Main reasons
There are many factors leading to the formation of cholestasis. They are divided into 2 large categories: extrahepatic and intrahepatic. The first group includes:
- Various metabolic disorders affecting the biliary tract. This group includes enzyme deficiency - alpha-1 antitrypsin and cystic fibrosis.
- Metabolic abnormalities without involvement of the bile ducts: tyrosinemia, galactosemia, pathology of enzymatic oxidation of fatty acids, excessive accumulation of fats and glycogen.
- Reduction in the number, size and volume of ducts (Alagille syndrome).
- Any defects and anomalies in the formation of the bile ducts in the embryonic period.
- Severe course of infectious and inflammatory processes in the body caused by bacterial or viral flora.
- Prolonged stay on parenteral nutrition or taking hepatotoxic medications.
- Cirrhosis of any etiology.
- Ideopathic hepatitis. The diagnosis is made when it is impossible to determine the exact cause of liver damage. Pathology occurs in 1-3% of cases.
The causes of cholestasis caused by damage to the biliary tract include pathologies such as:
- Primary cirrhosis of the biliary system.
- Primary sclerosing cholangitis. Arises as the outcome of any inflammatory lesion of the ducts.
- Immunoglobulin G4-associated cholangitis.
- Malformations of the ducts (tumor - hemartroma or Caroli's disease).
- Cholangiopathy that developed as a result of the use of toxic medications.
- Secondary sclerosing cholangitis against the background of ischemic or hemorrhagic damage to the walls of the ducts.
Forms of pathology
VX occurs in the following forms:
- functional - symptoms manifest themselves in the form of a decrease in the level of bile and organic anions;
- morphological - bile components accumulate in the ducts;
- clinical - components are retained in the blood.
The cause of the disease is the absence of obstruction in the main bile ducts. In this case, pathology can develop at the level of intrahepatic bile ducts or hepatocytes.
Other reasons for the development of pathology:
- bile acid activity;
- liver damaged by alcohol;
- virus;
- toxins;
- drugs.
Experts attribute disruption of the endogenous process and heart failure to the reasons for the development of intrahepatic cholestasis in pregnant women.
https://youtu.be/g0eTpazkYPQ
Classification
The disease has the following systematic categories
| Depending on the location of the primary lesion. |
|
| Depending on the intensity of the current |
|
| According to the presence of jaundice |
|
Prognosis and prevention
The prognosis is directly determined by the timeliness of conservative/surgical treatment. So, if a newborn child has biliary atresia, surgical intervention is not carried out on time, hepatocellular failure quickly develops, which turns into cirrhosis with increasing portal hypertension in the first months of the baby’s life.
With this picture, the prognosis is unfavorable, death occurs within 10-12 months. With an infectious or metabolic cause of bile stagnation, the prognosis is favorable (in 80% of cases) and negative if the disease progresses rapidly. Autoimmune disorders have a disappointing prognosis, most often ending in the death of the child.
Clinical manifestations
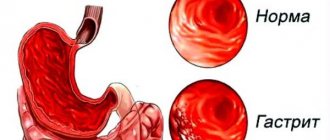
With cholestasis, excessive accumulation of bile occurs in the liver cells and hepatic tubules, the extent of which depends on the cause and severity of the disease. The following manifestations are characteristic:
- Increased liver size. In this case, painful sensations arise at rest and when touched in the right hypochondrium, a feeling of heaviness and discomfort.
- Change in stool color. Due to a deficiency of bile, the intensity of the typical color of stool decreases, down to a completely white color.
- Change in urine color. Bilirubin, the concentration of which in the blood rapidly increases, begins to be excreted through the kidneys, giving the urine a dark color. Outwardly, it resembles foamy dark beer.
- Yellow coloring of the skin, mucous membranes, and sclera of the eyeballs. The higher the total bilirubin and its fractions in the blood, the richer the color.
- Skin itching. Caused by irritation of receptor complexes located in the deep layers of the dermis by bilirubin crystals. Upon contact with water or in the evening, discomfort increases significantly, irritability, emotional lability, and insomnia develop.
- Dyspeptic disorders. Due to a deficiency of excreted bile, enzymatic processes in the gastrointestinal tract and absorption of substances are disrupted. There may be diarrhea, constipation, or alternation of these manifestations. Less commonly – nausea and vomiting, belching of stomach contents, pain and discomfort in the epigastric region.
- Increased bleeding. Caused by impaired absorption of vitamin K. The flow of blood from any minor injuries or scratches does not stop for a long time.
- Tendency to fractures caused by osteoporosis, which develops due to a lack of vitamin D. Normally, it is absorbed only with fatty acids.
- Decreased visual acuity, accommodation and convergence (vitamin A and E deficiency).
- Fibrous transformation of any internal organs, including the liver. The reason is excessive accumulation of copper during a long course of chronic cholestasis.
Expert opinion
Shubin Mikhail
Gastroenterologist, site expert
In rare cases, cholestasis develops gradually (up to 6-12 months), which causes significant difficulties in making the correct diagnosis. Most patients seek medical help due to itchy skin or changes in the color of stool.
What types of stones are there?
All stones formed during the disease need to be studied. Their number and structure help determine the characteristics of the therapeutic effect. All deposits in the gallbladder may differ in color, shape, weight, and components. It is difficult to predict the number of stones that will appear.
Based on their composition, sediments are divided into:
- Brown.
- Black.
- Cholesterol.
- Mixed type.
In patients with an established diagnosis, cholesterol deposits appear most often. Their colors are yellowish, brown, white, the structure is formed from several layers, and is soft. Mixed stones contain cholesterol, but the amount of this substance is approximately half of the total mass. There are always a lot of such deposits, their size is small. Pigment stones do not contain cholesterol, but they may contain bilirubin.
Symptoms are not always observed in patients. Approximately 10% of people did not describe any complaints or discomfort. Their pathology developed asymptomatically. In other cases, it was clear that the patient had liver stones. In the chronic form of the disease, 2 hours after eating fatty foods, aching pain occurs in the right side.
Sometimes all you feel is pressure. Some patients experience bitterness in the mouth and nausea. If there is a stone in the gall bladder, the symptoms are not determined by gender. Often the sac that accumulates bile expands, and pain is felt upon palpation. If fluid is retained in the bladder, stones form and must be removed surgically.
Complications
The list of adverse events with cholestasis includes the following:
- Liver failure. Long-term hypofunction of the liver (over 2-3 years), the toxic effect of bile on hepatocytes lead to death as a result of necrosis of organ tissue.
- Hepatic encephalopathy. The reason is a decrease in the detoxification capacity of the liver and, as a consequence, the toxic effect of many metabolic products (including bilirubin) on the tissues of the central nervous system.
- Sepsis is an extremely rare pathology. Occurs in diseases of the biliary tract caused by pathogenic flora (fungi, bacteria, viruses).
Therapeutic methods
For liver cholestasis, treatment is carried out using pharmaceuticals, traditional medicine recipes, and physiotherapy. In severe cases, surgical intervention is resorted to.
- glucocorticosteroids - Medrol, Metipred;
- ursodeoxycholic acid – “Ursohol”, “Ursosan”;
- antibacterial drug "Rifampicin";
- for itchy skin - Cholestyramine, Sertraline;
- vitamin complex, which includes A, D, E;
- for bleeding - Vikasol (Vit. K);
- for joint pain - calcium gluconate.
Diagnostics
Already at the first visit to a gastroenterologist, this clinical and laboratory syndrome is detected without problems during the examination and collection of anamnesis (disease and family). The next stage of diagnosis is to establish the exact causes of the deviation; for this, the following is carried out:
- General blood analysis. During bacterial inflammation, an increase in ESR and neutrophilic leukocytosis with a shift to the left are recorded. Viral etiology is characterized by lymphocytosis, leukopenia, and sometimes the ESR rises. In the presence of bleeding or intoxication (toxic hemolysis of red blood cells), signs of anemia may occur (decrease in red blood cells, hematocrit, CP, the presence of pathological forms of red blood cells).
- Biochemical blood test is the leading method in making a diagnosis. The following changes are characteristic: an increase in total bilirubin and its fractions (direct and indirect - in case of liver damage, direct - in pathology of the biliary tract), markers of liver cell death (ALT, AST), alkaline phosphatase, as well as perversion of the lipid profile (increase in total cholesterol and triacylglycerides).
- Immunological blood test. In autoimmune diseases, antinuclear or antimitochondrial bodies to hepatocytes and smooth myocytes appear in the blood.
- Ultrasound examination of the liver. Allows you to visualize the increased size of the liver, changes in its internal structure, pathology of the bile ducts (thickening or separation of the walls, obstruction).
- Retrogrand cholangiopancreatography is aimed at searching for stones in the biliary system. If it is impossible to administer a contrast agent through the major duodenal papilla, a percutaneous procedure is performed.
- MRI and CT are the most highly informative methods with almost 100% sensitivity and information content, allowing you to identify any changes.
- Liver biopsy followed by histological examination of biological material. Indicated when it is impossible to make an accurate diagnosis.
Expert opinion
Sevastyanov Roman
General practitioner, hepatologist, gastroenterologist, highest qualification category. Site Expert
Differential diagnosis with such pathologies as viral and drug-induced hepatitis, tumors of the biliary zone (benign and malignant), and developmental defects is of great importance.
Diagnostic tests
The definition of the disease is carried out in several directions. The patient is interviewed, the anamnesis is studied, and an instrumental examination is prescribed to exclude pathologies of the digestive system. When diagnosing cholestasis syndrome, laboratory parameters are taken into account: general and biochemical blood composition, urine analysis.
Instrumental methods:
- Ultrasound examination (ultrasound) allows you to determine the localization of the blockage in the bile ducts.
- Cholangiography shows the degree of expansion in the tracts.
- To confirm cholestasis syndrome, biochemistry is used to determine the activity of excretory enzymes.
- Cholescintigraphy using a marker is used to detect internal or external liver abnormalities.
- Magnetic resonance cholangiopancreatography.
If intrahepatic pathology is suspected, an organ biopsy is performed. This diagnosis is possible if the extrahepatic form is completely excluded.
Treatment of cholestasis
Therapy for cholestasis is always complex and follows the following directions:
- ensuring the outflow of bile (elimination of the etiological factor);
- adherence to diet;
- elimination of clinical manifestations;
- timely prevention and treatment of all complications.
Diet
All patients are recommended to receive adequate doses of proteins and carbohydrates, fatty acid intake should not exceed 40 grams per day, and in case of urgent need, dietary fats are replaced using parenteral solutions (TAS). Additionally, fat-soluble vitamins (A, E, D, K) are added to the diet. For mild cases, you can use the Complivit complex; for severe cases, they are administered intravenously.
Etiological therapy
Aimed at eliminating biliary decompression. Laparoscopic and laparotomic interventions are often used, which are effective in 97% of cases. Are used:
- Papillectomy – removal of the major duodenal papilla. Indicated for tumor processes. After excision of the formation, plastic surgery or installation of a stent in the common bile duct is performed.
- Dissection of the stricture - a surgical technique is indicated for the formation of adhesions or fibrous tissue in the bile ducts below their intramural part.
- Removal of an obstructing factor that is mobile (stone, helminths, incorrectly installed stent). Plastic and nitinol stents are used.
- Balloon dilatation of a narrowed duct is the introduction of a prosthesis through an endoscope, which is inflated and takes a stable shape, ensuring dilation of the duct and its adequate drainage function.
- Bougienage of the common bile duct is the gradual introduction of probes with increasing diameter to expand the structured duct.
- Photodynamic treatment is the intravenous administration of a solution with photosensitizing properties that can accumulate in benign and malignant actively proliferating tissues of the biliary tract. The procedure leads to the destruction of tumor cells.
- Endoscopic ultrasonography is the effect of an ultrasound device on stones, fibrous cords and other mechanical obstacles, followed by their destruction and removal through the bile duct system directly into the lumen of the gastrointestinal tract.
Pathogenetic treatment
In order to reduce the severity of manifestations and compensate for impaired liver functions, the following are used:
- Ursodeoxycholic acid preparations, which stimulate the transport of bile acids and reduce the severity of ductal damage. The medication also has a cytoprotective effect and increases local immunity factors.
- Amino acids, such as adenosine-L-methionine. Participates in the formation of sulfates, taurine and bile acids, leading to a decrease in their number in hepatocytes.
- Hormonal drugs. Prednisolone reduces the concentration of bilirubin in the presence of jaundice and eliminates staining of the skin, as well as itching.
- Blockers of nuclear receptor complexes. Reduces the destruction of hepatocytes and the level of alkaline phosphatase.
- Liver transplantation is indicated for a steadily progressing process and a rapid increase in symptoms of hepatocellular failure.
Diet
One of the methods of treating cholestasis is dietary nutrition. It should be aimed at sparing the liver. This means that it is necessary to consume only foods that do not cause increased formation of bile, since this substance accumulates in the gland, gradually destroying it.
Dietary recommendations:
- The diet of a sick person should not contain canned foods, smoked meats, fatty foods, spicy foods, baked goods, spices and meat broths.
- Eating fresh vegetables and fruits, as well as dishes made from them, can significantly improve the patient’s condition, as well as stop the progression of the disease.
- It is also recommended to drink medicinal mineral waters daily.
The prognosis of cholestasis is most often favorable, since with this syndrome liver function is preserved for a long time. But if symptoms are ignored for a long time, liver failure may develop. To prevent this from happening, it is important to promptly contact specialized medical institutions for diagnosis and treatment of the disease. After eliminating the causes of the disease, the patient recovers quite quickly.
Dietary recommendations
Treatment of the disease involves following diet No. 5. The diet is formed taking into account the permitted products:
- lean poultry, beef;
- cereals in unlimited quantities;
- vegetable purees, soups;
- non-sour fruits, juices, compotes;
- low fat dairy products;
- rye bread (wheat in small quantities);
- eggs no more than once every 5 days;
- weakly brewed tea, honey.
- fatty fish and meat (pork, lamb);
- fried eggs;
- spicy vegetables and seasonings: mustard, hot pepper, horseradish;
- sour berries, herbs, vegetables, fruits;
- marinades, smoked meats;
- pastries from butter dough;
- chocolate, ice cream;
- strong tea, coffee;
- alcoholic drinks.
Meals should be in small portions at least 5 times a day.
Fried foods are completely excluded. The menu includes only boiled and steamed products.