Syphilis is a chronic infectious disease caused by the spirochete pallidum (treponema); infection with syphilis most often occurs through sexual contact (“classic venereal disease”); Other routes of transmission of the pathogen are also possible: transfusion (such as a hospital infection), occupational (among medical workers). The disease can be transmitted from mother to fetus in the prenatal period - placentally, and this is the great insidiousness of this disease.
Syphilis can affect the skin, mucous membranes, bones, internal organs, and nervous system; proceeds in waves with a change of active and latent periods; Specific manifestations of infection may resemble other diseases.
A little history:
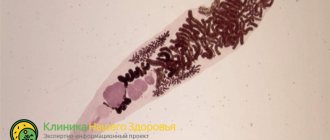
Treponema pallidum
For a long time, syphilis was not considered an independent disease. It was believed that syphilis, gonorrhea and chancroid were the same disease. Great confusion in the doctrine of syphilis was introduced by Genter. To prove the identity of syphilis and gonorrhea, he injected pus from a patient with gonorrhea into the glans penis and urethra. But the patient suffered from both syphilis and gonorrhea, so after 3 days gonorrhea developed, and after 3 weeks primary syphiloma appeared at the site of vaccination. This “experience” was so demonstrative and convincing, and Genter’s authority was so great that for more than 100 years it was believed that syphilis and gonorrhea were the same disease. Genter's mistake cost humanity dearly - the doctrine of syphilis as an independent disease was delayed for many years and went along the wrong path. Only in the 19th century did Ricor show that syphilis and gonorrhea are independent diseases; at the same time, he proved this in a cruel and inhumane way - he mass-infected “volunteers” with 600 people with syphilis and 800 people with gonorrhea. At the cost of their lives and health, he gained fame, without taking into account the future fate of these people - in the absence of effective treatment in those years! Ricor also identified three periods of syphilis (this division is still used today).
What is household syphilis
Transmission of treponema pallidum in everyday life, and not through sexual intercourse, is called household syphilis.
As a result of infection, the pathogen affects all vital parts and systems of the body, and if left untreated for a long time, it can even cause death. The main difference between domestic syphilis and sexual syphilis is the route of its transmission. At the site of penetration of the pathogen, 1-2 months after contact with the patient, a hard chancre appears, from which one can judge how the infection occurred. With household syphilis, the rash can appear and be transmitted:
- lips through a kiss;
- oral cavity through shared dishes, a toothbrush or even a cigarette;
- any part of the body if there are wounds or microcracks.
Photo of manifestations of household syphilis.
In a dry environment, Treponema pallidum dies very quickly without a carrier and when exposed to high temperatures. So, when exposed to a temperature of +60°C, it dies within 15 minutes, and at +100°C - immediately. But with a humid environment and low temperatures, the danger of the pathogen does not decrease. Even at a temperature of -70°C, the virus can maintain its activity for 10 years.
https://youtu.be/h10tGVr_5is
Causative agents of syphilis
The causative agent of syphilis is the bacterium spirochete pallidum or treponema. This single-celled microorganism is known for being very mobile and, depending on the conditions of the reproduction environment, capable of modification and transformation. The risk of contracting syphilis is that often this disease is not the only sexually transmitted disease in the body of an infected person and goes undetected for a long time. As a result, the problem is misdiagnosed and, accordingly, treatment is ineffective.
Syphilis can also be contagious during the incubation period of its development in the body. Also, virus carriers in rare cases can be present in the body in a latent form and not have a pathogenic effect for a long time. Because of this feature, it is extremely difficult to determine the presence of syphilis in a timely manner.
How is household syphilis transmitted?
Household infection with syphilis involves the use of the same personal hygiene products with the patient (toothbrush, washcloth, razor, towel, comb, handkerchief, etc.), clothing and bed linen.
A common way to become infected is by smoking one cigarette, as well as through utensils. The following transmission routes are also no less dangerous:
- when infected parents sleep together with their children, as well as when children use common dishes and a bathroom:
- through a kiss;
- if a healthy person has condylomas lata, in this case Treponema pallidum can easily penetrate the body;
- through thin epithelium without damage;
- through wounds and microcracks in the skin;
- if precautionary rules are neglected during the analysis of blood, semen, smears of patients with syphilis (failure to use protective gloves or untimely replacement of them).
How is household syphilis transmitted? Using someone else's cosmetics is considered an equally dangerous way of infection. For example, lipstick or pencil, as the patient’s saliva may remain on them.
Can household syphilis be transmitted from child to mother during pregnancy? Yes, this type of transmission is considered the most dangerous. When consumed, the danger is not for the mother, but for the child. Infection usually occurs in the last months of pregnancy through the placenta or blood. The risk of premature birth or miscarriage increases significantly.
During infection of the fetus, Treponema pallidum destroys bone tissue, brain and internal organs. Very often the child is stillborn. If the child does survive the infection, he is born with a rash all over his body, as well as scars and wounds. Such children have pathologies of the eyes, legs, heart and liver, as well as inflammation of the brain tissue and deformation of the skull, teeth and nose. They are significantly behind in physical and mental development. If fetal disease is detected early in pregnancy, a favorable outcome is possible.
Ways of transmission of syphilis:
The causative agent of syphilis is a pale spirochete or treponema (treponema pallidum), which apparently belongs to the class of protozoa
Infection in most cases occurs from patients with active infectious manifestations of syphilis. Consequently, the source of infection with syphilis can only be a sick person; under natural conditions, animals do not suffer from this disease; it is difficult to reproduce in experiment.
The most dangerous for transmission of infection are patients with active - weeping, eroded manifestations, whose discharge contains a large number of treponemes. In this case, the main route is infection through sexual contact, incl. through the rectum. Direct contact also occurs through kisses, bites, etc. Consequently, the most contagious are syphilides that lack epithelium (or the upper layers of the epidermis); their number matters, as well as the frequency, duration and type of sexual intercourse.
Intrauterine infection of the fetus is possible (see syphilis during pregnancy).
Extrasexual transmission is rare.
It is generally accepted that for infection to occur, damage to the skin is necessary (there may be microtraumas not visible to the naked eye!). In this case, a violation of the integrity of the skin creates an “entry gate” for the causative agent of syphilis; transmission of infection is also facilitated by the spiral shape of the spirochete and its movement (like a corkscrew) - which allows it to penetrate the tissue. Damage to the integrity of the skin, even extremely minor ones, may be sufficient for the penetration of the spirochete. Perhaps it is precisely the protective role of intact skin that explains the seemingly paradoxical fact - when out of 2 people who had contact with a woman (suffering from this infection) - one becomes infected with syphilis, and the other remains healthy. The situation is different with the introduction of the spirochete through the mucous membranes. Clinical observations and experimental data suggest that the pallid spirochete is capable of penetrating intact mucous membranes.
You should remember about the possibility of occupational infection (contact of medical personnel with the patient during examination and treatment procedures). Indirect contact and infection are possible through medical instruments (vaginal speculum, dental instruments), cigarette butts, spoons, mugs (variants of professional and household syphilis).
Under certain conditions, breast milk, sperm, blood (including menstrual blood), and cervical discharge can be infectious. Of interest is the fact that the pale spirochete can be found in patients with syphilis in the rash elements of concomitant skin diseases (psoriatic papule, genital warts, the contents of herpes blisters) - which makes them infectious under certain conditions.
If the infection occurs “bypassing” the skin and mucous membranes (usually by transfusion), then “decapitated” syphilis develops (begins with manifestations of the secondary period). Consequently, under special conditions of infection, the spirochete enters directly into the bloodstream (during blood transfusion, surgery, autopsy, etc.). At the same time, treponema pallidum can be detected in the blood of patients with syphilis at any period of the disease. However, their number varies depending on the period and duration of the disease. The more active the infection, the greater the number of treponemes in the patient’s blood. It is believed that in the latent period of the disease their number is significantly reduced, but it is sufficient to cause infection. In this regard, donors are subject to thorough examination. The problem can only arise with direct blood transfusion - in emergency cases - for health reasons.
Chancre
The incubation period for syphilis is on average 3-4 weeks. This is the time from the moment of infection to the first manifestations of the disease.
The incubation period can be shortened to 10-15 days (early incubation) or more often extended to 2-4 months.
An important role in prolonging the incubation period is played by the use (for various reasons) of antibacterial agents, especially with spirochetocidal and spirochetostatic effects (penicillins, cephaposporins, tetracyclines, macrolides, azalides, metronizadol, bismuth preparations, etc.). Used in smaller doses and with a different time interval, these drugs do not cure syphilis, but only prolong the incubation period and contribute to the transition of the spirochete into “survival forms” - one of the factors in the formation of seroresistance.
For example, when infected with syphilis and gonorrhea at the same time, the patient is prescribed antibiotics that cure gonorrhea, but do not prevent the occurrence of syphilis; At the same time, the incubation period of syphilis is prolonged. Therefore, patients with gonorrhea with an unknown source of infection (if dispensary observation is not possible) should undergo preventive antisyphilitic treatment. The rest (those with permanent residence) undergo clinical and serological monitoring for 3 months.
An extension of the incubation period can be observed in febrile conditions, mixed infections (gonococcal, trichomonas, fungal, etc.). The incubation period may vary in weakened individuals, with chronic diseases, immunodeficiency conditions, in the elderly, etc.
It should be noted that despite the absence of clinical symptoms of syphilis, treponema pallidum quickly moves away from the site of primary penetration, multiplying and spreading throughout the body, mainly through the lymphatic system. Moreover, the lymphatic system is not only a place of advancement, but also a place of reproduction of the pale spirochete. This is explained by the fact that lymph contains significantly less oxygen than arterial and venous blood (anaerobe spirochete). Therefore, the spirochete selectively lingers in the lymph nodes, survives in them longer than in other places, and resists treatment more stubbornly.
Experiments on animals have shown that if in the first hours (and even minutes) the site of spirochete insertion is excised, then this operation cannot prevent the disease. Thus, from the very beginning (from the first minutes after infection), syphilis takes on the character of a general disease. Unfortunately, there are known cases of infection through blood transfusions from persons who were in the incubation period (donors, before donating blood, even those who have done so more than once, must undergo a thorough clinical and serological examination).
Stages
It happens that syphilis has the same stages of development as syphilis during sexual contact.
That is, there are 3 main stages in which the symptoms and incubation period differ. An average of 14-60 days pass before the start of the first stage and from the moment of infection. It all depends on the person’s immunity and the presence of concomitant diseases.
The length of the incubation period is influenced by several factors. So, if during infection a person takes penicillin antibiotics, the incubation period can last up to six months. But with repeated infection, the duration of the latent period is reduced to 7-8 days. Stages of syphilis:
- Primary . It is characterized by the appearance of primary symptoms: a hard infiltrate (chancre) at the site of penetration of the virus, as well as the presence of fatigue.
- Secondary . Multiple contagious skin rashes appear.
- Tertiary . At this stage, damage occurs to the internal organs and systems of a person. Today, the tertiary form of syphilis is quite rare.
It is worth noting that at the site of infection, skin pigmentation may be impaired.
How to find out if you have been infected with syphilis
The primary ulcer at the gate of infection is painless and is often not detected by the woman (an ulcer deep in the genital tract), as well as by the man, if he was the passive party in homosexual contact. They may not be aware of their illness until the weeping rash appears. After questionable unprotected sexual intercourse, you should not have sex without a condom with other partners.
A month to a month and a half after it, it is strongly recommended to undergo standard serological tests to determine whether you have become infected or not, even if there are no rashes on the skin of the body.
The likelihood of infection is reduced if, immediately after questionable unprotected sexual intercourse, the contact surfaces are treated with miramistine/chlorhexidine.
Symptoms
At the very beginning of infection, a person may not experience any discomfort or pronounced symptoms for a long time. But with the onset of the primary stage, everything changes. The main symptoms of the disease:
- Lymph nodes increase significantly in size, chronic fatigue is observed for no apparent reason.
- A hard chancre appears on the body or mucous membrane, having smooth round edges of red color, ranging in size from 0.2 to 1.5 cm. In the middle of the chancre there is a serous substance, which over time turns into a crust. If it is removed, a bleeding ulcer will be exposed underneath.
- Possible increase in body temperature.
- Headache.
- In the presence of concomitant infections, necrosis may develop.
- It is not uncommon to develop inflammation of the lymphatic vessels, which feel hard to the touch and resemble tourniquets.
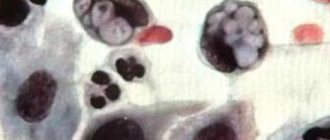
In the secondary stage, multiple rashes (papules) appear on the skin and mucous areas. They may be pink or red, dense, with bubbles or even pus inside, but they do not tend to merge. If left untreated at this stage, they disappear on their own after 2-3 weeks.
At least 3 years usually pass before the onset of the tertiary stage. Signs at this stage consist of damage to bone tissue, internal organs, spinal cord and brain, which can often lead to death or disability.
In children, the clinical manifestations are the same as in adults.
Classification of the disease
In medicine, the following classification of syphilis is accepted:
- the primary type is determined by a hard chancre in the place where the pathogen penetrated, swelling of a nearby lymph node. This period lasts up to 2 months;
- the secondary form lasts for several years. Infection spreads to internal organs. Specific rashes form on the skin, and hair loss begins. This stage is characterized by undulating periods of absence and appearance of symptoms;
- the hidden form is not characterized by mucous and skin manifestations. There are no signs of infection of internal systems. The disease can only be determined using clinical tests;
- the tertiary type is extremely rare, when the disease lasts for many years without treatment. The patient experiences irreversible damage to the body.
The central nervous system is especially affected. This type of disease leads to disability and then death.
In addition, syphilis is divided into visceral type, which affects internal organs, and neurosyphilis, which affects the patient’s nervous system.
Diagnostics
Before starting the diagnosis, you must make an appointment with a dermatologist or venereologist.
After a clinical examination, he will issue a referral for tests, the results of which will make it possible to make a diagnosis. Diagnosis of the disease includes the following tests:
- PCR diagnostics.
- RW blood test to identify the causative agent of syphilis.
- REEF.
- RIBT.
- TRNA analysis for detection of antigen to treponema.
It is possible to undergo a CT scan to obtain information about the condition of internal organs and the nervous system. It is possible to submit a smear taken from the rash for the presence of Treponema pallidum.
Syphilis infection among doctors
Healthcare workers can become infected while working with infected patients if they ignore protective rules.
The risk group includes the following specialists:
- Venereologists;
- Surgeons (if the patient’s blood comes into contact with the unprotected damaged skin of the doctor during a surgical operation);
- Dentists (possible infection through dental instruments that were in contact with an infected patient, as well as when working without gloves with contaminated oral mucosa and blood);
- Obstetricians-gynecologists (infection during the delivery of an infected woman through blood, birth secretions, and also from the blood of the child).
Although venereologists encounter patients with syphilis during the most active periods of the disease, they are extremely rarely infected. This is due to several reasons:
- Doctors know what diseases they are dealing with and what consequences they face;
- They always work with rubber gloves, or carry out their manipulations through cotton wool; take care of the skin of your hands, preventing it from being injured;
- Disinfectants (70° alcohol or carbolic acid) are always available, which can be used to disinfect the affected area if infection is suspected.
Find out if you can get HIV through a kiss.
How long after infection can syphilis appear? Read here.
Cheap and effective suppositories for thrush: https://venerolog-ginekolog.ru/gynecology/medicament/svechi-ot-molochnitsy.html
How to treat household syphilis
Treatment of household syphilis takes place in 2 stages: prescribing medication and establishing a quarantine regime at home.
Moreover, therapeutic therapy for each patient is individual and should be prescribed only by a specialist. It is worth noting that successful treatment is possible only at stages 1 and 2 of development, since at stage 3 changes in the body are already irreversible. Drug therapy consists of the following drugs:
- Antibiotics . They are prescribed in the form of an injection solution and tablets, which should be taken every 3 hours. The course of treatment is 14 days for primary household syphilis, and 31 days for secondary syphilis. The most common drugs are “Ampicillin”, “Erythromycin”, “Carbenicillin”, “Erythromycin”, “Benzylpenicillin”, “Oletetrin”, “Bicillin” and “Tetracycline”. All of them are included in the penicillin group of antibiotics.
- Immunomodulators . Necessary for boosting immunity and relieving inflammation in the body. Among them are “Cycloferon”, “Peat” and preparations containing aloe.
- Vitamins . The most important vitamins during this period are A, B, C, E.
In addition to the above drugs, medications containing heavy metal are often prescribed. They have an anti-inflammatory effect and have a detrimental effect on the virus, but have a lot of side effects and contraindications. One of these is “Biyoquinol”; in case of allergic allergies, it can be replaced with “Bismoverol”.
Who gets syphilis?
Most often, according to statistics, with syphilis, the routes of infection are associated with intravenous drug use. Drug addicts, in pursuit of the next dose of the drug, as a rule, are little concerned about the need to comply with basic rules of protection, and using one syringe, they transmit the infection along the chain. At the same time, cases of infection with this disease are recorded not only among drug addicts. Even those who carefully monitor their health and undergo regular diagnostics can “catch” the disease. Syphilis can also have a congenital form.
Complications
The most serious complications of household syphilis are considered to be tertiary stage pathologies. In this case, irreversible changes occur in the body. The human face and body are affected by ulcers, neoplasms and scars after formed ulcers. The brain and spinal cord, musculoskeletal system, heart and liver are affected. Paralysis, tabes dorsalis, blindness and deafness, and muscle ataxia of the lower extremities often develop.
Cases of heart attack and stroke, as well as death, are common.
How to avoid getting infected with syphilis?
Prevention of syphilis is simple and does not require much effort:
- Compliance with generally accepted hygiene standards (use only your personal hygiene items and separate utensils);
- When having sexual intercourse, use contraception and avoid casual sexual contact;
- If there was a fact of intimate intimacy with a stranger, it is necessary after some time (during the incubation period there are no manifestations of syphilis) to consult a venereologist for consultation, examination and subsequent treatment;
- Regularly visit a venereologist for preventive examinations, both yourself and with your sexual partner, in order to exclude infections with sexual diseases, including syphilis;
- Do not treat syphilis on your own or with folk remedies. Such actions will make it difficult to diagnose syphilis and will lead to questionable tests in the future;
- Before a planned pregnancy, it is advisable to undergo an examination for the presence of sexual diseases, and during pregnancy to conduct a serological test in order to protect the child from congenital syphilis;
- Provide additional treatment for syphilis during pregnancy in women who have had this disease and have been removed from medical registration;
- Limit close communication and contact with people with syphilis.
Avoiding casual sex and early contact with a specialist will help you protect yourself and your family from Treponema pallidum.
www.youtube.com/watch?v=WFA7Shgczsg
Prevention and prognosis
Preventive measures consist of observing the rules of personal hygiene; constant and regular treatment of the premises with antiseptic drugs is necessary.
Also, you should not use someone else’s clothes (trying on underwear and swimsuits on a naked body in stores), or personal hygiene items. Visit public catering establishments if there are suspicions of improper compliance with sanitary standards. Visits to beauty salons, hairdressers and manicure salons should be accompanied by checking the disinfection of all instruments. An important condition is timely and regular comprehensive medical examination of the body. After all, you can become infected with syphilis, both domestically and sexually, several years after complete recovery.
As for the prognosis, it is very favorable. The first two stages today can be successfully treated and fairly quickly. But if the disease is chronic, advanced or is at the tertiary stage of development, then disability most likely cannot be avoided.
Household syphilis is no less dangerous than sexually transmitted syphilis, but with timely detection and treatment, success is guaranteed. Therefore, you should pay close attention to your own health.
Consequences and complications
The consequences of syphilis are directly related to the stage of the disease.
The primary type of disease is characterized by the following complications:
- tissue necrosis in the area of formation of a specific chancre;
- paraphimosis;
- balanitis and self-amputation of the penis in men.
Such consequences are quite severe and can cause gangrene of tissues and the genital organ.
Secondary syphilis leads to the following consequences:
- diffuse baldness;
- complete baldness;
- loss of voice.
In extreme cases, the glottis narrows. This condition requires surgical intervention. The consequences of the third stage of syphilis appear in neurosyphilis, which affects brain cells. The patient experiences a decrease in intelligence, deterioration of attention and memory. There are known cases of damage to internal organs.
Most often they suffer from complicated visceral syphilis:
- brain;
- heart;
- digestive system;
- lungs.
Complications of tertiary syphilis cannot be treated. The patient's internal organs suffer from destructive changes that cannot be corrected even surgically.
How is syphilis transmitted through sexual contact?
Despite the fact that sexual transmission of infection is considered the main method, direct sexual intercourse is not necessary for infection. This strikingly distinguishes syphilis from HIV infection, the transmission of which requires friction of mucous membranes and a large volume of infected fluid. To become infected with syphilis, only short contact of mucous membranes is enough, for example, during a kiss.
In addition to traditional vaginal contact, the disease is transmitted through oral and anal sex without a condom. Moreover, the risk of transmission with such connections not only does not decrease, but even the opposite. This is due to the acidic vaginal environment, which somewhat neutralizes treponemes when they enter. While in the mouth and rectum there are no such protective mechanisms.
How long after infection do symptoms appear?
The incubation period, calculated from the moment Treponema pallidum enters the body until the formation of chancre, averages 3-4 weeks (see in detail about the first signs of syphilis and how it is treated). The following latent phase options are possible:
- shortening to 8-15 days with simultaneous infection from several sources
- extension to 100-190 days while taking antibiotics for the treatment of another pathology
That is, after infection, a person does not feel any symptoms for at least 2-6 weeks, which, with a large number of sexual partners, makes it difficult to determine the source of infection.
Transplacental infection of the fetus
There is a transplacental route of transmission of syphilis, when intrauterine transmission of the infection occurs from a sick mother to the fetus. Treponema pallidum is transmitted during pregnancy from mother to child through the placenta. This disease is called congenital. Often a fetus infected with syphilis dies in the womb.
Infection of the fetus can also occur during childbirth through the mother's infected birth canal.
It is possible to become infected with the disease through the milk of a nursing mother with syphilis, even if there are no clinical changes in the nipple area. This occurs due to the fact that syphilitic elements may be inside the mammary gland, i.e. in its ducts.