Antiphospholipid syndrome (APS) is an acquired autoimmune disease in which the immune system produces antibodies (antiphospholipid antibodies, aPL) to phospholipids in the membranes of its own cells or certain blood proteins. In this case, damage to the blood coagulation system, pathology during pregnancy and childbirth, a decrease in the number of platelets, as well as a number of neurological, skin and cardiovascular disorders are observed.
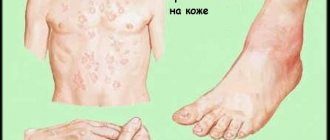
Skin manifestations of antiphospholipid syndrome
The disease belongs to the group of thrombophilic diseases. This means that its main manifestation is recurrent thrombosis of various vessels.
For the first time, information about the role of specific autoantibodies in the development of coagulation system disorders, as well as the characteristic symptoms of the disease, was presented in 1986 by the English rheumatologist G. R. W. Hughes, and in 1994, at an international symposium in London, it was proposed to use the term “syndrome” to refer to the disease Hughes."
The prevalence of antiphospholipid syndrome in the population has not been fully studied: specific antibodies in the blood of healthy people are found, according to various sources, in 1–14% of cases (on average 2–4%), their number increases with age, especially in the presence of chronic diseases. However, the incidence of the disease in young people (even, most likely, in children and adolescents) is significantly higher than in the elderly.
According to modern concepts, antiphospholipid antibodies are a heterogeneous group of immunoglobulins that react with negatively or neutrally charged phospholipids of various structures (for example, antibodies to cardiolipin, antibodies to beta-2-glycoprotein, lupus anticoagulant).
It is noted that women get sick 5 times more often than men, the peak occurs in middle age (about 35 years).
Synonyms: Hughes syndrome, phospholipid syndrome, antiphospholipid antibody syndrome.
Important information about antiphospholipid syndrome
A complex type of autoimmune pathology was first identified in 1986 thanks to the descriptions of the English rheumatologist Huge, after whom Huge syndrome was named. In medical reference books, antiphospholipid pathology is included in the section Thrombophilias, which are a group of diseases characterized by increased formation of blood clots. There is no information about the true distribution of APS; there is information about an insignificant level of antibodies (AT) in absolutely healthy people (2-4%), high titers were found in 0.2% of the examined individuals.
According to statistics, women of reproductive age (20-40 years) most often suffer from the pathology. The threat of phospholipid syndrome is especially high during pregnancy; the pathology can complicate its course, including termination of pregnancy.
The factor that provokes antiphospholipid syndrome is β2-glycoprotein I. By binding to phospholipids, this type of protein increases anticoagulant activity, causing increased production of antibodies in sick people. As a result, the synthesis of one's own anticoagulants (antithrombin, prostacyclin, etc.) is suppressed with increased formation of procoagulant mediators (thromboxane, etc.). This process induces activation of the endothelium along with platelets, causing neutrophil degranulation.
Possible complications and consequences
The main danger for patients with antiphospholipid syndrome is thrombotic complications, which unpredictably affect any organ, resulting in acute disturbances in organ blood flow.
Antiphospholipid syndrome leads to miscarriage
For women of childbearing age, in addition, significant complications are:
- miscarriage;
- intrauterine growth retardation as a consequence of impaired placental blood flow and chronic hypoxia;
- placental abruption;
- gestosis, preeclampsia, eclampsia.
According to various sources, antiphospholipid antibodies in the blood of healthy people occur in 1–14% of cases (on average 2–4%), their number increases with age, especially in the presence of chronic diseases.
Basics of pathogenesis
Specific factors that can be called the underlying causes of Huge syndrome have not been established. An increase in the production of antiphospholipid antibodies, which are part of the structure of the membranes of platelets and other cells, occurs due to a failure of the immune defense. Your own immune system mistakenly identifies its own structural components as foreign, directing all its efforts to destroy them.
According to general criteria, pathology can be provoked by the following factors:
- treatment with hormonal medications, psychotropic drugs, including antidepressants;
- a history of autoimmune diseases such as lupus, untreated rheumatoid arthritis;
- previous colds, including tuberculosis, infection of the oropharynx with streptococci.
It is precisely because of the peculiarities of pathogenesis that antiphospholipid syndrome is included in the group of autoimmune pathologies. There are several types of phospholipids:
- neutral lipids include phosphatidylethanolamine, phosphatidylcholine;
- in the negatively charged group - phosphatidylinositol, phosphatidylserine, cardiolipin.
Hepatitis C, malaria, infectious mononucleosis and endocarditis, HIV, even viral and bacterial infections occur with a transient increase in AF antibodies. High levels of antibodies to phospholipids are found in systemic lupus erythematosus, Sjögren's disease, rheumatoid arthritis, and periarthritis nodosa.
Signs of AT hyperproduction were noted in cases of suspected malignant neoplasms, in patients taking hormonal (contraceptives) and psychotropic drugs, as well as in those who stopped using anticoagulants. There is no exact data on the role of hereditary predisposition; most often, specific causes of autoimmune failure cannot be established.
Classification of API
The structuring of clinical and laboratory variants of autoimmune diseases is based on the features of etiopathogenesis, as well as the course of the disease.
- Symptoms of the primary form are not directly related to a disease that can provoke the induction of aPL antibodies.
- Signs of the secondary type of antiphospholipid syndrome accompany another autoimmune disease.
- A catastrophic form of the pathology, called acute coagulopathy, develops with many thromboses affecting internal organs.
- APL-negative (hidden) type of the disease, which occurs most often, is characterized by the impossibility of determining serological markers of pathology.
Comment. Laboratory methods for testing blood serum are used to identify antiphospholipid components. The quality of diagnostics varies - the presence of some antibodies can be determined, the presence of others is determined by their concentration in the blood.
Treatment
There are no generally accepted international standards for treating the disease; drugs with immunosuppressive effects have not shown sufficient effectiveness.
Pharmacotherapy of antiphospholipid syndrome is aimed mainly at the prevention of thrombosis, using:
- indirect anticoagulants;
- antiplatelet agents;
- lipid-lowering drugs;
- aminoquinoline drugs;
- antihypertensive drugs (if necessary).
Types of antibodies
Based on the results of tests performed in special laboratories, the following types of antiphospholipid antibodies are registered:
- The lupus type of anticoagulant is indicated by the presence of immunoglobulins lgG and lgM. For healthy people, the normal antibody concentration is 0.8-1.2 arbitrary units. An indicator that has increased to a value of 2.0 is a clear sign of antiphospholipid syndrome.
- The appearance of antibodies to cardiolipin in the serum is signaled by immunoglobulins IgA, IgG, IgM. If their concentration is less than 12 units per milliliter, we are talking about APS; syphilis is also diagnosed using this component. Values below the maximum norm indicate the absence of these diseases in the test subject.
- The presence of antibodies to beta-2-glycoprotein is indicated by immunoglobulins such as IgA, IgG, IgM. An analysis result exceeding the limit of 10 units can be considered a sign of autoimmune pathology. Values below the established norm are recorded in healthy people.
- Qualitative detection of titers to the group of phospholipids (cholesterol, cardiolipin, phosphatidylcholine) is performed during blood diagnostics for the Wasserman reaction. A positive test result in the absence of syphilis suggests an antiphospholipid malfunction.
The appearance of the described components is accompanied by damage to the membranes of the cellular structures of blood vessels, which results in an acceleration of blood clotting ability. By forming a large number of blood clots, the patient’s body tries to compensate for the emerging defects in the vascular walls.
The process of increased thrombus formation leads to the appearance of thrombosis - the lumens of the vessels become clogged with blood clots, preventing blood circulation. This leads to insufficient supply of tissues with oxygen and nutrients due to cell starvation. As a result, organ cells die, and the patient suffers from the characteristic clinical symptoms of antiphospholipid pathology.
Symptoms of presence
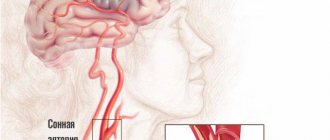
Vein blockage in APS is the most common manifestation. In this case, the veins of the extremities, liver, lungs, and retina of the eyes can become thrombosed. Arteries are affected less frequently, but provoke no less severe consequences:
- attacks of cerebrovascular accident;
- ischemic stroke;
- persistent headaches, migraines;
- convulsions;
- hearing loss;
- damage to the optic nerve, decreased visual acuity;
- dementia, mental disorders.
Cardiac dysfunction may manifest itself as thrombus formation in the myocardial cavity, myocardiopathy, increased blood pressure, or pulmonary hypertension . Valvular damage ranges from mild reflux to stenosis or regurgitation with significant hemodynamic changes. In addition, the following pathological signs are noted:
- the appearance of protein in the urine;
- nephropathy;
- renal failure;
- enlarged liver;
- hepatic vein thrombosis;
- blockage of intestinal vessels with severe abdominal pain, alternating constipation and diarrhea;
- splenic infarction;
- bleeding from the digestive tract;
- redness of the feet and soles;
- trophic ulcers;
- gangrene of fingers.
A disruption of the body's immune response is manifested by a decrease in platelet levels in the blood and hemolysis of red blood cells . Destruction of the head of the bone is the cause of pain in the hip joint and difficulty walking. Obstetricians often encounter autoimmune cell membrane damage syndrome. It leads to miscarriages, inhibits fetal growth, and causes oxygen starvation due to insufficiency of fetoplacental blood flow.
Variety of clinical manifestations of APS
From the point of view of modern medicine, the disease can be classified as an autoimmune thrombotic vasculopathy, accompanied by damage to vessels of various diameters. Due to the extensive localization of the syndrome, which extends not only to capillaries, but also to large blood streams (arterial, venous), antiphospholipid failure demonstrates a wide range of symptoms. In clinical practice, there are cases of both asymptomatic carriage of phospholipid antibodies and life-threatening manifestations of Huge pathology.
What is the danger of high volumes of antibodies?
The appearance of a critical number of antibodies to phospholipids negatively affects a number of body structures:
- In endothelial cells (endotheliocytes), the synthesis of prostacyclin, a vasodilator, which prevents platelet aggregation, is reduced. There is also an inhibition of thrombomodulin (protein), which is necessary for the start of the antithrombotic effect.
- The interaction of platelets with AT phospholipids stimulates the production of substances that increase the level of platelet aggregation. Exceeding the normal level of antibodies threatens the rapid destruction of blood cells, resulting in thrombocytopenia.
- A high percentage of phospholipid markers negatively affects the state of the system responsible for blood clotting. The volume of humoral components of this system in the blood decreases, which leads to thickening of the blood and weakening of the activity of heparin.
The listed effects of the negative influence of a high number of antibodies increase the clotting of the blood supplying all organs. The result is the formation of blood clots against the background of the development of symptoms of hypoxia.
Development mechanism
The pathological process is based on a group of changes. The algorithm for solving the problem is approximately the following:
- The human body is influenced by a certain provoking factor. These may include a previous infectious disease, viral or bacterial, there are several options. Systemic disorders of an inflammatory profile, but not of a septic nature.
Also the influence of a toxic factor, poisoning with salts of heavy metals, vapors of other substances. What caused the onset of the pathological process needs to be clarified through diagnostics.
- As a result of the influence of a negative factor, a problem like an autoimmune reaction develops. It is false because there is no longer a real threat. Such a failure can be of varying degrees of severity: from minimal, which is practically unnoticeable or has no symptoms at all, to critical violations.
- As a result of an autoimmune reaction, a large number of antibodies to phospholipids are produced. These compounds enter the structure of cells and the substances provoke the destruction of membranes, which leads to catastrophic consequences.
It should be noted that in almost 3% of people it is possible to increase the level of antibodies without any health problems. This is not considered a pathology, the body copes with the disorder, but it may well indicate the initial phases of the disorder, so this phenomenon should absolutely not be ignored.
- Antibodies to phospholipids cause cell destruction by dissolving the outer membrane. All cytological structures suffer indiscriminately, depending on how immune substances circulate.
As a result of APS syndrome, platelets, the structures of the brain and central nervous system in general, the heart, kidneys are most affected; in pregnant women, the placenta is affected, creating a huge danger to the fetus.
Ultimately, this reaction leads to disruption of the entire body. How dangerous it is depends on the amount of antibodies synthesized and the aggressiveness of the body’s immune response. It is necessary to begin treatment as quickly as possible. Otherwise, it will be impossible to predict complications.
According to statistics, women under the age of 35-45 are mainly affected. They are at increased risk and therefore require careful monitoring, especially during fertile years and during pregnancy.
Overview of violations in different systems
The main manifestation of antiphospholipid syndrome is the presence of recurrent thrombosis affecting various vessels. This leads to the appearance of dangerous neurological, cardiovascular, obstetric, and skin disorders, as well as the development of thrombocytopenia. The main conditions indicating the presence of aPL antibodies include violations of a certain localization.
Poor circulation
Among the typical symptoms of APS, characterizing impaired blood circulation:
- The appearance of recurrent venous thrombosis with a high probability of clot formation, which causes nutritional deficiency of tissues and organs. The threat of this condition is associated with the death of cellular structures with the subsequent development of gangrene.
- Signs of partial blockage are manifested by numbness of the limbs, a feeling of goosebumps, and lack of sensitivity to external irritants. Thrombosis most often affects both superficial and deep venous beds, mainly in the lower extremities.
- If the retinal veins are damaged, the patient is diagnosed with mono or binocular type of blindness, accompanied by rupture of blood vessels. For antiphospholipid pathology that affects the organs of vision, the most typical fact is simple ischemia. Destruction of the optic nerve results in loss of vision.
If the blood vessels are affected by the symptoms of APS, the patient will experience a sensory disorder followed by loss of motor activity. The tissues of the affected limbs change their color - from pale to purple, and may become purple or brownish. The color option depends on the type of affected vessels. The condition, accompanied by intense pain, progresses to necrosis, ending in gangrene.
Cases of clot rupture and migration are incompatible with life due to blockage of vital arteries.
The spread of APS through the vessels of the lungs, liver and stomach is indicated by a number of symptoms, including:
- signs of pulmonary hypertension;
- venous thrombosis of the hepatic portal vein;
- infarction of the liver, spleen;
- stomach bleeding.
Heart diseases
The threat to heart health due to the abundance of antiphospholipid antibodies is associated with damage to cardiac structures, which is manifested by characteristic clinical symptoms:
- Intense pain of a pressing or burning nature, indicating an ischemic cause of discomfort. A strong burst of pain sometimes lasts tens of minutes, then subsides.
- An abnormal heart rhythm leads to the development of tachycardia. The appearance of an unfavorable sign may be accompanied by nausea. Shortness of breath is possible, which patients note even in a state of absolute rest, without any physical exertion.
- The reaction of the central nervous system to antibodies is accompanied by dizziness. Its cause is insufficient nutrition of the brain, which is associated with a decrease in the contractility of the heart affected by APS. Repeated loss of consciousness is possible.
Bladder diseases
Renal manifestations include symptoms of both mild proteinuria and acute renal failure. Painful discomfort is felt immediately, but is accompanied at first by a slight pain intensity, manifested by aching or nagging pain. A change in the shade of urine from light to dark indicates the onset of hematuria and the enrichment of urine with protein. In some clinical situations, an increase in temperature cannot be ruled out. Such symptoms indicate possible renal failure, which requires urgent medical attention.
Pain during voiding is not recognized as a specific symptom of antiphospholipid syndrome. To make a diagnosis, a thorough history taking with a correct analysis of the patient’s complaints is important.
Nervous system
The central nervous system responds to brain damage:
- migraine-like headaches;
- development of asthenic syndrome, weakness;
- impaired ability to move and control one’s own activity.
Focal neurological symptoms of antiphospholipid attack include convulsive syndrome, progression of dementia, and uncontrollable trembling of the limbs. If the structures of the spinal cord are damaged, transverse myelitis develops; myocardial infarction, intracardiac thrombosis, and arterial hypertension warn of damage to the cardiovascular system. When parts of the brain are affected by the disease, the patient suffers from mental disorders.
Skin lesions
A specific type of skin lesion is associated with a failure of peripheral blood circulation; the disorder leads to thrombosis of small vessels. As a result, the skin is covered with a vascular network of a bluish-violet hue - a reticular type of livedo. Well-visible meshes are localized on the hands, thighs, legs and feet, causing the development of gangrene of the extremities. Traces of multiple hemorrhages in the nail bed resemble a splinter; rarely appearing pinpoint hemorrhages are similar to signs of vasculitis.
Other violations
In case of damage to the vessels of the excretory tract, typical disorders signal a failure of kidney function. Problems with the urinary process (dysuria) manifest themselves in many variations, most often a decrease or increase in daily urine volumes and urinary retention. To make a correct diagnosis, diabetes insipidus must be excluded.
The onset of asthenic syndrome is warned by the appearance of weakness, fatigue, and drowsiness, which prevents active activity and leading a normal lifestyle. With the appearance of a strong feeling of fear, the patient is plagued by mental attacks against a background of symptoms similar to angina pectoris. This condition requires hospitalization due to the risk of a heart attack.
Antiphospholipid syndrome has no gender or age restrictions, but children get sick less often, and women are 4-5 times more likely than men.
If signs of pathology are detected in a pregnant woman, this is a threat to the main stages of fetal development, when the fertilized egg is not able to implant in the uterine cavity. Due to impaired blood flow, placental insufficiency cannot be ruled out.
APS syndrome and pregnancy
Increased production of antiphospholipid antibodies during pregnancy leads to the development of several types of pathology:
- Intrauterine fetal death after the 10th week of pregnancy, which leads to recurrent miscarriage.
- Early preeclampsia and severe eclampsia.
- Placental ischemia.
- Fetoplacental insufficiency.
- Fetal growth restriction, fetal arrhythmia.
- The development of three or more unexplained spontaneous miscarriages before the 10th week of pregnancy.
- Thrombosis of veins and arteries in the mother.
- Intrauterine fetal death.
- Arterial hypertension.
- Chorea.
- Hellp syndrome.
- Early placental abruption.
- Stillbirth.
- Unsuccessful IVF.
Very important! A child born to a mother suffering from APS may develop thrombosis of various localizations from the first days of life, which confirms the genetic predisposition of antiphospholipid syndrome. Such children are more at risk of developing autism and circulatory disorders.
Diagnostic criteria
Antiphospholipid syndrome is diagnosed according to specially developed and approved clinical and laboratory research programs in 1999. Their assessment based on a combination of two criteria (clinical and laboratory) allows the correct diagnosis of APS to be made.
Clinical episodes
According to the list of clinical criteria, two important aspects are identified as the main diagnostic factors after a thorough examination of the anamnesis:
- Identified vascular thrombosis. Episodes of the disease affecting the network of small vessels of any organ must be confirmed instrumentally (Doppler) or morphologically (histology).
- The pathological course of pregnancy must be confirmed by one or more cases of fetal death (10th week of pregnancy), as well as the fact of premature birth without complications during the gestation period up to 34 weeks due to three functional failures - fetoplacental insufficiency, preeclampsia, eclampsia.
The criterion for APS can be at least three spontaneous miscarriages. Termination of pregnancy must be registered during its normal development, without anatomical or hormonal disorders, or chromosomal defects found in one of the parents.
Laboratory research
The list of laboratory criteria for diagnosing antiphospholipid syndrome consists of the following components of the study of blood serum:
- detection of antibodies to cardiolipin anticoagulants IgG or IgM of medium or high concentration at least 2 times, performed using the ELISA program (enzyme-linked immunosorbent assay);
- detection using a standardized ELISA method at least 2 times of an average or high concentration of antibodies to anticoagulants IgG or IgM, manifesting the presence of β2 glycoprotein-I;
- detection by standard international methods at least twice of markers characteristic of a lupus anticoagulant, with intervals between analyzes of at least 12 weeks.
The diagnosis is not considered confirmed if phospholipid antibodies are not detected in the patient during plasma testing for more than 5 years. The diagnosis of APS is also not confirmed in the absence of clinical indicators after examining blood taken less than 12 weeks after the discovery of clinical symptoms.
Please note: confirmation of antiphospholipid syndrome will be recognized as real and requiring treatment if a pair of criteria are met - one from the clinical and laboratory categories.
Which doctor should I contact?
Antiphospholipid syndrome is treated by a rheumatologist. Since most cases of the disease are associated with pregnancy pathology, an obstetrician-gynecologist is involved in therapy. Since the disease affects many organs, consultation with relevant specialists is required - a neurologist, nephrologist, ophthalmologist, dermatologist, vascular surgeon, phlebologist, cardiologist.
Lecture by Khasina M. Yu. on the topic “Diagnostics of antiphospholipid syndrome”:
Medical Director Veronika Ulanova talks about antiphospholipid syndrome:
How is Huge's vascular pathology treated?
The main goal of complex therapy is to prevent complications caused by thrombosis. The difficulty in choosing treatment measures is due to the lack of reliable information about the causes of the disease and the mechanisms of its development. The treatment regimen is built using a trial method - if the prescribed drug shows a good effect, they are recommended to continue treatment for APS.
During treatment, the patient will have to follow a number of vital rules:
- Reduce physical activity by avoiding excessive loads.
- Do not remain at rest for a long time without moving.
- Adhere to the daily regimen developed by your physician.
- Give up bad habits and air travel.
- Do not stop taking medications without consulting your doctor.
The therapeutic course of drug resistance to antiphospholipid syndrome is implemented in two directions - treatment and prevention. First, the signs of the acute form of incipient thrombosis are stopped, then they move on to preventive measures that provide protection against episodes of repeated thrombosis.
What is prescribed for thrombosis
To remove the patient from the phase of acute thrombosis, direct (Heparin) and indirect (Warfarin) anticoagulants are used. The combined principle technique allows you to quickly reduce blood clotting, which helps dissolve blood clots. Next, a drug treatment regimen is selected, which includes several types of drugs:
- anticoagulants (Warfarin and Heparin), which thin the blood, achieve a persistent decrease in its coagulability;
- to prevent relapses and blockage of blood vessels by clots, platelet inhibitors (Clopidogrel, Aspirin) are prescribed;
- glucocorticosteroids (Prednisolone, Dexamethasone) block the inflammatory process in systemic lupus erythematosus combined with APS.
The catastrophic form of antiphospholipid syndrome is blocked in intensive care settings by different groups of drugs.
Urgent treatment options include intensive therapy with high doses of Warfarin and Heparin. The systemic inflammatory process is stopped with glucocorticosteroids, and low platelet levels are replenished with intravenous infusions of immunoglobulin. If there is no effect from the use of intensive measures, cytotoxic drugs are used; against high antibody titers, plasmaphoresis is indicated to cleanse the blood.
Prevention methods
Thanks to timely diagnosis and methods of preventive therapy, it is possible to restrain the development and recurrence of thrombosis, achieve a favorable outcome of pregnancy and uncomplicated childbirth. To protect against the development of a secondary type of Huge's disease, it is necessary to control the underlying pathology and ensure infection prevention. The prognosis risks being unfavorable when recurrent and arterial thrombosis are combined with thrombocytopenia and a persistent increase in AT to cardiolipin levels.
Causes
Antiphospholipid syndrome (APS) occurs when the body's immune system makes antibodies (proteins) that attack phospholipids.
Phospholipids are a type of fat found in all living cells and cell membranes, including blood cells and the lining of blood vessels. What causes the immune system to make antibodies against phospholipids is unknown.
APS causes unwanted blood clots in the arteries and veins. Normally, blood clotting is a normal bodily process. It helps seal small cuts or breaks in the walls of blood vessels. This prevents you from losing too much blood. In antiphospholipid syndrome, blood clotting blocks blood flow, damaging organs.
Researchers don't know why APS antibodies cause blood clots. Some believe they damage or affect the lining of blood vessels, causing blood clots to form. Others believe that the immune system produces antibodies in response to blood clots that damage blood vessels.
How to live with a diagnosis of APS
Antiphospholipid syndrome should not be considered a death sentence; if you receive the necessary and timely therapy, the prognosis for APS will be favorable. It should be borne in mind that modern methods of therapy are a symptomatic process, but it is impossible to completely cure an autoimmune disease. The reason is associated with the emergence of dangerous complications accompanying the pathology:
- systemic lupus erythematosus;
- increased level of antibodies to cardiolipin antigen;
- development of thrombocytopenia;
- persistently high blood pressure.
You will have to take medications for life to minimize the threat of thrombosis, but without eliminating the causes of the problem itself. As a result, the patient has to be observed by a rheumatologist for the rest of his life, periodically monitor serological markers of the disease, and combat the manifestations of antiphospholipid syndrome. Patients need to plan ahead for the possibility of pregnancy to avoid miscarriage, fetal growth restriction (intrauterine) due to blood flow problems, and placental abruption
An elevated level of antibodies in the blood is not always considered a pathology. A small amount (2-4%) of antiphospholipid markers are found in the blood serum of even generally healthy people. To protect against the onset of the disease, modern medicine recommends undergoing regular examinations, which help not only to detect signs of concomitant pathology, but also to prevent thrombotic complications.
Forms of the disease
The following subtypes of antiphospholipid syndrome are distinguished:
- antiphospholipid syndrome (develops against the background of any disease, more often autoimmune, identified in 1985);
- primary antiphospholipid syndrome (described in 1988);
- catastrophic (CAFS, described in 1992);
- seronegative (SNAFS, separated into a separate group in 2000);
- probable APS, or pre-antiphospholipid syndrome (described in 2005).
In 2007, new varieties of the syndrome were identified:
- microangiopathic;
- recurrent catastrophic;
- cross.
In connection with other pathological conditions, antiphospholipid syndrome is classified as follows:
- primary (is an independent disease, not associated with other pathologies);
- secondary (develops against the background of concomitant systemic lupus erythematosus or other autoimmune diseases, lupus-like syndrome, infections, malignant neoplasms, vasculitis, pharmacotherapy with certain drugs).
Antibodies in men
Antisperm antibodies can appear at the stage of first-order spermatocytes, and their level of expression increases with development. These antibodies are distinguished by the property of autoantigenicity, that is, they are immunologically foreign in their own body. Among healthy men, sperm that are located in the epididymis may undergo phagocytosis if ejaculation does not occur. True, this is not associated with the formation of antisperm antibodies, which is probably due to the following:
- The presence of immunological tolerance caused by the processes of sperm resorption.
- Blockade of the formation of antisperm antibodies by other antibodies.
- Individual feature of antibody formation.
The formation of antisperm antibodies in various parts of the male reproductive system is prevented by certain mechanisms. Thus, in the testicles, protection is carried out by the blood-testis barrier, which isolates the cells of spermatogenesis from the immunocompetent elements of the body. The basis of this barrier is made up of special Sertoli cells with their processes.
After sperm leave the testicle, another defense mechanism operates, which consists in their ability to adapt to the environment. This ability is much more pronounced in viable sperm. In addition, the spermoplasm contains local regulatory factors that prevent the formation of antisperm antibodies and the formation of cellular antisperm sensitizations (for example, the immunosuppressive factor of the spermoplasm). Such factors are secreted in the accessory gland of the male reproductive system.
And a little about treatment...
The main goal of treatment is the prevention of thromboembolic complications. First of all, the patient is warned about the importance of adherence to the regimen:
- Do not lift heavy objects, physical activity is feasible, moderate;
- Staying in a stationary position for a long time is unacceptable;
- Sports activities, even with minimal risk of injury, are extremely undesirable;
- Air travel for a long time is strongly not recommended; short trips should be agreed with your doctor.
Treatment with pharmaceuticals includes:
- Indirect anticoagulants (warfarin);
- Direct anticoagulants (heparin, enoxaparin sodium, nadroparin calcium);
- Antiplatelet agents (aspiin, pentoxifylline, dipyridamole);
- In the case of a catastrophic variant, glucocorticoids and anticoagulants in large doses, fresh frozen plasma, and plasmapheresis are prescribed.
Treatment with antiplatelet agents and/or anticoagulants accompanies the patient for a long time, and some patients are forced to “sit” on them for the rest of their lives.
The prognosis for APS is not so bad if you follow all the doctors’ recommendations. Early diagnosis, constant prevention of relapses, timely treatment (with due responsibility on the part of the patient) give positive results and give hope for a long, high-quality life without exacerbations, as well as for a favorable course of pregnancy and a safe birth.
Difficulties in prognostic terms are presented by such unfavorable factors as the combination of ASP + SLE, thrombocytopenia, persistent arterial hypertension, and a rapid increase in antibody titers to the cardiolipin antigen. Here you can only sigh heavily: “The ways of the Lord are mysterious...”. But this does not mean that the patient has so little chance...
All patients with a specified diagnosis of “Antiphospholipid syndrome” are registered with a rheumatologist, who monitors the course of the process, periodically prescribes tests (coagulation, serological markers), carries out prevention and, if necessary, treatment.
Thrombosis in veins and arteries
Most often, doctors are faced with thrombosis, which is recurrent and affects the venous vessels of the legs. Blood clots formed there, breaking off, are sent to the vessels of the lungs, blocking them, and this leads to the occurrence of such a dangerous, and often fatal, condition as pulmonary embolism or PE. Here everything depends on the size of the incoming blood clot and the caliber of the vessel in which this blood clot is stuck. If the main trunk of the pulmonary artery (PA) is closed, then one cannot count on a favorable outcome - reflex cardiac arrest leads to instant death of a person. Cases of blockage of small branches of the pulmonary artery provide a chance for survival, but do not exclude hemorrhages, pulmonary hypertension, pulmonary infarction and the development of heart failure, which also does not “paint” particularly rosy prospects.
In second place in terms of frequency of occurrence can be thrombosis in the vessels of the kidneys and liver with the formation of corresponding syndromes (nephrotic, Budd-Chiari syndrome).
Although less common, thrombosis of the subclavian veins or retinal vessels occurs, as well as thrombosis localized in the central vein of the adrenal glands, which, after hemorrhages and necrosis, forms chronic adrenal insufficiency in the patient.
In other situations (depending on the location), thrombosis is among the triggers for the occurrence of inferior or superior vena cava syndrome.
Arterial thrombosis causes ischemia with the development of necrosis. In short, heart attacks, aortic arch syndrome, gangrene, aseptic necrosis of the femoral head are all a consequence of arterial thrombosis.
Preparing for analysis
Medications should be discontinued
For a reliable result, you must follow the recommendations before taking blood.
- Refrain from eating, drinking, or smoking 12 hours before the test.
- On the day of the test, you should not drink tea or coffee; you can drink plain water.
- All other studies (ultrasound, radiography) should be carried out after taking a blood sample.
- The results of the analysis for aPL are influenced by medications - hormonal contraceptives, psychotropic, antiarrhythmic drugs, so it is necessary to avoid taking them 5 days before the analysis.
- Blood donation for diagnosis should be done in the morning.
Forecast
Timely detection of pathology and preventive treatment provide a favorable prognosis for pregnancy and childbirth. Lack or refusal of treatment is fraught with pregnancy loss and the development of serious complications. All patients with detected APS are registered with a rheumatologist and regularly donate blood for coagulation and immunological parameters.
Sozinova Anna Vladimirovna, obstetrician-gynecologist
just today
( 55 votes, average: 4.47 out of 5)
Gonorrhea during pregnancy: risks for mother and fetus, treatment
Dental treatment during pregnancy: importance, possible risks and consequences
Related Posts
Etiology
The exact reasons for the formation of APS are unknown. Adverse effects of environmental factors are allowed. Factors predisposing to the formation and increase in the titer of antiphospholipid antibodies are identified:
- viral, bacterial infections (tuberculosis, infectious mononucleosis, hepatitis C, salmonellosis, HIV and others);
- taking COCs, psychotropic drugs;
- the presence of systemic lupus erythematosus and other connective tissue diseases (rheumatoid arthritis, periarteritis nodosa);
- malignant tumors;
- immobilization;
- surgical interventions;
- withdrawal of anticoagulants.
Important
A genetic predisposition to increased synthesis of antiphospholipid antibodies has been established in people who are carriers of a number of antigens and in relatives of patients with APS.
How does it manifest in women?
A woman's genital organs contain a large number of various immunocompetent cells. The natural entry of sperm into the genital canals can cause an immune response. True, the immunological process that occurs in the female body immediately after sperm enters has not yet been sufficiently studied. The formation of antibodies in the female body is usually prevented by various mechanisms that reduce the immune response.
During ovulation, the balance of T lymphocytes changes. For example, the level of T-helper cells decreases, and T-suppressor levels increase. Among other things, the total concentration of immunoglobulins and the C3 element of the complement system decreases. An important role in reducing the immune response to sperm, as a rule, is played by the male defense mechanism in the form of sorption and desorption of surface antigens when changing media, and, in addition, immunosuppressive factors of sperm plasma.
In addition, it is assumed that only a small number of genetically selected sperm enter the fallopian tube, which are immunologically different from the majority, and the rest, in turn, die and block local immunity.
Thus, antiphospholipid antibodies have a multifaceted effect on the hemostatic system, damaging any of its protective links in the form of the endothelial barrier, the function of natural anticoagulants, and endogenous fibrinolysis. Among other things, the platelet component of hemostasis with procoagulant factors is activated.
Postpartum period
After delivery, thromboembolism prevention should be resumed after 8-12 hours with Fraxiparin (Nadroparin) - 0.1 ml/10 kg, Clexane (Enoxaparin) 100 IU/kg, Fragmin (Dalteparin) 120 IU/kg, if there is no bleeding.
If a woman has a history of thrombosis, then therapeutic doses of these drugs are prescribed: Fraxiparine - 0.1 ml/10 kg 2 times a day, Clexane - 100 IU/kg 2 times a day, Fragmin - 120 IU/kg 2 times a day .
The use of LMWH must be continued for at least 10 days. And if there was an episode of proven thromboembolism, then anticoagulants are used for at least 3-6 months.
An increase in the concentration of antigens in the blood requires consultation with a hematologist or rheumatologist to decide on hormonal therapy.
Explanation of the research results
Correct interpretation - correct diagnosis
Positive test. An increased level of aPL is interpreted:
- risk of blood clots;
- risk of complications during pregnancy;
- API (if there are other supporting indicators);
- pathology of the vascular system;
- systemic diseases (lupus erythematosus);
- AIDS;
- syphilis;
- malaria.
A negative test means that the level of aPL was not elevated, but if obvious symptoms are present, the test is ordered again.
Price for tests
To identify APS, you can undergo diagnostics for a fee. Many private laboratories offer a panel for the determination of antiphospholipid antibodies. In the Invitro laboratory in Moscow, prices at the end of 2019 are as follows:
- detection of immunoglobulins G and M to cardiolipin costs 1990 rubles;
- diagnostics of secondary APS – price 3170 rubles;
- detailed serological test for APS – 4200 rubles;
- laboratory criteria for APS – 3950 rub.
In the Sinevo laboratory in Moscow, prices for analyzes of this panel vary slightly:
- immunoglobulins G and M to cardiolipin – 960 rubles;
- antibodies to beta2-glycoprotein I – 720 rubles;
- class G antibodies to phospholipids – 720 rubles;
- class M antibodies to phospholipids – 720 rub.
Other private laboratories in Russian cities can offer approximately the same prices.
Taking the test: what is this test used for and when is it prescribed?
An antiphospholipid antibody test is performed to determine the cause of thrombotic microangiopathy, as well as in a number of the following cases:
- To determine the causes of recurrent fetal loss in late pregnancy.
- To find out the causes of thrombocytopenia.
- In order to determine the long time of thromboplastin formation.
When is such a study prescribed? A doctor may recommend it in a number of the following cases:
- If a person is suspected of developing antiphospholipid syndrome (this study is carried out several times over six weeks).
- Against the background of repeated miscarriages, as an addition to the test for the period of thromboplastin formation.
- Against the background of a repeated episode of thrombosis in a patient at a young age.
- When a person develops thrombocytopenia.
- Against the background of symptoms of thrombotic microangiopathy (swelling of the extremities, shortness of breath and constant headaches).
What is the normal level of antiphospholipid antibodies?
Antisperm antiphospholipid antibodies and their norm
Antisperm antibodies are elements against sperm membrane antigens. They were first described in the serum of men who were infertile by Wilson in 1954. Substances are usually found in the blood, seminal plasma, cervical mucus, and, in addition, on the surface of sperm. Most often these are antiphospholipid antibodies IgG or IgM.
Normally, antisperm antibodies in healthy men are found in an amount of one to ten percent. In infertile representatives of the stronger sex they are present in the amount of twenty percent.