Fibroadenomatosis of the mammary glands
This component of hyperplastic syndrome includes a wide range of pathological changes in epithelial, stromal and other tissues (changes in adipocytes, vascular structures) in the mammary glands, united by the general concept of “fibroadenomatosis” or “mastopathy”.
It should be noted that the classification and analysis of this type of HS (hyperplastic syndrome) is very difficult and contradictory due to the lack of clear clinical and morphological criteria to distinguish between physiological and pathological changes in the mammary glands. This leads to numerous conflicting conclusions about the possible connection between benign changes in the mammary glands and the subsequent development of malignant neoplasms in them. The first attempts to classify hyperplastic changes in the mammary glands were based on purely clinical signs, when palpable formations were divided into diffuse forms (mastopathy) and nodular (nodose) - adenoma, fibroadenoma. According to the definition of GS in relation to the mammary glands, adopted by WHO (1984), mastopathy is a disease characterized by a wide range of proliferative and regressive changes in mammary gland tissue with an impaired ratio of epithelial and connective tissue components.
In accordance with the latest revision of the International Statistical Classification of Diseases (ICD-10), several variants of the disease have been identified, which are presented in Table. 4.3.
Classification of benign mammary dysplasia (according to ICD-10)
| Code | Breast diseases (codes 60–64) |
| 60 | Benign breast dysplasia |
| 60.0 | Solitary cyst of the mammary gland |
| 60.1 | Diffuse cystic mastopathy |
| 60.2 | Fibroadenosis of the mammary gland |
| 60.3 | Fibrosclerosis of the mammary gland |
| Cystic mastopathy with epithelial proliferation | |
| 60.4 | Breast duct ectasia |
| 60.8 | Other benign breast hyperplasias |
| 60.9 | Benign breast dysplasia, unspecified |
It should be noted that accurate statistical data on the incidence of FAM (fibroadenomatosis) are not available due to the lack of uniform diagnostic criteria and a clear pathogenetic classification of the disease. At the same time, a very rough estimate of the frequency of FAM (fibroadenomatosis) of the mammary glands indicates a significant spread of the disease. Thus, it is believed that in the premenopausal period, fibroadenomatosis occurs in about 70% of all benign breast diseases. Perhaps more accurate incidence rates are reflected in cohort studies, in which the cumulative incidence of FAM (biopsy-proven diagnoses) by age 65 years was 8.8%, and for fibroadenoma it was 2.2%.
Morphological changes observed in the mammary glands of patients with fibroadenomatosis are characterized by the following features (Semiglazov V.F. et al., 1992):
1) hyperplasia of the epithelial lining of the ducts and lobules of the mammary gland (adenosis or masoplasia). There is an increase in the number and size of the mammary gland lobules;
2) fibrosis of interlobular connective tissue. Manifested by an increase in the number of collagen fibers and a decrease in the number of connective tissue cells;
4) proliferation of epithelial cells, which can be observed in ducts, lobules and cysts.
All these changes can be determined in isolation or combined in different proportions, develop in limited areas of the mammary glands or have multifocal development.
Assessing the severity of proliferative changes in the epithelium in the ducts and lobules of the gland is of primary importance for determining the prognosis and the relative risk of developing breast cancer. In this regard, three forms of FAM are distinguished based on a morphological study of biopsy material:
1) non-proliferative form;
2) proliferative form, without atypia;
3) intraductal atypical proliferation.
Taking into account this classification, the greatest risk of developing breast cancer is observed in groups of women in whom signs of atypical proliferation were detected in the mammary gland.
The most common non-proliferative form of FAM is not characterized by proliferation of the epithelium of lobules and ducts. The relative risk of developing breast cancer for this group of women does not exceed that for the general population. The proliferative form of FAM and, especially, the proliferative form with atypical proliferation increases the risk of developing a malignant neoplasm by 3–5 times.
There is also a pattern in the age-related dynamics of changes in FAM. In girls during the period of formation of menstrual function, immature fibroadenomas are often encountered; in the mature reproductive period (25–39 years), bilateral diffuse FAM increasingly develops. During perimenopause and with the onset of postmenopause (40–49 years), the development of localized forms of FAM, cystic FAM, and sclerosing adenosis is characteristic. With the onset of deep postmenopause, the frequency of proliferative processes and various forms of mastopathy sharply decreases and non-proliferative processes (ductectasia, galactophoritis, fatty involution) come to the fore. But in the same period, the incidence of breast cancer increases sharply (Semiglazov V.F. et al., 1992).
The noted age-related evolution of benign changes in the mammary glands is undoubtedly determined by the age-related dynamics of the secretion of sex hormones. The peak secretion of sex hormones, which occurs throughout the reproductive period, stimulates the proliferation of target tissues, while the decline of ovarian function determines a decrease in hormonal (primarily estrogen) levels and the development of involutive changes in the entire reproductive system.
It is appropriate to note here that using the example of the mammary gland one can see a “concentrated” expression of the entire spectrum of diagnostic problems inherent in hyperplastic syndrome in the reproductive homeostat.
Indeed, the noted disorders are characterized by an extremely wide age range in which they can manifest themselves: from adolescence, in adulthood and in postmenopause.
A fairly wide morphological spectrum of changes in the glandular and ductal epithelium of the mammary glands is determined, which in various “whimsical” combinations form complexes of structures that are very difficult to accept an acceptable morphological classification (see Table 4.3). The situation is saved by simply identifying three main forms of mastopathy, according to morphological criteria: proliferative, without proliferation and with atypical proliferation of the ductal epithelium. According to clinical manifestations, diffuse and nodular forms are distinguished.
Share “Mammary fibroadenomatosis”
Information
Sources and literature
- Minutes of meetings of the Expert Commission on Health Development of the Ministry of Health of the Republic of Kazakhstan, 2013 1. Berg V.A., Blum D.D., Cormack D.B., et al. Combined screening of ultrasound and mammography versus mammography alone for women at increased risk of breast cancer. 2008 May 14; 299(18): 2151 – 63. 2. McCavert M, Odonnell ME, Aruri S, et al. Ultrasound is a useful adjunct to mammography in the evaluation of breast tumors in all patients. International Journal of Clinical Practice. November 2009; 63(11): 1589 – 94. 3. Guimair B, Khan MI, Bibusal T, et al. Accuracy of triple testing in the diagnosis of a palpable breast lump. Journal of Nepal Medical Association. 2008; 47(172): 189 – 92. 4. Corsetti V, Hussami N, Ferrari A, et al. Breast screening with ultrasound in women with mammographically negative breast density: Evidence for detection of advancing cancer and false-positive results. European Journal of Oncology. 2008; 44: 539 – 44. 5. Hung WK, Chan SWW, Suen DTC, et al. Referral to the clinic to mammologist specialists. Surgical Journal. December 2006; 76(5): 310 – 12. 6. Afonso N. Women at high risk of developing breast cancer - What primary care physicians need to know. American Journal of Family Medicine. 2009; 22: 43 – 50. 7. Medical advisory secretariat. Mammography screening for women aged 40 to 49 years at average risk of developing breast cancer. Ontario Health Technology Assessment Serial Study. 2007; 7(1). 8. Gottz PK, Nielsen M. Screening for breast cancer using mammography. Cochrane Database of Systematic Reviews. 2009 Oct 7(4): CD001877. 9. Thistlewaite D, Stewart RA. Clinical breast examination in asymptomatic women: A study of the evidence. Australian family doctor. 2007 March; 36(3): 145 – 50. 10. Agency for Quality and Healthcare Research. Guide to the Clinical Prevention Recommendations of the American Preventive Services Task Force, Government 2009. (Online communication February 12, 2010 at https://epssahrq). 11. Kosters D.P., Gotts P.K. Regular self- and clinical examinations for early detection of breast cancer. Cochrane Database of Systematic Reviews. 2003; 2: CD003373. 12. Harvey M., Hooper L., Howel A.H. Central obesity and breast cancer risk: a systematic analysis. Obesity analysis. 2003 August; 4(3): 157 – 73. 13. Innu M, Noda M, Kurahashi N, et al. Influence of metabolic factors on subsequent cancer risk: results of a large population-based cohort study in Japan. European Journal of Cancer Prevention. 2009 June; 18(3): 240 – 47. 14. McCormack VA, Dos Santos Silva I. Breast density and parenchymal features as markers of breast cancer risk: A meta-analysis. Epidemiological biological markers of cancer prevention. 2006; 15(6): 1159 – 69. 15. Marchbanks PA, McDonald DA, Wilson HG, et al. Oral contraceptives and the risk of breast cancer. New England Journal of Medicine. 2002; 346 (26): 2025 – 32. 16. Gao Y, Shu H, Dai Q, et al. The relationship of menstrual and reproductive factors with the risk of breast cancer: results of the Shanghai Breast Cancer Study. International Journal of Oncology. 2000; 87: 295 – 300. 17. Hartman LK, Sellers TA, Frost MH, et al. Benign breast diseases and the risk of developing breast cancer. New England Journal of Medicine. 2005; 353(3): 229 – 36. 18. Collins L, Baer HD, Tamimi RM, et al. The influence of family history on the risk of developing breast cancer in women with biopsied benign breast disease. Oncological diseases. 2006; 107: 1240 – 7. 19. Worsham MD, Abrams D, Raju U, et al. Incidence rate of breast cancer in a group of women with benign breast disease. 2007; 13(2): 115 – 21.
Information
III. ORGANIZATIONAL ASPECTS OF PROTOCOL IMPLEMENTATION List of protocol developers indicating qualification data: Nurgaziev K.Sh. Doctor of Medical Sciences, Director of the Kazakh Research Institute of Oncology and Radiology Mukhambetov S.M. Candidate of Medical Sciences, Mammologist, Kazakh Research Institute of Oncology and Radiology Reviewers: Head. Department of Oncology AGIUV Doctor of Medical Sciences Baltabekov N.T.
Indication of absence of conflict of interest: none. Indication of the conditions for reviewing the protocol: review of the protocol 5 years after its entry into force and/or when new diagnostic/treatment methods with a higher level of evidence become available.
https://youtu.be/wLpCsKhMe_A
Fibroadenoma of the breast
FIBROADENOMA IS A BENIGN HORMONE-DEPENDENT TUMOR OF THE BREAST, CHARACTERIZED BY FOCAL EXCESSIVE PROGRESS OF FIBROUS AND Glandular TISSUE.
In the International Classification of Diseases (ICD-10), fibroadenoma is classified as a benign tumor of the mammary gland (D24). However, some scientists believe that fibroadenoma is a consequence of hyperplasia of individual lobules and should not be classified as true tumors. To establish a diagnosis of breast fibroadenoma , a clinical examination, technical imaging (ultrasound or mammography) and fine-needle biopsy are sufficient. Such a triple test gives 99% confidence in the quality of the process.
Breast fibroadenomas are detected in every fifth woman throughout her life, but the peak incidence occurs at 20-30 years of age. In young women, a multiple form of the disease is more common; large fibroadenomas (up to 20 cm) are typical for adolescents. During menopause, tumor growth stops or decreases markedly. During pregnancy, the process can progress quickly.
Causes of fibroadenomas
In most cases, the appearance of breast fibroadenomas is associated with hormonal imbalances, in particular, with an increase in estrogen levels during the formation of the menstrual cycle. Hormonal imbalance can also be a consequence of pathology of the thyroid gland or ovaries.
Fibroadenoma on mammography
Despite numerous studies on this problem, clear reasons for the development of the tumor have not been identified to this day. Risk factors include family history (breast tumors in maternal relatives), various menstrual irregularities, prolonged stress and poor environmental conditions.
Causes of the disease
The causes of this disease are not known. Specialists from different fields give different answers to the question of the etiology of the disease. Some believe that this disease may be traced back to psychological problems in women. The branch that studies this aspect is called psychosomatics.
Traditional mammology suggests that risk factors are:
- general hormonal disorders (obesity, diabetes);
- diseases of the female genital area that cause disturbances in the concentration of sex hormones in the blood;
- abuse of OK;
- multiple and frequently repeated abortions;
- chest injuries;
- refusal to breastfeed;
- pregnancy after 35 years;
- STDs and chronic inflammatory processes of the pelvic organs;
- bad habits;
- liver diseases.
Most likely, even an experienced mammologist will not answer why you have fibroadenoma.
Fibroadenoma of the breast
FIBROADENOMA IS A BENIGN HORMONE-DEPENDENT TUMOR OF THE BREAST, CHARACTERIZED BY FOCAL EXCESSIVE PROGRESS OF FIBROUS AND Glandular TISSUE.
In the International Classification of Diseases (ICD-10), fibroadenoma is classified as a benign tumor of the mammary gland (D24). However, some scientists believe that fibroadenoma is a consequence of hyperplasia of individual lobules and should not be classified as true tumors. To establish a diagnosis of breast fibroadenoma , a clinical examination, technical imaging (ultrasound or mammography) and fine-needle biopsy are sufficient. Such a triple test gives 99% confidence in the quality of the process.
Breast fibroadenomas are detected in every fifth woman throughout her life, but the peak incidence occurs at 20-30 years of age. In young women, a multiple form of the disease is more common; large fibroadenomas (up to 20 cm) are typical for adolescents. During menopause, tumor growth stops or decreases markedly. During pregnancy, the process can progress quickly.
Causes of fibroadenomas
In most cases, the appearance of breast fibroadenomas is associated with hormonal imbalances, in particular, with an increase in estrogen levels during the formation of the menstrual cycle. Hormonal imbalance can also be a consequence of pathology of the thyroid gland or ovaries.
Fibroadenoma on mammography
Despite numerous studies on this problem, clear reasons for the development of the tumor have not been identified to this day. Risk factors include family history (breast tumors in maternal relatives), various menstrual irregularities, prolonged stress and poor environmental conditions.
The tumor is represented by a clearly limited node of dense elastic consistency. On section, it is most often whitish with noticeable lobulation. The size of most fibroadenomas does not exceed 3 cm, but giant nodes are also found. Histologically, the tumor is represented by the proliferation of two components - fibrous and glandular in different proportions. Long-existing fibroadenomas can become denser due to hyalinosis and calcification. In this case, as a rule, the size of the formation decreases, and calcifications appear in the structure. In large nodes, infarctions may occur as a result of circulatory problems. Leaf-shaped fibroadenomas are histologically characterized by increased cellularity; the malignant variant is characterized by invasive growth and an abundance of mitotic figures, which are signs of aggressive growth.
Attached files
| 1. (Benign_neoplasm_of the mammary gland.pdf) | read/download file |
Send Mobile application “Doctor.kz”
Looking for a doctor or clinic? “Doctor.kz” will help!
The free mobile application “Doctor.kz” will help you find: where to see the right doctor, where to get examined, where to get tested, where to buy medicine. The most complete database of clinics, specialists and pharmacies in all cities of Kazakhstan.
Approaches to the classification and treatment of fibrocystic mastopathy
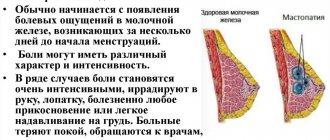
Fibrocystic mastopathy (FCM) is a pathology of the mammary gland, which is characterized by abnormal proliferation of the glandular or connective tissue component of the organ. This is accompanied by certain symptoms (pain in the mammary glands, their hardening, and less often, pathological discharge). Fibrocystic mastopathy is a benign disease, but its presence predisposes to the development of breast cancer.
- 1. Classification and information about the disease
- 2. Causes of occurrence
- 3. Diagnosis and treatment
Classification and information about the disease
In accordance with the domestic classification, diffuse and nodular forms of fibrocystic mastopathy are distinguished.
Both types of disease have similar symptoms, but with nodular disease, in addition to pain in the breast tissue, dense mobile nodules of various sizes are detected on palpation.
In the International Classification of Diseases, X revision, fibrocystic mastopathy is considered under the heading of benign mammary dysplasia (N 60).
Other categories in this section include:
| ICD-10 code | Disease |
| N 60.0 | Breast cyst (BC) |
| N 60.1 | Cystic breast |
| N 60.2 | Breast fibroadenosis (breast fibroadenoma excluded (code D 24) |
| N 60.3 | Breast fibrosclerosis (cystic mastopathy with epithelial proliferation) |
| N 60.4 | Dilatation of the mammary ducts |
| N 60.8 | Other benign breast dysplasias |
| N 60.9 | Benign breast dysplasia, unspecified |
Treatment of mastopathy: effective folk recipes How to protect yourself from mastopathy when menopause has begun? Fibrocystic mastopathy of the mammary gland: what it is, symptoms, treatment
Classification and information about the disease
In accordance with the domestic classification, diffuse and nodular forms of fibrocystic mastopathy are distinguished.
Both types of disease have similar symptoms, but with nodular disease, in addition to pain in the breast tissue, dense mobile nodules of various sizes are detected on palpation.
In the International Classification of Diseases, X revision, fibrocystic mastopathy is considered under the heading of benign mammary dysplasia (N 60).
Other categories in this section include:
| ICD-10 code | Disease |
| N 60.0 | Breast cyst (BC) |
| N 60.1 | Cystic breast |
| N 60.2 | Breast fibroadenosis (breast fibroadenoma excluded (code D 24) |
| N 60.3 | Breast fibrosclerosis (cystic mastopathy with epithelial proliferation) |
| N 60.4 | Dilatation of the mammary ducts |
| N 60.8 | Other benign breast dysplasias |
| N 60.9 | Benign breast dysplasia, unspecified |
Clinic of the disease
Most often, the formation is detected during palpation examination by a gynecologist, with the size of the tumor being about 1-5 cm (largest diameter). Usually this is a single formation with an elastic consistency, movable (it can be easily moved with your fingers). If the neoplasm is quite large, it can be seen visually.
Subjective symptoms may be absent or mild. They boil down to thinning of the skin over the tumor, and discomfort in this area when the tumor reaches a significant size.
In the postmenopausal period, this formation regresses. Involuting fibroadenoma turns into a small calcified nodule. Lumps with calcifications usually do not cause discomfort; they can move freely and are not fused to the surrounding tissues.
Diagnosis and treatment
If you experience chest pain, you should consult a doctor (mammologist, oncologist) and undergo an examination. In Russia, fibrocystic mastopathy is treated by oncologists, not gynecologists, despite the fact that it is a benign pathology. List of necessary examinations:
- examination and palpation of the breast;
- ultrasound examination of the breast;
- mammography;
- puncture biopsy.
In order to visualize changes in the mammary gland, an ultrasound examination (before 40 years) or mammography (after 40 years, and, if necessary, at an earlier age) is performed. When nodular formations are identified, it is recommended to puncture them under ultrasound control with examination of the obtained material. This is necessary to exclude the malignant nature of the neoplasm.
Treatment of the disease depends on the form. For nodular mastopathy, surgical intervention is performed to remove the formations. For the diffuse form, conservative treatment is indicated. The basis of therapy is the use of hormonal drugs. The most popular at the moment are products for external use based on natural progesterone (Progestogel, Crinon).
Recovery postoperative period
Carrying out surgery on the mammary gland due to the occurrence of fibroadenoma is considered the simplest among other surgical interventions.
The procedure takes no more than an hour. Complications after removal almost never occur. Bed rest is not required. The patient remains in the hospital for only a few hours, less often – up to two days.
The applied sutures are removed after 9-12 days. In a situation where a cosmetic suture is used, it resolves on its own. There are usually no visual defects left, the only exception being the removal of an adenoma that is too large.
During the postoperative period, a woman usually does not experience any pain.
However, doctors note the risk of relapse of the disease even after removal of the tumor. In addition, cysts may appear.
Fibroadenoma of the mammary gland, ICD code 10
Peak detection occurs at 20-30 years of age. However, asymptomatic fibroadenoma can be first detected at a much later age during a preventive examination.
There are mature fibroadenomas (with a dense capsule, dense elastic consistency, slow growth or not growing at all), and immature fibroadenomas (soft elastic consistency, tendency to progressive growth).
Mature fibroadenomas occur mainly at the age of 20-40 years. Immature fibroadenomas are observed in girls going through puberty. These fibroadenomas can sometimes degenerate on their own without any treatment after the establishment of a regular menstrual cycle.
Most often, fibroadenoma is detected as a single breast tumor, but there are frequent cases of multiple fibroadenomas, which can be localized simultaneously in both mammary glands.
Fibroadenoma has a characteristic clinical picture:
- Upon examination, a large fibroadenoma can be visually determined as a subcutaneous tumor-like formation of the mammary gland
- On palpation, it is defined as a clearly demarcated, movable tumor of dense elastic consistency from 1 to 5 cm in its greatest dimension.
- It is usually located outside the areolar zone. The most common location is the upper outer quadrant of the mammary gland.
Causes of formation of a benign tumor
The insidiousness of the disease lies in determining the cause. Doctors have not yet identified a clear root cause of the pathology. However, there are hypothetical reasons that provoke the development of fibroadenoma. They can be divided conditionally into external and internal.
Internal causes of breast adenoma
- Hormonal imbalance, in which the amount of estrogen significantly exceeds the permissible norm. This can also occur during pregnancy and puberty.
- The presence of various types of pathological conditions:
- liver diseases;
- diseases of the endocrine system, thyroid gland;
- pathologies of the ovaries and adrenal glands;
- problems with the pituitary gland;
- diabetes mellitus, obesity;
- gynecological problems of various forms, including menstrual irregularities.
External reasons
- Bad ecology.
- Nervous stress or exhaustion.
- Regular or severe stress.
- Passion for solariums and prolonged exposure to the sun.
- Frequent showers or baths with a temperature exceeding 37.5 degrees.
- Breast injury, improper massage or heat exposure.
Reasons that can provoke the occurrence of pathology also include:
- hormonal therapy;
- frequent abortions;
- incorrect or irregular use of oral contraceptives or the presence of a hormonal-based intrauterine device;
- incorrectly selected oral contraceptives;
- lack of pregnancy (the cause of fibroadenoma during menopause).
Some doctors are inclined to argue that hereditary reasons also play a role. However, there is no concrete evidence that the tendency to do this is transmitted at the genetic level. The only caveat: the occurrence of fibroadenomas can occur in women who have a family history of cancer patients. Most often, in such cases, leaf-shaped fibroadenoma is diagnosed.
Diagnosis and differential diagnosis of breast fibroadenoma
To establish an accurate diagnosis in the vast majority of cases, the following methods are sufficient:
- Clinical examination and palpation of the breast
- Ultrasound of the breast
- Fine needle aspiration biopsy of the tumor followed by cytological examination
If there is doubt about the diagnosis, X-ray mammography, core needle biopsy, or therapeutic and diagnostic sectoral resection of the mammary gland with intraoperative histological examination can be used.
Differential diagnosis should be carried out with the following conditions:
Prevention of breast diseases
Propaganda for the prevention of breast diseases occupies a priority place in working tactics among gynecologists and oncologists. This should include social advertising, various medical brochures, preventive conversations with patients at appointments, increasing the popularity of a healthy lifestyle, as well as the approval of World Breast Cancer Day.
To minimize the risk of developing the disease, and not to miss it at an early stage, you should adhere to the following rules:
· refusal of smoking and drinking alcohol;
· treatment of acute diseases, as well as prolongation of the remission phase of chronic ones;
· undergoing preventive examinations, especially over the age of 35;
· performing independent palpation of the mammary glands at home at least once every 4-6 months.
Treatment and medical tactics
The doctor’s tactics in the treatment of fibroadenoma are determined by two main properties of fibroadenoma:
- Fibroadenoma does not respond to conservative treatment
- Fibroadenomas are not capable of malignancy (except for leaf-shaped fibroadenoma, which in 10% of cases can degenerate into breast sarcoma)
Based on these two facts, the indications for surgical treatment of breast fibroadenoma are:
- Leaf-shaped structure of fibroadenoma (absolute indication)
- Large sizes (over 2 cm), or sizes causing a cosmetic defect
- The patient's desire to remove the tumor
- Rapid tumor growth
In other cases, after morphological confirmation of the diagnosis, fibroadenoma can be observed. For the surgical treatment of fibroadenoma, enucleation of the tumor from the para-areolar approach is currently most often used.
Complications and consequences
After surgical treatment of fibroadenoma, suppuration is possible due to low immunity, so the woman is prescribed a course of antibiotics, as well as immunomodulating agents.
The main danger that warns a woman after surgical removal of fibroadenoma is its recurrence. To avoid relapse, which according to statistics occurs in 15% of cases, it is necessary to complete the course of treatment, eliminate concomitant diseases if possible and correct the functioning of the ovaries.
If there was a small lump in the breast before pregnancy that was not diagnosed, high levels of hormones can cause it to grow rapidly. In the leaf-shaped form, tumors often degenerate into cancer during pregnancy. Therefore, delayed surgery may affect the woman's health.
If the fibroadenoma is not removed before the baby is born, the blocked ducts will lead to stagnation of milk and lactostasis, which in turn can cause infectious mastitis.