Benefits of laparoscopy for uterine fibroids
The laparoscopy technique has become firmly established in everyday surgical practice, specialists know the necessary techniques, operating rooms are equipped with equipment, and patients know the advantages of the method and therefore strive to be operated on minimally invasively.
The cosmetic effect after surgery is very important for a woman, because no one wants to walk around with a noticeable scar, and after laparoscopy, barely noticeable scars will remain on the anterior wall of the abdomen. However, in addition to the purely aesthetic side, laparoscopy has many other, more serious, advantages that make it much more attractive than usual surgery.
laparoscopy
The advantages of laparoscopy include:
- Minor surgical trauma, respectively, and pain syndrome and adhesions will be minimal;
- Low blood loss and safety for nearby organs;
- Low incidence of complications during the intervention and rare tumor relapses subsequently;
- Short rehabilitation period;
- Possibility of preserving both the uterus and childbearing ability.
Laparoscopy also has disadvantages, although they are few. These include the impossibility of removing submucosal and intersitial nodes due to the difficulty of access and probable massive bleeding, as well as the not always feasible condition of having both equipment and a qualified surgeon.
Excision of uterine fibroids using the laparoscopic method has the following advantages:
- Low probability of injury and complete absence of severe consequences.
- Laparoscopy is a procedure after which there is no postoperative pain, and the rehabilitation period proceeds quickly, without unpleasant symptoms.
- The organs of the reproductive system in women are quickly regenerated, and their work is normalized. The risk of adhesions and bleeding is minimal.
- With the help of laparoscopy, it is possible to save the uterus. This is very important for those ladies who have not given birth.
- Short recovery period. Within a couple of hours the patient can get back on her feet, and 4-6 days after the operation she is discharged home.
- Laparoscopy is an effective way to remove large tumors. The risk of relapse and growth of a new tumor node is minimal.
- After the operation, there will be no scars on the surface of the peritoneal cavity that remain during traditional types of surgical treatment.
https://youtu.be/wwAfmUWbe9o
How is laparoscopy performed?
Laparoscopic surgery is performed under general anesthesia, which means the patient is sound asleep during the procedure. The duration of the operation is from forty minutes to three hours, it all depends on the case. When performing an operation, the day of the cycle does not matter, but the operation cannot be performed during menstruation, as this increases the percentage of blood loss.
To clearly see the operated area and surrounding pelvic organs, the doctor inserts a trocar and injects carbon dioxide into it. The abdominal wall rises, and the surgeon, having introduced another trocar, can freely examine the operation area through a microvideo camera. And determine where to start. Thus, the tumor, its diameter, location, shape of the reproductive organ and appendages are clearly visible. Are there any adhesions or other complications?
Typically, during laparoscopy, three to four punctures are made through which trocars are inserted to remove fibroids. The surgeon cuts through adhesions, if any, makes cuts in the tissue above the tumor, and pulls it out of the membrane. If necessary, coagulation of blood vessels is performed. It all depends on the specific case. Small and medium-sized fibroids are removed through the punctures that were made to insert the trocar. If the neoplasm is large or the uterus is removed, the doctor first excises the tissue using a morcelator. It is inserted into one of the punctures. The crushed pieces of tissue are removed through punctures, so no additional cuts are made. After the fibroids are removed and removed, the doctor will re-examine the operated area to make sure there is no internal bleeding. The instruments are then removed from the abdominal wall. Stitches are placed on the punctures.
Preparation and technique for performing the operation
Preparation for surgery includes undergoing a comprehensive examination, and if there are concomitant diseases, they should be brought to such a course as not to provoke complications, or, if possible, cured.
In some cases, before removing the tumor, hormone therapy is prescribed for several months to curb the growth of the tumor and reduce its size, and embolization of the arteries supplying the node is also possible, facilitating laparoscopy for large tumor sizes.
Before the intervention, the patient undergoes general and biochemical blood tests, urine, undergoes a blood clotting test, determination of group affiliation and Rh factor. Upon admission to the hospital, it will be necessary to present the result of fluorography and a cytological smear of the cervix.
Before the operation, the woman visits a gynecologist in the clinic, who examines her, palpates the nodes, determines their size and location, takes smears from the cervix and cervical canal for the presence of atypical cells, as well as from the genital tract to exclude inflammation and infection. Infections and inflammatory processes can become an obstacle to surgery. For accurate topical diagnosis of fibroids, ultrasound is indicated.
After completing all the procedures, the patient visits the therapist, who signs his permission to intervene. At this point, all medications that may cause bleeding or adversely affect the course of the operation are discontinued.
At the appointed time, the woman comes to the clinic, where she is consulted by a surgeon, once again making sure that the operation can be carried out according to the previously determined plan. On the eve of the intervention, a cleansing enema is carried out, the last meal and water is taken no later than six o’clock in the evening. Before going to bed, it is recommended to take a shower, change clothes and calm down, even if this means taking a sedative or sleeping pill.
Before the operation, the anesthesiologist talks with the woman, talks about the intended anesthesia and makes the necessary prescriptions. To prevent thromboembolic complications, elastic bandaging of the lower extremities is indicated.
Laparoscopy of uterine fibroids is performed under general anesthesia and lasts on average from 40 minutes to one and a half to two hours, depending on the number of tumor nodes and their location. The operation can be performed on any day of the cycle, except for menstruation due to increased bleeding during this period; the optimal period is considered to be the period between 15 and 25 days, that is, after ovulation and before menstruation.
For good visibility of the pelvic organs, the first trocar is inserted into the abdomen, through which carbon dioxide is pumped. The gas lifts the abdominal wall, and the surgeon examines the area of interest using a video camera inserted through another trocar along with a light source. During the examination, the doctor specifies the location of the nodes, their sizes, the configuration of the uterus and appendages, the presence of adhesions, etc. In total, to remove fibroids, you will need to insert 4 trocars through 4 punctures in the abdominal wall.
Using endoscopic instruments, the surgeon can dissect adhesions, cut the outer tissue of the uterus above the node, remove the formation from the capsule, coagulate bleeding vessels and apply sutures to the cut tissue. The sequence and technique for removing nodes varies in each case, since the location and number of nodes are always individual, and the surgeon acts based on the specific clinical situation.
If the myomatous nodes are small, then they can be removed through the punctures through which the instruments were inserted. If there is a large tumor or the entire uterus is removed by laparoscopy, it will be problematic to get the cut-off tissue out, so there is a need to grind it. The morcellator device helps to crush the removed formations by cutting them with knives of different sizes.
At the end of the operation, the surgeon once again examines the operating area, makes sure that there is no bleeding, removes the instruments from the abdomen and sutures the trocar punctures, covering the wounds with sterile napkins. Drainage of the pelvic cavity is usually not required.
If, after diagnosis, the doctor decides to remove the fibroid using laparoscopy, then first the patient needs to undergo a series of preparatory measures. The first stage will be taking tests and performing instrumental diagnostics. Then contraindications are identified and the doctor sets a date for the operation.
Myomectomy begins with the administration of anesthesia. It can be either general or epidural. Then the peritoneal wall is pierced in specific places and instruments are inserted there. Then carbon dioxide is supplied. The walls of the peritoneum are lifted, which allows you to create the necessary space for the procedure.
Now is the time to introduce the laparoscope. Thanks to him, it is possible to examine the uterus and organs, and also understand the areas for further puncture. Special instruments are used to remove the node or the entire uterus. The most important advantage of laparoscopy remains safety and painlessness.
With complete removal of the uterus, the pain is less pronounced, the duration of the intervention is reduced, the patient will be able to get back on her feet the next day, and the risk of developing adhesions is reduced.
Contraindications
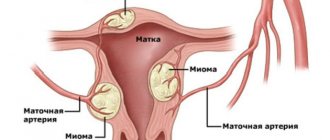
The third method of treating fibroids is uterine artery embolization (UAE).
This minimally invasive intervention is highly effective (up to 95%), does not require general anesthesia (performed under local anesthesia), and does not leave scars. A catheter is inserted through a puncture into the femoral artery. And the doctor, monitoring the process using x-rays, carries it into the uterine artery. Through this catheter, medications are injected into the vessels supplying the fibroid nodes, which stop the blood supply to the fibroids. After the operation, the patient must observe complete rest for a week and abstain from physical activity and sexual activity for another month. The disadvantages of UAE include its high cost (costs about 100 thousand rubles), the risk of formation of adhesions and inflammation. In addition, for a certain type of tumor (submucous fibroid), this intervention is not always effective.
If the fibroid does not grow and is asymptomatic, it should not be operated on. It is better to treat with medication and observe. With the onset of menopause, it can go away on its own, so after 40–45 years it is better to delay the development of the tumor with the help of medications, without resorting to surgery.
Surgical removal of the reproductive organ is highly not recommended in the following cases:
- worsened blood clotting process;
- the presence of all kinds of infectious diseases that are at the acute stage;
- presence of a serious form of diabetes mellitus;
- progression of hypertension;
- presence of unstable angina;
- the presence of cancer of the reproductive organs (ovaries, uterus) at the last stage of development.
Only in the most difficult situations, when a woman’s life is in serious danger, does a medical professional have the right to turn a blind eye to existing contraindications and perform an operation to remove the uterus.
Fibroids are characterized by slow growth and a low likelihood of malignant degeneration. They prefer to be localized at the body level, but there is a small percentage (up to 10%) of detection in the cervix.
If the fibroid is located on the surface of the uterine body and its size is insignificant (up to 2–3 cm), then it is most often not accompanied by obvious clinical manifestations. But with an increase, compression of adjacent organs (bladder, rectum), lymph nodes, blood vessels, and nerves is noted. The result is discomfort, pressure, pain in the lower abdomen, pelvic dysfunction, extramenstrual bleeding, and irregular cycles.
The appearance of such symptoms is an indicator of pathological changes that require professional consultation. They cannot be ignored; you should immediately contact a gynecologist. If the myomatous node has reached an impressive size and there are objective complaints, the doctor will prescribe surgery.
Removal of uterine fibroids (myomectomy) is indicated for nulliparous women of reproductive age. In some cases, when the cause of difficulties in conceiving a child is deformation of the uterine cavity due to submucosal or large interstitial nodes, removal of the tumor is considered a treatment for infertility. Removal of fibroids is carried out after conservative therapy does not reduce the size of the tumor and does not affect the intensity of its growth.
Indications for surgical intervention are also:
- Large mima sizes (12 weeks pregnancy or more);
- The presence of concomitant pathological processes, such as ovarian cancer or endometriosis;
- Necrosis of the myomatous node caused by torsion of the leg or other factors leading to malnutrition of the tumor;
- Impaired functionality of organs located close to the uterus, for example, disruption of the intestines or bladder;
- Severe pain syndrome;
- Risk of malignancy of the tumor;
- Heavy bleeding that cannot be corrected, as well as regular uterine bleeding leading to anemia;
- Intensive growth of tumor and myoma nodes.
The decision to remove fibroids is made if the tumor interferes with conception or bearing a child. An indication for radical removal of fibroids along with the reproductive organ may be the large size of the tumor, the specificity of its location or development.
You may be interested in: Diagnosis of uterine fibroids and size for tumor removal surgery
Myomas vary in size:
- small, when the tumor is no more than 2 cm (5-week pregnancy);
- medium, when the tumor size is 2-6 cm (11 - week pregnancy);
- large when the size of the fibroid is more than 6 cm (12 - 15 week pregnancy);
- gigantic, when the uterus enlarges to the size of a 16-week pregnancy.
Surgical treatment is used for all tumor sizes if there are indications for this (necrotic processes in the tumor, impediment to conception). However, in most cases, tumors that are 12 weeks pregnant or more must be removed.
Myectomy is not allowed in the presence of large or multiple nodes, when the tumor is located in the cervical region, or when active growth of fibroids is registered in a patient who is in menopause. Limitations for myectomy are the patient’s severe somatic condition, the presence of current infectious and septic ailments, and problems with general anesthesia. In such cases, alternative treatment methods without general anesthesia are chosen and combined with conservative therapy.
It is also not allowed to remove fibroids if:
- profuse and uncorrectable uterine bleeding (menometragia), leading to severe anemia and a risk to the patient’s life;
- large-scale necrosis of the neoplasm, especially if it is accompanied by a secondary bacterial infection, septic endometritis, thrombosis, or when there is a possibility of developing peritonitis;
- severe disruption of the functioning of organs located near the uterus (bladder, ureters, intestines), caused by their displacement and compression by a large myomatous node or an enlarged reproductive organ.
https://youtu.be/BsQB5L9zqBA
If the above conditions are present, a hysterectomy is performed.
What not to do after abdominal surgery to remove fibroids
The presented technique is not applicable when:
- there are various pathologies of the lungs, blood vessels and heart;
- the woman recently suffered a heart attack or stroke;
- there is a serious pathology of blood clotting;
- during the diagnosis, impaired functioning of the liver and kidneys was discovered;
- oncology of various pelvic organs.
Patients are interested in what can and cannot be done after surgery to remove uterine fibroids. Rehabilitation usually consists of the procedures and recommendations described above. The main thing is to listen to your doctor and take care of your health. The early period is considered the most important: a number of restrictions are caused by the fact that the wound has not yet healed completely and there is a risk that the stitches will come apart.
Consequences and complications of the postoperative period
Any surgical intervention is stressful for the body. Its consequences depend on the age, weight, general health of the patient, methods and quality of treatment and other factors, but there are a number of the most common complications depending on the rehabilitation period.
Early
- Complications after anesthesia: a sharp rise or fall in temperature, constant temperature measurements, vomiting, tongue retraction, arrhythmia.
- Inflammatory processes: infection or suture dehiscence, swelling, redness, purulent discharge, peritonitis as a result of inflammation.
- Circulatory disorders: thrombosis, internal and external bleeding, hematomas, hematomas, etc.
- Painful sensations: any damage to tissue integrity is accompanied by a painful symptom. Rehabilitation after surgery to remove uterine fibroids allows you to minimize pain. Discomfort often occurs when urinating. This is considered normal, but still requires treatment.
- Disorders of urination and stool excretion, intestinal obstruction, etc. The impact of surgery affects metabolism and leads to various adverse consequences.
- Pneumonia, usually caused by prolonged bed rest.
Typically, these consequences and complications are characteristic of all surgical interventions, and not just for this particular disease.
Late
- Intestinal disorders.
- Hernias.
- Depression. The state of depression is caused by emotional exhaustion associated with an unpleasant diagnosis and subsequent treatment. Mood is affected by changes in lifestyle, thoughts about infertility, the presence of scars (they remain if abdominal surgery was performed, with laparoscopic surgery there are practically no traces), etc.
During the late period, the main healing processes are completed. Significant complications are rare.
Remote
- Recurrence of the disease: This is usually due to the fact that the doctor did not eliminate the cause of the tumor or did not take into account other factors, such as hormone levels.
- Menopause: Hormonal changes cause various reactions in the body, including the early onset of menopause.
- Osteoporosis: The disease and subsequent surgery negatively affect the body's calcium levels. Its deficiency leads to increased bone fragility.
- Diseases of the genitourinary organs: this may be infertility (many operations, for example, laparoscopy of uterine fibroids, allow you to preserve reproductive function, but a number of surgical interventions lead to infertility immediately or after some time), prolapse
- vagina, urinary incontinence, as well as diseases caused by non-compliance with personal hygiene rules, doctor’s recommendations and infection.
- Transformation of benign cells into malignant ones: special attention should be paid to the condition of the mammary glands, since they are most at risk.
- Depression and other psychological problems.
Complications can be determined not only at a doctor’s appointment. Increased body temperature, uncharacteristic discharge, burning sensation in the genital area and other changes are a reason to visit a specialist.
Recovery after surgery to remove uterine fibroids allows you to minimize the negative consequences.
Any surgical intervention can lead to complications. With laparoscopy their probability is 1-2%. The consequences of the technique include:
- mechanical trauma to internal organs with surgical instruments or damage due to the introduction of carbon dioxide into the peritoneal cavity;
- damage to a blood vessel when performing a puncture;
- development of internal bleeding;
- penetration of carbon dioxide under the skin;
- injury to the intestines, urinary tract and other internal organs.
How to speed up the recovery process after removal of uterine fibroids
Removal of fibroids using laparoscopy is performed in a sterile operating room in a hospital or private clinic. In this case, the medical institution for this operation must be equipped with resuscitation equipment.
The duration of the operation varies from 30 minutes to 3 hours, depending on the size and number of myomatous nodes.
The operation occurs in several successive stages:
- General anesthesia (endotracheal with the use of artificial ventilation).
- When doctors are sure that the anesthesia has worked and the patient is in a stable condition, they proceed directly to the operation. In the lower part of the peritoneum, 3 small punctures with a diameter of up to 15 mm are made, through which special surgical equipment will be inserted, allowing surgeons to see the internal organ and neoplasms of the uterus on the monitor screen, and perform manipulations without significantly compromising the integrity of the abdominal area.
- Injection of carbon dioxide using an insufflator for better visual control of the progress of the operation.
- Insertion of the laparoscopic instrument and performance of the necessary surgical procedures. If the formation has a leg, it is simply cut off. If the node is located inside the muscular wall of the uterus, enucleation will be done.
- Coagulation of bleeding areas.
- Suturing the damaged myometrium by applying an endoscopic suture.
- Extraction of formations from the abdominal area through punctures. If the fibroid nodes are large, the morcellator first crushes the tissue and then sucks it in.
- Inspection of the abdominal area and sanitation.
- Removing equipment and ports for its insertion.
- Applying sutures to puncture sites.
- Removing a woman from a state of anesthesia.
When a woman undergoes fibroid removal, recovery from even minimally invasive surgery can last up to 3 months. A number of procedures allow you to speed up this process, make it more comfortable and quickly return to your normal lifestyle; it is also important to follow the basic recommendations of a specialist. As a rule, the doctor voices them to each patient personally, but there are a number of universal tips:
- Wear a postoperative bandage: it provides the condition necessary to maintain the desired position of the internal organs, which helps prevent vaginal prolapse, etc.
- Observe contraception: pregnancy is not allowed for a year, but this period may last longer, depending on individual health indicators. It is optimal if contraceptive methods are selected by a doctor.
- Refuse thermal procedures: visiting a solarium, bathhouse, beach, seaside holidays, etc. is prohibited.
- Eat right: foods should be easy to digest. You should not eat fixing foods; you should give preference to soups, cereals, etc. After discharge from the hospital, you can add fruits, raw or baked vegetables, fish, and lean meat to your diet. It is recommended to completely avoid fatty, fried, viscous foods, carbohydrates, alcoholic beverages and coffee.
- Maintain a daily routine: it is worth including full sleep, daily walks, moderate physical activity (morning exercises, exercise therapy).
- Get rid of bad habits: smoking, stress, lack of sleep, etc. are prohibited.
And, of course, do not forget about regular examination by a doctor, even if there are no signs of complications.
Recovery after removal of uterine fibroids: methods
- Drug therapy. Removal of fibroids does not leave its mark on the body. Depending on the patient’s condition, the doctor selects medications. Usually these are drugs that relieve pain, strengthen the immune system, help replenish blood loss, as well as drugs to prevent blood clots. To restore hormonal levels and as a means of preventing relapse, the doctor individually selects hormonal drugs.
- Physiotherapy. A number of procedures, for example, SMT, lymphatic drainage massage, ultrasound and magnetic therapy, improve blood circulation and accelerate tissue regeneration processes, help avoid problems associated with changes in hormonal levels, early menopause, and are a means of preventing adhesions, swelling of the lower extremities, urinary disorders, etc.
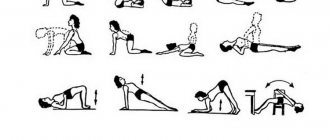
- Physiotherapy. Moderate physical activity under the supervision of a specialist can strengthen the immune system and restore muscle tone. The optimal sports are gymnastics and regular walks, but any water sports will have to be abandoned. Kegel exercises help relieve urinary incontinence. Breathing exercises help avoid adhesions and speed up recovery.
- Psychotherapy. Women often experience depression caused by infertility after surgery to remove uterine fibroids. Rehabilitation in this case is impossible without psychotherapy. The doctor helps restore your emotional state and overcome depression.
Features of the operation
Laparoscopy is a minimally invasive surgical procedure. It is carried out not through incisions, but through small punctures into which a laparoscope and other instruments are inserted. The surgeon monitors the progress of the operation through a mini-video camera, which is also inserted through a puncture. This technique for eliminating fibroids is considered one of the most minimally traumatic. With its help, doctors remove fibroids without touching the uterus or affecting neighboring organs. Patients recover quickly and can become pregnant within six months.
How long does it take to recover after removal of uterine fibroids?
Rehabilitation after removal of uterine fibroids is associated with a number of limitations. For example, at first, bed rest is indicated: you cannot walk or stand for a long time. Thermal procedures and sunbathing are prohibited. You should also not be in the cold: hypothermia has a negative effect on the body. It is contraindicated to lift weights (more than 2 kg at first and more than 10 kg after discharge), overexertion (this includes daily household chores and physical exercise).
You should abstain from sexual activity for about two months after surgery; pregnancy is not allowed for about a year. It is important to eliminate stress and emotional overload. For 1-2 months you should not use tampons, only pads; until the stitches are completely healed, you should not go to the pool or swim in bodies of water.
It is difficult to determine in advance how long rehabilitation will last, since this parameter depends on many conditions: from the patient’s age to the treatment method. For example, the early postoperative period after hysterectomy is 10-14 days, and recovery after laparoscopy for uterine fibroids usually does not exceed 5 days. The late and late periods also differ from each other in duration.
In addition to the type of intervention, the period determines the age, general health of the woman and the quality of the selected treatment. As a rule, complete recovery in the absence of serious complications takes about a year.
Postoperative period after hysterectomy
To speed up this process, the patient is required to follow the following recommendations:
- Develop a proper, balanced diet to prevent constipation. Otherwise, the sutures on the uterus may heal more slowly.
- To avoid stagnant changes in the pelvic area, moderate systematic physical activity should be added - walks in the fresh air, Pilates, yoga, swimming. It is advisable to exclude active sports until the permission of the attending physician.
- Wear a support bandage after an abdominal hysterectomy.
- Strictly take all medications prescribed by your doctor.
- Avoid visiting bathhouses and saunas for up to 2 months after surgery. Sunbathing is not recommended at this time.
- Do not skip periodic medical examinations in combination with ultrasound of the pelvic organs.