The location of the pancreas is such that it is not very accessible for palpation, so diagnosing its diseases requires instrumental and laboratory research methods.
Of the instrumental methods, one of the fastest, most informative and safest, allowing one to determine the density and size of the pancreas in normal and pathological conditions, to detect inflammation, developmental abnormalities, tumors, the presence of stones, cysts, fistulas, is ultrasound examination (ultrasound).
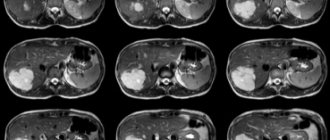
Other methods either do not provide the necessary information or are less accessible, such as MRI. It is more accurate and visual, but is not available everywhere and is much more expensive than ultrasound.
Laboratory indicators are important for diagnosing pancreatic diseases - determination of enzymes in the blood and urine. Normally they shouldn't be there. Therefore, if their appearance is detected, the patient is almost always prescribed an ultrasound.
When should you do an ultrasound of the pancreas?
The doctor may prescribe an ultrasound of the pancreas and other abdominal organs in the following cases:
- long-term pain in the epigastrium;
- recurrence of pain;
- painful reaction when palpating this area;
- presence of palpable formations;
- identification of possible complications of previously diagnosed chronic or acute pancreatitis;
- assumption of the presence of an abscess, hematoma, stone, cyst or tumor of the pancreas;
- newly diagnosed diabetes mellitus;
- additional examination after deformation of the posterior wall of the stomach detected by gastroscopy;
- detection of changes in the shape of the duodenum during X-ray examination.
This examination can be prescribed to adults and children both for emergency reasons and on a routine basis. Modern equipment makes it possible to conduct research at the patient’s bedside.
The essence of the study
The essence of the method is the registration of waves (echoes) reflected from organs by a sensor. Fabrics with different densities reflect them differently. The information is displayed on the screen in the form of a picture, where areas with higher density appear darker.
The examination is carried out with the patient lying on his back, the examination begins with the identification of large vessels located in the abdominal cavity - this serves as a guide to determine the position of the gland. The position of the gland relative to the spine is also determined.
The main part of the study is carried out at maximum inspiration.
It may be necessary to examine in other projections, in the position on the left and right side, as well as in an upright position.
The examination is completely safe and painless.
During the examination, the endoscopist fills out a standard protocol form, which indicates the size of the gland and its parts, density, uniformity of structure, clarity of the contours of the organ and ducts, and the presence of areas with altered density. If necessary, photographs can be attached to the protocol.
What do deviations from average values indicate?
The final diagnosis is made by a qualified specialist based on the analysis of the following parameters.
Deviation of pancreas size
Dilatation of the Wirsung duct of more than 3 mm indicates chronic pancreatitis; with the introduction of secretin (a peptide hormone that stimulates pancreas function), its parameters do not change. The presence of a neoplasm in the gland is indicated by an increase in the diameter of the organ or its individual parts. Narrowing of the main duct is observed in cystic formations. A malignant tumor of the head is characterized by a significant increase in size – more than 35 mm. It is thanks to ultrasound that approximately 10% of pancreatic cancers are diagnosed.
Changes in the outlines of the lobes of the gland
The presence of an inflammatory process is indicated by an image with blurry contours, however, in some cases, swelling of the organ can be caused by gastritis, gastric ulcer and duodenal ulcer. A convex and smooth shape of the contours of individual areas is observed with cystic changes or an abscess. Uneven borders indicate pancreatitis or a tumor formation, which is characterized by individual parameters - they are taken into account by an experienced sonologist.
Structure indicators
The average density of the pancreas is similar to the structure of the spleen and liver. Ultrasound results indicate the presence of small areas of inclusions in the granular structure and uniform echogenicity - its increase indicates chronic pancreatitis, the presence of stones, and the presence of a tumor-like formation. The absence of reflection of high-frequency waves is observed with cystic changes and abscess.
Presence of abnormal forms of the pancreas
It can be spiral, split into two isolated halves, ring-shaped, aberrant (additional). These changes indicate either congenital defects or a complex pathological process.
The patient is given a conclusion that describes all the parameters of the pancreas and indicates the identified pathologies. For minor deviations from normal parameters, a preliminary diagnosis is not made. Some pancreatic defects do not affect the normal functioning of the body, but some pathological changes can develop further and worsen a person’s health. However, it should be remembered that ultrasonography reveals only their echogenic signs; additional studies must be carried out to confirm or refute the preliminary diagnosis!
At the end of the above information, I would like to emphasize once again that preventive ultrasound examination of the pancreas should not be ignored! Many diseases are detected even in the absence of signs disturbing the patient - the pathological clinic in such cases is in a sluggish period. Timely diagnosis of illnesses and rationally administered treatment gives successful results and ensures a decent quality of life for patients.
Diseases of the pancreas have a similar symptomatic picture. To make an accurate diagnosis and select the appropriate treatment, doctors prescribe their patients to undergo an ultrasound examination (ultrasound), which allows them to assess the condition of the organ, the presence of pathological processes in it and their extent. An ultrasound scan of the pancreas lasts about 10-15 minutes. The procedure is completely painless for the patient and does not require prior hospitalization. The transcript of the pancreatic ultrasound is given to the patient immediately after the examination.
How to prepare for an ultrasound examination?
A routine endoscopic examination of the abdominal organs must be carried out on an empty stomach, the stomach must be empty. Otherwise, the reliability of the study is significantly reduced.
Imaging accuracy may be affected by increased gas production in the intestines. It needs to be minimized and intestinal motility improved.
Therefore, on the eve of a scheduled ultrasound, a gentle diet is recommended for 2-3 days, avoiding legumes, black bread, cabbage, carbonated drinks, and sweets. The last meal should be no later than 19 hours before the test day.
Preparation for an ultrasound of the pancreas and neighboring organs may include taking activated charcoal, laxatives, enzymes and drugs that reduce gas formation.
In emergency cases, ultrasound can be performed without preparation.
Preparing for an ultrasound scan for pancreatitis
To carry out the procedure correctly, you should be thoroughly prepared. If we are talking about an emergency operational situation, ultrasound is performed without preparation. The accuracy will be much lower, visible results are not guaranteed. For a routine ultrasound, the patient must be explained how to prepare for the examination. Let's take a closer look at the procedure:
- Ultrasound is often prescribed in the morning, on an empty stomach; at this time, little air has accumulated in the digestive system.
- If time permits, 2 days before the procedure, remove foods that cause gas formation (fruits, vegetables, dairy products, soda) from your diet.
- To reduce flatulence, you can take activated carbon or espumizan.
- The last meal should take place at least 12 hours before the ultrasound, otherwise the result will be distorted.
- It is recommended to do an enema before the study.
- It is undesirable to use medications, alcohol, or smoking before the upcoming process.
A complete picture of the disease will require accurate data. Compliance with the listed preparation rules will allow you to obtain them.
How does the ultrasound protocol describe a normal pancreas?
The human pancreas at birth has a length of up to 5.5 cm and increases during the first year of life to 7 cm. The size of the head initially does not exceed 1 cm. Then growth continues until approximately 18 years.
Therefore, the norm in children varies depending on age and weight; to determine the pathology, calculations are made using special tables. The experience of the doctor conducting the study is also important.
In addition to the length, which reaches from 16 to 23 cm in adulthood, the pancreas has a width of up to 9 cm and a thickness of up to 3 cm, which smoothly decrease from head to tail.
The structure of the gland is normally homogeneous, consisting of small lobules that produce digestive juice and islets of cells that secrete hormones that regulate carbohydrate metabolism.
A duct called the Wirsung duct is visible in it; its width normally should not exceed 2 mm.
During the ultrasound examination, a comparison is made with normal values. How is the pancreas described in the protocol? Dimensions, standard:
- pancreatic head size – up to 32 mm;
- body – up to 25 mm;
- tail - about 30 mm;
- contours are smooth and clear;
- the diameter of the Wirsung duct is 1.5 - 2 mm and its expansion to 2.5 - 5 mm in response to intravenous administration of secretin;
- additional education – no;
- echostructure – homogeneous, similar to the echostructure of the liver;
- echogenicity – neither increased nor decreased.
An increase in the echogenicity of pancreatic tissue with age is not always associated with pathology.
This is what the norm looks like in adults.
Changes in size, contours and echostructure indicate the presence of congenital or acquired pathology of the organ.
Indicators of chronic pancreatitis
The ultrasound screen shows individual changes characteristic of chronic pancreatitis. Features of manifestation:
- constant expansion of the duct over 2 mm;
- the boundaries of the organ reveal a jagged membrane, sometimes with small tubercles;
- in addition to increased size, echogenicity will be less;
- sometimes pseudocysts are found in advanced disease, in such a case the echogenicity will be higher;
- as the disease progresses, the monitor screen shows how visually the pancreas becomes smaller compared to the enlarged duct, due to atrophy;
- if there is a suspicion of stone formation in an organ, you will see a circle-shaped spot with an echogenic trace;
- the structure of the organ is heterogeneous, with diffuse errors.
If moments are found when the signs of chronic pancreatitis are distorted or do not provide a complete description of the situation on ultrasound, the examination continues in other ways using MRI or CT (magnetic resonance or computed tomography).
Interpretation of ultrasound of the pancreas
In the case of normal indicators, no questions arise. If the laboratory parameters are also without deviations, we can talk about the correct functioning of the pancreas.
A diagnostic sign of acute pancreatitis is an increase in size and a decrease in the echo density of the gland due to edema.
In the case of chronic pancreatitis and cancer, echo density is increased as a result of replacement of glandular tissue with fibrous or tumor tissue. Also, in these conditions, an increase in the size of the entire gland or its individual parts is detected.
The expansion of the Wirsung duct, as well as the lack of its response to the introduction of secretin, also signals an inflammatory process.
In cases of impaired blood supply and atrophy, a decrease in the size of the gland is noted.
With pancreatic cancer, there may be an increase in individual segments, uneven structure, uneven contours, as well as depressions on the surface of the liver, compression or displacement of the aorta and inferior vena cava.
If a tumor is not visible, the doctor can assume its presence by the deviation of the tail of the gland.
The presence of fluid in cysts is determined by the observed changes in formation at different body positions.
Ultrasound visualizes areas of necrosis, abscess, and blockage of ducts with stones.
Neighboring organs must be examined - liver, spleen, duodenum, duct and vascular system. The presence of a pathological process in any of them can be the cause or consequence of pancreatic disease.
Organ sizes and their role in the human biomarker system
An organism is a biological system where all organs and functions are adjusted to each other. This means that an organism functions normally only when each of its structural parts has a size standard once determined by evolution.
In medicine and biology, there is a complex system of indicators that can be used to determine the state of the body or some part of it. The most significant indicators are:
- Body temperature;
- height to weight ratio;
- arterial pressure;
- heart rate;
- the presence, quantity or absence of substances and cells of a certain type in the blood and urine;
- organ sizes.
These, of course, are not the only biomarkers by which the state of our body can be determined, but they are the ones that give a picture of the primary diagnosis.
The dimensions of structures such as the liver, heart, pancreas, and spleen provide information about their normal or pathological condition. Usually, when pathological processes occur, the organ increases in size. This may occur due to the formation of a tumor. In addition, the organ often increases its volume, trying to compensate for the loss of function. A change in size may also be a consequence of inflammatory processes, which are accompanied by edema.
Important information: Can a person live without a pancreas?
Final diagnosis
It is important not to miss any ailment associated with pancreatic disease. The availability of ultrasound in this situation cannot be overestimated. The sooner changes in the organ are detected and appropriate measures are taken, the greater the chance of cure.
The diagnosis is made only by a doctor based on a combination of clinical manifestations, laboratory parameters and instrumental studies. In the future, dynamic monitoring of changes in the condition of the gland is needed.
The main contribution from the patient is not only strict adherence to treatment recommendations, but also maintaining a healthy lifestyle, giving up bad habits, overeating, abuse of alcohol, sweets, fatty and fried foods.
Important for the health of the pancreas is maintaining immunity, protecting against stress, and eliminating household and professional intoxications.
The effectiveness of ultrasound in pancreatitis
Using ultrasound, they examine the general visual picture of the condition of the organ, regarding the size, shape, and silhouette of the object. When changes occur, there is a reason to concentrate attention on this point. The use of ultrasonography is considered a mandatory method for diagnosing pancreatitis in any form of manifestation. The use of an examination method helps in making a diagnosis, prescribing the correct treatment for a complex disease, and allows for periodic analysis of the condition of internal organs.
Thanks to ultrasound, the initial stage of the disease is detected, and it is easy to monitor organs. For the doctor and the patient, it is easier to prevent an impending threat than to fight it later.
Computed tomography indicators
In unclear diagnostic cases, MRI (magnetic resonance imaging) is more often used to clarify the pathology of the abdominal organs. If for some reason it is not suitable for the patient, computed tomography is used, which has received good feedback from doctors of all specialties. The method allows you to make layer-by-layer sections of the digestive organs in various projections and construct a three-dimensional image.
The tissues are exposed to x-rays, and the results are processed by a specially developed computer program. The exact dimensions of the pancreas are assessed and additional formations are identified. For a clearer image of the pancreas, iodinated contrast is used. It allows you to accurately detect changes in the vascular pattern, pathological changes in pancreatic tissue, and assess the prevalence of the tumor process.
There are contraindications: pregnancy, childhood, iodine intolerance (if performed with contrast), liver and kidney pathology.
The development of modern medical technologies makes it possible to diagnose pancreatic pathology at the initial stages of its appearance. Knowledge of normal sizes and the ability to interpret the results obtained reduce morbidity and maintain a high quality of life.
Bibliography
- Mitkov V.V. Doppler ultrasonography of celiac blood flow is normal. Ultrasound and functional diagnostics 2001 No. 1 pp. 53–61.
- Sidu P.S., Chong W.K. Ultrasound measurements. Practical guide. Medical literature Moscow 2012
- Ultrasound diagnostics: standards, materials and guidelines. Edited by S.A. Balter. M. Interprax 1990
- Drobakha I.V., Yakusheva L.V., Malysheva T.F., Chavgun L.B. Ultrasound examinations in the diagnosis of acute pancreatitis. Congress of the Association of Ultrasound Diagnostics in Medicine, abstracts. M., 1995, p. 82.
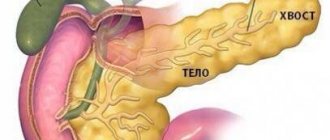
Dimensions and location
The pancreas is localized in the abdominal cavity on the left side below the stomach (hence the name) parallel to the costal arches in close proximity to the liver and spleen. There are three sections: the head (opens directly into the duodenum), body and tail.
Its role in the body is the formation of digestive enzymes and the synthesis of insulin, which is responsible for the concentration of glucose in the blood. Thus, iron participates in tissue nutrition. Disturbances in its work lead to serious pathologies of an endocrine nature.
During inflammation, the release of digestive enzymes becomes difficult; they begin to digest the parenchyma of the organ, causing the replacement of normal tissues with connective tissues; necrosis can cause the development of an oncological process.
In a healthy adult, the normal size of the pancreas is in the range of 16–23 cm. The size of the head is 32 mm. The longest part is the tail, it should not exceed 35 mm. The width of the organ is 5 cm.
If everything is normal, then the person does not feel pain or any discomfort; the organ cannot be felt during palpation. When the size of the pancreas exceeds 25 cm and the size of the tail exceeds 35 mm, this will indicate the presence of a pathological process (with pancreatitis and oncological processes it increases, a decrease indicates ischemia or atrophy).
The note. The size of the pancreas does not depend on a person’s gender, so they are the same in men and women.
The structure of the pancreas
In infants, the size of the organ is approximately five centimeters. By the first year of life it will increase by two centimeters, and by ten years the size will be 15 cm. Further growth will be slowed down until hormonal changes in the body.
During puberty, the organ grows to normal size, like that of an adult, and is fully formed by the age of 18-20. For many, final formation occurs by the age of 16.
The main excretory channel for digestive enzymes produced in the gland is the Wirsung duct (length 20 cm), into which smaller excretory ducts drain. It begins in the tail and runs along the entire gland, eventually flowing into the duodenum.
If its size exceeds the norm, then this indicates the presence of a painful process, which in most cases is pancreatitis. In this case, the digestion and absorption of food is disrupted, since enzymes do not enter the stomach in the required quantities. Their excess in iron leads to the fact that it begins to digest itself.
You can see changes using ultrasound, CT or MRI. The last two methods are the most informative, but the price of such diagnostics is quite high, and during computed tomography a person is exposed to a significant dose of radioactive radiation.
Research objectives
Any examination has certain goals and objectives, in addition to confirming the main diagnosis. An ultrasound examination will show whether the norm or deviation is observed at the time of the procedure.
The following tasks are to be identified:
- location of the pancreas;
- the configuration of this organ;
- size at the time of the examination to understand whether there is an increase;
- How distinct are the contours?
- structure of the parenchyma.
Additional tasks of the procedure:
- understand whether echogenicity is increased or within normal limits;
- determine the diameter of the main pancreatic and bile duct.
An ultrasound examination allows the doctor to determine the condition of the tissue surrounding the organ. The examination will help determine the condition of the blood vessels, and it will immediately be visible on the monitor screen whether nearby organs have been damaged or not.
For special indications, in the process of hardware research, doctors conduct a more detailed and in-depth study of the power of blood flow passing in the vessels located inside and next to the pancreas. The structure is also examined more closely.
The objectives of the study are to compare existing deviations from the norm and anomalies in the structure of the organ.
The doctor also determines:
- inflammation (of varying degrees of manifestation);
- tumor (it can be of various origins - benign or cancerous);
- focal forms of fatty degeneration.
Changes that come with age will also be visible on ultrasound. Chronic pancreatitis manifests itself quite clearly, so the doctor will be able to determine the severity of the disease and develop therapy appropriate to the condition.
If necessary, during this procedure a special analysis can be performed - sampling a section of gland tissue. The action is performed with a thin needle, the entire procedure is carried out under ultrasound control.
Tissue sampling is required for careful examination in a histology laboratory. Based on the data obtained, the final diagnosis will be made.
Causes of local growth of the pancreatic head
It was not possible to determine the direct factor that leads to cancer of the head of the pancreas, and the disease is still being studied.
Often the male gender is affected by the disease. In addition, there are a number of negative reasons that affect the enlargement of the head of the pancreas.
- Poor nutrition. Excessive consumption of fatty foods leads to the production of large amounts of cholecystokinin. If there is an excessive amount of this hormone, cell hyperplasia may occur.
- Chronic diseases, including pancreatitis. Stagnant, damaging juice can lead to the degeneration of benign tumors into malignant neoplasms.
- Gallbladder diseases provoke tumor formation. Unsafe diseases include chronic calculous cholecystitis, psychocholecystectomy symptom, and cholelithiasis.
- Smoking, excessive drinking.
alcohol abuse
Not least important in the development of malignant tumors is hereditary predisposition. Therefore, if relatives have this disease, the risk of occurrence increases. In addition, people who work in unfavorable conditions when pancreatitis occurs in pregnant women are at risk.
In this case, a formation on the head of the pancreas also happens:
- due to operations previously performed on the pancreas;
- long-term use of medications;
- abscesses;
- cysts with fluid - detected on ultrasound as an anechoic formation;
- pseudocyst - accumulated pancreatic juice and fragments of parenchyma, surrounded by fibrous tissue, which on sonography is visible in the head of the pancreas as a hypoechoic formation in the form of a shadow;
- clogging of the Wirsung canal with calcification.
Impairments in the functionality of internal organs cannot always be felt; some pathologies pass without symptoms.
In turn, when the head of the pancreas is affected, the disease often occurs without symptoms, but in other cases, the patient will encounter a number of manifestations.
Based on age and physical well-being, signs of the disease are:
- painful discomfort of varying strength, radiating to the left limb or to the back;
- a burning sensation in the upper part of the peritoneum, where the ribs diverge;
- the temperature increases, which is not amenable to antipyretic drugs;
- often there is an attack of nausea, which leads to vomiting;
- the intestines are emptied unstably - diarrhea gives way to constipation.
pancreas hurts
Additional symptoms of pancreatic head cancer include:
- weight will rapidly decrease to the point of anorexia;
- lack of desire to eat;
- belching;
- dry mouth;
- feeling of heaviness in the peritoneum;
- thirst.
Then the clinic changes. The formation of the head of the pancreas increases, and the growth of metastases in other organs and tissues is observed. The patient experiences signs of yellowing of the skin and mucous membranes, discoloration of feces, unbearable itching and dark urine. It happens that your nose bleeds, your head hurts and your heart beats faster.
Additionally, the pathology develops through the accumulation of fluid in the abdomen, blood clots occur in the veins of the legs, bleeding in the intestines, the functionality of the heart muscle is impaired, and splenic infarction.
When the gallbladder becomes inflamed, the patient develops heartburn and colitis.