Pathologies of the digestive tract have similar symptoms and first signs. To identify a specific disease and begin treatment, it is necessary to undergo diagnostics. Tests for pancreatitis, ulcers or gastritis include urine, feces, blood, and, in some cases, saliva. Based on the results, the gastroenterologist judges the presence of a particular diagnosis, the degree of severity and other factors.
Pancreatitis, gastritis or ulcers often lead to undesirable consequences. Testing for gastrointestinal disorders is a mandatory part of treatment. Timely diagnosis of pathology reduces the risk of complications. Therefore, if you are predisposed to this kind of disease, doctors advise regularly taking the necessary tests.
General blood analysis
If the doctor suspects the presence of an inflammatory process in the patient’s body, the first step is to do a general blood test. It is worth noting that it can only indicate the presence of inflammation, but does not determine the diagnosis.
Data that should not be changed without attention:
- Leukocyte level. An upward shift in this indicator indicates pancreatitis or cholecystitis. Elevated white blood cells also mean the presence of inflammatory processes in the kidneys or urinary system. The normal level of leukocytes in the blood is considered to be from 7.5 to 8.5.
- Erythrocyte sedimentation rate. The norm varies from 12 to 16. It should be noted that in women, even the normal value may be exceeded by several units. A noticeable increase in level indicates the presence of inflammation.
- Hemoglobin. The hemoglobin level is different for men and women. For the former it is 130-170 units, for the latter it is 120-140. If the blood test shows an indicator significantly lower than normal, it means diseases of the digestive tract in an advanced stage, for example, with bleeding.
Blood test results take several hours to prepare.
It is recommended to take a blood test for stomach ulcers, pancreatitis and other diseases of the digestive system in the morning. Before the manipulation, you should not eat any food, as this leads to a change in the results.
Biochemical research
A biochemical blood test for pancreatitis is necessary for a more detailed study of its composition.
Let's take a closer look at what indicators are used to determine inflammation of the pancreas or gastric mucosa:
- Sugar level. Many people believe that an increase in blood sugar levels exclusively indicates diabetes. In fact, this opinion is wrong. This indicator can also be increased with pancreatitis. We are talking about a slight increase in level (for example, 0.3 units more). The norm is 5.5-5.8 units.
- Cholesterol levels. The normal rate varies from 6.4 to 6.8 units. A high level of the substance may indicate the presence of diseases of the digestive tract. These include cholecystitis, inflammation of the pancreas, inflammation of the gastric mucosa, and gastric ulcers.
- Amylase. This indicator has no clear boundaries. Many factors influence changes in amylase levels in the blood. The norm is 30-100 units. If the level is significantly elevated, we are talking about an exacerbation of the disease of the digestive system. Too low an indicator indicates problems with the bile ducts.
- Globulin. The only signal that may indicate the presence of inflammation of the pancreas is too low a level in the blood. The norm is considered to be from 8 to 15 units. If there is an illness, the level drops to 2-3 units.
Biochemistry is given on an empty stomach. For this reason, blood tests for gastritis, ulcers and other gastric pathologies are taken in the morning.
Causes of anemia in gastric ulcers
The disease disrupts the process of iron absorption.
Gastric ulcer is accompanied by anemia for two reasons:
- An ulcer almost always develops against the background of gastritis, which is accompanied by impaired absorption of iron and vitamins (cyanocobalamin and folic acid), which are responsible for the formation of red blood cells. Their percentage in the blood decreases, which causes anemia.
- When a peptic ulcer worsens, bleeding begins from mucosal defects. In this case, tests will show a decrease in hemoglobin and red blood cells, and the stool may become dark in color (melena). This is a dangerous condition because blood loss can be large.
Urine examination
Urinalysis for pancreatitis is an informative diagnostic measure that tells about many features of the disease. Not to mention studying urine in a laboratory, a person himself is able to notice something wrong in a portion of natural liquid.
If you suspect pancreatitis, you should pay attention to the following:
- First, the shade of urine. Normally, it should be light, with a slight yellowish tint. The main thing is that the urine should be clear. If the liquid is saturated yellow or even dark in color, this is a signal that there are diseases of the digestive tract (especially pancreatitis) or problems with the urinary tract.
- Secondly, the presence of clots. If bright yellow flakes of impressive size are observed in the urine, this indicates a high level of bilirubin. Also, this symptom may be a signal of the presence of cancer of the pancreas or stomach.
- Thirdly, the composition of urine. If, after laboratory diagnostics of urine, the presence of sugars in the liquid is detected, this means an advanced stomach ulcer, acute pancreatitis or cholecystitis. Normally, this substance should not be found in urine. The same applies to hemoglobin.
If at least one of the indicators does not correspond to the norm, the doctor orders a repeat test.
Collection of analyzes
Urine should be collected immediately after waking up. It is necessary to use a special, disinfected container. Tests for gastritis may be normal, but in the presence of an ulcer, pancreatitis or cholecystitis, the main indicators are often overestimated.
Before taking a urine test, the patient must carefully prepare, namely, a few days before the procedure, refuse junk food. This includes fatty and spicy foods and alcohol. It is recommended to eat bland food and drink a lot of water these days.
Careful preparation for testing is necessary so that the results are as truthful as possible.
Nutrition rules
How to increase hemoglobin to normal
If you have a stomach ulcer, your doctor will tell you in detail. This disease requires following a certain diet, but you need to try to saturate your diet with foods that will help get rid of anemia and improve the general condition of the body.
There is a list of foods that contain high levels of essential iron. If you use them regularly and correctly, your indicators will return to normal and your condition will improve significantly.
- Beef is the undisputed leader among other types of meat in terms of iron content. Pork and rabbit meat do not come after. Considering that if you have a stomach ulcer, eating spicy, fried, or smoked foods is strictly prohibited, it is best to cook meat in the oven or slow cooker with minimal addition of salt and spices. Particular attention should be paid to beef liver, it is a hematopoietic organ and can increase hemoglobin. It is better to consult your doctor about possible methods of preparing it.
- To raise hemoglobin levels, it is also recommended to regularly consume beets or freshly squeezed beet juice. The course of such treatment is at least 2 months, during which you need to eat 200 g of cooked beets or drink 30 g of the juice of this vegetable. It should be remembered that beets have a laxative effect, so they may not be suitable for everyone. The vegetable is easy to cook in the oven or slow cooker.
- All the iron contained in buckwheat porridge is quickly and easily absorbed. If there are no contraindications to the use of this product, then it should be introduced into the daily diet, adding a little salt and oil. Sometimes even such supplements are contraindicated. You can add a slice of beetroot and a steamed beef cutlet to the buckwheat porridge. This set of products is ideal for eliminating anemia.
- To normalize the level
hemoglobin, doctors advise eating apples every day. The most iron is in those fruits that quickly darken when cut. If the doctor has forbidden you to eat fresh fruits, you can cook them in the oven, adding a small amount of cottage cheese and honey. This dessert will speed up your recovery.
- Also, in the absence of contraindications, you can eat a small amount of dark chocolate daily. A fourth of the tile will be enough.
- A lot of useful iron is contained in pomegranates and its juice. You need to consume such a tasty product very carefully and only after your doctor allows it, otherwise there is a risk of causing a worsening of the condition.
- Along with apples, it is also recommended to eat several walnuts daily. You can add a teaspoon of honey to them, this will improve the absorption of nutrients.
You should also remember that the substances contained in coffee and tea do not allow protein to be fully absorbed, so it is best to wash down your food with clean water or fresh vegetable juices, which are recommended by your doctor.
Saliva examination
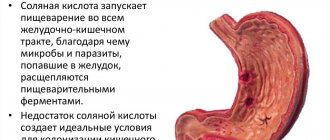
A person's saliva is taken to test for the presence of a substance called amylase.
Depending on the specific disease, as well as its severity, the indicator is present or absent altogether.
Only a qualified specialist can find out whether the test results are normal and determine pancreatitis in a patient.
How to raise hemoglobin using folk remedies - 7 proven recipes
Naturotherapist, phytotherapist
Hemoglobin is a complex protein that delivers oxygen to every cell of the body and removes carbon dioxide. For the synthesis of hemoglobin, a large set of proteins, vitamins and microelements is required.
Due to various failures, the adequate process of hematopoiesis may be disrupted, which will lead to a reduced concentration of hemoglobin in the blood and the development of disorders caused by hypoxia of organs and tissues.
Many people ask whether there are folk remedies that are effective in increasing hemoglobin (yes, they exist). And also whether they can replace drug treatment (no, they cannot). See below for details.
Why might hemoglobin be reduced?
Before talking about the effectiveness of various remedies, it is important to understand the causes of the condition.
The main reason for low hemoglobin levels in the body is anemia.
There are many reasons for the development of anemia, but in 90% of cases the cause is a lack of important elements necessary for the synthesis of hemoglobin - iron, folic acid, cyanocobalamin (vitamin B12).
The remaining 10% is due to various hereditary diseases and intoxications.
The main reasons include:
- Insufficient intake of iron or B vitamins, folic acid from food.
- Diseases of the stomach and duodenum, accompanied by atrophic changes in the mucous membrane.
- Metabolic pathologies with disturbances in fermentation and iron transport.
- Chronic blood loss, which occurs in a wide range of pathologies: from peptic ulcers to dysfunctional uterine bleeding.
- Haemorrhoids.
- Intoxication (including chronic). The most common causes of anemia are: tobacco smoke, heavy metal salts.
- Oncological diseases. In this condition, hematopoiesis is inhibited.
- Helminthic infestations.
Separately, it should be noted the prevalence of pathology. According to scientists from the USA, the incidence of anemia in adult women and men is 25%. Approximately 70% of patients learn about this diagnosis by chance during examination for other pathologies or during professional examinations.
Is traditional medicine effective?
Almost all herbal folk remedies are insufficiently effective.
As we have already found out, in 90% of cases, anemia is caused by a lack of iron, folic acid or vitamin B12. In turn, 100 g of any plant material contains a maximum of 9-11 mg of iron or 0.05 mcg of vitamin B12 or 90-100 mcg of folic acid. And, for example, to treat iron deficiency anemia you need about 150-300 mg of iron per day.
It turns out that you need to completely switch to a different diet, limit yourself to other essential vitamins and microelements, but even this will be insufficient due to the different bioavailability of each plant, which is also influenced by the anatomical and functional state of the gastrointestinal tract.
Sources: https://1zhkt.ru/yazva/kak-povysit-gemoglobin.html https://gemoglobin.top/kak-povysit-gemoglobin/ https://travnik.online/cardiovascular/blood/podnyat-gemoglobin-narodnymi -sredstvami.html https://otvetprost.com/616-kak-povysit-gemoglobin-rebenku.html
Additional diagnostics
In addition to tests for gastritis of the stomach, peptic ulcer or pancreatitis, the patient is recommended to undergo the following types of studies:
- CT scan. It is necessary to clearly examine the contour of a particular formation in the digestive system. Most often, this diagnosis is carried out when a tumor is suspected.
- Biopsy. The examination involves taking biomaterial. When a tumor is found, the doctor needs to pinch off a microscopic piece of it (or a piece of an organ) for examination. The procedure will show the nature of the formation: benign or malignant.
- Ultrasound diagnostics. Mainly used to study pancreatitis. Using ultrasound, the doctor identifies the presence of inflammation of the pancreas, its size and other individual characteristics.
- Fibrogastroscopy. Recommended for examining the gastric mucosa. Using this manipulation, the presence of ulcers on the surface of the digestive organs is diagnosed, and inflammation can be seen. The procedure is the most informative, therefore it is used more often than others when gastrointestinal diseases are suspected.
In addition to laboratory and instrumental types of diagnosis of pancreatitis, the doctor asks some questions: are there pains in the abdomen or intestines, with what intensity, when did the discomfort begin, and the like.
Do not forget that any analysis or type of diagnosis of gastrointestinal diseases is carried out exclusively on an empty stomach. This is because the products seriously interfere with the examination and distort the results. At the first alarming symptoms of pancreatitis or another disease of the digestive system, go to the hospital and get the necessary tests. Diseases of the food tract are identified at an early stage, and sometimes you can get by with a short course of medications.
Signs of anemia
A dangerous decrease in iron concentration in the blood can be recognized by pronounced symptoms. If they appear, you should consult a doctor to clarify the diagnosis and prescribe treatment. Each patient exhibits signs of anemia individually. Usually several symptoms are present at the same time. However, they gradually intensify in the absence of treatment.
The first signs of a lack of iron-containing protein:
- slow metabolism;
- general malaise;
- weakness;
- fast fatiguability;
- urinary disturbance;
- fragility and dryness of the nail plates, hair loss, peeling of the skin;
- dyspnea;
- swelling;
- pallor of the skin.
With a sharp drop in the hemoglobin level, in addition to the above symptoms, the following symptoms develop:
- dizziness;
- fainting;
- inability to navigate in space;
- hallucinations;
- noise in ears.
If the deviation from the norm is small, anemia does not cause concern, contributing to the rapid development of the underlying disease. But it is impossible to restore hemoglobin levels on your own. Therefore, medical assistance is necessary to correct the level of iron-containing protein. With prolonged development of the disease, internal organs suffer. Diseases of the heart and blood vessels, digestive organs, and urinary system develop. But if a low hemoglobin concentration is diagnosed in a timely manner, it can be quickly eliminated. At the same time, it becomes possible to identify hidden diseases of the digestive system.
Iron deficiency provokes changes in the structure and shade of the tongue. It takes on a bright red color. A person’s sense of smell is impaired and unusual taste preferences appear. Because of this, there is a craving for non-food products - chalk, clay, earth. Some patients begin to like the smell of acetone. The nails of those suffering from anemia often break, peel, become ribbed and become stained. In some people, a lack of iron-containing protein provokes atrophic changes in the mucous membrane of the esophagus and pharynx.
Symptoms of peptic ulcer.
How can you find out if you have a stomach ulcer if you are currently unable to see a specialist? Stomach ulcers can be identified by the symptoms inherent in the disease. There are seven main signs that will help you identify a stomach ulcer yourself.
What symptoms bother a patient with a peptic ulcer? Let's look at the clinical picture of the disease.
The leading signs of the disease are pain and dyspeptic (heartburn, sour belching, nausea, vomiting) syndrome.
Diagnostics and examination methods
Ultrasound is one of the methods for diagnosing peptic ulcer disease.
Ultrasound examination (ultrasound) is performed in the morning on an empty stomach. Examination using the FGDS method guarantees an accurate diagnosis in 90% of cases.
The method allows you to see the location of the lesion, determine the size and nature of the ulcer. It is possible to take tissue for a biopsy.
If the FGDS procedure, which has many contraindications, cannot be done for any reason, an X-ray examination is performed. Its accuracy is 80%. The most commonly used agents are contrast agent and air.
Diagnosis is carried out using tests - invasive (examination of a tissue particle for biopsy) and non-invasive - these are tests of urine, blood, saliva and exhaled air. Non-invasive tests are as follows:
- A shortened breath test is based on the fact that the bacterium Helicobacter pylori can decompose urea. The patient takes two breath samples on an empty stomach. Then he has breakfast and drinks a special solution. Every 15 minutes for an hour, samples of exhaled air are checked using equipment provided for these purposes. The accuracy of bacteria detection is very high.
- Immunological test. It is based on the detection of antibodies in the immune system's reaction to the bacteria Helicobacter pylori.
- Quick stripped down. Examination of tissue particles using a special indicator.
- Bacteriological test. Its accuracy is 100%. For this purpose, special equipment and expensive reagents are used. The study lasts 7 days.
Major and minor symptoms
Among the main signs of ulcerative anemia are:
- Dizziness due to lack of oxygen reaching the brain. This condition is caused by a decrease in the number of cells carrying it.
- Increased heart rate (HR). The heart tries to compensate for the lack of blood.
- Reduced blood pressure. Despite the efforts of the heart muscle, the volume of circulating blood is insufficient.
- Weakness and pallor, which may be followed by loss of consciousness.
- Metallic taste in the mouth.
- Flickering of flies before the eyes, which indicates hypoxia of the optic nerve.
Return to contents
Anemia due to blood loss from an ulcer in the stomach is accompanied by:
- Vomiting contents resembling coffee grounds. Vomit acquires this color due to the influence of stomach hydrochloric acid on the blood with the formation of hydrochloric acid hematin. Fresh blood is mixed with it.
- Black stool (melena). Mechanism: conversion of hemoglobin into hemin under the influence of hydrochloric acid of gastric juice and various gastrointestinal enzymes.
- Pain in the epigastric region.