs for treatment
First of all, it is important to eliminate any provocateurs of itching:
- Synthetic underwear, aggressive depilation.
- Scented sanitary pads.
- Replace washing powder, soap, and intimate hygiene products with hypoallergenic ones.
- Remove allergenic foods from your diet.
- Review medications taken based on possible adverse reactions.
- Change barrier contraception and so on.
Along with this, it is necessary to influence the very cause of unpleasant symptoms.
Depending on it, the doctor may prescribe the following medications:
- 1 Antihistamines: Desloratadine, Loratadine, Ketotifen, Fenkarol, Bikarven, Suprastin, etc.
- 2 Hormonal: Prednisolone, Dexamethasone, Hydrocortisone, Advantan, Elokom, etc.
- 3 Sedatives: Phenobarbital, Amizil, Benzoclidine, Seduxen.
- 4Sorbents: activated carbon, Polysorb, Smectu.
- 5Antibiotics, antiparasitic and antifungal drugs for local use and orally (as indicated).
After making a diagnosis, the attending physician prescribes appropriate therapy.
Treatment of itching depending on the cause
| Disease | Drugs |
| Pubic lice | Paranit, Nittifor, Pedilin |
| Scabies | Benzyl benzoate, Spregal |
| Atrophic vaginitis | Ointments and suppositories with estrogen |
| STI | Antibiotics and antivirals depending on the type of infection. Both partners need to be treated. |
| Thrush | Locally - Clotrimazole, Pimafucin, Butoconazole (Ginofort), Miconazole (Ginezol 7); orally - Fluconazole (Flucostat) |
| Fungal skin infection | Ointments with glucocorticoids and antifungals - Triderm, Lorinden S, Akriderm GK, Kanizon Plus, etc. Orally - suprastin, tavegil, fenistil. |
| Liver diseases with cholestasis | Cholestyramine, naltrexone. Sedatives - phenobarbital. |
| Eczema, allergic dermatitis | Locally - ointments with glucocorticosteroids - Elokom, Advantan, Akriderm, etc. Orally - desloratadine, loratadine, cetirizine, etc. |
| Neurosis | Psychotherapy and distraction medications can relieve discomfort |
| Vaginitis | Clindamycin, Terzhinan, Neo-penotran, Polygynax, etc. |
Treatment
To eliminate itching in the intimate area, it is important to exclude all possible provocateurs of this sensation and refuse:
- underwear made from unnatural fabrics and aggressive hair removal methods;
- sanitary pads with aromatic effect;
- consumption of food allergens.
It is also recommended to change detergents to hypoallergenic ones, choose an appropriate method of barrier contraception, review the side effects of medications taken, etc.
Based on the cause of itching, therapy is selected using:
- antihistamines (suprastin, loratadine, etc.);
- hormonal drugs - prednisolone, dexamethasone, Elokom, etc.;
- sedatives - seduxen, phenobarbital, etc.;
- sorbents (smecta, enterosgel);
- antibiotics, antiparasitic and antimycotic agents of local or systemic action.
How can you treat yourself at home before consulting a doctor?
To get rid of itching while waiting for a doctor's appointment, you can use cold lotions and cool baths. Any creams and ointments that contain menthol, zinc, diphenhydramine can be applied to the skin (attention: not to the mucous membranes!!!). They have a distracting effect, somewhat improve well-being and do not interfere with the diagnosis:
- 1Tsindol, zinc ointment;
- 2Calamine, lotion;
- 3Menovazine, pharmaceutical menthol solution.
Ointments and gels with anesthesin and lidocaine can be used only in the absence of an allergic reaction to anesthetics. You should not use vaginal suppositories or douching before consulting a doctor; they make it difficult to make a diagnosis and identify an infection!
Folk remedies do not help cure the disease, so they cannot be used at home without examination by a gynecologist.
Itching and burning in the genitals as consequences of diseases of other systems and organs
You might be interested in:
- Herpes in women: symptoms and treatment
- Thrush: symptoms and treatment
- Syphilis in women: symptoms and treatment
- Chlamydia in women: symptoms and treatment
Itching and burning can be the consequences of certain diseases. Their appearance can signal the development of:
- Diabetes mellitus.
- Oncological tumors.
- Anemia.
- Leukemia.
- Lymphogranulomatosis.
- Hormonal disorders.
In order to get rid of the burning sensation, you must first cure the underlying disease.
Consequences
Itching, if left untreated or inadequately treated, can become a serious problem. It is capable of causing:
- insomnia;
- depression;
- depression;
- irritability;
- neurotic conditions;
- refusal to eat;
- decreased performance;
- social isolation.
When scratching, an infection gets into the wounds, inflammation develops, accompanied by pain, purulent discharge, the spread of rashes, and so on.
Some people with severe itching of the genitals try to fight it in a rather unique way: they use various objects that injure the skin and mucous membranes, which only aggravates the situation.