What is condyloma?
Condylomas are flesh-colored warts that appear on the genitals and anus. These growths are also found on other parts of the body, but much less frequently. According to research, the occurrence of genital warts (condylomas) is promoted by the DNA-containing human papillomavirus, whose presence in the body can go unnoticed for a long period of time.
Regardless of the fact that condylomatosis is classified as a sexually transmitted disease, this is not the only method of infection - infection can occur through household contact, as well as during natural childbirth. Condylomas in women require immediate and high-quality treatment; their formation in the cervical area leads to a precancerous condition.
Diagnostics
A girl may suspect that she has genital warts by comparing their appearance with the images below. If any growths occur in the genital area, you should consult a gynecologist. Diagnosis of genital warts begins with collecting complaints and a brief conversation.
The gynecologist asks the patient about her life history, the number of sexual contacts, especially unprotected ones, and identifies risk factors. The specialist then examines the affected area, genitals and anus. After the external examination, it’s time for a gynecological examination.
Examination in the mirrors allows you to see formations in the vagina, on the outer part of the cervix, and determine their nature. The gynecologist takes smears for microflora and oncocytology. Colposcopy is performed, which helps to identify flat condyloma, a violation of the surface of the cervix.
A special study to search for papillomavirus and clarify its serotype is the PCR (polymerase chain reaction) method. Blood or biomaterial from the site of the lesion is taken for analysis, after which the DNA of the virus is detected in the collected material using special equipment.
PCR is the main and most informative method for diagnosing genital warts. A study is also carried out to determine the amount of antibodies to the virus in the patient’s blood, an analysis for HIV and hidden genital infections.
Reasons for the appearance of formations in women
According to statistics, the papilloma virus lives in the body of more than 15% of women, but it does not always manifest itself. However, representatives of the fair sex, its carriers, are capable of transmitting the infection to people with whom they are in close contact. Infection with the virus occurs both through traditional sexual contact and through oral or anal sex. Because of this, condylomas form not only inside the vagina, but also on the labia, face, tongue, neck, mouth and even on the chest.
In a household way, the virus spreads through discharge from condylomas. The presence of wounds or even microcracks on the skin or mucous membranes facilitates the penetration of infection into the body. During childbirth, natural transmission of the virus from mother to child is possible if genital warts are located directly on the walls of the vagina.
- Papillomas on the body - causes of appearance, treatment methods and how to stop growth
- Condilin - instructions for use, indications, composition, side effects, analogues and price
- HPV types 16 and 18 in women - causes, symptoms, necessary tests and treatment
When a woman is a carrier of the virus, there is also the possibility of becoming infected herself, which is increased by a weakened immune system. What factors influence decreased immunity? The reasons that create a gap in the body’s defense mechanism include:
- Stress (physical and psycho-emotional), nervous breakdowns.
- Diets, since at this time the body suffers from a lack of essential substances that are used in the process of synthesis of antibodies that protect it.
- Postpartum period. The process of childbirth itself is a serious stress for a woman and her body, but a newborn baby also requires constant attention, as a result of which the new mother is constantly exposed to overwork.
- Self-medication, abuse of drugs, the action of which leads to disruption of the body's microflora and the state of the immune system.
The danger of condylomas for men and women
To understand how dangerous a particular type of growth is, you need to understand the characteristics of each.
In today's article we will look at candilomatosis (genital warts in women), treatment, photos and prevention.
The predominant route of transmission of HPV is sexual.
If the immune system is in good condition, the virus can remain inactive for some time, and when the body weakens, it can develop activity.
- The genital area: pubis, groin, female genital organs, that is, vulva, vagina, labia minora.
- The anus is the anogenital region.
- Internal warts can form on the walls of the urethra and cervix.
In rare cases, condylomas occur on other mucous membranes of the female body, for example, inside the mouth or oronasal cavity.
Condylomas acuminata
Most often, HPV is transmitted through unprotected sexual contact with carriers of the virus. Sometimes the method of transmission is through household contact, for example, through close contact in the absence of personal hygiene rules.
In addition to the entry of the HPV bacterium into the female body, its activation also requires the presence of a number of pathogenic factors, under the influence of which the immune system is unable to defeat the disease. Among them:
- unhealthy diet and unhealthy lifestyle;
- taking strong medications;
- pregnancy and postpartum period;
- stress and nervous shock;
- other acute and chronic inflammatory processes or infectious diseases that weaken the body.
Such papillomas are sometimes called exophytic, they appear on the skin, resembling a small nodule or papilla, their color is most often close to flesh-colored, sometimes has a slightly pinkish tint.
After diagnosis, exophytic condylomas can be treated with various methods, but most often a specialist prescribes their removal. This is due to the fact that most of the bacteria are located inside the condyloma and in the tissues around it, which, if necessary, can also be cut off during surgery.
In female representatives, genital warts (see photo) usually form around the clitoris, anus, at the entrance to the urethra, on the mucous membrane of the labia minora and majora. Sometimes this type of condylomas in women is localized on the walls of the vagina or urethra, as well as on the skin of the groin areas, thighs and buttocks.
As soon as its protective forces are weakened, the HPV becomes active, “bores” the surface layer of the epithelium - the epidermis and comes out in the form of condyloma.
Among the surgical methods of treating condylomas, the following methods are most in demand:
- Laser destruction. With this method of exposure, condylomas are removed using a surgical laser. Under the influence of laser radiation, the tissue of the skin outgrowth is destroyed. At the site of the condyloma, a small wound is formed, covered with a crust. After a short time, healthy tissue is restored underneath. The method is safe and painless, but expensive, since special equipment is used for the operation.
- Thermocoagulation. This method of treating epithelial warts and growths in women involves burning the tumors using a special device. During this procedure, the woman is given local anesthesia, as the method is quite painful. It is important that thermocoagulation was carried out only by a highly qualified gynecologist, since the slightest contact with healthy tissue by the device leads to the formation of deep scars.
- Chemical destruction. The essence of this method is that condylomas are treated with drugs that can destroy tumor tissue. Such drugs are very effective, most of them contain nitric acid. Even when removing multiple and overgrown condylomas, only two or three procedures are enough to get rid of them completely. After the procedure, the tissues heal quickly, leaving no scars on the skin. If the medicine accidentally gets into healthy tissue, such drugs do not cause any harm. The method is quite inexpensive, quite reliable, effective and safe.
- Radiosurgical method. This method of treating condylomas, like the previous one, is a very expensive procedure. The method of radio wave surgery is characterized by directing a beam of high-frequency waves to the affected area, with the help of which a tissue incision is made and the condyloma is removed along with its stem. The operation is very gentle and leaves no marks on the skin after it is performed.
- Cryodestruction. With this method, condylomas are cauterized with liquid nitrogen. Under the influence of low temperatures, the tissues of the formations freeze and fall off, leaving clean skin in their place. This method is considered one of the most inexpensive; it does not require special equipment or expensive medications. At the same time, the method is not safe; it requires great care and experience from the doctor, since when liquid nitrogen comes into contact with the skin, it causes burns to healthy tissues.
In cases where the condyloma is located in the urethra and is located below 1 cm from its external opening, it can only be removed using a urethroscope. Using the device, the doctor examines the canal along its entire length and treats the condyloma with a special drug that destroys it.
To treat genital warts, drugs can be used to necrotize the tissues of the formation, but they should not be acidic. Such products as Condiline, Condiline are suitable. The drug is applied exactly to the condyloma. Removal in this way is quite dangerous - it is difficult to apply the drug without affecting healthy areas.
DETAILS: Barn mushrooms: photos and description
Despite the fact that treatment is carried out at home and independently, the patient must be examined by a doctor before treating genital warts and after the procedure. During the procedure, unpleasant side effects are possible: pain, burning, redness. There are also contraindications - during pregnancy, genital warts cannot be removed by this method, and those who are planning to conceive should postpone pregnancy for six months.
Local treatment methods include injections of interferon, which is injected into the area of condyloma formation. However, experts do not recommend using this method, since its effectiveness is controversial and the presence of side effects is high.
Genital warts can be treated not only with traditional methods, but also with folk methods, but only after the doctor allows it. Below we will look at the main methods of therapy.
- Eggs - you will need chicken eggs. In order to carry out the treatment, you do not need to take the whole egg, you only need the white. Break the egg and remove the yolk, then prepare the bandage. Gently soak it in the protein, then apply it to the affected areas and secure it with an adhesive plaster on top. You can use such lotions three times a day, each time for no more than 10 minutes. The duration of treatment depends on how quickly the formations disappear.
- Celandine - to treat with this plant you only need juice. It is not difficult to obtain, because immediately after cutting the plant, juice will begin to come out of it. They need to gently cauterize the condylomas several times a day. Try to ensure that the medicine gets exclusively on the affected area. Apply celandine until you see that the growths have disappeared.
- Iodine is the most popular treatment. The affected area is lubricated up to five times a day, but this must be done carefully so that healthy areas of the skin are not affected. Apply one coat of medicine, then wait until it dries before applying a second. The course of treatment lasts until the problem completely disappears.
As for the use of folk remedies, they can only be used if the growths affect the genital organs from the outside, because you will agree that applying lotions to the cervix is inconvenient and dangerous.
The human papillomavirus is widespread and highly contagious. More than half of sexually active people are infected with one or more strains of HPV. In the human body, HPV changes the pattern of tissue growth, which leads to diseases of the skin and mucous membranes (genital warts, warts, papillomas, dysplasia and cervical carcinoma).
The appearance of human papillomavirus infection and its further development is caused by a weakening of human immunity. This infection is characterized by an asymptomatic course; in many infected people it does not manifest itself in any way. Most people who are carriers of the corresponding strains of HPV do not develop genital warts. Factors that increase the risk of contracting genital warts include:
- previous STDs (chlamydia, gonorrhea, trichomoniasis, herpes, candidiasis, etc.);
- free sexual behavior (with frequent changes of sexual partners, through a partner who has previously had sexual contact with an HPV carrier);
- internal factors of the body (reduced immunity, lack of vitamins, exposure to stress);
- pregnancy;
- vaginal dysbiosis.
The male penis is a very delicate and tender organ. Any impact not only causes inconvenience, but can also seriously injure him. That's why
treatment of genital warts
and especially,
on the head of the genitals
prescribed and carried out only by a specialist.
- juice of celandine, young apples, dandelion, pineapple, aloe;
- propolis tincture;
- garlic or onion;
- Kalanchoe;
- rowan berry compress;
- egg white.
- use of antiviral agents and immunomodulators;
- use of liquid nitrogen;
- laser exposure to the skin;
- diathermocoagulation;
- radio wave treatment;
- electrocoagulation;
- excision;
- the use of cauterizing and mummifying drugs.
Types of condylomas in women (photo)
Viral condylomas in women come in various shapes and sizes. However, they often have the appearance of pinkish-gray skin outgrowths, the size of which reaches several millimeters. As a rule, at the initial stage, condylomas are located separately from each other, but with active reproduction, the cells of the growths merge, evolving into huge formations that are comparable in appearance to cauliflower. There are two types of condylomas in women:
- pointed;
- flat.
Pointed
Pointed (exophytic) condylomas in females usually form around the clitoris, anus, at the entrance to the urethra, on the mucous membrane of the labia minora and majora. Sometimes this type of condylomas in women is localized on the walls of the vagina or urethra, as well as on the skin of the groin areas, thighs and buttocks.
Flat
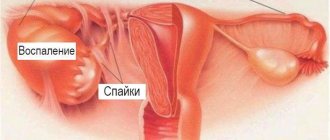
Flat (endophytic) condylomas form on the cervix and are almost impossible to see without a microscope. This feature makes them much more dangerous. Endophytic condylomas that are not detected and eliminated in a timely manner become the cause of cervical cancer. In this regard, you should undergo regular examinations with a gynecologist.
Where can genital warts be located?
The main route of transmission of papillomavirus is through sexual contact, so genital warts are localized in the corresponding areas.
For women this may be:
- labia majora and minora;
- clitoris;
- entrance to the vagina;
- the inner surface of the lower third of the vagina;
- perianal region;
- mucosa of the final sections of the large intestine and anus;
- external part of the urethra;
- skin of the perineum and inguinal folds;
- inner thighs;
- mucous surfaces of the oral cavity, larynx, esophagus.
In men, external manifestations are usually localized in the groin area, on the penis, the skin of the scrotum, and at the external opening of the urethra.
Symptoms and signs of the disease
As a rule, any condylomatous manifestations are local in nature. Condylomas formed around the anus are accompanied by itching and burning in this area, and also create a feeling of the presence of a foreign body there. Because of this, women with similar problems suffer around the clock from terrible discomfort caused by signs of condylomatosis.
For fused condylomas, which grow over much larger areas of the body, in addition to the above symptoms, fluid discharge is also characteristic. It has an unpleasant odor and brings discomfort due to the constant feeling of moisture. If the outgrowths are accidentally injured by clothing or during sexual intercourse, irritation and inflammation appear on the skin.
Endophytic (flat) condylomas are usually not accompanied by any symptoms; only in rare cases may mild vaginal discharge and itching in the genital area be observed. Genital warts are diagnosed by their specific appearance. But with flat representatives of the virus the situation is somewhat more complicated; they cannot be recognized with the naked eye. If you detect the slightest suspicious signs of the disease, you should consult an experienced doctor for a thorough diagnosis.
- Molluscum on the skin of a child: causes and treatment
- Papilloma on the genitals
- Cyst on the cervix - what is it, why is it dangerous. Treatment of cysts on the cervix
Forecast and consequences
Even if genital warts are successfully removed, complete cure of the disease is impossible. Therefore, persons infected with HPV must undergo preventive examinations by a gynecologist once every 6 months with mandatory blood tests and smears for oncocytology.
Genital warts in women, photos of which can help with self-diagnosis, may reappear. It is necessary to contact an obstetrician-gynecologist, even if the patient has an old treatment regimen. In the absence of adequate and timely therapy, complications of condylomatosis may develop.
The consequences of advanced disease include:
- Spread of neoplasms to healthy areas.
- Decreased local immunity, addition of STDs.
- Transformation into a malignant neoplasm.
- The appearance of ulcers.
- When located on the birth canal of a woman in labor, the newborn becomes infected.
- Traumatization of growths, their inflammation and bleeding.
To avoid the dangerous consequences of genital warts, girls who discover the first signs of the disease need to consult a gynecologist as soon as possible. The type of growth can be determined by comparing them with photographs, but an examination by a specialist is required.
How to treat condylomas in women?
When diagnosed with condyloma, a woman must undergo a course of treatment. These neoplasms represent an inexhaustible reservoir of infection and can contribute to the emergence of more serious diseases. The list of the most effective and widely used methods for treating condylomas includes:
- Laser destruction. The method involves destroying the tumor by exposing it to a surgical laser.
- Radiosurgery. During the removal of condyloma using this method, the tissue of the resulting outgrowths is cut with a narrowly directed beam of high-frequency waves. Healing after such an operation occurs quickly.
- Thermocoagulation, which is carried out in a special room using a device that burns condylomas under high temperature.
- Chemodestruction. Often, when chemically burning genital wart tissue, agents are used whose active ingredient is nitric acid.
- Cryodestruction. The essence of this method is to destroy tissue damaged by condylomas with liquid nitrogen.
- A modern means of combating skin formations at home - Papilight
Causes
Infection does not always require direct contact.
When examining sexual partners, the virus is detected in both. Papillomavirus is benign in nature and, under favorable conditions, can degenerate into a malignant tumor. This is the reason for the mandatory removal of growths on the skin, regardless of their location and size. Genital warts form more often in women than in men. Reasons for appearance:
- reduced immunity;
- recurrent candidiasis;
- inflammation of the genitourinary system;
- sexual contact without protection.
At risk are women over 25 years of age, without a permanent partner, and leading an active sex life. After infection, a minimum of 2 months will pass, and a maximum of 9, when the first symptoms appear. Sometimes the latent period lasts for years, the virus does not manifest itself in any way.
To combat the pathology, both conservative drug therapy and surgical treatment methods are used.
Among the surgical methods of treating condylomas, the following methods are most in demand:
- Laser destruction. With this method of exposure, condylomas are removed using a surgical laser. Under the influence of laser radiation, the tissue of the skin outgrowth is destroyed. At the site of the condyloma, a small wound is formed, covered with a crust. After a short time, healthy tissue is restored underneath. The method is safe and painless, but expensive, since special equipment is used for the operation.
- Thermocoagulation. This method of treating epithelial warts and growths in women involves burning the tumors using a special device. During this procedure, the woman is given local anesthesia, as the method is quite painful. It is important that thermocoagulation was carried out only by a highly qualified gynecologist, since the slightest contact with healthy tissue by the device leads to the formation of deep scars.
- Chemical destruction. The essence of this method is that condylomas are treated with drugs that can destroy tumor tissue. Such drugs are very effective, most of them contain nitric acid. Even when removing multiple and overgrown condylomas, only two or three procedures are enough to get rid of them completely. After the procedure, the tissues heal quickly, leaving no scars on the skin. If the medicine accidentally gets into healthy tissue, such drugs do not cause any harm. The method is quite inexpensive, quite reliable, effective and safe.
- Radiosurgical method. This method of treating condylomas, like the previous one, is a very expensive procedure. The method of radio wave surgery is characterized by directing a beam of high-frequency waves to the affected area, with the help of which a tissue incision is made and the condyloma is removed along with its stem. The operation is very gentle and leaves no marks on the skin after it is performed.
- Cryodestruction. With this method, condylomas are cauterized with liquid nitrogen. Under the influence of low temperatures, the tissues of the formations freeze and fall off, leaving clean skin in their place. This method is considered one of the most inexpensive; it does not require special equipment or expensive medications. At the same time, the method is not safe; it requires great care and experience from the doctor, since when liquid nitrogen comes into contact with the skin, it causes burns to healthy tissues.
In cases where the condyloma is located in the urethra and is located below 1 cm from its external opening, it can only be removed using a urethroscope. Using the device, the doctor examines the canal along its entire length and treats the condyloma with a special drug that destroys it.
To protect against infection, a number of measures are followed:
- avoid stress;
- a complete diet;
- vitamins and minerals;
- complete rest;
- Spa treatment;
- protect yourself from hypothermia and overheating;
- sufficient sleep;
- maintaining sexual hygiene (one partner);
- mandatory visit to the doctor for any changes in health;
- do not self-medicate, only after examining a gynecologist do they decide on a further plan of action;
- physiotherapy, hardening, massage.
If measures and treatment are followed, patients lead a normal lifestyle. This does not negate compliance with the rules of hygiene and protection of the partner from infection.
The reasons for the appearance of condylomas can be different. But, basically, infection with condylomas occurs through sexual contact. Moreover, the more pronounced the clinical manifestations of HPV are, the higher the risk of infection from an infected partner. In most people, the virus is in a latent, asymptomatic state, and therefore the risk of infection from such a partner is minimized.
Factors that increase the risk of infection include:
- the presence of inflammatory diseases of the genitourinary system,
- microtrauma of the skin, for example, after shaving,
- immunodeficiency states,
- AIDS.
Next, we’ll find out what condylomas look like in men; we’ll see photos of the formations in the next section.
The human papillomavirus currently cannot be treated, but it is possible to get rid of condylomas and prevent the development of a malignant process. Therapy is carried out using medications and traditional methods, using antiviral drugs. Condylomas on the penis (photo of formations above) are removed surgically, or using a laser or liquid nitrogen. Condylomas on the head of the penis are also treated.
Prevention of HPV includes a timely visit to a urologist in order to identify and treat possible infectious and inflammatory diseases, and the mandatory use of condoms during sexual intercourse.
Very often, men confuse condylomas on the penis and warts. We advise you to read the articles in the section
Warts
to avoid incorrect treatment. And find out their causes:
And also learn time-tested ways to treat warts in men.
Watch the video below with Elena Malysheva about how to treat condylomatosis. If you still have questions, you will find more information in our section.
To answer the question of what genital warts are, it is necessary to determine the main causes of the appearance of neoplasms. In most cases, genital warts are benign formations that can quickly take the form of a malignant tumor. According to ICD-10, the disease has code A63.0.
| HPV type | |
| HPV with the highest risk of malignancy | 16, 18, 31, 33, 45, 46 |
| Genital condyloma papillomavirus | more often 6, 11, and also 8, 16, 18, 42, 43, 44 |
It is the oncogenic types of the virus that account for more than 95% of all cancer cases, and up to 70% of oncology cases are provoked by types 16 and 18 in combination. The disease is transmitted through sexual contact, however, the everyday method of transmission of the disease cannot be excluded. Sometimes the disease can pass through breast milk or during pregnancy.
Condylomas, or genital warts, are caused by one of the DNA-containing human papillomaviruses.
Papilloma virus is a fairly common pathology among women and is characterized by a latent course of the disease, without pronounced clinical manifestations.
Sexual transmission is not the only way of contracting the virus; infection very often occurs during the use of household items of a sick person or a carrier of the virus, as well as during the passage of an infant through the birth canal of a sick mother. Genital warts in women are a condition that requires immediate treatment, since the occurrence of these neoplasms in the cervical area creates the preconditions for the development of cancer of the female reproductive system.
Genital warts are small nodules in a woman's groin area.
The growth on the skin and mucous tissues may appear alone, or it may occupy large areas of the skin, causing various inconveniences. What is candilomatosis?
Is this problem dangerous?
And how to get rid of its unpleasant signs?
We will look at all this in this article.
Condyloma is a benign neoplasm of the papillary or verrucous type. It can occur due to exposure to the human papillomavirus.
According to statistics, HPV occurs in 80% of women, but its clinical manifestations in the form of condylomas occur in only 3%. Various factors can provoke their growth: weakened immunity, pregnancy, improper hygiene.
Treatment of condylomas in women is a set of measures to safely remove them and support the body. Therapy is prescribed taking into account the cause of the tumor.
According to recent studies, more than 80% of the world's population are carriers of the human papillomavirus. It is this microscopic pathogen that provokes the development of condylomas on the female body. Genital warts are localized mainly on the external and internal genital organs of women, and can provoke the development of malignant neoplasms.
Condylomas are a rather dangerous disease for both women and men. They pose a great danger to the weaker sex. Condylomas in women are a symptom of the papilloma virus, which poses a threat to women's health, since with this disease there is a high probability of developing cervical cancer and dysplasia. How to treat genital warts in women, what are the causes and symptoms of their occurrence?
Treatment of condylomas with folk remedies
There are a number of folk methods that help combat genital warts. The simplest of them is regular cauterization of the growths with iodine. This drug will dry out the tumors, so that after some time they will disappear on their own. Using the same scheme for the treatment of condylomas, the following is used:
- juice of celandine, young apples, dandelion, pineapple, aloe;
- propolis tincture;
- garlic or onion;
- Kalanchoe;
- rowan berry compress;
- egg white.
How is it treated?
Treatment is aimed at strengthening the immune system and “bringing the virus under control.” Those. preventing the appearance of new growths and deterioration of the patient’s condition. Another procedure that needs to be performed is the removal of existing genital papillomas.
Removal is performed locally. There are several removal methods:
- Using current (electrocoagulation). Impact on genital warts using high temperature. A crust forms at the site of growth, which disappears within a few days. The procedure is performed under local anesthesia. It is considered one of the most affordable and most painful;
- With the help of nitrogen. The condyloma is simply frozen; under the influence of low temperature, the protein located inside is destroyed. The neoplasm dies and disappears, and a wound appears in its place, healing within 2 weeks. The procedure is carried out in a hospital. Does not cause pain, but the cost is much higher;
- Using concentrated alkali or acid. Treatment of the neoplasm is carried out only by an experienced doctor; high precision of application must be observed, as there is a possibility of damage to healthy skin;
- Using radio waves.
- Using a laser. Exposure to a narrowly targeted beam leads to drying out of the condyloma with the formation of a scab (disappears within a week). The advantage of the method is the absence of traces and scars after removal;
- Surgical intervention. It is an outdated method and is rarely used. It can only be performed under anesthesia, local or general. A suture is placed at the incision site. Scarring may appear;
Causes and features of treatment of condylomas during pregnancy?
Pregnancy often causes activation of the papilloma virus. Characteristic formations appear on the skin and mucous membranes of women affected by infection. If condylomas appeared earlier, then during pregnancy they actively multiply, growing and increasing in size and quantity. This is due to the fact that during pregnancy, hormonal levels undergo changes, and the woman’s immune system weakens.
During pregnancy, any medical procedures, including removal of condylomas, should be carried out only after carefully weighing the existing risks and benefits for the mother and fetus. What is at stake is not just the health of the expectant mother, but the preservation of the pregnancy itself and the successful development of the baby. Taking into account this factor, treatment tactics for each individual woman with the problem of condylomatosis should be developed individually.
Systemic therapy
Systemic therapy is based on neutralizing the activity of the virus and completely stopping its reproduction.
You might be interested! Hemangioma in children: causes and methods of treatment
There are two main goals of therapy:
- Reduce virus activity
- Increase the body's immune functions
The assigned tasks are achieved through the use of systemic drugs.
Systemic drugs
Immunocorrective and antiviral medications are effective against papillomavirus.
To enhance the body’s immune function, as well as to increase the effectiveness of systemic therapy, the following medications are used:
cycloferon or inosiplex
– immunostimulating drugs are used to enhance the effectiveness of therapy;- novirin is an antiviral drug effective against the papilloma virus;
- Viferon - has an immunostimulating effect on the cells of the human body;
- allokin-alpha - used intramuscularly, by injecting directly into the area where condylomas are located;
- tincture of eleutherococcus or echinacea - strengthens the immune system, activates the production of interferon;
- supradin, complivit, centrum - will comprehensively increase the content of essential vitamins and minerals in the body;
Reviews
Condylomatosis in women is a problem that has become widespread. Here are some reviews that will help you believe that this disease can be successfully treated.
Irina, 29 “I first encountered the problem of condyloma four years ago. Initially, I tried to get rid of the tumors on my own using various ointments, but nothing helped. After going to the doctor, I decided to undergo cryodestruction of condylomas. They haven’t bothered me for several years now.”
Veronica, 25 years old “A year ago I decided to get pregnant. During a preliminary examination, I was diagnosed with condylomas. The doctor prescribed me a special gel - Panavir. But in addition to daily application of this gel, I regularly burned condylomas with celandine juice and took vitamins to improve immunity. I am now in my second month of pregnancy. Repeated examination showed that I do not have condylomas. I advise all women who want to have a child to undergo a preliminary examination so as not to expose the baby to the risk of infection in the future.”
Olga, 27 years old “I have repeatedly had to fight with condylomas. I first encountered this problem during my first pregnancy. For treatment I used mainly folk remedies, as well as special gels. Before the second pregnancy, condylomas reappeared. I decided to use a more radical method of treatment - cauterization with liquid nitrogen. I’ve been living without condylomas for the last three years.”
Yulia, 21 years old “Eight months ago, during a routine medical examination, I was diagnosed with condylomas. I treated these formations with gels for several weeks, but after a while the condylomas reappeared. The doctor advised me to get rid of them using chemotherapy. For the last six months, the problem of condylomas has not bothered me. I recommend using radical methods to combat these tumors, because ointments and folk remedies, as a rule, do not save for a long time.”
When should you see a doctor?
The penetration of the papilloma virus into the human body may not manifest itself clinically for a long time, but its activation and the formation of condylomas in advanced cases can lead to cancerous tumors. It is very important to immediately consult a doctor if you notice symptoms of this disease.
A modern visit to a specialist will help prevent the development of complications and the formation of condylomas on the skin and mucous membranes of the genital organs.
When do condylomas appear after HPV infection?
When infected with HPV, the incubation period can range from one month to three.
Sometimes it turns out to be longer.
Most often, the infectious process does not manifest itself and remains asymptomatic.
Based on the severity and activity of the lesion, three main forms of the clinical course of the disease can be distinguished:
- Manifest: as a rule, genital warts or condylomas appear in the genital areas.
- Subclinical: small flat genital warts can only be detected by testing with 5% acetic acid, or tissue examination of the affected area is carried out.
- Latent: neither the clinical picture of the disease nor the histology provide any information, and the diagnosis can only be established by directly detecting the DNA of the papillomavirus.
Clinical picture
In accordance with the clinical and histological classification of human papillomavirus infection, the clinical manifestations of the latter are:
- Skin papillomas.
- Condylomas (must be distinguished from those with secondary syphilis and skin papillomas).
- Laryngeal papillomatosis.
Skin papillomas
Skin papillomas, or warts, are also caused by one of the HPV strains. The clinical difference between condyloma and papilloma is due to different types of human papillomavirus. There are simple (vulgar), subungual, mosaic, plantar, flat and other types of these formations. The most common form is vulgar papillomas, which are single or multiple dense elements with clearly defined boundaries and sizes from 1-2 mm to 10 mm. Often there are skin papillomas of larger sizes (“maternal”), surrounded by “daughter” elements of smaller sizes.
The surface of warts has a yellowish-gray color and is covered with cracks formed by layers of plates of the horny epithelium. A characteristic sign of skin papillomas is brownish-black dots on the surface, resulting from the formation of blood clots in their capillaries. They are especially visible when examining warts under a magnifying glass.
Condylomas
The following forms and types are conventionally distinguished:
- Exophytic form (growing outward), represented by genital warts.
- Endophytic, or subclinical - elements grow mainly inside the tissue and show almost no effect.
- Giant Buschke-Levenshtein condyloma, or Buschke-Levenshtein tumor.
Condylomas acuminata
They have a shape corresponding to their name and are flesh-colored or pink-colored fibroepithelial formations on the skin surface or on the surface of mucous membranes. They have a thin stem or (much less often) a wide base. On the skin, their surface is covered with stratified squamous epithelium, usually with hard (less often soft) keratinization. In the latter case, they have an external resemblance to papilloma.
The elements can be in the form of single or multiple point (up to 1 mm) nodules. Outgrowths up to 10-15 mm or more are often formed. If they are multiple, they merge and resemble a cockscomb or cauliflower inflorescences. These formations are the most characteristic clinical manifestations of HPV. Because of their specific localization, they are also called genital.
Condylomas in women occur predominantly in areas with the maximum possible surface maceration - the clitoris, labia minora and majora, the area of the vaginal opening and the mucous membrane of the lower 1/3 of the vagina, the area of the anus and the external opening of the urethra. In half of women with damage to these parts, formations are detected in the form of whitish elements on the cervix. Here they are especially clearly visible during colposcopy after treating this area with a 5% solution of acetic acid.
Genital warts in men are localized on the scrotum and in any part of the penis - on its head, body, in the area of the frenulum of the foreskin and on its inner surface, in the area of the coronary sulcus, directly at the external opening of the urethra, where they usually have a bright red color. coloring, and only in 0.5-5% - on the mucous membrane of the urethra.
During anal sex with an infected partner or friction of healthy areas of skin in contact with affected condylomas, condylomas spread to the perianal area, to the mucous membrane of parts of the rectum close to the anus, to the area of the perineum and inguinal folds, and even to the skin of the upper inner surface of the thighs next to the inguinal folds.
The anus and perineum area are more often affected in women, and the urethra - in men, which is associated with some differences in the characteristics of sexual behavior. Pathological elements, if they are single, may represent only a cosmetic defect and not manifest themselves as subjective sensations. Sometimes they can be brittle and bleed.
However, large growths can macerate, resulting in bleeding, weeping, the addition of a secondary infection, an unpleasant odor, itching and burning, a feeling of pain, irritation, especially when touched. In addition, condylomas can limit the entrance to the vagina, anus and the diameter of the external opening of the urethra, cause pain and burning during urination and defecation.
Unpleasant feeling and pain during sexual intercourse in 13% are the reason for complete refusal of sexual intercourse. They often lead not only to psychological discomfort, but also to severe neuropsychic disorders, the only adequate treatment for which can only be radical removal of condylomas in intimate places and in the genital tract.
Differentiated diagnosis of genital warts
Of great importance is the differential diagnosis of these skin formations through additional studies such as polymerase chain reaction (determination of pathogen DNA), examination of smears and histological examination of tissue biopsy from the lesion. In some cases, only on the basis of the results of these studies can a differential diagnosis be made and a final decision made on how to get rid of condylomas of anogenital localization.
This is due to the fact that visually and in appearance they have much in common with cutaneous papillomas, and, more importantly, with cutaneous malignant neoplasms. In many ways, they are very similar even to such a manifestation of the second stage of syphilis as condylomas lata, which occur in every 5-10 patients, and more often in women. Their location and external resemblance to cauliflower inflorescences are identical to the pointed formations caused by HPV.
The main differences between syphilitic elements:
- in addition to the anogenital area, they can be localized on the skin under the mammary glands, in the armpits, in the folds between the toes, in the navel;
- At first, small dense bluish-red rounded nodular rashes appear on a short and wide base, in contrast to genital warts, the base of which is long and thin;
- when pressing on the nodules, serous fluid is released from the syphilitic elements;
- the individual elements then enlarge and merge with each other, forming red conglomerates with a purple or bluish tint and an ulcerating, weeping surface covered with a whitish coating;
- the surface of individual weeping elements and “inflorescences” contains a large number of pale treponema (the causative agent of syphilis), identified in smears or during histological examination of tissue biopsy.
Endophytic condylomas
Elements can be:
- flat;
- inverted;
- atypical.
They are usually located in the mucous membranes.
Flat condyloma has clear contours, but, as a rule, is not visually determined, since it is located in the thickness of the epithelial layer and does not rise above its level. When analyzing a smear or histological examination, a large number of koilocytes are found on their surface.
The inverted form differs from the flat one in that pathological elements are capable of false ingrowth into the underlying tissues and into the opening of the excretory ducts of the glands of the mucous membrane of the cervix. Both forms are similar to each other and are often combined. During colposcopy, their capillary network is not determined, but dilated vessels can be seen in the form of red dots.
Atypical formations are often detected during colposcopy in the form of small, without clear contours, spiky elevations above the surface of the mucous membranes of the vagina and/or cervix, which is why their surface has a speckled appearance.
Video: Diagnosis of genital warts
Giant Buschke-Levenshtein condyloma
It is a rare pathology that can be caused by 1, 16, 18 or 33 strains of the virus, but mainly by types 6 or 11 of HPV. The usual localization is the anogenital area, especially the areas of the glans penis, scrotum and anus, very rarely - the skin of the groin areas and face, mucous membranes, including the oral cavity.
The disease begins simultaneously in several areas with the appearance of nodules similar to papillomas or genital warts, which quickly increase in size and merge with each other. Clinically, the disease manifests itself as a giant exophytic fast-growing formation, consisting of many growths (vegetations) in the form of cauliflower. It is accompanied mainly by pelvic pain, burning, itching, spotting and bleeding from the vegetation of the tumor-like formation and an unpleasant odor, as well as disturbance of the act of defecation (if appropriately localized). Satellite elements appear around it.
The tumor continues to grow, growing into the underlying deeper tissues and causing their destruction. It is characterized by a high tendency to relapse and can transform into squamous cell carcinoma without a tendency to metastasize.
1. Condylomas acuminata 2. Giant condyloma of Buschke-Levenshtein
Main manifestations of the disease
Condylomas are one of the manifestations of the human papillomavirus. There are a large number of its varieties, and some of the strains are very dangerous and can lead to dysplasia or cervical cancer. The disease is prone to a chronic relapsing course, is widespread, and there is a high susceptibility to the virus among the population.
Condylomas are transmitted primarily through sexual contact, through all possible types of sexual contact. A condom does not provide an absolute guarantee of safety, since the virus can penetrate through microcracks in the skin or mucous membranes in areas not covered by the condom.
Several strains of HPV can be present in a woman’s body at the same time, while she will not even suspect it. The virus leads to a change in the nature of tissue growth, which causes various types of diseases of the mucous membranes and skin.
Most often, HPV types 6 and 11 are found in the female body, which affect the urogenital tract and provoke the appearance of anogenital growths. In order for external manifestations to appear, the pathogen must accumulate in sufficient quantities in the body; in addition, weakened immunity plays a significant role in the manifestation of the disease.
Thus, the causes of the disease are focused on the state of immunity and additional factors.
Risk factors that can trigger the occurrence of condylomas in women include:
- pregnancy;
- vaginal dysbiosis;
- history of STDs;
- frequent change of sexual partners;
- lack of nutrients in the body;
- decreased immunity.
Most often in women, condylomas on the genital organs are located at the vestibule of the vagina, on the labia, on the clitoris, in the vagina and cervix, in the urethral opening, as well as in the perineum and anus. Sometimes condylomas can occur in the oral cavity; they are characterized by a constant increase in size due to constant mechanical damage.
The growths have the shape of papillae, but sometimes they can grow to huge formations, similar to cauliflower. Their color can vary from flesh-colored to reddish-pink. How HPV develops depends on the state of the immune system.
Depending on this, different variants of the course of the disease may be observed:
- Self-healing and regression of growths may occur; this is most often observed if condylomas occur in pregnant women. They disappear for some period after childbirth.
- Absence of any kind of dynamics over a long period of time, i.e. the person is simply a carrier of the virus.
- Gradual or rapid growth of condylomas (increase in the number and size of growths).
- Malignant degeneration of growths.
Depending on how high the risk of developing malignant processes is, the following groups of virus strains can be distinguished:
- non-oncogenic;
- with a low degree of oncogenicity;
- moderate degree of oncogenicity;
- high risk.
Medium- and high-risk strains of the virus (16, 18, 31, 33, 35) can cause cervical dysplasia and increase the risk of developing cervical cancer, but are not capable of causing genital warts.
When the virus enters the body, epithelial cells are damaged. In affected cells, the pathogen can exist in one of two forms: extracellular (benign) or intracellular (integrated into the cell genome, malignant).
The latent course of HPV is characteristic of the extracellular form; this condition does not cause pathological changes in cells and does not lead to clinical manifestations.
Symptoms in women depend on the location of condylomas, most often observed:
- irritation;
- itching;
- pain and discomfort during sexual intercourse;
- bleeding due to injury to growths.
Condylomas of the anus in women and the urogenital tract can have a complicated course, which is accompanied by injury, bleeding and subsequent infection. In addition, the disease becomes an obstacle to normal sexual life and childbirth, and is accompanied by a feeling of psychological discomfort due to a cosmetic defect.
There are not only condylomas on the labia or other parts of the genitals. Women may also experience other types:
- Giant condylomas most often occur in pregnant women due to decreased immunity.
- Papular - have a dark red tint and a dome-shaped shape, the surface is smooth, and are located on the keratinized epithelium.
- Keratotic - look like cauliflower, most often located on the labia.
- Condylomas of the cervix - can be external (almost no different from anogenital growths), internal flat (condylomas inside the vagina and cervical tissue that cannot be detected during a routine examination) or in the form of epidermodysplasia (multiple polymorphic flat papular rash with a warty surface) .
Note! In most cases, growths appear simultaneously, sometimes it takes a maximum of a few days for them to appear.
How to diagnose and treat growths
The diagnostic instructions include a mandatory examination. Usually women turn to a dermatovenerologist or gynecologist. Condylomas, which are located inside the cervix, can only be detected by a doctor during a full examination with colposcopy. If there is a typical clinical picture of genital warts, the strain is not always determined.
Quite often, condylomas at the entrance to the vagina and on the labia are confused with micropapillomatosis, which is a normal variant. If condylomatosis is suspected, exclude the possibility of molluscum contagiosum and condylomas lata with syphilis.
The use of the following procedures is justified:
- extended colposcopy and urethroscopy;
- cytological examination of smears from the cervical canal;
- histological examination;
- PCR;
- immunological tests.
In cases where HPV is not detected but condylomas are present, there is a high probability that the rules for collecting material were violated or the analysis was carried out incorrectly.
Symptoms and treatment of growths in women are closely related. It would be logical to assume that the mere presence of a virus in the body is not an indicator for the use of any drugs. Various types of therapy are used only in relation to formed condylomas.
Treatment methods are selected together with the attending physician
Treatment of condylomas in women can be carried out using medications (local necrotizing, antiviral, immunostimulating) or surgical methods aimed at removing growths.
As part of drug treatment, the following options are used:
- Antiviral agents - epigen spray, isoprinosine tablets, oxolinic and salicylic ointments, Viferon suppositories for condylomas in women, bonafton. These drugs have high antiviral activity and are used topically. The product is applied to the affected area several times a day.
- Immunostimulating drugs are used to increase immunity, since HPV relapses are closely related to the state of the immune system. Cycloferon, polyoxidonium, and reaferon are used for treatment.
- Local necrotizing agents - a fairly common treatment for condylomas in women - drugs have a necrotizing effect on the tissue of the growths. The composition includes various chemicals and acids, treatment at home is allowed, but you need to be extremely careful: if it comes into contact with healthy tissue, a severe burn can occur, so healthy areas need to be protected with a plaster or fabric bandage, and it would be best for the procedure to be carried out by a specialist . Recommended products: condiline, supercelandine, solcoderm.
Removal of genital warts in women using surgical methods is carried out using the following methods:
- Cryodestruction - liquid nitrogen is used for the procedure, which has a cooling effect. Against the background of exposure to the substance, the growths die and disappear. After removal there are no rough scars left, the procedure causes almost no pain. One of the disadvantages of this effect is the long period of tissue restoration.
- Electrocoagulation - the basis of the method is the effect of high temperatures, which are created by high-frequency waves. The electric knife burns the affected tissue, forming a scab that disappears after 5-10 days. Local anesthesia is used for the procedure. The method is suitable for removing both single and multiple formations.
- Using the radio wave method - how are condylomas removed in this case? High-frequency radio waves are used, as a result of which heat is released from the tissues, which destroys the growths. The procedure leaves almost no scars, is bloodless and is widely used in various areas of medicine. The duration of the intervention is about 10-30 minutes.
- Laser removal is one of the most popular methods; it can be used to remove condylomas in the vagina and anus. The laser burns out growths and can sometimes leave scars. Local anesthesia may be used due to the pain of the procedure. The healing period is short.
- Removal with a surgical scalpel - the condyloma is excised along the edges. Today it is practically not used, since it is very painful, requires constant wound care, and damaged tissue takes a long time to recover.
The doctor must choose how to treat condylomas based on the clinical picture and test results. It is important to remember that you should not try to remove the growths yourself, as this can lead to serious complications.
Pharmaceutical celandine is used to remove growths
From the photos and videos in this article, we learned how HPV infection occurs, how the disease manifests itself, and what methods can be used to get rid of growths.
Symptoms of venereal warts
The initial stage is manifested by the fact that patients of the gynecologist or dermatologist complain of pain, burning, itching, and bleeding in the anogenital area.
- Objectively, upon examination, growths are detected in most clinical situations.
- Common locations in men: glans, frenulum, coronal sulcus of the penis and urethral region.
- In women, condylomas, in addition to the space at the entrance to the vagina, are found around the urethra, on the cervix, and clitoris.
- The size of the papillae, characteristic of ordinary genital venereal warts, does not exceed one centimeter in length.
Typically, such growths create significant obstacles to normal sexual life, making it impossible due to general discomfort, pain and complexes.
There is a high probability of infection of such formations.
Then the described symptoms are accompanied by manifestations of the inflammatory process: fever, general malaise, increased pain in the perineal area.
A psychological problem provokes an anxiety-neurotic disorder. Or, to put it simply, neurosis.
The cause of anogenital warts is infection with the human papillomatosis virus.
There are several dozen types of it. Each type of virus leads to the formation of different types of warts - plantar, common, focal epithelial hyperplasia, condylomas and others.
After infection with the papillomatosis virus, on average, 2-3 months must pass before the first symptoms of the disease appear - genital warts.
If a person has a strong immune system, then the incubation period can last a very long time - sometimes several years.
After the end of the incubation time, the first symptoms of infection by the virus appear on the surface of the body - warty growths with sharp peaks, similar to a cock’s comb.
Each condyloma is small in size - 1-2 mm, so it is hardly noticeable. But genital warts tend to grow, forming numerous groups.
Such formations can completely cover the anus, groin and genitals. The first, still isolated, genital warts in men form on the skin of the foreskin.
Initial genital warts in women are found in the vulva and at the entrance to the vagina.
Anogenital warts do not disappear spontaneously, but if they are damaged, ulcers appear in this place.
Candylomatosis is a viral disease, and all diseases of a viral nature are difficult to treat.
Good immunity can become a barrier to the spread of the virus, lengthening the incubation period, but sooner or later the first condyloma will still appear on the genitals or anus.
The further development of the disease will also depend on the state of the immune system: the weaker it is, the more significant the area will be covered by genital warts.
However, a long fight against the virus can weaken the healthiest body. Infection with condylomas has a particularly negative effect on one’s own immunity of the organs and genitals located in the pelvis.
Carriers of papillomaviruses are more likely than healthy people to be affected by other diseases transmitted genitally.
Human papillomavirus infection is most often complemented by other sexually transmitted diseases.
In this case, curing the patient will be much more difficult and expensive, and the treatment itself will take longer.
The virus can be found in the blood by chance during any examination. Thus, genital warts in women can be detected as a result of one of the prenatal screenings.
In this case, the warts themselves may not exist. The virus is simply waiting for the right moment to appear as rashes on the genitals.
In such cases, there is a need to receive recommendations from an immunologist on lifestyle changes and undergoing a course of treatment.
Basic treatment methods
Drug treatment
Medicines are not able to eliminate the disease completely, but they can be used to necrosis and cause destruction of the condylomas themselves. In this case, the viral infection will remain in the body and when favorable conditions are created, a relapse will occur. Doctors often recommend using the following medications during treatment:
Genital warts can be completely cured with special pharmaceutical medications, ointments, and gels.
- "Condilin", which has an antimycotic and cytostatic effect on education. The product is able to block the spread of viral cells at the stage of their division.
- Solcoderm, which contains several acids (oxalic, nitric, acetic, lactic) and copper nitrate, is considered effective. The drug is in the form of a solution and is applied exclusively by a medical professional. The procedure is carried out once, but if there is no desired effect, it can be repeated after a month.
- "Viferon" in the form of a gel or ointment has an antiviral and immunostimulating effect. Indicated for use together with other medications to achieve maximum effect. Therapy lasts 7 days, every day the ointment is applied no more than 5 times.
- Imiquimod cream is indicated for large and medium-sized condylomas. The product is applied to the affected area before bedtime up to 3 times a week. In the morning, wash off the cream from the genitals with soap. To achieve visible results, you should use the drug for several weeks.
All medications are used exclusively as prescribed by a doctor, who indicates the dosage.
Removal of condylomas
Removal of condylomas of the external genitalia is carried out exclusively by surgery. There are such methods by which the disease is eliminated:
- Chemical treatment, in which condylomas can be removed using cauterization with medications.
- During radiocoagulation, papillomas are eliminated using high-frequency radio waves. This procedure is painless and does not leave scars on the body.
- A characteristic feature of laser therapy is that during the procedure the condyloma evaporates and only a dry crust remains.
- Cryotherapy involves removing the tumor using liquid nitrogen. A side effect of this treatment is pigmentation that occurs at the site of condylomas.
- Determocoagulation is characterized by cauterization of papilloma using an electric knife. Within a week, the mucous membrane returns to normal.
After diagnostic procedures, the attending physician will select the most appropriate method of surgical treatment of genital warts. After removal of the papilloma, the patient is not immune from relapse, especially if the body has not overcome the infectious disease. It is strongly not recommended to try to remove papillomas at home, since in this case suppuration and complications are possible.
Folk remedies
It is possible to use folk remedies in combination with drug or surgical therapy, but only with the approval of the attending physician. First of all, therapeutic measures using traditional medicine are aimed at stabilizing the immune system. A decoction made from chamomile and honey is well suited for this. At 2 tbsp. l. Chamomile flowers and honey require 400-500 ml of boiling water. First you should pour the flowers and leave them to brew for at least 3 hours. Then honey is added.
The following traditional medicine recipes will help in removing papillomas:
- A tincture based on celandine, which should be used to lubricate warts up to 7 times a day.
- Garlic juice can overcome almost any viral disease, since it has a detrimental effect on pathogenic microorganisms. It is recommended to lubricate the affected genital area three times a day.
- For the next recipe you need to take sour apples and squeeze the juice out of them. Apply the resulting liquid to the area where papillomas are formed 2-3 times every day until a visible result appears.
Types of genital warts, what they look like (photo)
Benign genital neoplasms are classified as follows:
- Genital condylomas are exophytic - they grow outward, and accordingly, they are located on the skin.
- Flat condylomas - endophytic - grow inward, that is, they penetrate into the deep subcutaneous layers. It is these condylomas that have a high oncogenic index, which means they can provoke cancer. In addition, the danger lies in the fact that they are more difficult to detect than pointed ones.
When it comes to genital condylomas, we most often mean genital warts, but there are other types:
- Papular - the shape of such warts resembles a dome, the color is dark red, the surface is smooth.
- Keratonic - most often found in the pubic area, on the foreskin or on the penis itself. These warts have a stalk.
- Giant condylomas - look like separate patches of skin and can secrete an unpleasant-smelling secretion.
- Endourethral - develops mainly near the urethra.
- Wide - such formations only superficially resemble condylomas; in fact, they are not a consequence of the papilloma virus - they are caused by syphilis.
Ways of infection with the virus
The virus develops exclusively in the human body, and its transmission occurs through certain contact with people. The main form of infection is intimate contact; even when using contraception, a person is at risk.
More often, transmission of the disease occurs as a result of a weakened immune system, stress and poor lifestyle habits.
Diagnosis is difficult due to the fact that the disease does not manifest itself for a long time, is in a latent form and develops covertly. The risk group includes a certain category of people:
- Early sexual life.
- A person's age ranges from 17-33 years, genital warts are most often diagnosed in 20-24 years.
- Unstable partners and chaotic intimate life.
- Anal sex.
The incubation period ranges from several weeks to several years. Then pinkish colored formations of different sizes begin to develop. The disease can be identified by characteristic and constant itching, irritation of the epidermis, mild pain and difficulty during movements or intimacy.
Prevention (prevention of growths)
To prevent condylomas from appearing again, it is advisable that there is only one sexual partner, who should also be offered an examination for the purpose of prevention.
It is necessary to strengthen the immune system (vitamins, echinacea preparations), lead a healthy lifestyle, eliminate chronic stress, eat right, undergo a medical examination, and observe personal hygiene rules.
It is possible to offer vaccination to children against infection with the most dangerous types of papillomavirus in order to protect them from infection in the future.
Treatment
Treatment of condylomas is aimed at eliminating the symptoms of the disease, removing tumors, restoring immunity, and preventing malignancy.
First, patients are prescribed medications. Doctors strive to correct immune disorders by prescribing immunomodulatory therapy. If the patient has single tumors that are small in size, the probability of recovery is 80%.
Destruction
Anogenital venereal warts are subject only to qualified medical treatment and removal.
Considering the danger of condylomas both for the carrier and others, their immediate excision and anti-relapse treatment are recommended.
Medication
- Drug therapy is reduced to the use of pharmaceutical drugs for the destruction of benign neoplasms (solkovagin, solcoderm, podophyllin), which are a mixture of substances with high acidic activity.
- Also immunomodulatory drugs designed to increase the body's resistance to infections.
It is worth noting that home treatment using agents that cause destruction of warts is not recommended.
Unfortunately, there is no drug treatment yet that can kill or remove condylomatous viruses from the patient’s blood that cause genital warts.
Treatment consists of surgical removal of the growths in a hospital and a course of drug therapy carried out at home to maintain immunity.
As for the actual removal of warty growths, doctors have several ways to do this.
Cryotherapy is the removal of condylomas with liquid nitrogen.
The procedure is inexpensive, and if the doctor has experience, complications with this method of treatment are excluded.
A little liquid nitrogen is applied to the wart, its tissues freeze, their protein contents are destroyed, after which the formation itself will disappear, and in its place a small mark will remain, which will heal within a week.
Your doctor may treat you with one of the prescription genital wart removal medications, which contains concentrated acid.
This treatment is more expensive than cryotherapy, but it is more convenient and safer. An acid preparation is applied to the genital wart.
After contact with acid, only a small scab will remain at the site of the wart, which will fall off on its own in a few days.
You can get rid of condylomas by exposing them to high temperature, or, in simple terms, by cauterizing them. In medicine, this method is called determocoagulation.
The high temperature, which is destructive for protein molecules, is achieved by emitting high-frequency radio waves, which are created by a special medical device - a high-frequency scalpel.
In this case, wart removal is carried out under local anesthesia. The patient will be able to continue his intimate life within a week after treatment.
Laser treatment of genital warts is popular. Under the beam, the overgrown tissue disintegrates, leaving behind a hard crust, which will fall off on its own a week after cauterization.
Where the wart was, only clean skin will remain.
Forecast
Options for the development of pathology and the effectiveness of eliminating pathological neoplasms:
- If a man, especially at a young age, becomes infected with papillomatosis , as a rule, due to the high levels of the body’s protective functions, the disease does not develop and does not manifest itself. In the case of formation, one course of immunostimulating, antiviral drug treatment is often sufficient to relieve the pathology. Therefore, the prognosis is favorable;
- A man is a carrier of a papillomatous infectious agent ; he himself is not sick, but infects his partner. The prediction is a high probability of remaining a carrier despite treatment;
- In advanced forms and the absence of drug intervention, neoplasms of viral etiology fester and bleed . And thanks to the resulting microtraumas, a secondary infection easily attaches;
- The presence of large conglomerates makes sexual relations difficult . As they grow, they can completely cover the surface of the genital organs;
- The worst prognosis will be the transformation of genital warts into cancer.
Prevention
To avoid unpleasant viral infections of the genitals, preventive measures should be taken. An important point is sexual intercourse: it is not recommended to practice frequent changes of partners or engage in sexual intercourse without protection. It is necessary to adhere to proper nutrition and balance the diet. An active lifestyle and hardening activities are also important. Another preventive measure is maintaining intimate hygiene. If a person avoids stressful situations, gives up bad habits and has a normal schedule, then the risk of infection will significantly decrease.
Why does the disease occur?
Genital warts on the genitals are nothing more than a human papillomavirus infection, that is, PVI. Infection with the HPV-6 and HPV-11 viruses usually occurs during sexual intercourse through damaged mucous membranes or injured skin.
The most difficult thing in recognizing an infection is that its carriers do not show any external manifestations, but they are the dangerous source of infection for a healthy partner. Neither of them realizes that they are joining the ranks of the sick against their own will, and are serving as potential carriers of a viral infection.
Both men and women fall ill with equal success
The disease is not selective based on gender; both men and women are equally affected. The only difference is that in women the clinic is more noticeable and easier to identify.
In order to protect yourself from viruses entering the body, avoid accidental sexual intercourse and undergo examinations by specialists more often. Even using a condom cannot always protect against transmission, since the perineum and other areas of the skin are left unprotected.
Methods for removing genital warts in men
Currently, there are a huge number of methods to combat genital warts in men.
Cryodestruction
Cryodestruction is a method of exposing condyloma to liquid nitrogen.
After 15-20 seconds of cauterization, the wart tissue turns white and a bubble forms on the epidermis.
If the growth is large, re-treat it with nitrogen after 15 minutes.
After several days, the growth dries out and falls off, sometimes leaving a small scar. The period of complete healing takes 14-20 days after the procedure.
The duration of the course is determined by the size and number of growths.
Contraindications:
- Tendency to allergic reactions;
- If the patient is at risk of developing colloidal scars;
- The presence of one of the class of diseases that develop as a result of the pathological production of autoimmune antibodies;
- Taking immunosuppressive medications;
- Susceptibility of the skin to pigmentation.
This method is prescribed when the area of the lesion is at least three centimeters. The procedure is carried out in a hospital setting. This method is painless and low cost.
Electrocoagulation
Elimination of growths of a pathological nature by the targeted impact of electrical discharges on the affected area, coordinated in frequency and strength.
Conducted in a clinical setting by an experienced physician.
It is cauterized with a special apparatus that has an electrode, which is heated to high temperatures as a result of exposure to current.
The duration of the procedure is 5-10 minutes.
The method is painful, so local anesthesia is required. After cauterization, colloidal scars remain.
Indications for use:
- Small pathological growths on the leg;
- Warts in the anus.
Contraindications:
- Allergy to anesthetic drugs, intolerance to electrical procedures;
- Pathological blood clotting disorders;
- Infectious, somatic diseases in acute form;
- Poor quality of the growths;
- Not recommended for diabetes;
Laser treatment
Using a laser knife, a laser beam is directed to the affected area of the epidermis.
The laser affects condylomatous growths, which leads to necrosis of diseased tissue.
Productive, but expensive method. It takes place under local anesthesia.
The advantages of the procedure include the absence of scars, the disadvantages are the high price and the risk of relapse.
It is used for the localization of condylomas in men on:
- foreskin;
- glans penis;
- scrotum;
- around the urinary canal;
- urethra;
- internal and external sides of the anus.
The method has almost no contraindications. One day before therapy, it is prohibited to drink alcohol-containing drinks.
Radio wave method or Surgitron apparatus
Surgitron is a radio wave device.
The principle of operation is to transform electric current into high-frequency waves.
There is no pain, as local anesthetics are administered.
The energy of high waves evaporates the liquid in the cells of the growths and tissue necrosis occurs. Tip - a loop is placed on the growth and acts for a few seconds, then the diseased area is removed.
It is recommended to use the Surgitron device if you have condyloma on:
- penis;
- lower extremity of the anus;
- pharynx and oral cavity;
- centuries;
- armpits.
Contraindications for use:
- The presence of a cardiac device in the patient;
- Pulmonary and cardiac pathologies;
- Oncological lesions;
- Inflammatory processes on the skin;
- Epilepsy;
- Glaucoma;
- Disorders of the gastrointestinal tract;
- Hepatitis and pancreatic dysfunction;
- Diabetes.
Removal with a scalpel
Excision with a scalpel is not a gentle method, but is highly reliable.
A long recovery period is required.
Physical activity, sexual activity, and overheating of the body are prohibited.
The duration of the procedure is 20-60 minutes. The procedure takes place under local anesthesia.
The surgeon treats the area of skin with disinfectants, removes unhealthy tissue, and applies sutures.
Indications:
- Localization of condylomatosis on the superficial layers of the epidermis.
In addition to safety, low price, and the absence of resumption of symptoms during remission, this method has no contraindications.
Main causes of genital warts
Papilloma viruses that are present in the human body can provoke genital condylomas. According to statistics, almost half of the world's population is infected with this pathology. The infection can be transmitted through sexual contact or through household objects. For infection to multiply, the following conditions are required:
- decline of defense mechanisms for various reasons;
- injury to the skin and mucous membrane of the genitals;
- frequent exposure to stressful situations;
- hormonal imbalance;
- hypothermia of the genitals and the whole body;
- the presence of other infectious diseases in the genitourinary system;
- frequent change of sexual partner;
- anal contact;
- unprotected sex with a carrier of condyloma.
The pathology has a superficial course, so the virus is not able to pass into the blood. Coming out, it forms condylomas on the penis or labia majora.
In everyday life, this type of papilloma is transmitted by using contaminated dishes, cutlery, and towels. There is a possibility of becoming infected with genital warts during childbirth if poorly disinfected medical instruments are used. If a pregnant woman already has the virus in her body, there is a risk of transmitting the disease to the fetus. In this case, signs of the disease will begin to appear in adolescence.
You should not take genital warts lightly and perceive the disease as a normal rash. Some viruses that cause formations have a high level of oncogenic effects and can provoke cancer. Therefore, as soon as the first unpleasant signs are discovered, you should consult a doctor.
Risk factors
People at risk are:
- men and women aged 17 to 30 years;
- with low immunity;
- homosexual orientation;
- HIV-positive;
- practicing early sexual intercourse;
- not observing hygiene rules in public places such as baths, saunas, swimming pools.