When the stomach hurts during menstruation, a woman or young girl sometimes becomes completely unable to work. Every 10 women suffer from unbearable pain during menstruation, often leading to fainting and even cramps. It is believed that menstruation is a natural process in a woman’s body, which should not be accompanied by very severe cramping pain in the lower abdomen, much less vomiting, nausea, headache, diarrhea or constipation. Gynecologists strongly recommend that in case of intense painful periods, you first find out the cause of its occurrence, since this may not just be a feature of your body, but be symptoms of a serious disease or dysfunction of the nervous, reproductive, endocrine system, be a symptom of connective tissue dysplasia or an anomaly in the development of the genital organs, etc. In this article we will talk about how to reduce pain during menstruation for a girl or woman, what should be done to relieve pain during menstruation and determine the true cause of such an abnormal state of the body.
How to relieve pain during menstruation for young girls?
In gynecology, it is customary to divide painful periods into primary, when a girl has never had painless periods from the very beginning of menstruation, and secondary, when severe pain during menstruation occurs in women after 30 years of age against the background of various infectious and inflammatory diseases of the female genital organs, hormonal imbalances, after surgical interventions, etc.
According to many women and doctors, primary algomenorrhea (pain during menstruation) can go away on its own after a woman gives birth to a child, then the uterus will contract less painfully during menstruation. But, if this does not happen, moreover, if a young woman cannot become pregnant and she experiences a whole range of symptoms both before menstruation - premenstrual syndrome, and during menstruation, it is imperative to undergo a comprehensive examination not only from a gynecologist, but also from such specialists such as gastroenterologist, phthisiatrician-gynecologist, neurologist, endocrinologist, osteopath, psychotherapist.
Since the main causes of painful periods in girls can be general systemic diseases, such as connective tissue dysplasia, expressed in the development of curvature of the spine, dysfunction of the gastrointestinal tract, frequent dislocations, varicose veins of the legs and pelvic organs. Also, the cause of primary algomenorrhea can be genital tuberculosis, leading to abnormal development of the genital organs, underdevelopment of the mammary glands, uterus and uterine appendages, which is the cause of persistent infertility. Various diseases of the nervous system, mental disorders, emotional instability in girls can be a consequence of the same genital tuberculosis or be an independent disorder that has hereditary or congenital roots.
Considering the above, you should first exclude these pathologies, and then, based on the establishment or exclusion of these diagnoses, decide on methods for relieving pain during menstruation.
Causes of pain during menstruation
- Heredity (there is no need to run to thank mommy, she herself suffered a lot from painful periods at one time; rather, she can advise the methods she has tried to get rid of pain during her period).
- Weak pelvic muscles and the entire ligamentous apparatus (with a lack of load, the muscles weaken and then become more sensitive to abdominal cramps).
- Lack of essential microelements in a woman’s diet, menstruation becomes especially noticeably painful with low intake or poor absorption of calcium and magnesium.
- A history of gynecological diseases, such as uterine fibroids, fibroids, developmental defects, for example, uterine flexion, endometriosis, polycystic disease, single ovarian cysts, polyps, adhesions in the peritoneum (mostly postoperative).
- Hormonal disorders.
- Sometimes the intrauterine device reminds itself of itself in such an inadequate way.
Typically, pain during menstruation is stronger in sensitive individuals with a mobile nervous system, accompanying VSD (vegetative-vascular dystonia), primary disorders in the production of thyroid hormones.
Risk factors include curvature of the spine, especially in the lumbar region, pinched nerve endings at the pelvic level, sciatica, neuralgia, severe infectious diseases, the presence of varicose veins of the small pelvis, disturbances in the conduction of nerve impulses after operations, and micro-stroke.
Non-drug ways to relieve period pain
To reduce pain during menstruation in girls with primary algomenorrhea, it may be sufficient to use non-drug methods to combat painful menstruation, such as:
- Stress management
It’s very easy to say, but it’s quite difficult to learn to relax, calm down, not get upset, and cope with stress. In our difficult times, the abundance of negative information, the anger of people around us, financial problems, and failures in personal relationships expose the modern woman to constant emotional turmoil. Thought is material, if you know how to control yourself and tune in to a certain positive wave, you can cope with any problem, you just need to constantly work on yourself, control your thoughts, not pay attention to little things, and set priorities correctly. Yoga and meditation help with this.
- Smoking and alcohol
It may sound trivial, but giving up these habits can reduce pain during menstruation. The female body is not able to cope with the nicotine and alcohol attack, like the male body. Smoking has a very detrimental effect on the entire female body, causing early aging, painful periods, approaching menopause, provoking the occurrence of various diseases and increasing the risk of cancer. In our time of oncological tension, when cancer affects even young women of childbearing age, if you add daily nicotine poisoning and alcohol intoxication, this overloads the immune system, which gradually stops destroying cancer cells and allows them to grow.
- Bodyflex and yoga classes
If you have pain during menstruation, you should limit physical activity and sexual intercourse in the second phase of the menstrual cycle, however, in the first phase it is very useful to do yoga or Bodyflex. Why? These two types of physical exercises have a positive effect on the female genital organs, since both yoga and Bodyflex provide a powerful massage of the internal organs, including the pelvic organs. These exercises promote the resorption of adhesions, stimulate ovulation, and generally have a beneficial effect on the respiratory, musculoskeletal, and cardiovascular systems of the body.
- Diet
Proper nutrition has a positive effect not only on relieving pain during menstruation, but also on overall health. A few days before menstruation, you should eat as many fruits and vegetables as possible, do not overeat, especially limit the consumption of fatty and sweet foods, flour and refined foods, exclude fast food, sausages, meat and dairy products. You should drink more liquid, up to 2-2.5 liters per day, it is better if it is not tea and coffee, but mineral water, freshly squeezed vegetable and fruit juices - carrot, beetroot, apple, orange, pineapple, and hot herbal teas are also useful with chamomile, mint.
- Avoid hypothermia
Any hypothermia, thin tights in the cold, poor-quality autumn and winter shoes that cause wet feet in the cold and rainy season provoke inflammatory processes in the pelvis, causing salpingitis, adnexitis (see inflammation of the appendages - symptoms and treatment), disrupting the menstrual cycle and leading to painful menstruation and even infertility.
- If severe pain occurs, you can press your legs to your chest and place a heating pad on your stomach.
How to relieve pain during menstruation? Apply a bottle of warm water or a heating pad to your stomach and lie with your legs pressed to your chest, this helps increase blood flow and reduces painful cramps; you should hold the heating pad for no more than 15-20 minutes, otherwise it may increase bleeding.
- Fresh air
Sometimes being in a stuffy room aggravates the condition, increasing pain during menstruation; if you go out into the fresh air, take a walk in the park, or simply ventilate the room well, this can alleviate the condition, reduce headaches, and pain in the lower abdomen.
- It is very important to preserve the first pregnancy during primary algomenorrhea
The first medical abortion (consequences) in a woman with painful menstruation can provoke the development of further infertility and aggravate pain during menstruation. After pregnancy, in most cases, pain during menstruation decreases.
- Physiotherapy, massage, acupuncture
A fairly effective method of physiotherapeutic treatment is electrophoresis on the solar plexus area with novocaine; the doctor can prescribe 6-8 sessions with the expectation that the treatment will be completed by the beginning of menstruation. It is also possible to carry out various options for reflexology, acupuncture - general, acupressure, cupping therapy, bloodletting with the help of hirudotherapy also have a beneficial effect on the entire body and on the genitals, including the genitals, however, it is better to trust such treatment methods to professionals. If it is not possible to carry out a therapeutic massage before menstruation, during menstruation you can independently do a passive massage using the Kuznetsov applicator, apply it to the lower back and lie on your back, lie there for 10-15 minutes.
- Keep a record of the methods performed and a menstruation calendar
Girls and women with painful periods should keep a calendar of the nature and symptoms of menstruation. It should indicate the duration of menstruation, the duration of the menstrual cycle, the intensity of bleeding, scanty menstruation or heavy menstruation (uterine bleeding), as well as the nature, location of pain, and other symptoms accompanying menstruation. Women trying to get pregnant can also take into account their basal temperature in the calendar, which helps in determining ovulation. In your menstrual diary, it is worth recording the options for therapy carried out to relieve pain; this will help in the future to determine the effectiveness of a particular remedy or method of pain relief, and will also help you remember and describe your symptoms when visiting a gynecologist.
- Maintaining sleep, rest and work schedules
Adequate 8-10 hour sleep, adherence to a daily routine and diet, the habit of going to bed at exactly the same time, avoiding overwork are simple tips, but very effective. Following a routine in everything calms the nervous system, makes life measured and calm, and helps cope with stress.
How to relieve period pain
Pain and discomfort in the lower abdomen is a common condition for many women during the menstrual cycle. Scientifically, this phenomenon is referred to as “algomenorrhea” (dysmenorrhea). Statistics show that about 70-80% of women suffer from pain during menstruation. To eliminate all kinds of unpleasant symptoms, it is first necessary to understand the etymology of pain. Having found out the causes of pain, you can understand: is this a common phenomenon inherent in natural processes in a woman’s body, or is it a reason to immediately consult a doctor and how to reduce pain during menstruation.
Causes of painful periods
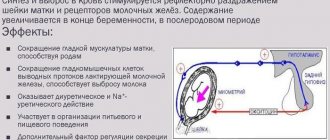
During menstruation, the uterine tissue produces prostaglandin, which provokes its contraction. The severity of pain depends on the level of this hormone. Doctors distinguish two groups of causes of menstrual pain.
Primary dysmenorrhea
Inherent in women under 35 years of age and adolescents. With primary algomenorrhea, hormonal changes occur associated with an increase in the amount of prostaglandin. In simple words, the causes of cramping pain and vascular spasm are hormonal disorders and a state of anxiety and stress. It is observed that teenage girls experience especially severe pain.
Symptoms of primary dysmenorrhea:
Headache.
Stool disorder.
Pain of the same intensity throughout the entire cycle.
In addition to nagging pain in the lower abdomen and lumbar area, reactions such as nausea, vomiting, and fainting may occur. In the absence of serious problems, discomfort disappears with age, as well as after childbirth.
Secondary dysmenorrhea
Women over 35 years of age are susceptible. Secondary algomenorrhea is a sign of inflammatory diseases and pathologies of the pelvic organs. It may be associated with the development of fibromatous nodes, pelvic neuritis, endometriosis, fibroids, polyps in the uterus, as well as the consequences of gynecological and abdominal operations (abdominal adhesions). An intrauterine device can also cause severe pain during menstruation. Bleeding and pain in this case are more intense. A visit to a gynecologist is the first thing to do in such situations, who will already tell you how to get rid of abdominal pain during menstruation.
Causes of painful periods not related to reproductive system problems:
Imbalance of the female genital organs, excessive activity of the thyroid gland.
Intrauterine device.
High threshold of sensitivity to changes in the body. Instability of the nervous system.
Pain due to abortion or childbirth.
Incorrect position of the uterus.
Hereditary predisposition.
Deficiency of magnesium, calcium.
Unbalanced diet.
Women suffering from secondary dysmenorrhea have low libido, they feel dissatisfaction with their sex life, a tendency to depression, a depressed state, and sometimes even psychological deviations can be observed.
At the same time, cure for diseases associated with algomenorrhea contributes to the almost complete cessation of pain during critical days. But with younger, healthier looking women the situation is more complicated.
In this case, it is necessary to undergo all recommended examinations. If gynecological problems are not identified, and the pain does not stop, then this is already a reason for a more serious approach to clarifying their etymology.
If discomfort increases, heavy bleeding, nausea, or migraines appear, you should immediately consult a specialist, take the recommended tests, undergo an ultrasound examination, which will help you figure out how to relieve pain during painful periods.
Methods for eliminating pain
There are many ways to get rid of pain during menstruation that give a noticeable effect. They can also be used at home (subject to existing contraindications). Let's take a closer look at each of the categories that provide the answer to how to reduce or alleviate pain during menstruation without pills and at home. Medications
This method is suitable for those who are adherents of traditional medical technologies in treatment, resolving the issue of how to relieve pain during menstruation if the lower abdomen hurts.
Over-the-counter medications. In this category are NSAIDs, that is, non-steroidal anti-inflammatory drugs, for example ibuprofen. Antispasmodics. These include “No-shpa”, “Ketonal”, “Spazmalgon”, “Analgin”. Sedative. Pain caused by stress or overexcitation of the nervous system can be treated with a common sedative (for example, valerian).
Before using medications to relieve abdominal pain, you should consult a doctor or independently study all its aspects according to the instructions. Another category of drug treatment is oral contraceptives (birth control pills). In this case, medications are taken strictly as prescribed by a specialist. Contraceptives contain hormones that restore hormonal levels in a woman’s body and thereby relieve menstrual pain. Birth control pills are used for daily use. They are affordable and sold in almost all pharmacies. Contraceptive methods for eliminating pain in the lower abdomen also include contraceptive patches, a contraceptive vaginal ring, hormonal injections, and an intrauterine device. Before using these remedies to relieve pain, you should consult your doctor.
An option for those who are interested in home treatment methods. Alternative ways to relieve menstrual pain without pills include:
Medications to reduce pain during menstruation
- Sedatives
If menstruation in girls is accompanied by significant neuropsychic signs, such as changes in the perception of smells, taste disturbances, unmotivated weakness, hysteria, increased irritability, depressed mood, anorexia, then sedatives should be used - tincture or tablets of valerian, Relanium, Trioxazin and other sedatives medications prescribed by a doctor.
- Analgesics, antispasmodics, NSAIDs
If all of the listed non-drug remedies do not provide relief, antispasmodics such as Spazgan, No-shpa and non-steroidal anti-inflammatory drugs - Ketanov, Ibuprofen, Butadione, Nise - are indicated to reduce pain during menstruation. The safest among these remedies is No-shpa or the domestic analogue of Drotaverine hydrochloride, Papaverine, they are approved for use even during pregnancy, you can use 2 tablets at once up to 3 times a day. NSAIDs, of course, have a more pronounced analgesic effect, however, they have a number of side effects, negatively affecting all systems and organs, especially the gastrointestinal tract and central nervous system.
- Hormonal oral contraceptives
On the recommendation of a gynecologist, in case of primary algomenorrhea, in order to get rid of pain during menstruation, hormonal contraceptives are prescribed, such as Ovidon, Antiovin, Triziston, Diane-35, Yarina (see list of all oral contraceptives), as well as the use of drugs made from natural progestins, for example, Duphaston.
- Vitamins and minerals
It is advisable to get all vitamins from food, fruits and vegetables, but if you take a biochemical blood test and determine the deficiency of specific vitamins or minerals, you can make up for the deficiency with the help of vitamin complexes or individual vitamins in injections. Most often, women experience calcium deficiency - you can take Calcium D3, B vitamins, vitamin E, magnesium B6.
Treatment of secondary algomenorrhea
When a woman who already has children begins to experience pain during menstruation, accompanied by additional sets of symptoms - nausea, headache, depression, fainting, tachycardia, joint pain, itching of the skin - this is due to the development of various diseases of the endocrine, nervous, vegetative-vascular system , or caused by various pathologies and diseases of the female genital organs.
Most often, secondary algomenorrhea appears with endometriosis, polyps in the uterus, adhesions in infectious and inflammatory diseases of the genital organs - salpingitis, oophoritis, salpingo-oophoritis, as well as with uterine cancer, ovarian cancer, varicose veins in the abdominal cavity and lower extremities, with pelvic neuritis, with cicatricial narrowing of the cervix from frequent medical abortions, intrauterine interventions, diagnostic curettages and other surgical operations.
Therefore, in order to relieve pain during menstruation with secondary algomenorrhea, treatment should be aimed at eliminating the cause, treating the disease that caused such a disorder. Sometimes incorrectly installed intrauterine contraceptives contribute to the development of pain during menstruation, in which case they should be removed. In case of adhesions, endometriosis or tumor lesions of the genital organs, appropriate therapy or surgical operations are recommended, after which a course of rehabilitation, physiotherapeutic procedures and sanatorium treatment is prescribed.
How to get rid of pain during menstruation? With secondary algomenorrhea, as with primary algomenorrhea, you can try to relieve pain during menstruation using non-drug methods. If there is no effect from them, medicinal methods are indicated, symptomatic therapy based on reducing pain during menstruation through antispasmodics and NSAIDs, sedatives to reduce psycho-emotional symptoms.
Causes of severe pain during menstruation
Pain during menstruation most often occurs in nulliparous women due to the anatomical features of the location of the uterus. If the pain syndrome is accompanied by dizziness, diarrhea, vomiting and leads to disability, they speak of algomenorrhea. Pathological symptoms indicate disturbances in various body systems.
Attention! Identification and treatment of the underlying disease that leads to pain during menstruation can reduce its intensity.
Pain during menstruation is a disorder of menstrual function. According to statistics, about 10% of women experience intense cramping pain during menstruation, which can be reduced by taking painkillers.
Pain syndrome can occur 12 hours before the next menstruation and last for several days. Sometimes the pain moves to the area of the bladder, lower back, and rectum. The constant expectation of discomfort leads to psycho-emotional disorders, insomnia, depression and anxiety.
If algomenorrhea is unexpressed, the pain does not require relief with medications. Gynecologists emphasize that the initial degree of algomenorrhea becomes more severe over time. That is why, if there is pain during menstrual periods, it is necessary to conduct an appropriate examination.
Attention! After childbirth, minor pain during menstruation often goes away on its own.
If the pain syndrome is of moderate severity, the following accompanying symptoms are also observed:
- nausea;
- frequent urination;
- chills;
- general weakness.
A woman's performance may decrease. Pain can be reduced through preliminary examination and medication correction.
If algomenorrhea is severe, fainting, fever, and vomiting are noted. The woman loses her ability to work. Usually the pathology is associated with an inflammatory process or congenital anomalies of the genital organs.
Functional dysmenorrhea
Primary algomenorrhea (dysmenorrhea) occurs after the onset of the first menstruation for 3 years. It has been established that the pathology is characteristic of emotionally unstable representatives with an asthenic physique. Often the pain is accompanied by PMS.
Primary dysmenorrhea includes the following types:
- Adrenergic. The failure of the hormonal system is caused by an increase in the production of dopamine, norepinephrine, and adrenaline. Symptoms include intense headaches, constipation, fever, insomnia, pale skin, and rapid heartbeat.
- Parasympathetic. An increase in the concentration of serotonin is noted in the cerebrospinal fluid. This causes a decrease in body temperature, heart rate, diarrhea, edema, and weight gain.
Primary algomenorrhea is a consequence of the following pathologies:
- connective tissue dysplasia (concomitant disorders of the gastrointestinal tract, scoliosis, flat feet, excessive joint flexibility);
- neurological disorders (decreased pain threshold, psychosis, emotional instability, changes in pain perception);
- underdevelopment, uterine kinks and malformations.
With abnormalities of the uterine body, the outflow of menstrual flow is difficult. Contractile activity increases, causing pain.
Acquired dysmenorrhea
Secondary algomenorrhea occurs in women who have given birth or the fairer sex after 30 years. This disorder occurs in approximately every 3 women and often occurs in moderate or severe form. Usually the pain syndrome is combined with heavy bleeding.
Depending on the predominance of characteristic features, several main groups are distinguished:
- bloating, hiccups, nausea or vomiting (vegetative symptoms);
- numbness of the arms or legs, rapid heartbeat, dizziness, fainting (vegetative-vascular manifestations);
- increased irritability, depression, impaired perception of smell or taste (psycho-emotional disorders);
- skin itching, joint pain, weakness (endocrine and metabolic disorders).
Important! The occurrence of symptoms depends on the patient's medical history.
Often, women with acquired algomenorrhea experience pain during sexual intercourse, which may be due to the following pathologies:
- inflammation;
- adhesive process;
- benign or malignant tumors;
- varicose veins;
- pelvic neuritis;
- endometriosis.
Experts name the following factors that provoke pain during menstruation:
- use of an IUD;
- frequent intrauterine manipulations, abortions leading to scar tissue deformation;
- postpartum complications;
- overwork, stress.
Important! To reduce severe discomfort during menstruation, therapy comes down not so much to pain relief, but to finding and eliminating the causes of the pathological condition.
Folk remedies - how to get rid of pain during menstruation
Folk remedies for reducing pain during menstruation are based on the use of various herbal mixtures. However, it should be remembered that any medicinal plant or herbal collection is the same medicine as tablets, with possible contraindications and allergic reactions. If a woman has a tendency to allergic manifestations, then she should use herbal teas very carefully, checking the body’s reaction to each remedy. It is recommended to take herbal infusions warm and drink slowly.
- Elecampane root - 1 teaspoon, pour a glass of boiling water, leave for 1 hour, take 1 tablespoon 3 times a day.
- Horsetail - to prepare the infusion you need 1 tbsp. pour 300 ml of boiling water into a spoon, leave for one hour, take 50 mg every hour, increase the dosing interval as the pain subsides.
- Collection: bloodroot, centaury, horsetail, knotweed, in a ratio of 5:3:1:5, pour one tablespoon of the mixture into a glass of boiling water, leave for 1 hour, take 1 sip during the entire first day of menstruation.
- Celery root - 2 tbsp. spoons should be filled with a glass of clean cold water, leave for 2 hours, strain, take a third of a glass 3 times a day.
- Wild strawberry leaves - 1 tbsp. spoon is filled with 1 glass of cold water, infused for 6-8 hours, you should drink half a glass a day.
- Collection: valerian root, peppermint leaves, chamomile flowers in a ratio of 1:1:2, pour 1 tbsp of boiling water. spoon of the mixture, leave for half an hour, take 3 times a day, 2 tbsp. spoons.
- Raspberry leaves - 3 teaspoons of leaves, pour 1 glass of boiling water, leave for 15 minutes, take in small sips throughout the day.
Author:
Selezneva Valentina Anatolyevna physician-therapist
I have painful periods. What to do?
6
If nothing helps, what will the doctor do?
If your doctor decides that it is not a medical condition, he or she may advise you to take NSAIDs differently (for example, more often) or prescribe prescription painkillers.
Another standard remedy is hormonal contraceptives. They suppress ovulation and the menstrual cycle and keep the endometrium in an inactive state, which prevents it from producing too many prostaglandins. These can be any hormonal contraceptives: those that contain progestin and estrogen (combined), and those that contain progestin alone. In other words, pills, patches, vaginal rings, implants, intrauterine devices, and injections are suitable.
True, combined contraceptives in this regard have been better studied, and in case of painful periods, doctors usually give preference to them. By the way, hormonal contraceptives cannot be used without a doctor’s prescription: they have quite a few contraindications. If you want to use these remedies without the required breaks and thereby stop bleeding for several months, in this case you also need to consult a doctor.
If none of this helps within three months, the doctor should think about some kind of disease.