What is menopause and why do menstruation stop?
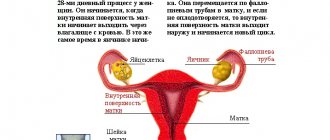
Menopause is a physiological state of the female body caused by the cessation of ovulation, age-related changes and reduced production of sex hormones. Due to weakening of the ovaries, the synthesis of follicle-stimulating and luteinizing hormone increases, which leads to the development of anovulatory cycles and follicular atresia.
Due to hormonal imbalance, ovarian tissue undergoes sclerosis. The menstrual cycle increases, bleeding becomes more scarce and gradually stops. Insufficiency of sex hormones affects the functioning of the reproductive, cardiovascular, nervous, and immune systems. For this reason, the menopause is accompanied by general malaise, headaches, hot flashes, and increased irritability.
Causes of uterine bleeding at the postmenopausal stage
Diagnosing abnormal uterine bleeding at the postmenopausal stage is not particularly difficult, since at this stage of menopause menstruation completely stops, and the appearance of any unplanned discharge is perceived as a deviation from the norm.
As a rule, the occurrence of uterine bleeding at the postmenopausal stage is associated with:
- taking hormonal medications designed to alleviate the symptoms of menopause;
- malignant processes affecting the endometrium;
- cervical cancer;
- vaginitis;
- diseases of the cervical canal;
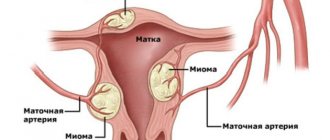
- uterine fibroids;
- endometrial hyperplasia;
- uterine polyposis;
- endometrial atrophy;
- neoplasms in the ovaries.
The appearance of any discharge at the stage of menopause is a reason to visit a gynecologist and undergo a full examination of the body, since the likelihood of eliminating unpleasant symptoms and the reason underlying their appearance directly depends on the time of visiting a doctor. In addition to spotting, women often suffer from hot flashes during menopause. This problem is very common, which is why there are so many ways to combat hot flashes during menopause.
Is bleeding possible during menopause?
After menopause, periods stop completely. Bleeding during menopause is allowed only while using hormonal drugs. When carrying out replacement therapy (HRT), synthetic analogues of estrogen are prescribed in combination with progesterone. Treatment leads to the appearance of light menstruation, the uterus may bleed a little with a red spotting secretion. The discharge does not contain clots and lasts no more than 3–5 days.
In any other cases, the development of metrorrhagia is a pathology and requires urgent attention to a gynecologist. Postmenopausal uterine bleeding may indicate the formation of benign or cancerous tumors.
When you need to see a doctor urgently
- unexpected bleeding after a long absence of menstruation during the postmenopausal period;
- the appearance of bleeding after physical activity;
- bleeding after sexual intercourse, with constipation and severe cough;
- duration of menstruation more than 7 days;
- frequently recurring periods (even scanty ones) at intervals every 2-3 weeks;
- absence of menstruation for more than 4 months during premenopause;
- bleeding while taking hormonal drugs;
- profuse bleeding.
Any prolonged bleeding requires immediate attention to a specialist, regardless of the volume of blood. The reason for a visit to the doctor may be constant spotting of a brown or dark brown color with a specific odor.
Why does metrorrhagia occur?
The reasons for the development of metrorrhagia depend on the period of menopausal changes and the presence of concomitant systemic diseases. In premenopause, conception is still possible, and bleeding indicates ectopic gestation, spontaneous abortion, or pathological location of the placenta. With polycystic ovary syndrome, there is a long absence of menstruation, menstrual periods are very heavy, lasting 7–10 days or more.
Why do uterine bleeding occur during menopause?
- endometrial polyps;
- myomatous nodes;
- cancerous tumors of the uterus, fallopian tubes, ovaries;
- taking hormonal medications;
- hyperplastic pathologies of the endometrium;
- erosion of the cervical uterus;
- pathologies of the thyroid and pancreas;
- hemocoagulation;
- cirrhotic liver.
Acyclic bleeding during menopause is often diagnosed in patients with a history of medical abortions, surgical operations in the pelvic area, chronic diseases of the reproductive organs, and arterial hypertension. Bloody discharge appears during hormone replacement therapy during early menopause. Metrorrhagia can also be provoked by endocrine disorders (obesity, diabetes mellitus), a weakened immune system, climate change, severe stress, overwork, and severe poisoning.
In the majority of cases, bleeding during menopause develops as a result of endometrial hyperplasia. The disease occurs in women in pre- and menopause; in postmenopause, pathology is not observed. The disease is accompanied by scanty blood loss or heavy bleeding. The growth of the inner layer of the uterus increases the risk of the formation of polyps and cancerous tumors.
Symptoms
A woman notices the first disruptions in the nature and duration of menstruation during premenopause. Already at the beginning of menopause, monthly bleeding becomes irregular, more abundant or scanty, and may disappear for 2-3 months and then appear again. Such changes usually do not indicate the presence of organic pathologies; they are signs of hormonal changes and are considered physiological.
The following types of uterine bleeding during menopause should be the reason for a mandatory visit to a gynecologist:
- intense bleeding, in which a woman has to change the pad every half hour or hour;
- presence of clots in menstrual blood;
- spotting after sex;
- the appearance of bleeding in the intermenstrual period;
- the occurrence of menstrual bleeding in less than 21 days;
- absence of menstruation for 3 months.
The general well-being of a woman after pathological menopausal bleeding depends on many factors: the volume of blood loss, the severity of signs of anemia and the presence of concomitant diseases (liver pathologies, thyroid dysfunction, hypertension, oncological processes). With massive blood loss, a woman will experience the following symptoms:
- increasing weakness;
- pallor of the skin and mucous membranes;
- dizziness (up to fainting);
- rapid pulse;
- decrease in blood pressure.
Prolonged and severe anemia that occurs against the background of heavy menopausal bleeding can lead to systemic disorders.
How to recognize bleeding during menopause?
Clinical signs of uterine bleeding during menopause:
- hemorrhagic discharge of varying intensity;
- the appearance of clots in the secretion;
- blood after intimacy.
Prolonged, heavy hemorrhages during menopause in women over 40–45 years of age are the reason for urgent treatment at the hospital. Pathology is considered to be bleeding for more than 7 days, resumption of menstruation in less than 20 days, and the need to change sanitary pads more than once every 2 hours. Prolonged uterine bleeding during menopause often leads to anemia. Patients note general weakness, dizziness, fatigue, and pasty skin.
Classification of pathological bleeding:
- menorrhagia;
- metrorrhagia;
- menometrorrhagia;
- polymenorrhea.
Menorrhagia is characterized by regular periods lasting more than 7 days, or heavy discharge of more than 80 ml/day. Menorrhagia is the irregular appearance of bloody secretions in small quantities. Signs of menometrorrhagia include systematic bleeding at various intervals, and polymenorrhea - regular menstruation with an interval of less than 21 days.
Preventive measures
To avoid problems during menopause, you need to fulfill the following requirements:
- The most important measure for the prevention of uterine bleeding is a timely visit to the gynecologist. Women over 40 years old should visit it at least once every six months.
- It is also important to observe the rules of hygiene of the intimate area. During this period, a woman experiences changes in the structure of her genital organs; they become more vulnerable to external influences and infectious lesions. Keeping this area clean, using bactericidal detergents and frequently changing linen will protect the woman’s body from unnecessary problems.
- If possible, you should live with one sexual partner, preferably your husband. But at this age, many women are lonely and not everyone has a permanent partner. Therefore, you need to use a condom to avoid catching some kind of sexually transmitted disease.
- It is also important not to get pregnant during this period. During the first time of menopause, this possibility still exists, but the fetus can rarely be full-fledged. Most often, such a pregnancy does not bring joy, but, on the contrary, it only causes problems.
- Regularly check the condition of the thyroid gland and hormonal balance in the blood. If pathologies occur, take timely treatment.
- Avoid stressful situations, do not overexert yourself and do not overexert yourself physically.
During menopause, a woman’s body changes not only, but also her psychological state. Therefore, she needs a lot of positive emotions at this time. She needs to communicate with people, walk in the fresh air, eat well and properly. Usually at this age children are already adults, and it is time for a woman to pay more attention to herself.
https://youtu.be/OakcMyFUH9M
Diagnostic tests
To establish a diagnosis and determine the cause of bleeding during menopause, a bimanual examination of the genital organs is performed. Additionally, gynecological smears, laboratory tests and instrumental diagnostics are performed. A consultation with a gynecologist-endocrinologist is required; if a cancerous tumor is suspected, it is recommended to visit an oncologist.
List of clinical tests:
- general blood test, urine test;
- hCG level test to exclude premenopausal gestation;
- studies on the concentration of sexual hormones;
- analysis for tumor markers;
- coagulogram;
- cervical smear to check for cancer cells;
- analysis of the level of thyroid hormones – TSH, T3, T4;
- blood chemistry.
To assess the condition of the uterus and appendages, MRI, ultrasound, angioscanning of blood vessels, hysteroscopy, and colposcopy of the uterus are performed. If cancer is suspected, a piece of tissue is taken for biopsy, and diagnostic curettage of the endometrium and cervical canal is prescribed with further morphological analysis.
Diagnostics
To identify all possible causes of uterine bleeding during menopause (they can be combined), diagnosis is performed in several stages.
At the first stage of the examination, the woman consults a gynecologist-endocrinologist, who should have experience in managing patients with menopausal problems. The doctor carefully studies the patient’s complaints and analyzes her monthly bleeding schedule. After this, a gynecological examination is performed on a chair using a mirror, during which a specialist can assess the nature and abundance of the discharge. In some cases, this procedure makes it possible to identify the source of bleeding. Outside the bleeding period, material is collected to perform a smear for oncology.
At the second stage of diagnosis, the patient is prescribed a transvaginal ultrasound. Such a study makes it possible to identify pathologies of the genital organs and confirm or exclude the fact of pregnancy. In addition, the patient is prescribed laboratory tests:
- general and biochemical blood test;
- blood test for thyroid hormones;
- coagulogram;
- blood test for sex hormones and gonadotropins;
- blood test for β-hCG levels;
- blood test for tumor markers.
An important part of the diagnosis for pathological uterine bleeding during menopause is to conduct a separate diagnostic curettage of the uterine cavity under the control of hysteroscopy. Scraping of endometrial tissue makes it possible to perform a histological examination of the sample and conduct a differential diagnosis between dysfunctional blood loss and bleeding caused by organic pathologies of the genital area.
As additional diagnostic methods, patients may be prescribed the following procedures:
- MRI of the pelvic organs;
- hysterosalpingography;
- color Dopplerography of the vessels of the genital organs.
How is uterine bleeding treated?
Treatment methods for metrorrhagia are selected taking into account the primary cause that caused bleeding during menopause. The goal of treatment is to stop blood loss, restore hemostasis, generally strengthen the body and prevent relapses. In some cases, only medication is required. In case of heavy, pathological hemorrhages, surgical curettage of the endometrium is performed. After surgery, hormonal therapy is prescribed.
Ways to stop bleeding
If symptoms of uterine bleeding appear during menopause, how to stop it before the ambulance arrives? The patient must be laid on a flat surface, with a soft cushion placed under her feet, this will reduce blood flow to the lower part of the body.
A cold compress on the abdominal area will help relieve the condition and relieve cramps. You can use ice wrapped in cotton cloth or a rubber heating pad filled with ice water. Cold causes blood vessels to constrict, which slows down blood loss.
Heavy bleeding in postmenopause can lead to dehydration, anemia, and loss of consciousness. To maintain your water balance, you should drink more fluids. It is useful to drink sweet tea; sugar replenishes glucose deficiency and gives energy.
In case of uterine bleeding, it is prohibited:
- apply heat to the stomach;
- take medications on your own;
- perform douching;
- take a shower, bath;
- lift loads.
Important! Heavy bleeding after menopause should greatly alert a woman. In order to clarify the cause and further treatment of metrorrhagia, you should immediately consult a doctor!
Therapy for menopausal bleeding
Surgical curettage of the cervical canal and uterine cavity is the primary method of treating bleeding during menopause, the causes of which are not clear. The procedure allows you to quickly restore hemostasis, examine the collected tissues, and perform differential diagnostics.
At the initial stage of menopause, bleeding is treated with gestagens; drugs of this group (Norkolut, Pregnin) are used up to 48 years. Drug therapy is prescribed after diagnostic curettage of the uterus and stopping metrorrhagia. Hormonal drugs are taken from 6 months to 2 years, the ultimate goal of treatment is the permanent cessation of menstruation.
Treatment of pathologists in postmenopause
The presence of bleeding during menopause after menopause requires hormonal therapy. Women are prescribed drugs with low estrogen content, androgens, or combination drugs. Androgens (Testosterone Propionate, Methyltestosterone) are used to treat patients over 48 years of age with glandular cystic endometrial hyperplasia and an increase in the size of the uterus.
Drug treatment
For moderate anemia (hemoglobin level above 100 g/l), hemostatic drugs are prescribed: Vikasol, Menadione, Ascorutin, Etamzilat. Oxytocin injections are given to contract the walls of the uterus. Prostaglandin synthetase inhibitors (Naproxen, Flurbiprofen) increase endometrial vasospasm and stimulate platelet aggregation.
Taking into account the cause of bleeding, hormonal agents based on gestagens (Gestaden, Progesterone) can be prescribed. The drugs promote digital tissue atrophy. For endometriosis and hyperplasia of the inner layer of the uterus, women are prescribed anti-estrogenic drugs (Danodiol, Gestrinone). Their action is aimed at regressing pathological foci, reducing endometrial tissue, and relieving pain.
After stopping the bleeding, the doctor prescribes therapy for the underlying disease that caused the metrorrhagia. Treatment tactics are selected taking into account the nature of the identified pathology.
The effectiveness of ultrasound ablation
If conservative therapy is ineffective for uterine bleeding, ultrasound ablation of the endometrium is performed. During the procedure, a low-traumatic removal of the inner layer of the uterus occurs, which leads to the cessation of blood loss. A special instrument is inserted into the cavity of the reproductive organ, with the help of which ultrasonic waves are applied.
Types of endometrial ablation:
- electrical – destroys the endometrium with electric current;
- microwave - occurs due to an increase in the temperature of the upper layer of the mucous membrane;
- hydrothermoablation – performed using heated silicone;
- cold endometrial resection is performed by freezing the tissue.
The treatment procedure is indicated during menopause and premenopause. The recovery period lasts 7–10 days. In the first few days, you may experience nausea, cramps, and frequent urge to empty your bladder. Bloody or clear discharge persists for up to 3 weeks.
Treatment is not advisable in postmenopause, with cancerous tumors, infectious diseases of the urogenital tract.
What happens in the female body with the onset of menopause?
All physiological signs of the female body are associated with the ability to bear children. The organs that form a single whole at the birth of the follicle and before the fertilization of the egg are closely interconnected. Any disruption in the reproductive chain of female organs with age leads to physiological menopause. In other words, menopause is a natural process that is associated with the decline of the functional state of the ovaries.
Menopause consists of several successive periods, each of which is characterized by individual characteristics:
- Premenopausal period. This is the initial stage of menopause, during which, against the background of a decrease in estrogen production, a hormonal imbalance occurs in a woman’s body in the form of a violation of the cyclicity of menstruation.
- Menopause period. The average duration of the menopause stage. It begins from the moment of the last menstruation and is characterized by its complete absence for 12 months.
- Postmenopausal period. The longest stage of the menopause. It is characterized by a complete absence of the ability to give birth and pronounced attacks (hot flashes, fever, chills).
During each period of menopause, a woman may experience a different type of discharge, which can be either in the form of spotting or heavy bleeding. The causes of these blood losses are different, let’s look at each of them.
First aid and treatment
Treatment for bleeding depends on what causes it. How and how to treat bleeding caused by any reason can only be decided by a qualified doctor. The woman must remain in bed. But basically the following is prescribed:
- Coldness in the lower abdomen. It will help reduce blood loss. Because the blood vessels narrow.
- Drink plenty of fluids. The body must receive the required amount of fluid to replenish the loss.
- Hemostatic drugs.
- Hormonal drugs. Helps stop bleeding.
- Surgical treatment: curettage, cryodestruction, endometrial ablation (removal with laser).
The nature of menstruation during menopause
Changes in the menstrual cycle during menopause occur individually. The nature of menstruation will be influenced by genetic predisposition, the presence of concomitant diseases, as well as the age of the patient.
In practice, the following types of changes in the menstrual cycle are encountered:
- A gradual increase in the time intervals between menstruation until they stop completely.
- An abrupt stop of menstruation, while other symptoms characteristic of premenopause are observed.
- Increasing the duration of the cycle to 3-4 months and the subsequent onset of menopause.
- Cycle failures, alternating duration and nature of discharge. Scanty periods give way to heavy and prolonged ones.
To monitor changes in a woman’s condition and promptly identify deviations, it is recommended to visit a gynecologist once every six months.
Periodicity of menstruation during menopause
Menstruation at the onset of menopause can have different durations and intensity. As menopause approaches, the interval between them can increase to 3 months. If spotting is not observed within a year from the last menstruation, it is considered that menopause has occurred.
Heavy periods during menopause
If during menopause - premenopause - you get your period, this is considered normal. However, if heavy bleeding is noted after menopause, you should consult a specialist.
In some cases, consultation with a doctor will be required before menopause. When bleeding is so heavy that a sanitary pad fills in an hour or less, it indicates the development of underlying medical conditions. These include:
- polyp;
- myoma;
- inflammatory process in the vagina;
- uterine prolapse;
- malignant neoplasm.
In addition to the pathologies listed above, heavy bleeding can be provoked by certain medications, as well as poor blood clotting and cystitis.
Prolonged periods during menopause
Menstruation lasting more than 7 days can be called protracted. Long periods before menopause are explained by the following factors:
- poor blood clotting;
- polycystic disease is a disease of the ovaries, which is characterized by a long absence of menstruation, followed by heavy discharge;
- neoplasms such as polyps and fibroids;
- pathologies of the endometrium, in which its pathological growth occurs as a result of failures in the development of the egg;
- incorrect use of oral contraceptives or discontinuation of the course.
To identify the cause of long periods during menopause, the doctor prescribes an ultrasound of the pelvic organs, a blood test (including assessment of coagulation parameters), and a cytological examination of a smear from the cervix. If serious pathologies are excluded, hormonal drugs and sedatives are prescribed.
Frequent periods during menopause
During premenopause, another type of cycle disorder occurs - frequent menstruation. As a result of hormonal imbalance, ovulation fails and anovulatory cycles develop. These processes provoke frequent periods. Subsequently, the intervals begin to lengthen again, and delays appear.
Painful periods during menopause
Painful sensations during menstruation during menopause are not a deviation from the norm. It may also be accompanied by a general deterioration in health, dizziness, and irritability.
Dark periods during menopause
Not in all cases, dark periods against the background of cycle disruption during menopause should be a cause for concern. Blood acquires a brown tint as a result of mixing with vaginal secretions.
However, if you have the following symptoms, you should consult a doctor:
- painful sensations;
- presence of watery or yellowish discharge;
- frequent urination;
- uterine bleeding;
- pain during sexual intercourse;
- burning, itching;
- depression;
- vaginal dryness;
- mouth ulcers;
- loss of appetite.
Brown discharge along with the above symptoms may indicate the presence of pathologies. Dark periods during menopause in women occur with vaginal infections such as gonorrhea or chlamydia. They may also indicate the presence of polyps in the uterus. Therefore, if you notice accompanying symptoms, you should immediately consult your doctor.
Is uterine bleeding normal during menopause?
It is difficult to say why, but uterine bleeding during menopause is often not perceived by women as a dangerous signal. It is no secret that under the influence of hormonal changes, global restructuring occurs in the body. It also affects the sexual sphere. For example, changes may manifest themselves in shortening or lengthening the menstrual cycle or duration of menstruation, increasing or decreasing the amount of discharge.
However, it is necessary to distinguish between blood loss associated with changes in the menstrual cycle and blood loss that is independent. Any bleeding during menopause may also have a pathological underlying cause, which requires medical consultation. A woman should be wary of the following indicators:
- excessively heavy menstruation during the period until premenopause has ended;
- copious discharge of blood clots;
- intermenstrual menopausal bleeding;
- reducing cycle duration to 21 days or less;
- an increase in the duration of menstrual flow (up to 7 days or more), and repeated repetition of this phenomenon.
Premenopause is characterized by the persistence of menstruation, but during this period several types of pathological cyclic discharge may occur. Depending on their duration, intensity and abundance, there is the following classification:
- Mennorrhagia is prolonged intense menstruation that lasts more than a week and repeats several cycles in a row.
- Metrorrhagia is discharge of varying intensity that is recorded during the period between menstruation. With this type of blood loss, the presence of mucous inclusions is possible.
- Menometrorrhagia is a discharge that is profuse and occurs spontaneously, regardless of the menstrual cycle.
- Polymenorrhea is bleeding that occurs regularly at intervals of less than 21 days.
If a woman notices any of the above conditions, then she should not hesitate to visit a gynecologist. These pathological blood losses can be both a characteristic sign of approaching menopause and a symptom of ailments of various etiologies.
This symptom can indicate the presence of serious pathological changes, delay in treatment of which can be fatal.
Kinds
Depending on the time of occurrence:
- In newborns, uterine bleeding usually occurs in the first week of life. It is associated with hormonal changes in the body. There is no need for treatment, as everything goes away on its own.
- Uterine bleeding before puberty. The phenomenon is typical for girls under 10 years of age. The pathology is associated with ovarian tumors, as they secrete large amounts of sex hormones.
- Juvenile uterine bleeding. They occur in girls during the period of active hormonal changes in the body, from 12-18 years. They are associated with dysfunction of the ovaries.
- Bleeding during the reproductive period. Occur between the ages of 18-45 and can be dysfunctional, organic, associated with pregnancy or childbirth.
- Bleeding during menopause. The reason for this is a disruption in the production of hormones or diseases of the genital area.
Depending on the reason:
- Iatrogenic : due to taking hormonal contraceptives and non-hormonal contraceptives. And also after installation of the IUD.
- Organic : damage to internal organs (diseases of the blood, liver) or pathologies and genital organs.
- Dysfunctional : ovulatory and anovulatory.
Juvenile
Bleeding is typical for girls entering puberty. Approximately 12-18 years. Usually the phenomenon is anovulatory in nature: an egg is not formed. The cause of this pathology may lie in dysfunction of the ovaries. The following unfavorable factors can lead to this:
- Low immunity.
- Frequent illnesses (flu, ARVI, etc.).
- Improper and irregular nutrition.
- Lack of vitamins.
- Tumors of the ovaries, cervix and uterine body.
- Chronic infections.
- Excessive physical activity.
- Tuberculous lesions of the genital organs.
- Blood clotting disorder.
Attention! Bleeding is seasonal. In the autumn and spring periods, complications of diseases are observed, as well as the occurrence of uterine bleeding.
With prolonged course of the disease, anemia may develop. Uterine bleeding at this age should be treated in a hospital setting:
- For this purpose, hemostatic drugs, vitamins, and iron are used.
- Physical therapy is prescribed.
- Nutrition during periods of poor health should be regular and balanced in vitamins and minerals.
- If the bleeding does not stop for a long time, then hormonal drugs are used.
In the future, the patient takes medications to normalize the menstrual cycle.
During reproductive age
This is the period from 18 to 45 years. The reasons may be the following:
- Ovarian tumors that cause active production of hormones.
- Uterine fibroids.
- Endometriosis.
- Uterine tumors are both benign and malignant.
- Chronic endometritis.
- Cervical diseases.
- Miscarriage.
- Abortion.
- Ectopic pregnancy.
- Hormonal disorders.
- Predisposing factors:
- Stress.
- Physical exercise.
- Infections.
- Excess weight.
- Poisoning with toxic substances.
- Taking certain medications.
- Diabetes.
Important! There are many reasons for uterine bleeding during reproductive age, so when treating pathology, you must first identify and eliminate the main one.
Classification and causes of uterine bleeding
The appearance of bleeding at each stage of menopause, first of all, signals serious problems in the female body. Most often, women attribute these phenomena to fatigue, illness, or the use of medications. This is just self-consolation. And the reasons can be so critical that life may even be threatened, especially in cases where diseases such as uterine fibroids, endometriosis or adenomyosis were previously diagnosed.
Uterine bleeding is classified depending on the volume of discharge:
- menorrhagia - heavy blood loss during premenopause;
- metrorrhagia – minor irregular blood loss;
- menometrorrhagia – blood loss that combines signs of menorrhagia and metrorrhagia;
- polymenorrhea - heavy and prolonged menstruation.
Reason one
During perimenopause, bleeding may range from spotty dark to bright red heavy discharge with small blood clots. The reason for this is the onset of ovarian dysfunction and a lack of progesterone production, as a result of which some of the follicles do not mature and lead to disruptions in the menstrual cycle.
Menstruation may come with delays and be accompanied by nagging and aching pain in the lower abdomen, in the appendage area, and in the lower back. During this period, a woman seems to be bursting. She is gaining weight, her stomach is noticeably increasing in volume. It is at such moments that a woman has doubts about an unplanned pregnancy. During this period, it is important to use reliable contraception.
Bleeding during irregular periods can be either scanty or heavy. This is explained by a violation of the integrity of the endometrial surface and its functional rejection. As a result, endometrial detachment occurs in pieces and may come out unevenly.
During this period, it is important for a woman to control her body weight and monitor the course of her periods. If the pad is changed more often than once every two hours, you need to undergo an examination to rule out other causes of bleeding.
Reason two
Since during menopause the ovaries continue to reproduce follicles for a short time, women during this period still try to protect themselves with hormonal drugs. Synthesized progesterone, which is part of these drugs, can create destabilization of ovarian function and cause bleeding in the middle of the cycle.
Reason three
Sudden heavy bleeding at any stage of menopause may have other causes associated with pathology of the pelvic organs.
These reasons include diseases of the uterus and ovaries of benign and malignant origin. These include diseases such as uterine fibroids, polyps on the walls of the uterus, endometrial hyperplastic process, adenomyosis, and ovarian cyst.
Each of these diseases has its own functional origin, which causes bleeding:
- Uterine fibroids can be benign or malignant. As a rule, it occurs even before the onset of menopause as a result of hormonal imbalance. It is a tumor on the wall of the uterus, which creates an irritant for the uterus and causes its constant contractions, accompanied by sharp pain and discharge at any time of the cycle. Menstruation is expressed by menorrhagia. Myoma grows until the end of menopause, then its growth stops. The growth of fibroids during menopause may indicate its malignant degeneration.
- Hyperplastic process of the endometrium or adenomyosis. These two diseases often go together. Under normal conditions, the upper layer of the endometrium peels off during menstruation and comes out. As endometriosis progresses, endometrial cells grow deep into the uterine wall, thickening it. Endometrial cells become hyperemic and filled with blood. Oversaturation of cells leads to sudden rejection of the upper layer of the endometrium. The bleeding is profuse, with dark red endometrial clots.
- Ovarian cyst. Develops against the background of general hormonal imbalance. A cyst can have different origins, one of which is functional. Cysts themselves do not disappear, but their presence inside or outside the ovary inhibits the development of follicles, thereby causing irregular periods.
- Uterine polyps. They are small growths on the inner surface of the uterus, which over time can enlarge and cause metrorrhagia. Bleeding occurs when epithelial cells filled with blood separate from the polyps. The danger of polyps is that epithelial tissue can degenerate into cancer cells.
Do not confuse uterine bleeding with vaginal bleeding, in which functional and physiological changes in the vaginal walls with the onset of menopause take on a pathological character that can only be detected by a gynecologist. This is not dangerous, but also requires treatment to prevent other bacterial diseases from occurring.
When stopping bleeding, you need to seriously understand the current state of the body during menopause. Stopping does not mean eliminating the cause of the problem.
How to stop uterine bleeding during menopause?
First of all, you need to take a lying position, your legs should be slightly raised at the knees, and place a rubber heating pad with ice on your lower abdomen. It is necessary to take into account that the cold cannot be kept for more than 1-2 hours, otherwise inflammation of the appendages will be added to stopping the bleeding.
Can be taken for uterine bleeding from the medications Vikasol, Ascorutin, Tranexam, Etamzilat. These drugs have a long-term coagulant effect, increase blood clotting and improve the strength of blood vessel walls. But we should not forget that these drugs are contraindicated for other diseases, so before taking the drug, you must read the instructions.
It is safest to use herbal infusions, which have the same properties as medicines, but not in a pronounced effect. Before use, you need to pay attention to whether you are allergic to a particular herb.
These herbs include:
- Yarrow. The infusion is prepared based on 200 ml of boiling water, add 2 teaspoons of pharmaceutical herbs. Leave for 1 hour. Use ¼ cup before meals.
- Stinging nettle. An infusion is prepared with 200 ml of water, two tablespoons of pharmaceutical herbs are added and boiled for 10-15 minutes. Apply one tablespoon every three hours.
- Shepherd's purse. The infusion is made at the rate of 200 ml of boiling water, add one tablespoon of pharmaceutical herb. Leave for 1 hour. Use 1 tablespoon at least three times a day.
These tips are for advisory purposes only. They apply, first of all, to women who, due to territorial situations, cannot get to a medical institution within the next 24 hours. In any case, the ultimate goal for a patient with bleeding during menopause is hospitalization.
In conclusion, we inform you that any bleeding during menopause can lead to iron deficiency anemia and loss of consciousness. For your own safety, do not experiment on your body, call a doctor and do not be afraid. Uterine bleeding does not always require surgical intervention. The main thing is to help yourself in time.
Full treatment of uterine bleeding during menopause is carried out based on the diagnosis. The first thing that is required during emergency hospitalization of a patient is to stop the intense blood loss. For this purpose, hemostatic drugs are used: Vikasol, Dicion, aminocaproic acid, as well as hormonal drugs. Vikasol is also used to stop heavy periods.
If blood loss does not pose a threat to the woman’s condition, and its cause is a hormonal imbalance, then the woman is prescribed hormone replacement therapy. An alternative option may be the use of oral contraceptives. If a woman is still going through premenopause, they will not only help prevent recurrent bleeding, but also protect against unplanned pregnancy.
Treatment
If menopausal bleeding occurs, a woman should immediately consult a doctor, and in case of excessive bleeding and signs of post-hemorrhagic anemia (weakness, loss of consciousness, dizziness), call emergency help. Treatment of any bleeding during pre- or postmenopause is carried out only in a hospital and begins with separate curettage, which is not only diagnostic, but also therapeutic. After curettage, drug therapy is prescribed. In order to further stop bleeding, the following is administered:
- uterotonics (contractors) – oxytocin, methylergometrine;
- hemostatic drugs (tranexam, aminocaproic acid, sodium etamsylate - intramuscular and intravenous);
- intravenous infusions of saline solutions (physiological, glucose solution and others) in order to restore the volume of circulating blood;
- blood transfusions (according to indications) - administration of red blood cells, cryoprecipitate, platelets;
- prescription of iron-containing drugs (hemoglobin restoration).
After bleeding stops, hormonal therapy is prescribed (long-term). Treatment with hormones is selected individually and depends on the woman’s age, concomitant gynecological and extragenital pathology. After 55 years, it is recommended to take antiestrogenic drugs (danazol, gestrinone). In the presence of uterine fibroids, the following may be prescribed:
- Gonadotropin-releasing factor agonists:
- diferilin or triptorelin - taken from the 3rd day of menstruation for six months;
- goserilin or buserelin – at least 6 months;
- Zoladex injections from the 1st to the 5th day of menstruation.
- Antagonists of gonadotropic hormones:
- norethisterone – from the 5th day of menstruation, 5–10 mg orally daily for six months;
- medroxyprogesterone - a similar regimen as when taking norethisterone;
- installation of the Mirena IUD - an intrauterine contraceptive with a hormonal component;
- norkolut or primolut - from 16 (in some cases from 5) days to 25.
Norkolut/primolut is also prescribed to women aged 45 to 55 years according to the regimen recommended above.
Further treatment with combined oral contraceptives (Logest, Tri-Regol) or hormonal antimenopausal drugs (Livial, Kliogest, Klimonorm, Femoston and others) is also allowed.
Surgical intervention for menopausal bleeding (complete or partial removal of the uterus) is carried out in the following cases:
- adenocarcinoma (cancer) of the uterus;
- atypical endometrial hyperplasia;
- multiple uterine fibroids of significant size;
- submucosal uterine fibroids;
- combinations of fibroids and uterine endometriosis.
First aid
What to do if menopausal bleeding occurs at home and how to stop it? First of all, a woman needs to calm down, not panic and pull herself together. If the bleeding is very heavy, you should call an ambulance; in case of moderate bleeding, a number of measures must be taken:
- lie down in bed, placing a cushion or pillow under the lumbar region to facilitate the outflow of blood and normalize blood circulation in other organs;
- apply a bubble of cold water or ice to the lower abdomen (be sure to wrap it in a diaper) - the duration of the cold on the abdomen is 15 minutes with 5-minute breaks, and the total is about 2 hours;
- consume large amounts of sweet liquid (tea, rosehip decoction, fruit drinks) in order to restore water balance.
It is strictly prohibited:
- taking warm or hot baths;
- douching;
- performing any, especially strenuous, physical exercises and heavy lifting;
- sexual intercourse;
- taking a horizontal position with raising the lower extremities - this position retains blood in the uterine cavity and contributes to the formation of hematometra.
Folk remedies
To prepare the decoction, add 4 tablespoons of dry leaves to a glass of water and simmer over low heat for 10 minutes. Strain the broth and take a tablespoon 4 – 5 times a day.
Ripe viburnum berries should be crushed and mixed with a small amount of sugar. Dilute the mixture with boiled water 1:1. Take one tablespoon three times a day (an essential source of vitamin C, which has a hemostatic effect).
Pour 2 teaspoons of dry herb with a glass of boiling water and leave for an hour. Strain the infusion and take a quarter glass four times a day.
Pour a tablespoon of dry raw material into a glass of boiling water and leave for an hour. Strain the infusion and drink a tablespoon 4 times a day before meals.
Wash the peels of 5 to 6 oranges and pour one and a half liters of boiling water, leave for an hour, strain and drink 4 tablespoons 3 to 5 times a day.
Take a third of a glass of freshly squeezed beet juice three times a day.
How to diagnose pathology?
Reason three
Let's consider the pathological conditions that most often cause bleeding during menopause.
This is a common culprit of this disease. A decrease in the production of estrogen by the ovaries in a woman’s body leads to a whole complex of transformations that directly affect the activity of the reproductive organs. Against the background of a hormonal imbalance, uterine bleeding is quite possible. Their nature and intensity can vary significantly in each individual case.
Sometimes bleeding during menopause is provoked by taking hormonal medications used to minimize the pathological manifestations of menopause. Most often, such discharge is moderate in nature, sometimes it is not even bleeding in the literal sense of the word, but smearing.
Taking oral contraceptives during premenopause can also act as a provocateur of this unpleasant phenomenon. As a rule, this is explained either by the fact that the product was chosen incorrectly, or by the individual reaction of the woman’s body. Sometimes bloody vaginal discharge, if it appears in the first months of taking OCs, can be explained by the body’s adaptation to this drug.
Uterine fibroids
Uterine fibroids are a benign neoplasm that develops against the background of a violation of the quantitative ratio of estrogens and progestins. Typically, this neoplasm increases the intensity and duration of discharge during menstruation, however, in some cases, bleeding may be noted in the middle of the cycle.
The disease is an abnormal growth of the basal or functional layers of the endometrium, in which endometrial cells grow into the deeper layers of the uterus. Periodically, the mucous layer is rejected, which provokes bloody discharge. It should be noted that such a symptom is not always characteristic of hyperplasia in menopause; very often it develops asymptomatically. The danger of this disease lies in the possibility of malignant degeneration of cells.
Uterine polyps
This is one of the forms of endometrial hyperplasia that develops locally. Polyps are peculiar growths on a stalk in which a large number of blood vessels are concentrated. When these formations are injured, bleeding begins. Most often it is of a moderate nature. In some cases, blood is not removed from the uterine cavity immediately, but after some time.
Hypothyroidism
A lack of thyroid hormones quite often leads to a woman experiencing heavy bleeding.
Oncology
After menopause, a similar reason for the occurrence of the phenomenon in question is not at all uncommon. Unfortunately, cancer of the reproductive organs most often does not manifest itself in any way at the initial stage. Discharge with blood is a dangerous sign, especially if it is accompanied by an unpleasant odor, pain in the lower abdomen and lower back, general weakness and malaise. The intensity of bleeding may vary.
Pregnancy
Perimenopause is an insidious time when, due to disruptions in the menstrual cycle, it is easy to miss the conception that has occurred. Bloody discharge in this case may accompany an ectopic pregnancy or indicate a threat of miscarriage.
Coagulopathy
Coagulopathy (that is, a violation of the blood clotting process) can also cause intense blood loss, threatening the health and life of a woman. Diagnosis of uterine bleeding
Establishing the main causes of uterine bleeding during menopause is the most important condition for successful therapy. Since a wide variety of conditions and diseases can cause this pathology, diagnosis can become quite problematic. To make an accurate diagnosis, you may need to undergo a comprehensive examination, which includes the following methods:
- direct examination by a gynecologist, combined with a detailed questioning of the patient about the characteristics of her condition;
- general analysis of urine and blood;
- hysteroscopy;
- blood test for hormone concentrations;
- analysis for hCG hormone (to exclude the possibility of pregnancy);
- blood testing for the presence of tumor markers;
- blood clotting test;
- transvaginal ultrasound;
- taking a smear for cytology from the cervical canal of the uterus;
- endometrial tissue biopsy;
- sonohysterography - ultrasound examination of the uterus and fallopian tubes with preliminary administration of saline;
- color Doppler mapping;
- MRI of the pelvic organs;
- morphological study of the endometrium.
After collecting the information necessary for diagnosis, there may be a need for additional examination of the patient by specialized specialists: endocrinologist, hematologist, oncologist.
Menopausal bleeding requires careful diagnosis using the most modern methods. Only they can accurately establish the diagnosis, the cause, and only then can treatment be prescribed. First of all, you will need a detailed medical history, in which the doctor will find out the symptoms, history of the onset of menstruation, childbirth, abortion, surgery and other manipulations.
The doctor may also ask about breastfeeding and the presence of gynecological diseases in close relatives. A thorough gynecological examination is required, during which smears are taken from the vagina. Based on initial examinations, the following diagnostic procedures can be prescribed:
- Testing for a hormonal panel, blood testing and blood clotting.
- Additional studies of the liver, kidneys, and thyroid gland.
- Testing for tumor markers, liver tests.
- A vaginal or transvaginal ultrasound is performed.
- A biopsy is performed and biological material is examined to detect cancer.
- An MRI of the pelvic organs is performed
Depending on the results of the study, additional examination procedures may be prescribed. Sometimes the diagnosis of uterine bleeding requires consultation not only with a gynecologist, but also with an endocrinologist, mammologist, oncologist, therapist, and hematologist. If a woman has a number of concomitant diseases, then this problem must be solved comprehensively, using all available specialists.
Possible causes of bleeding during menopause in the premenopausal period include:
- Hormonal imbalance
Due to suppression of the ovaries and rare maturation of eggs, menstruation becomes irregular. As a result, during the period of absence of menstruation, the endometrium grows significantly, which leads to significant bleeding.
Myomatous nodes not only increase the area of the uterine cavity, and, accordingly, the endometrium, but also disrupt the contractile function of the uterus. These factors cause bleeding.
Endometrial polyps also significantly increase its area, in addition, the presence of polyps indicates a hormonal imbalance. Bloody discharge becomes not only abundant, but also irregular.
Excessive growth of the inner layer of the uterus, which is accompanied by copious bleeding.
Wearing an IUD causes an increase in bleeding (excessive contraction of the uterus).
With regular use, the amount of blood lost during menstruation is significantly reduced, but if you take a break or stop taking it, bleeding may occur.
- Pathology of the thyroid gland
Thyroid hormones, to a certain extent, influence the menstrual cycle. Both with their deficiency (hypothyroidism) and with their excess (hyperthyroidism), uterine bleeding appears.
- Scleropolycystic ovarian disease
The pathology is accompanied by long-term, up to 6 months, delays in menstruation, which leads to the development of endometrial hyperplasia and, as a consequence, uterine bleeding.
- Taking anticoagulants or bleeding disorders
Both lead to “thinning” of the blood and provoke uterine bleeding.
The following factors can provoke excessive bleeding:
- heavy physical activity;
- stress;
- rise in blood pressure;
- acute infectious disease;
- constipation;
- cough;
- sexual intercourse
And although with age (45) the chances of getting pregnant decrease sharply, pregnancy is still possible. As a rule, if women miss their periods for more than three cycles, they stop taking precautions, which can result in an unexpected pregnancy. Pregnancy at a late age often occurs with pathology (ectopic or threatened miscarriage), which is accompanied by bloody discharge, often profuse.
Postmenopausal
In postmenopause, there should be no bleeding of any intensity. The only factor that explains the appearance of spotting and is considered normal is hormone replacement therapy (estrogens plus progesterone). All other cases of bleeding and bleeding indicate pathology:
- uterine fibroids (although fibroids usually disappear with the cessation of menstruation);
- polyposis and endometrial hyperplasia;
- atrophic colpitis.
But postmenopausal bleeding should first of all suggest the presence of malignant tumors:
- cervical cancer;
- ovarian cancer;
- endometrial cancer.
Caused by pregnancy and childbirth
In the early stages of pregnancy, bleeding can only mean one thing, the threat of miscarriage. If you consult a doctor when a pathology is detected, the pregnancy can be saved. Otherwise, curettage will be necessary.
Bleeding, which is accompanied by signs of pregnancy and is additionally accompanied by pain in the lower abdomen, is characteristic of an ectopic pregnancy. In this case, the fertilized egg is attached not to the uterine cavity, but to the fallopian tubes or ovary. In this case, the help of a doctor will be simply necessary. This condition is fatal to a woman's life.
In the second half of pregnancy, bleeding is very dangerous for the life of mother and child. This is due to the fact that it usually occurs with incorrect placenta previa or abruption, or uterine rupture. Bleeding can be internal or external. But in any case, emergency help from specialists is needed.
Bleeding during or after childbirth is a consequence of placental pathology or poor uterine tone. Poor blood clotting or incompletely expelled membranes are also the cause.
During menopause (menopause and postmenopause)
The causes of bleeding after 45 years are hormonal changes in the body. Therefore, bleeding may sometimes occur. But this does not mean that you do not need to see a doctor. Sometimes pathology can signal painful processes in the cervix or body of the uterus.
Even if minor bleeding appears, you need to consult a doctor, because this can be a sign of tumors. In the early stages, neoplasms can still be treated. You should especially be wary of bleeding after menstruation has completely stopped. The condition is usually treated with hormones.
Dysfunctional
Such bleeding occurs in women at any age. The pathology is associated with impaired production of sex hormones. It manifests itself in the form of an irregular monthly cycle: menstruation lengthens, and the amount of discharge also increases. In addition, the cycle itself is irregular. Sometimes the period between menstruation can range from several months to six months.
The pathology is usually of an ovulatory nature, which usually occurs in women of reproductive age. And also anovulatory, it is typical for adolescence and women during menopause. Intervals can be not only long, but also short (up to 21 days).
Prolonged bleeding, especially if treatment is ignored, leads to anemia. Possibly also infertility or miscarriages, diseases of the uterus, such as endometriosis. Hormones are prescribed and concomitant diseases are treated. If conservative treatment is ineffective, surgical treatment is prescribed.
Important! Heavy bleeding can result in death.
Breakthrough
Usually characteristic when taking hormonal contraceptives. This is a kind of adaptation of the body to this drug. But if these bleedings do not correspond to the menstrual cycle, then you should consult your doctor so that he can adjust the dose or select another medication.
Bleeding may occur after insertion of an intrauterine device. This means that damage to the uterine wall has occurred. In this case, the help of a specialist is simply necessary.
Breakthrough bleeding mainly occurs due to an imbalance of hormones : estrogen and progesterone. Discharge with this pathology is insignificant, but in any case you need to consult a gynecologist.
Defeat of individual systems
Also, bleeding in the uterus during menopause can occur due to severe disruptions in the body that occur when the production of hormones, blood clotting, and other difficulties in metabolic processes are disrupted.
Most often, such lesions occur during hypothyroidism. Difficulties in the functioning of the thyroid gland can occur due to injury, the presence of cancer, or inflammation. Symptoms do not appear immediately, so the disease in most cases is detected already at the last stage of development.
In addition, bleeding in the uterus during menopause can lead to blood clotting disorders
It will be quite difficult to diagnose such a disease, and it is very important to use some diagnostic equipment. In this case, the woman’s condition can be improved with the help of medications with a hemostatic effect or through blood transfusion
Iatrogenic bleeding
Iatrogenic bleeding begins as a result of an incorrectly performed operation or the use of certain medications. This primarily applies to medications that help thin the blood and also prevent blood clots from forming.
The bleeding process begins abruptly and continues for several days. It can be either very strong or insignificant, in any case the woman loses a certain amount of blood
In this case, it is important to stop taking the medication that caused the bleeding process. To improve the general condition of the patient, it is necessary to use hemostatic drugs
Perimenopause and bleeding
The postmenopausal period is described by the fact that significant hormonal changes occur in a woman’s body. As a result, this leads to the woman suddenly experiencing heavy bleeding.
At this time, it is very important to begin to closely monitor all the changes that occur in the body. A consultation with your doctor is required if:
- there is too much discharge and it continues for quite a long time;
- there are characteristic clots;
- no menstruation for several months;
- bleeding occurs after sexual intercourse.
Heavy bleeding may indicate that polyps have formed in the uterine cavity. In addition, malignant and benign tumors can develop this condition. In addition to bleeding, in this case, severe pain in the abdominal area can also be noted. Heavy bleeding as a result leads to deterioration in physical activity, as well as to the formation of many complications in the body.
Postmenopause and complications
At this time of bleeding, women should immediately pay attention. During this period, the ovaries no longer work and do not perform their characteristic functions, which is why bleeding during postmenopause can only occur if hormone-containing drugs are used
All other cases will indicate that the woman has pathology in the genital organs and certain diseases.
Disturbances in uterine bleeding during postmenopause can occur if:
- polyps;
- vaginitis;
- disturbances in the hormonal system;
- formation of fibroids;
- difficulties of the endocrine system;
- hyperplastic disorders in the endometrium.
In addition, such a disorder may indicate the presence of tumor formations in the uterus or ovaries. Heavy discharge occurs after menstruation if the muscle fibers have atrophied, which has led to thinning of the mucous membranes and increased trauma.