Home / After childbirth / Cervical erosion is not a death sentence
14192
0
In our 21st century, many women, after the birth of their first child, are diagnosed with cervical erosion. For some, this sounds like a death sentence, because they do not know what this disease is and how it is treated. Erosion (ectopia) of the cervix is a disease caused by a defect in the mucous membrane of the cervix. This is considered a pathological benign process.
True erosion is a bright red spot located on the mucous membrane of the cervix. The defect is formed due to tissue trauma, in which epithelial cells are rejected.
When the epithelium becomes thinner, a bleeding wound remains in its place, which can easily become infected. Sometimes after sexual intercourse a woman complains of bloody discharge. Cases of infection joining erosion are not uncommon.
What is erosion
Pathology is a violation of the integrity of the cervical mucosa. In this case, the normal squamous epithelium of the pharynx is replaced by cylindrical tissue of the cervical canal (ectopia of the cervix). As a rule, erosion is a benign process that does not cause a woman discomfort or unpleasant sensations. The frequency of diagnosing the disease during gestation is determined by the absence of symptoms and rare visits to the doctor before fertilization. A thorough medical examination after conceiving a child helps to identify the presence of an erosive process.
https://youtu.be/fkPN6E8gfzA
Effect of erosion
Superficial damage disrupts the integrity of the epithelium and can cause infection to enter the uterus. Before conception, as well as during pregnancy, this tendency does not at all contribute to the healthy course of processes.
When wondering whether it is possible to become pregnant with large or small erosion, you should consider the mechanism of influence in more detail.
Is conception possible?
It is quite possible to become pregnant if there is erosion. The exception is cases when its appearance was provoked by other serious deviations in the functioning of the body.
This damage does not affect the passage of sperm through the cervical canal or the production of eggs by the ovary. If a girl is diagnosed with this condition, but the desired pregnancy still does not occur, she will have to undergo a series of examinations.
Perhaps previous infections led to the formation of adhesions. Or hormones that affect the normal course of processes in the body are not produced correctly. It is these reasons, and not the wound itself, that lead to infertility.
Many women are interested in whether it is possible to give birth with erosion. Indeed, for some, this disease manifests itself already during pregnancy.
Pregnancy
Depending on the severity of the disease, there are certain risks. Based on the results of the examination and laboratory diagnostics, the gynecologist will be able to say with confidence how erosion affects the course of pregnancy.
The answer to the question whether a woman with cervical erosion can become pregnant is positive. But this is not a fact that you can bear a healthy baby. The most basic risks include the following facts:
- Due to the violation of the integrity of the mucous membrane, infection may enter.
- The previous fact can cause a miscarriage.
- Tissues eroded during childbirth may rupture. In case of an extensive, advanced form of the disease, the child will be born by caesarean section.
These consequences are quite rare. Most often, damage to the mucosa does not lead to such serious consequences. However, timely treatment carried out under the supervision of a qualified specialist can guarantee the absence of problems in the future. Waiting for the baby will be normal, bringing a lot of positive emotions to future parents.
Is it possible to get pregnant with cervical erosion?
A woman will not experience difficulties conceiving, since the pathology does not in any way affect the maturation or fertilization of the egg. However, if the erosive process was discovered before pregnancy, it is strongly recommended that the disease be treated first. You can plan to conceive as early as a month after treatment, provided that healing proceeds normally and without complications. If there is extensive damage to the mucous membrane of the cervix and slow tissue restoration, planning a pregnancy should be delayed for 4-6 months.
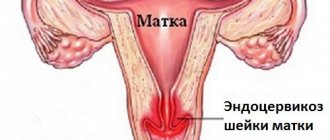
Concept of ectopia
If the cylindrical epithelium, which lines the inside of the cervical canal, displaces the flat epithelium from the surface of the cervix, which extends into the vagina, then when examined with the help of mirrors, this is striking. A red spot appears around the canal.)
Here it is appropriate to talk about such a mucosal defect as cervical ectopia . The pathology has other names - pseudoerosion, endocervicosis.
Ectopia can be mistaken for erosion of the cervix . But these two conditions have a significant difference. In the presence of true erosion, the mucous membrane of the cervix is damaged, and ulcers are visible on its surface under a microscope. For ectopia, ulceration of the mucous membrane is unusual.
Gynecologists of the old Soviet school insist that pseudoerosion is a precancerous condition and requires surgical treatment methods.
Until recently, ectopia was mercilessly cauterized or frozen with liquid nitrogen.
At the present stage of development of medical science, this condition is considered normal. In other countries, ectopia is left without treatment if it is asymptomatic.
It happens that ectopia is accompanied by cervicitis with accompanying discharge.
Then a laboratory test of the smear is necessary to identify the causative agents of inflammation. Drug treatment is prescribed to eliminate the source of the disease.
If pseudo-erosion causes pain during sexual intercourse and bleeding after it, an in-depth examination is necessary.
If the likelihood of developing cancer is excluded, surgical treatment is necessary.
For small sizes of the altered surface, pharmacological or chemical coagulation .
If pseudo-erosion occupies a large surface, treatment methods based on the effects of laser, radio waves, high temperatures, electricity or liquid nitrogen would be appropriate.
About ectopia and erosion in this video:
https://youtu.be/CLIpnI1Gw3s
Erosion during pregnancy
According to doctors, disruption of the integrity of the epithelium of the uterine cervix does not pose a serious danger to pregnancy. The pathology does not cause delays in fetal development, provided that tests do not reveal the presence of infectious pathogens. Erosion during pregnancy can be dangerous if a woman has:
- trichomoniasis;
- genital herpes;
- syphilis;
- papilloma virus.
Symptoms
As a rule, cervical erosion during pregnancy does not manifest itself as any discomfort, so this disease is diagnosed directly during a routine gynecological examination. If the disease appeared before pregnancy, then there is a possibility of aggravation of the erosive process due to hormonal changes characteristic of bearing a child. In this case, the following symptoms of a violation of the integrity of the uterine epithelium may appear:
- pain during intercourse;
- discharge of ichor after intimacy (not related to menstruation);
- mucous or purulent discharge.
Possible complications
The course of pregnancy with cervical erosion should be monitored by a doctor. Examinations are carried out regularly, this is due to the risk of complications in a woman during pregnancy and after childbirth. The list of possible ones includes:
- early miscarriage;
- premature birth;
- proliferation of erosive foci due to the growth of the uterus;
- dysplasia;
- an increase in lesions due to injuries received during childbirth.
Only timely detection and supportive therapy can provide prevention. The appearance of consequences for a woman during pregnancy. The most dangerous complication is dysplasia; the condition is classified as a group of precancerous lesions, so its treatment should be given due attention.
Erosive lesions of the cervix do not pose a danger to the mother and child; the danger lies in possible complications. To minimize the effect of negative factors, a woman at the stage of pregnancy planning needs to undergo a full examination in order to weigh all the risks present.
Causes
The factors that caused the erosive process during pregnancy or before must be determined. This will help you choose the optimal treatment and quickly eliminate the cause of the disease. Common factors that stimulate erosion include:
- sharp hormonal fluctuations in the female body;
- prolonged use of oral contraceptives or taking other hormonal drugs before pregnancy;
- the presence of sexually transmitted infections, for example, gonorrhea, chlamydia, ureaplasmosis, etc.;
- early initiation into sexual relations;
- inflammation of the genital organs that is not infectious;
- the presence of malignant tumors in the reproductive system;
- artificial termination of pregnancy;
- rough sexual intercourse, sexual violence;
- decreased immunity;
- damage to the mucous membrane of the uterine pharynx due to improper douching or installation of an intrauterine device;
- frequent severe stress on the body.
Diagnosis of erosion
Methods for examining the cervix during pregnancy are determined by the doctor. The primary type of diagnosis is examination of the organ in mirrors. Using this procedure, you can identify epithelial defects that look like a outlined red spot. Other diagnostic techniques used when an erosive process is suspected include:
- Krobak's test. Probing of erosive tissue is necessary to determine the density of the affected tissue.
- Smear from erosion and cervical canal. This is necessary for cytology, including bacterioscopic and bacteriological examination.
- Colposcopy. The diagnosis is confirmed by the presence of clearly defined damage to the mucous tissue of the cervix with a visible zone of stroma.
- Carrying out a biopsy. Used when a malignant process is suspected.
Let them become a thing of the past!
, electrocoagulation of the cervix was widely used to treat cervical ectopia . The method is based on the destruction of ectopia by the action of current. Today, this type of cervical coagulation, especially in young nulliparous girls, is not used, as it causes complications: the formation of rough scars and endometriosis.
Also, at present, conservative methods are not used to treat cervical ectopia (various douching; tampons with Vishnevsky ointment, honey, other so-called “medicinal” tampons), since their absolute ineffectiveness has been proven. Moreover, ointment treatment, by loosening the cervical tissue, contributes to the development of cervical cancer.
“Therapeutic” tampons DO NOT EXIST! No tampons can cure gynecological diseases. Moreover, they can be harmful to health, as they disrupt the vaginal flora and cause inflammation. Treat yourself competently and you will always be healthy!
How does erosion affect pregnancy?
When planning a pregnancy, a gynecological examination is mandatory. As a rule, during this procedure it is possible to find out whether there are pockets of erosion on the uterine cervix. It is important to do an examination because erosion during pregnancy can be dangerous: the ulcerated surface is an excellent environment for the development of pathogenic flora that can cause an inflammatory process. The most dangerous consequences that the disease can lead to during pregnancy include:
- spontaneous termination of pregnancy (miscarriages occur especially often in the first trimester);
- progression of inflammatory pathologies, treatment of which is complicated by the woman’s position;
- premature birth in late gestation;
- rupture of the membranes, infection of the fetus, its death;
- transition of erosion into a malignant tumor.
What is erosion and what is the danger?
An erosive lesion is diagnosed if areas of redness are detected on the surface of the vaginal membrane during a speculum examination. These lesions can be multiple or single.
Interesting! Cervical erosion is the most common diagnosis made by doctors to parous and nulliparous women; more than 50% of women worldwide experience the lesion.
There are 3 forms of erosion:
- True – is the result of external factors (trauma to the mucous membranes). After damage, the mucous membrane sloughs off, and erosion occurs in place of the lining layer; it has an irregular shape, red color, and bleeding is possible.
- False - manifests itself as a result of the replacement of epithelial cells with cylindrical ones. Often occurs after childbirth (45% of women). Symptoms appear as a result of infection; in other cases, the disease occurs in a latent form.
- Congenital - occurs due to displacement of the boundaries of the columnar epithelium lining the cervical canal. This change often occurs in the prenatal period, and is therefore called congenital.
The list of the main reasons provoking the development of erosive lesions includes:
- inflammatory processes occurring in the female genital organs;
- sexually transmitted infections;
- women's hormonal imbalances;
- injuries to the mucous membranes of the external genitalia;
- early onset of sexual activity, early childbirth.
The danger of the disorder is that it does not manifest itself for a long time, and the woman does not consult a doctor. Against this background, polyps and dysplasia (precancerous condition) appear. If left untreated, erosion can cause cervical cancer.
Erosion is not a contraindication for childbirth, but against its background, the risk of ruptures in a woman increases, because the affected neck of the organ stretches less well. Cauterization is contraindicated at this time; treatment is carried out using medicinal methods.
Is it possible to plan a pregnancy with erosion?
Damage to the cervix is not associated with the possibility of successful pregnancy. The risk of negative consequences for the child is minimal. The only limitation is that a woman is not recommended to plan a pregnancy during the first 6 months after cauterization in order to exclude intrauterine developmental defects.
An erosive lesion often occurs in conjunction with various infections, so when it is detected, doctors recommend undergoing an examination to exclude the presence of additional factors that can aggravate gestation. If STIs are not detected, erosion during pregnancy is not cauterized, since the scar formed after the intervention will complicate labor. Conservative treatment is selected for the pregnant woman.
The addition of sexually transmitted infections is dangerous for the fetus. The risk of premature termination of pregnancy increases significantly if the mother develops the following diseases:
- HPV – human papillomavirus;
- trichomoniasis;
- chlamydia;
- gonorrhea.
Treatment of these infections in pregnant women is mandatory.
Risks depending on the type of lesion
With pseudo-erosion, pathological changes in the cervix do not appear, therefore it is not a contraindication for pregnancy. At the planning stage, the woman should undergo a full gynecological examination. This is necessary so that the doctor can monitor the condition of the lining layer. The only danger with pseudo-erosion is that during labor the risk of injury increases due to the fact that the area cannot stretch to its fullest extent.
True erosion is considered more dangerous. Colposcopy is performed to confirm the diagnosis. The doctor collects tissue for bacteriological examination to refute the possibility of developing an infectious process. If there are no infections in the smear, there are no contraindications for pregnancy. Treatment is provided with medication, and after birth, cauterization is performed. There are no risks for the child; the likelihood of ruptures in the mother during childbirth increases.
The most dangerous option is advanced erosion or dysplasia. The cause of its development is often the human papilloma virus. The risk to the baby is possible infection, so delivery is carried out by caesarean section.
Is it necessary to treat cervical erosion?
Doctors recommend that girls undergo treatment for the disease even before conceiving a child, and either surgical or conservative methods can be used. However, despite the stereotype that pregnant women cannot be treated for erosion, since after cauterization scarring can form, which impairs the elasticity of the uterus and aggravates pain during childbirth, therapy is still carried out.
Doctors resort to treatment of the erosive process only when there is a large area of organ damage with signs of inflammation. In this case, cauterization is not necessarily used, since there are other safer methods for treating erosive areas, including laser coagulation. In medical practice, there are many cases where damage to the cervical mucosa heals on its own during pregnancy, but more often the pathology is successfully treated after childbirth.
Diagnostic rules
Colposcopy helps to detect ectopia. Visual inspection of the cervix is possible only with the help of a mirror. The doctor must insert a gynecological instrument into the vagina.
Ectopia is often diagnosed during pregnancy, which gives rise to the false idea that pregnancy provokes the disease. Another myth is associated with the statement that the cause of ectopia is the onset of sexual activity. This is explained by the ban on colposcopic examination of virgins.
In fact, epithelial proliferation can be congenital or acquired. The nature of the pathology determines when the process began.
Areas of columnar epithelium that come out and are represented by zones with uneven contours indicate a congenital form of cervical ectopia. The acquired type of ectopia looks like cluster-shaped clusters of papillae, ranging in color from bright pink to bright red.
Treatment
Therapy for patients carrying a baby differs from standard treatment. Such popular techniques as cryodestruction or cauterization can be used only after the birth of the child. During pregnancy, only the most gentle methods of therapy can be used in combination with supportive treatment. The main goal is to stop the progression of the pathological process and prevent the progression of the disease. However, some doctors choose a wait-and-see approach: if complications do not develop, there is no point in treating it with medications.
If a woman periodically experiences a burning sensation or spotting, methyluracil can be used in the form of vaginal suppositories. They are administered for 14 days twice a day. When the erosive process is complicated by inflammation, doctors prescribe antibacterial and antiviral agents, the choice of which is based on bacterial culture.
Is it possible to cauterize erosion during pregnancy?
For pregnant patients, gynecologists always prescribe the most gentle treatment methods, which are mainly preventive in nature to prevent exacerbations. The range of drugs approved for use during pregnancy is very limited: most drugs are not recommended for use or are completely contraindicated. Cauterization of lesions with a laser is prohibited, so experts advise getting rid of the disease even before conceiving a child.
Is it possible to give birth with cervical erosion?
Since this disease increases the risk of serious complications, including the addition of purulent or inflammatory processes and threatens spontaneous abortion, doctors strongly recommend treating erosion at the stage of planning the birth of the baby. A healthy cervix is one of the important conditions for bearing and giving birth to a child.
If the pathology was diagnosed after conception, the patient is provided with constant medical supervision and optimal preventive treatment using conservative methods. In the absence of concomitant diseases of the genital organs, as a rule, pregnancy has a successful outcome. Once every three months, women with erosion are advised to undergo additional tests - cytology analysis and colcoscopy. Most pregnant women with this disease give birth to completely healthy babies and do not experience difficulties during pregnancy, since the pathology is asymptomatic.
Is it worth giving birth?
The presence of erosive lesions on the cervix and vagina does not indicate that a woman will not be able to become a mother. Also, a disease that is not complicated by hormonal changes cannot cause infertility. The main risk for a woman with erosion is the likelihood of tears in the surface of the mucous membranes.
Erosive lesions, regardless of the type and stage of the process, are not a contraindication for pregnancy. During gestation, doctors monitor the condition of the lesion and prescribe medication support as necessary. Radical methods of therapy are used only after childbirth.
True and pseudo-erosion is not a contraindication for either the first or the second or third pregnancy. The course of the birth process is no different. If there are no infections, you can give birth on your own. If there is a risk of the baby contracting an STI as it passes through the birth canal, the woman is recommended to have a cesarean section.
Childbirth with cervical erosion
As a rule, natural childbirth is allowed in the presence of pathology, but additional staff must be present in the ward in case of complications. Erosion and childbirth often coincide, and cesarean section is not a mandatory indication, however, many doctors recommend this method of resolution. If the doctor has given the go-ahead for natural labor, the woman should not worry, since the birth will most likely take place without complications.
What is the danger of cervical erosion after childbirth?
Pathology that develops after the birth of a child has a favorable prognosis. As a rule, the defect disappears on its own and does not require special treatment. Therapy may be needed only if pseudo-erosion forms, then postponing treatment will not work. A woman with pseudoerosion who has not been treated for a long time may develop a malignant tumor. This explains the need for timely consultation with a doctor who will help eliminate the problem that can lead to infertility and other dangerous consequences.
The prognosis of the disease directly depends on how quickly treatment began, so timely and regular monitoring by a gynecologist is extremely important. In addition, it is important to choose the optimal treatment method that will not cause tissue scarring. Thus, the success of treatment is influenced not only by the timeliness of therapy, but also by the chosen methods and qualifications of the specialist.
Features of treatment of erosion during pregnancy
If after the examination good results are obtained, and externally the doctor determines erosion of the cervix, then sometimes this can be physiologically normal during pregnancy - the cervix seems to turn out, and after childbirth it returns to normal. Then there is no need to treat this condition. In other cases, if the examination results are not very good, the treatment plan is individualized.
There is a misconception that erosion cannot be cauterized for young women who have not given birth. Previously, one could agree with this because the methods were crude and led to the formation of scars on the cervix, which prevented its dilation during childbirth. Now in the modern world there are modern methods - cryotherapy, laser, argon plasma treatment of erosion. But all these methods are inappropriate in our case - only after childbirth!
This is why pregnancy should be planned in order to identify and treat all diseases of the female reproductive organs before pregnancy!
And yet, if tests confirm the infection, and there are complaints about unpleasant discharge from the genital tract, sanitation is prescribed with vaginal tablets, suppositories (allowed during pregnancy and at certain times) and herbal suppositories (sea buckthorn - which have a healing effect).
You can use douching with herbal decoctions (only under the supervision of a doctor, so as not to damage the mucous membrane itself, and only with those herbs that your doctor prescribes, as they can cause allergies or harm the baby if treated independently). And then mandatory observation, control of histology, smears and colposcopy. Childbirth can be natural if there are no foci of infection.
In cases where cervical cancer is histologically confirmed, a council of doctors gathers and the issue of further pregnancy and treatment in an oncology hospital is decided!
The most important thing is that if you follow all the prescriptions of your gynecologist and regular visits to the antenatal clinic during pregnancy, you can safely give birth to a healthy baby on your own, even with such a diagnosis as cervical erosion! But of course, to avoid all complications from this disease, it is necessary to be examined when planning a pregnancy, and also treated before its onset, undergoing regular medical examinations! Health to you!
Pregnancy and childbirth after treatment of erosion
The theory of infertility after cauterization of lesions has not been confirmed, but the risk still exists. In this regard, it is optimal that cervical erosion and pregnancy planning coincide, and the woman has time to get rid of the problem before conceiving a child. The disease may not have any effect on fertilization and gestation of the baby, but the erosive surface is an ideal environment for the proliferation of pathogenic microbes, which can provoke various inflammatory phenomena that are dangerous to the fetus.
In the absence of complications and normal healing, a month after treatment of the pathology, you can plan to conceive a child. If the therapy was not easy or the erosive lesions were large, gestation will have to be postponed for six months or longer. Pregnancy during erosion is also possible and in most cases proceeds normally, but it is advisable to get rid of the disease in advance in order to avoid various troubles and risks. If true erosion is not treated, the consequences for pregnancy can be negative:
- premature birth;
- rupture of the membranes;
- inflammation of the genital organs;
- transition of the erosive process into a malignant form;
- miscarriage.
What is actually dangerous about erosion during childbirth?
There are many legends around this disease, in which there is always some truth. Erosion is damage to a certain area of the mucous membrane of the cervix. This disease does not have serious consequences and does not interfere with the birth process. But in rare cases, it can cause infection to penetrate the uterus and appendages, which will lead to infertility, or develop into cervical cancer. All this does not happen with a hundred percent probability, but any woman understands that even an unlikely risk remains a risk, so immediate treatment is necessary. According to statistics, in most cases, cervical erosion does not manifest itself in any way. It is rare to notice spotting after sexual intercourse, heavy exertion, or a gynecological examination. Therefore, only a professional can detect this disease. It’s not for nothing that they recommend visiting a gynecologist at least once a year, even if you feel completely healthy. Treatment of cervical erosion usually occurs through cauterization, but other methods are also possible: laser or radio wave treatment.
In order not to detect erosion during pregnancy, you need to be regularly examined by a gynecologist.
Will a woman be able to give birth naturally with erosion?
It happens that cervical erosion occurs during pregnancy. It can develop even in the first month, even in the ninth, but most often it is detected before twelve weeks. After this diagnosis, women panic, fear of childbirth, fear for the life of the unborn child and their own life creeps into them. How justified is this fear and is it possible to give birth with cervical erosion? It all depends on the type of erosion. There are two types:
- pseudo-erosion;
- true erosion.
Pseudo-erosion of the cervix or ectopia is not a disease, just cracks. In this case, the epithelium is not damaged; the ordinary squamous epithelium is simply replaced by columnar epithelium. This condition is a defect and not a pathology. Doctors say that this is a normal, although different from the usual, condition of the cervix of a healthy woman. Ectopia is not a disease and does not require treatment either during pregnancy or after childbirth. Childbirth also cannot be complicated due to pseudo-erosion, so there is no need to worry about this condition. If you have been diagnosed with true erosion, the situation is more complicated. But if you follow the doctor's instructions, nothing bad will happen.
First degree dysplasia is not dangerous during pregnancy. If the erosion does not go away on its own within two or three weeks, the woman undergoes a course of treatment prescribed by the doctor and calmly awaits childbirth.
With dysplasia of the second and third degrees, the situation worsens. In this case, treatment is contraindicated due to the risk of miscarriage or premature birth. All that remains is to regularly visit the gynecologist so that he can monitor the progress of the disease and control it. The gynecologist will prescribe a course of treatment only after childbirth. Childbirth itself with true erosion is not dangerous. If everything proceeds within normal limits, the birth will take place without complications.
Stages of cervical dysplasia: the first is not dangerous, the second and third can cause complications