Symptoms
If there is a high concentration of glucose in the blood, you should consult a gynecologist and take a smear, this will help identify candidiasis at an early stage.
The presence of thrush can be detected independently; it is characterized by the presence of:
- Itching, burning, which are detected in the genital area.
- Increased dryness, drying out in the mucous membrane, which is also observed in diabetes mellitus.
- The discharge is white and cheesy in appearance.
- Pain and discomfort during sexual intercourse.
In women, vaginitis is detected more often in most cases; in men, the pathology is diagnosed as balanoposthitis or urogenital pathology.
Clinical picture of the disease
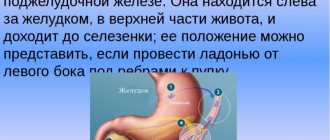
Damage to the female body by diabetes mellitus is accompanied by a disruption in the blood supply to organ tissues. Lack of proper nutrition to cells leads to their oxygen starvation.
Violation of the acid-base composition, a decrease in the body's defenses leads to the development of infectious diseases. This state of the body becomes a consequence of the development of pathogenic fungi and microbes. The pathological process develops quickly in the absence of proper treatment. Infection of microcracks causes painful and unpleasant itching sensations in the female genital organs.
It must be taken into account that high blood sugar slows down the healing of wounds, which contributes to the deep spread of infection. The doctor will be able to make the correct diagnosis after the patient has undergone tests. A smear taken from the vagina is examined for the presence of a fungal infection. Signs of present candidiasis in women are characteristic, which facilitates diagnosis.
Thrush in diabetes: treatment
First, before starting therapy for candidiasis, you should restore your sugar level. It is compliance with this condition that will help inhibit the development of the fungus. For these purposes, diabetic nutrition is prescribed, and after determining the glycemic profile, the required dose of the medication is selected.
To measure blood sugar levels you will need a glucometer; how to choose the right device, read the article
.
To eliminate pain and irritation, before using medications, it is recommended to toilet the genitals using a soda solution (bath). After visiting the toilet, the genitals should be treated, because... Remains of urine can become an excellent environment for the progression of infection.
The main treatment approach is to meet three conditions:
- Removing the manifestations of each disease.
- Use of local agents for therapy.
- General drug treatment.
The clinical picture of the complications that have arisen must be determined by the doctor, who will also establish an effective method for eliminating the disease.
Diet for thrush in women
The occurrence of thrush in diabetes mellitus is caused by a high concentration of sugar in the body. Eating foods with a minimum amount of carbohydrates is the main rule of a therapeutic diet for vaginal candidiasis.
The following foods should be excluded from the diet of diabetic women with thrush:
- flour products, baked goods;
- sweets;
- sweet fruits;
- starchy vegetables.
The introduction of meat, cheese, fish and seafood, vegetables, and nuts into food has a beneficial effect on the body.
Thrush in diabetes mellitus: treatment for women
Therapy for candidiasis that develops against the background of diabetes takes place in several stages. Initially, general antifungal medications are taken, these are tablets or injections:
- Fluconazole.
- Nystatin.
- Clotrimazole.
- Natamycin.
The dosage is determined by the attending physician, taking into account the history of the disease. If thrush is diagnosed in women with diabetes, treatment occurs by taking topical medications (ointments or suppositories). This is necessary if the disease was diagnosed for the first time or is localized in the vagina. Livarol is most often prescribed (for 5 days - 1 suppository per day before bedtime). Also, a good effect is created from the use of: Gyno-Pevaril, Mikogal, Macmiror, Zalain, Rumizol, Metronidazole.
If you consult a doctor early, the disease can be cured in 10-14 days. Medications will be prescribed for two doses. This facilitates the treatment of candidiasis in the presence of diabetes mellitus type 1, as well as type 2. The chronic form of thrush takes longer to resolve; it may take about a year to eliminate symptoms and prevent relapse.
Causes of thrush
Women most often complain about obvious symptoms of the disease, without attaching much importance to them. Causes:
- failure to comply with personal hygiene rules;
- contaminated underwear allows microorganisms to multiply quickly;
- incorrect selection of hygiene products for the intimate area;
- allergic reaction of the body to synthetic underwear;
- rarely, but if the partner has an aggressive fungal strain, there is a possibility of contracting candidiasis through sexual contact;
- pregnancy;
- concomitant chronic infections;
- long-term use of antibiotics.
Thrush in men with diabetes: treatment methods
The disease is treated by prescribing antifungal drugs, ointments and creams are prescribed for topical use. In the presence of a systemic and pronounced inflammatory process, systemic antifungal formulations are used.
Simultaneous therapy (general and local) and control of blood sugar levels are important; these measures will help eliminate the breeding ground for the development of pathogens.
To prevent the possibility of re-infection, both sexual partners are involved in treatment.
If the disease is completely cured, people with any form of diabetes should undergo tests and examinations by a gynecologist or urologist every six months. This is due to the fact that candidiasis has a tendency to cause chronic relapses.
Causes and symptoms
Candida is considered an opportunistic pathogen. It is present on the mucous membranes, but does not always cause an inflammatory process.
Thrush in diabetes or candidiasis occurs under the influence of a number of factors:
- excessive dryness of the skin, loss of elasticity and the formation of microcracks as a result of impaired blood circulation;
- a significant decrease in the body’s protective functions;
- violation of the acid-base balance of the vaginal microflora, the formation of a neutral or alkaline environment;
- hormonal disorders;
- urogenital infections in chronic form (chlamydia, mycoplasmosis, ureaplasmosis);
- hot climate;
- wearing uncomfortable, tight underwear made of artificial materials;
- long-term use of antibacterial drugs;
- abuse of foods high in glucose;
- use of intrauterine contraceptives - spirals, rings;
- failure to comply with intimate hygiene rules.
Thrush and diabetes often exist inseparably from each other.
The signs and symptoms of thrush in diabetes mellitus are so pronounced that a woman can independently find out about the development of the inflammatory process. The following symptoms are typical for vaginal candidiasis:
- itching and burning of the genitals;
- white coating on the mucous membranes;
- vaginal discharge, which may have a curd-like consistency;
- painful and uncomfortable sensations during urination and sexual intercourse.
If such signs are detected, women suffering from diabetes should immediately seek help from a specialist. Self-treatment of thrush during the development of this endocrine disorder can cause serious harm.
Sometimes a woman encounters thrush without discharge, and in order not to miss the onset of the development of pathology, it is worth undergoing regular examination by a specialist.
Traditional methods of treatment
To relieve the symptoms of candidiasis (swelling of the genital organs, itching), accelerate the normalization of the balance of the inflamed mucous membrane, infusions and decoctions of herbs are used. These procedures are used for washing and douching.
Let's look at effective recipes:
- In 10 tbsp. dissolve 1 tbsp of clean water. liquid honey. The resulting solution is used to treat mucous membranes.
- An infusion of herbs (calendula or chamomile) is used for douching or washing. To prepare it, 1-1.5 tbsp. dry herbs, pour a glass of boiling water (250 ml), leave and strain.
- Soak a cotton swab (disk) with kefir (yogurt without additives) and place it in the vagina overnight. This composition will help normalize the microflora and bacterial layer on the mucous membrane.
If discomfort occurs during any procedure, it must be stopped and a new treatment method must be selected.
It is also important to understand that traditional methods of treatment do not replace drug therapy prescribed by a doctor. They should be used in combination, help relieve symptoms of the disease and speed up recovery.
Will folk remedies help?
The effectiveness of folk remedies can only be that of diabetics with normal compensation for the disease, in the absence of complications. In addition, the use of such techniques should be discussed with a specialist. Most often, folk remedies are introduced at the initial stages of candidiasis as measures that complement the main recovery course.
How to take mumiyo correctly to treat diabetes?
Thrush can be treated using natural honey diluted in 10 parts of boiled warm water. Next, the mucous membrane is lubricated with the resulting solution, which eliminates the appearance of microcracks and promotes their successful healing.
Calendula infusion can be used. For this, one tbsp. l. dissolves in 200 ml of cool water. Systematic use of such calendula baths helps speed up recovery. The next method is:
- a gauze tampon soaked in kefir with a minimum degree of fat content is placed in the vagina before going to bed;
- the procedure is carried out within five days;
- If tamponing is associated with unpleasant sensations, it is recommended to consult a specialist as soon as possible.
Prevention
To prevent the development of candidiasis in diabetes, it is important to follow certain preventive measures:
- Toilet your genitals every day. Urea residues are a good nutrient medium for various microorganisms. For hygiene, you should use products that have a neutral pH level.
- If you have casual sex, use contraceptives to prevent possible infection.
- Wearing underwear made from natural fabrics will help prevent diaper rash, chafing, which causes inflammation and other diseases.
- Lead an active lifestyle and diet.
- If you are undergoing long-term treatment for colds, viral or other diseases that contribute to the development of diabetes, you should additionally take medications containing lactobacilli.
The described preventive measures must be followed not only to prevent the disease, but also during therapy to prevent relapse.
Share link:
Treatment of the disease
The medicinal components that are prescribed by a specialist in the presented situation should not differ in any way from the usual methods in the treatment of various fungal pathologies.
If thrush is not treated for such an endocrine disorder, it will progress and soon develop into a chronic form, which is especially dangerous. Treatment of thrush in women with diabetes has its own characteristics, since it acts as an additional complication of this disease.
First of all, the specialist prescribes drugs to relieve acute inflammation. At this stage of therapy, symptomatic treatment of candidiasis is carried out: anti-inflammatory and antifungal agents are prescribed. You also cannot do without the use of drugs that restore the disturbed vaginal microflora.
To stop the signs of thrush and speed up the recovery process, at the time of treatment it is important to follow the following recommendations:
- Avoid sexual intercourse until complete recovery. This will prevent mutual infection of partners with the fungus. For these purposes, it is important to treat the man. Despite the fact that males do not suffer from sexual candidiasis, they act as carriers of the fungus, infecting women with it.
- Strictly observe the rules of personal hygiene. For water procedures, it is recommended to use alkaline water. A solution of potassium permanganate, decoctions of chamomile, sage, and calendula have a beneficial effect on the inflamed mucous membrane. Soap should not be used during the treatment period; it will only intensify the inflammatory process. After such procedures, it is necessary to apply an antifungal gel or ointment to the affected areas.
- If the peak of candidiasis occurs during menstruation, you should avoid tampons. It is recommended to use pads and change them every three hours.
In gynecology, in the treatment of thrush in women with diabetes, tablets, vaginal suppositories and ointments, and preparations for external treatment of the source of inflammation are used. The following antifungal drugs have proven themselves to be effective:
- Nystatin;
- Fluconazole;
- Candide V;
- Kandibene;
- Myconaz;
- Pimafucin;
- Clontrimazole;
- Butoconazole;
- Pimafucin.
They are available in the form of tablets, suppositories or ointments. In severely advanced forms of the disease, drugs of all pharmacological forms are prescribed simultaneously. Livarol suppositories are also effective; for recovery, it is enough to use a suppository for 3 days in a row.
Pain, itching and burning with thrush.
Treatment of candidiasis in diabetes mellitus types 1 and 2 must be comprehensive and must include the following conditions:
- a woman should monitor her blood glucose levels daily;
- the required antifungal therapy is carried out;
- the mucous membrane of the genital organs is populated with normal microflora;
- a woman must provide her genitals with the required intimate hygiene.
It is worth paying attention to the fact that treatment of candidiasis should begin with compensation for diabetes mellitus. The absence of such a condition will not allow creating conditions in the vagina that are favorable for the development and restoration of mucous membranes.
An endocrinologist will help you obtain maximum compensation for the disease. The doctor will be able to select the volume of insulin injections, prescribe the required diet, and recommend medications.
To treat thrush, only pharmacological agents are used. The treatment regimen is determined by a gynecologist-endocrinologist. You should not use traditional methods for treatment. Such techniques are not highly effective and can cause chronicity of the pathological process.
In the chronic course of thrush, the risk of relapse of the disease appears with ordinary consistency. To achieve better results in treatment, women should use systemic and local drugs.
When treating mild thrush in a woman with diabetes mellitus, the duration of treatment is minimal. If the disease is chronic, the woman will have to undergo a course of treatment lasting about six months.
You should not try to cure the disease yourself.
To relieve the acute phase of the disease, Fluconazole and drugs based on it can be used. Use one tablet for 3 days. To prevent relapse, the drug can be prescribed at a dose of 1 tablet per week for 6 months.
A similar scheme of use is suitable for local means of influence. The list of popular drugs used for systemic therapy for thrush includes the drugs listed in the table.
The specialist should inform the woman that local and systemic therapy should be provided simultaneously. To achieve better results, high compensation for diabetes should be achieved.
Attention! Traditional methods of treating candidiasis in women with diabetes mellitus should not be used.
To obtain the best results in treatment, the patient must follow a diet. Often the manifestation of thrush can be triggered by an increase in the concentration of sugar in the body. Consumption of foods with a minimum amount of carbohydrates is the basic principle of a therapeutic diet.
Healthy diet.
The following foods should be eliminated from women's diets on an ongoing basis:
- all flour products;
- bakery;
- sweets;
- sweet fruits;
- starchy vegetables.
A woman’s diet should include:
- meat;
- cheese;
- fish;
- seafood;
- vegetables and nuts.
Treatment for patients with diabetes begins with lowering blood sugar levels. This is necessary in order to create negative conditions for the further growth and development of fungal pathogenic organisms.
Drugs that are used to treat candidiasis can be divided into 2 large groups: local, which include suppositories, ointments and gels, and systemic - injections and tablets. Only after a comprehensive examination and obtaining a complete picture, the doctor prescribes adequate treatment that is suitable for a particular woman.
However, the types and forms of medications may vary. If at the initial stage the thrush progresses - itching, redness, and other pain are very disturbing, then it is advisable to begin treatment with the use of special baths.
To prepare them, use a special solution of potassium permanganate or soda. After such water procedures, the genital organ is treated with a special antifungal cream or gel.
As a rule, such procedures should be carried out once a day, before going to bed. However, it should be remembered that when external signs of the disease disappear, treatment should in no case be stopped.
The next stage of treatment is complete and comprehensive therapy.
For patients suffering from diabetes, doctors, as a rule, select the most gentle drugs that can be used for children and pregnant women.
At the next stage of treatment, as a rule, the drugs Clotrimazole, Butoconazole, and Natamycin are used. They can be introduced into a woman’s body in the form of vaginal suppositories, capsules or tablets. The use of systemic drugs such as Fluconazole is also indicated.
Many experts consider the use of Levorin or Nystatin in treatment to be erroneous. The fact is that the percentage of bioavailability of these drugs is quite low, which is why outside the gastrointestinal tract they practically lose their effectiveness.
You should not think that thrush in diabetes requires specific treatment or any restrictions. Medicines prescribed by a doctor are no different from traditional methods of treating fungal diseases. But due to the fact that diabetes is almost impossible to cure instantly, and sometimes it accompanies a person throughout his life, you need to be prepared for repeated relapses of thrush.
This is due, first of all, to the fact that the environment in which fungi develop depends on the consumption of sugar and the production of glucose by the body. A sharp increase in blood sugar contributes to the development of candidiasis. If after treatment, after some time, a person again discovers symptoms of thrush, then treatment will have to be done again.
In order to make a correct diagnosis, it is necessary to undergo a full examination by a gynecologist, for this you should take all tests to determine the presence of candidiasis.
As in normal cases, traditional remedies are used to treat thrush in diabetes mellitus
- drugs with an antifungal effect that stop the growth of the fungus;
- drugs that restore vaginal microflora.
At the same time, when treating thrush, it is necessary to carefully monitor blood sugar.
With a sharp increase in it, itching and burning in the vaginal area begins, as well as dryness and irritation. The growth of the fungus increases and if treatment and further prevention of the disease are not started immediately, the disease begins to spread in the body, affecting other organs. Thus, in diabetes, candidiasis can develop in the respiratory tract, which leads to frequent colds, bronchitis, and sometimes asthma.
The presence of a number of chronic diseases, in particular diabetes, greatly complicates the treatment of thrush. To alleviate the patient’s condition and exclude relapses of the disease, it is necessary to follow some rules, including
- Diet with the exception of carbohydrates.
- Using sweeteners instead of sugar to reduce the calorie content of food and drinks.
- Insulin therapy in severe stages of diabetes.
- Constant monitoring of blood sugar, preferably having your own glucometer.
Aids
Green pharmacy preparations can only be used as an auxiliary, but not as a primary remedy if the patient has diabetes. As a rule, such herbal remedies are designed to reduce the symptoms of thrush. For example, you can use good natural honey, which is diluted with boiled water in a ratio of 1:10. The resulting solution should lubricate the mucous membrane. Calendula tincture also helps a lot. 1 tbsp. l. The tincture is diluted with a glass of cold boiled water. The solution is used for regular baths.
You can make a tampon from medical gauze and, moisten it generously in low-fat kefir, place it in the vagina overnight. In the morning, it is removed and douched with chamomile tincture.
In this case, you must follow the instructions. This procedure is best carried out over 5 days. All of the above manipulations can be done only with the consent of your attending physician. Any unpleasant symptoms or side effects should be reported to him immediately.
It must be remembered that only an integrated approach to treatment can lead to positive results. That is, local medications combat the symptoms and manifestations of thrush, and systemic medications help destroy the vaginal reservoirs of pathogenic microorganisms.
The course of tablet drugs is usually 2 weeks or more. Other medications are used once, less often twice. In some cases, advanced, chronic thrush is treated for six months, and sometimes a whole year. Only strict adherence to all the instructions of the attending physician is guaranteed to get rid of this unpleasant illness.