What is cervicometry
Cervicometry is a method of ultrasound examination of the cervix of a pregnant woman. Using it you can determine:
- length of the uterine cervix;
- condition of the tissues and mucous membrane of the internal canal;
- condition of the pharynx, internal and external.
The procedure uses a special vaginal sensor with ultrasound radiation. This allows you to more accurately examine the cervix and determine the indicators.
The procedure does not cause discomfort and is practically safe. The ultrasound wave that comes from the transducer is reflected from the tissue of the cervix and produces an image on the screen.
If pathologies or diseases were discovered during the study, the specialist will give recommendations to ensure that the pregnancy proceeds normally.
Indications for regular cervicometry
If the pregnant woman has a history of previous premature termination of pregnancy or has undergone surgery on the walls of the cervix, it is imperative to inform the specialist who performs the ultrasound about this. In such cases, as well as in multiple pregnancies, regular cervicometry is prescribed every 2 weeks starting from 16 and for at least two months. This procedure is also very important for those who are carrying a fetus for the first time, since the pregnant woman’s medical history is incomplete and there are no indicators from previous pregnancies to make any predictions. Therefore, during the first pregnancy, it is very important to undergo cervicometry in time to make sure that the length of the cervix is satisfactory and there is no dilatation. And also check again all the indicators of your internal genital organs and the condition of the developing fetus.
Why is the length of the cervix measured during pregnancy?
A pregnant woman who receives a referral for this diagnostic method asks the question, “Why was cervicometry prescribed?”
The cervix is a cylindrical muscular organ that opens the entrance to the uterine cavity. The inner space of the cervix is called the cervical canal.
The normal length of the cervical canal during pregnancy is 4 cm.
An increase or decrease in this indicator indicates the risk of complications during pregnancy. And also about the likelihood of spontaneous miscarriage or premature birth.
The length of the cervix is an important indicator of a properly progressing pregnancy. Based on the size of this organ, it is possible to identify the problem in the early stages of development and prevent it.
Preparing for the study
Cervicometry during pregnancy does not require any special preparation other than emptying the bladder. Another important point is the absence of gas in the intestines. 2-3 days before the study, the patient is asked to exclude from the diet foods that increase gas formation (bread, dairy products, vegetables, etc.).
Cervicometry result
Based on the results of measuring the length of the cervix, the specialist issues a conclusion in which he describes the result and its compliance with the norm at a certain stage of pregnancy. So, the larger the fetus becomes, the shorter the cervical canal becomes. At a period of 16 to 20 weeks, the length of the cervical canal can reach 4-4.5 cm, at 25-28 weeks of pregnancy - 3.5-4 cm, after reaching a period of 32-36 weeks, the length of the canal decreases to 3-3.5 cm If the cervical length is less than 1.5 cm at the end of the second trimester, the probability of miscarriage is quite high.
Timely ultrasound diagnostics will help monitor the course of pregnancy, preserve the fetus, and carry and give birth to a healthy child.
Indications
Like any medical procedure, cervicometry has its indications and contraindications.
Indications for:
- history of preterm birth;
- a history of miscarriage in late pregnancy in the expectant mother;
- the likelihood of developing cervical canal insufficiency;
- pregnancy with twins or triplets;
- cervical ruptures during previous births and the presence of surgical scars on it;
- painful sensations in the abdominal area of the expectant mother;
- hypertonicity of the uterus;
- surgeries performed on the cervix.
This procedure has no contraindications.
For what period is it prescribed?
The method of diagnosing the cervix and cervical canal can be carried out at any stage of the perinatal period, if necessary.
The ideal period is considered to be 12-22 weeks of pregnancy. During this period, it is possible to most accurately assess the condition of the pregnant woman’s cervix.
Often the condition of the uterine cervix is assessed dynamically, starting from the 14th week of pregnancy. Subsequent studies are carried out every 2 weeks.
In cases where the expectant mother is diagnosed with “risk of premature birth,” cervicometry can be performed exclusively for health reasons in a hospital setting and under the strict supervision of doctors.
Author: ® Barto R.A., 2017Isthmic-cervical insufficiency (ICI), as defined by the American College of Obstetricians and Gynecologists (ACOG), is the inability of the cervix to maintain pregnancy in the second trimester in the absence of uterine contractions [1]. This condition in the English-language literature is described by the term “cervical insufficiency or cervical incompetence”.
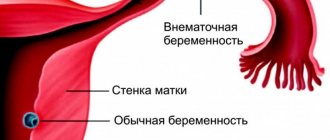
Rice. 1. Isthmic-cervical insufficiency. Transvaginal scan.
Isthmic-cervical insufficiency implies functional inferiority of the cervix and isthmus of the uterus. This leads to painless premature effacement of the cervix, accompanied by dilation and opening of the uterine os during pregnancy. In most cases, premature opening of the uterine os occurs in the 2nd trimester, usually between 18 and 26 weeks. The incidence of isthmic-cervical insufficiency, according to the literature, ranges from 0.2% to 2%.
Rice. 2. The mechanism of formation of cervical shortening during pregnancy.
Premature birth can result from numerous causes, including spontaneous abortion, premature rupture of membranes, antepartum hemorrhage, multiple pregnancies, early delivery for maternal or fetal indications (eg, maternal hypertensive conditions, intrauterine growth restriction, fetal hemodynamic abnormalities, fetal hypoxia) . Isthmic-cervical insufficiency is the cause of all premature births in only 8-9%. Clinical and laboratory studies suggest that pregnancy loss and preterm birth may result from several pathogenic processes, including premature activation of the fetal hypothalamic-pituitary-adrenal axis, intrauterine infection, decidual inflammation, hemorrhage, and abnormal uterine distension.
Diagnosis of isthmic-cervical insufficiency is primarily based on indications of the loss of a previous pregnancy in the 2nd trimester:
- Asymptomatic cervical dilatation and sagging membranes in the second trimester
- Premature rupture of membranes (PPROM)
- Rapid birth of the fetus
- Infrequent or absent uterine contractions
In the absence of these signs, the diagnosis of cervical insufficiency is based on a combination of the following signs:
- Clinical picture
- Physical examination
- Ultrasonography
In most patients, cervical insufficiency is asymptomatic or clinical manifestations may be erased:
- Feeling of pelvic expansion
- Stomach ache
- Spasms
- Back and lower back pain
- Increased vaginal discharge
Diagnosis of isthmic-cervical insufficiency
- Ultrasound examination of the length of the cervix (cervicometry) has an inverse correlation with the risk of spontaneous preterm birth, especially in women with a history of preterm birth [2,3].
- Fetal fibronectin (fFN) testing in addition to cervical length assessment significantly increases the risk of preterm birth in women with positive fetal fibronectin and a cervical length of less than 30 mm [4, 5].
Ultrasound cervicometry is a measurement of the length of the cervix:
- Measuring the length of the cervix should only be done with a transvaginal sensor.
- Cervical shortening of less than 25 mm is associated with an increased risk of preterm birth, regardless of other risk factors [2, 3].
- Correct performance of cervicometry requires special training of an ultrasound physician
Shortening of the cervix begins from the internal os and then occurs caudally with the appearance of a funnel-shaped opening on the side of the internal os (“funnel”), which leads to progressive shortening of the cervical canal [6]. However, the presence of a funnel does not increase the risk of preterm birth with a short cervix [7].
Rice. 3. Diagram of cervical measurements.
In pregnant women without clinical manifestations (so-called asymptomatic patients) with a history of previous premature birth, sequential transvaginal screening of the cervix is performed from 14-16 weeks of gestation. Then cervicometry is repeated every 2 weeks until 26-28 weeks of pregnancy, then according to indications.
For women not experiencing preterm labor, the American College of Obstetricians and Gynecologists (ACOG) recommends transabdominal assessment of cervical length during fetal anatomical examination (between 18 and 22 weeks of gestation) and a transvaginal measurement if cervical shortening is suspected [7]. Although a 2013 Cochrane review did not find sufficient evidence to recommend routine cervical screening for all pregnant women, ACOG confirms that this screening strategy may be considered [8, 9].
It should be borne in mind that all available in the literature guidelines for ultrasound diagnostics in any trimester of pregnancy indicate the need not only for a thorough study of the anatomy of the fetus, but also its membranes, including the uterus, appendages, tumors, anatomical disorders, with a mandatory accurate description identified changes. We must not forget that asymptomatic women may already have cervical disease or an ovarian tumor in a short period of time.
Transvaginal cervicometry is performed on all pregnant women at risk of premature birth. Even in the presence of uterine contractions, the likelihood of preterm labor is unlikely with a cervical length greater than 30 mm [10, 11]. On the contrary, it has been shown that a cervix less than 15 mm long and symptomatic in approximately 60% will lead to preterm birth within 7 days of the detected changes [12].
Method of performing ultrasound cervicometry (see link)
Tactics for isthmic-cervical insufficiency
In women with a history of isthmic-cervical insufficiency or asymptomatic second-trimester cervical dilation on physical examination, cervical cerclage placement at the cervicovaginal junction is indicated, according to the 2014 practice bulletin of the American College of Obstetricians and Gynecologists (ACOG) [1].
Circlage is performed transvaginally or transabdominally. The most common methods:
- Vaginal suturing of the cervix according to McDonald (McDonald cerclage)
- Vaginal suturing of the cervix according to Shirodkar cerclage
- Transvaginal Cervico-Istmic Cerclage (TVCIC)
- Transabdominal Cerclage (TAC)
- Laparoscopic cerclage
The history of surgical treatment of isthmic-cervical insufficiency begins with the cerclage, which was placed transvaginally on the distal cervix as a stitch in an attempt to improve its strength and reduce distension. At the present stage, cerclage is applied through transvaginal or transabdominal access, the main task of which is to strengthen the cervix as close as possible to the level of the internal os, thereby increasing the functional length of the cervix. Of the most commonly performed transvaginal techniques, the MacDonald cerclage is performed with sutures around the perimeter of the cervix in a “tie-to-bag” type, which pass through the stroma of the cervix in the form of a “noose,” while Shirodkar suturing requires tissue dissection and displacement of the bladder anteriorly, and straight intestines posteriorly to place the suture at the level of the internal os. Transabdominal cerclage (TAC) is typically used for patients with anatomical restrictions (eg, post-trachelectomy) or ineffective transvaginal cerclage.
Rice. 4. Diagram of cerclage application according to MacDonald.
Rice. 5. Scheme for suturing according to Shirodkar.
Transabdominal cerclage was proposed by Benson in 1965. In view of the development of laparoscopic access and surgical technologies, transabdominal cerclage remains the method of choice in cases where laparoscopy is not possible: for example, with technical difficulties or during pregnancy, when the uterus is large.
Rice. 6. Scheme of the transabdominal cerclage.
Rice. 7. Scheme of Benson’s transabdominal cerclage (Fedorov A.A., 2014).
In singleton pregnancies, cervical cerclage is the mainstay of surgical treatment of cervical insufficiency and is reasonable in the following situations [1]:
- Loss of a previous pregnancy in the second trimester with asymptomatic cervical dilatation
- Cerclage placement during a previous pregnancy
- Presence of asymptomatic cervical dilatation in the 2nd trimester of pregnancy
- Cervix length less than 25 mm at 16-24 weeks, indicating previous spontaneous preterm birth before 34 weeks of pregnancy
Preoperative assessment of the pregnant woman should include the following:
- Qualified ultrasound examination (clarification of gestational age, fetometry, exclusion of fetal development anomalies) with mandatory assessment of the amount of water, the structure of the membranes, uterus, examination of the appendages, examination of the cervix and internal os, the relationship of the membranes with the internal os)
- Clinical examination to exclude bleeding, threat of preterm labor, and intra-amniotic infection
In the postoperative period, observation and prevention of surgical complications are carried out, including cutting of sutures, rupture of membranes, and chorioamnionitis.
Despite the successes of surgical treatment, many studies confirm the positive effect of treatment with progesterone (utrogestan) in pregnant women at risk of isthmic-cervical insufficiency. In addition, the obstetric pessary may be a noninvasive alternative for the treatment of cervical insufficiency, although research in this direction is needed. The presence of a pessary does not guarantee protection against the progression of ICI and requires monitoring (clinical, physical, ultrasound).
Indications for the application of laparoscopic cerclage when planning pregnancy (Fig. 8):
1. Patients with previous cervical surgery:
- Trachelectomy
- Amputation or high amputation of the cervix with absence of the vaginal portion or cervical length less than 25 mm
2. Ineffectiveness of previous surgical correction of ICI and cervical length less than 25 mm
Indications for the application of transvaginal cerclage when planning pregnancy:
- Amputation or high amputation of the cervix with the presence of the vaginal part of the cervix and a cervical length of more than 25 mm
- Ineffectiveness of surgical correction of ICI by suturing the cervix during a previous pregnancy and the length of the vaginal part of the cervix is more than 25 mm
The objects of surgical intervention are the distal part of the uterus and uterovaginal anastomosis after trachelectomy or the isthmus, a preserved fragment of the cervix after its amputation. Preoperative examination before cerclage must be carried out in a center specializing in the correction of this pathology and should include:
- qualified ultrasound examination
- office hysteroscopy
Rice. 8. Pregnancy 18 weeks. Longitudinal transvaginal scanning of the cervix. Circlage in the form of a loop at the level of the internal pharynx. White arrows indicate the anterior and posterior parts of the synthetic prosthesis (cerclage).
Method of applying laparoscopic cerclage (MONIIAG):
Using laparoscopic access, the vesicouterine fold of the peritoneum is opened and the bladder is mobilized. A section of the uterovaginal junction is identified along the anterior wall of the uterus, the lateral surface of this zone is mobilized with the formation of tunnels in the parameters between the ribs of the uterus and the uterine vessels when the latter, together with the ureter of the same side, are displaced laterally. Next, the posterior layer of the peritoneum is opened above the uterosacral ligaments.
A polypropylene flap (Gynemesh soft) 12-15 mm wide or a mersilene tape 5 mm wide is inserted into the abdominal cavity, which, under tension, is placed circularly through previously formed tunnels around the distal isthmus of the uterus or the cervix, if it is preserved. The flap is fixed with separate extracorporeal sutures to the anterior surface of the uterus, then peritonization is performed.
Literature:
- Practice bulletin no. 142: cerclage for the management of cervical insufficiency. Obstet Gynecol. 2014 Feb. 123(2 Pt 1):372-9.
- Iams JD, Goldenberg RL, Meis PJ, Mercer BM, Moawad A, Das A, et al. The length of the cervix and the risk of spontaneous premature delivery. National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network. N Engl J Med. 1996 Feb 29. 334(9):567-72.
- Crane JM, Hutchens D. Transvaginal sonographic measurement of cervical length to predict preterm birth in asymptomatic women at increased risk: a systematic review. Ultrasound Obstet Gynecol. 2008 May. 31(5):579-87.
- Gomez R, Romero R, Medina L, Nien JK, Chaiworapongsa T, Carstens M. Cervicovaginal fibronectin improves the prediction of preterm delivery based on sonographic cervical length in patients with preterm uterine contractions and intact membranes. Am J Obstet Gynecol. 2005 Feb. 192(2):350-9.
- Schmitz T, Maillard F, Bessard-Bacquaert S, Kayem G, Fulla Y, Cabrol D, et al. Selective use of fetal fibronectin detection after cervical length measurement to predict spontaneous preterm delivery in women with preterm labor. Am J Obstet Gynecol. 2006 Jan. 194(1):138-43.
- Zilianti M, Azuaga A, Calderon F, Pagés G, Mendoza G. Monitoring the effacement of the uterine cervix by transperineal sonography: a new perspective. J Ultrasound Med. 1995 Oct. 14(10):719-24.
- Berghella V, Owen J, MacPherson C, Yost N, Swain M, Dildy GA 3rd. Natural history of cervical funneling in women at high risk for spontaneous preterm birth. Obstet Gynecol. 2007 Apr. 109(4):863-9.
- Practice bulletin no. 130: prediction and prevention of preterm birth. Obstet Gynecol. 2012 Oct. 120(4):964-73.
- Berghella V, Baxter JK, Hendrix NW. Cervical assessment by ultrasound for preventing preterm delivery. Cochrane Database Syst Rev. 2013. 1:CD007235.
- Tsoi E, Fuchs IB, Rane S, Geerts L, Nicolaides KH. Sonographic measurement of cervical length in threatened preterm labor in singleton pregnancies with intact membranes. Ultrasound Obstet Gynecol. 2005 Apr. 25(4):353-6.
- Iams J.D. Prediction and early detection of preterm labor. Obstet Gynecol. 2003 Feb. 101(2):402-12.
- Sotiriadis A, Papatheodorou S, Kavvadias A, Makrydimas G. Transvaginal cervical length measurement for prediction of preterm birth in women with threatened preterm labor: a meta-analysis. Ultrasound Obstet Gynecol. 2010 Jan. 35(1):54-64.
Sincerely, ultrasound diagnostics doctor, Barto Ruslan Alexandrovich, 2017
All rights reserved®. Quoting only with the written permission of the author of the article.
Technique
To understand how cervicometry is done during pregnancy, it is necessary to consider the basic techniques. The cervicometry procedure can be performed in 2 ways:
- outer;
- interior.
External or transabdominal cervicometry is performed with an external ultrasound sensor through the abdominal wall. To obtain a high-quality image, a woman needs to fill her bladder.
Internal cervicometry or transvaginal is performed using a special sensor that is placed in the vagina. In this case, it is recommended to first go to the toilet and empty your bladder. This is necessary to obtain a high-quality, clear image.
More accurate information can be obtained with a transvaginal examination. With this diagnostic method, you can measure all the necessary parameters and draw a conclusion about the condition of the organ.
Transabdominal cervicometry does not provide accurate results. With its help, you can only visually assess the condition of the cervix, but it is impossible to take measurements.
Cervicometry as a way to measure the cervix.
Cervicometry under ultrasound is carried out in two ways. Regardless of the choice of cervicometry method, both are effective, so the method of implementation depends on the characteristics of the body and the indications for the use of each of them:
- The transabdominal route is a method of performing cervicometry through the abdominal cavity. This type of study requires a full bladder. With this research method, the visibility of the internal pharynx is poor, and without its results, the data obtained may not be entirely correct.
- Transvaginal is a method of performing cervicometry by inserting a sensor directly into the vagina; during this study, the bladder must be emptied. When performing cervicometry using the transvaginal method, there is no danger to the fetus or the mother, and the norm for carrying out this procedure is considered to be no more than three times during the entire period of gestation.
Ultrasound is usually performed from 18 to 22 weeks of pregnancy. Often, cervicometry is carried out together with other studies. If termination of pregnancy has already occurred, then the study is carried out at an earlier date, starting from 10 weeks, this is done to prevent possible termination of pregnancy. Cervicometry is a fairly convenient and effective type of examination that allows you to maintain pregnancy and identify possible pathological disorders in the early stages of pregnancy.
To prepare for cervicometry using the transvaginal method, it is necessary to empty the bladder. The specialist conducting the research will do the rest, and after the examination he will give the necessary recommendations.
It is worth noting that the cervical examination procedure itself using an ultrasound sensor is absolutely harmless to the unborn child. The woman also does not feel any action during cervicometry. There is no reason to worry about undergoing cervicometry, since the appointment of the procedure does not pose any harm and there is no reason to worry about side effects after the procedure - there are simply none. Carrying out cervicometry completely eliminates the risk of complications and reduces the likelihood of pregnancy failure to zero.
Interpretation of results and norms
Like any medical study, cervicometry during pregnancy has certain norms of values.
The normal length of the cervix is 30 mm. A slight deviation of 1 mm is not a reason to panic. This is just a signal for control. When the length decreases to 25 mm, the risk of early birth increases.
If the indicator does not exceed 20 mm, only 45% of pregnant women will be able to carry and give birth to a child on time.
An alarming signal is the appearance of pain against the background of a decrease in the length of the uterine cervix. This is a sign of the onset of labor.
If you notice such a symptom, you should seek help from a doctor as soon as possible.
The internal pharynx is assessed from the point of view of its shape. Normally, it should resemble the letter “T”.
A change in this indicator has an extremely negative effect on the course of pregnancy. The amniotic sac begins to sag downward and, therefore, the risk of rupture increases.
Risks
For pregnant women, the cervicometry procedure is practically safe. Therefore, expectant mothers should not be afraid of it or worry about the possibility of complications occurring after it is performed.
In terms of its effect on the body, cervicometry does not differ from the usual ultrasound examination. The child is exposed to waves of ultrasonic radiation, but because... The procedure is short-term, they do not cause harm.
When performing cervicometry transvaginally, a pregnant woman may experience short-term, scanty discharge mixed with blood. This is not a cause for concern.
Normally, such discharge goes away on its own within a couple of days. Therefore, the expectant mother is recommended to remain in bed for 2 days after cervicometry.
After the procedure, it is not advisable to engage in active physical activity.
If the blood in the discharge does not disappear within 5 days, this is a reason to consult a doctor for advice.
Patency of the cervix
Patency of the cervix is an important indicator of a successful pregnancy. Normally, before the onset of labor, the cervix should be impassable and closed with a mucus plug.
With the onset of contractions, the cervical canal gradually opens and becomes passable for the fetus.
If during cervicometry it was determined that the cervix is not tightly closed, this signals the likelihood of premature birth.
Cervical dilatation of 1 finger is considered normal for a period of 38.5 weeks. In primiparous women, with this value, the child will be born no earlier than after 1.5 weeks.
If the cervix opens much earlier than the term, this is an indication for hospitalization of the pregnant woman.
In a hospital setting, pregnancy is maintained and monitored by specialists.
Scores
During cervicometry, the following parameters are analyzed:
- degree of opening of the cervical canal;
- parameters and dimensions of the uterus;
- degree of closure of the pharynx;
- the degree of penetration of the amniotic membranes into the cervical canal of the cervix.
Each result obtained is assigned a point depending on its value.
Cervicometry scores for certain indicators:
- dense cervix along the entire length – 0 points;
- there is compaction only in the pharynx area – 1 point;
- soft neck – 2 points;
- cervical length more than 20 mm – 0 points;
- length 10-20 mm – 1 point;
- length less than 10 mm – 3 points;
- closed throat – 0 points;
- 1 finger opening – 1 point;
- opening in 2 fingers – 2 points.
If the total score is less than 3, then the cervix is immature, up to 6 points - ripening, up to 10 points - mature.
Normally, complete ripening of the cervix occurs at the onset of labor. If this indicator appears earlier, then measures should be taken to maintain the pregnancy.
Cervicometry is an accurate method for diagnosing the condition of the cervix of a pregnant woman. It is completely safe and allows you to determine the likelihood of premature birth. If you notice any alarming symptoms, you should consult a doctor as soon as possible.
https://youtu.be/GQ3z3g8biTA
Types of cervical pathologies
The most common problems identified after cervicometry are:
- shortened neck from 1 to 2.5 cm long;
- immature cervix. Features of the immaturity of the reproductive organ at the 37th week of pregnancy are: density or slight softening of the tissues of the cervix, while the softness of the muscle layer should be along the entire length of the cervix;
- closure of the cervical canal or its opening to a width of no more than a fingertip, instead of the required two;
- the cervical canal is deviated posteriorly, whereas normally it should be in the middle;
- the length of the canal is more than 2.5 cm versus the normal two, and before birth the length is less than 1 cm or is completely smoothed out.
Short neck
Causes of shortening of the cervix:
- hormonal disorders: increase or decrease in the level of the male hormone testosterone;
- decrease in the level of the corpus luteum hormone - progesterone;
- a combination of hyperandrogenism with elevated levels of male hormones with progesterone deficiency;
- increased or decreased levels of estrogen in the blood.
- congenital defects in the structure of the uterus and cervical canal;
A shortened cervix can cause premature labor
This pathology can lead to dangerous consequences, such as:
- threat of prematurity;
- high probability of spontaneous miscarriage;
- excessively rapid birth from 2 to 6 hours with perineal ruptures, birth injuries and hypoxia from lack of oxygen in the child due to the unpreparedness of the birth canal for the passage of the child’s head;
- development of isthmic-cervical insufficiency;
- infection of the membranes, and then the fetus, due to the bulging of the bladder from the body of the uterus into the cervical region.
Treatment tactics for shortened neck:
- medicinal: prescription of hormonal drugs to equalize hormone levels: vaginal use of micronized progesterone;
- hormonal drugs to lower testosterone levels in the blood: Danazol;
- Dexamethosone;
- Digoxin;
- estrogens;
- installation of a unloading pessary that prevents the cervix from opening prematurely. The device redistributes the pressure on the organ and allows you to extend the gestation period as much as possible, starting from the second trimester. The disadvantage of this method is the need to treat the pessary with sterile solutions every two weeks to prevent inflammation of the pelvic organs. Before birth, but not earlier than the 37th week, the pessary must be removed;
A gynecological pessary redistributes the load and prevents the cervix from opening prematurely