Paraproctitis is inflammation of the fatty tissue around the rectum. This disease ranks 4th among proctological pathologies and paraproctitis is often diagnosed in children. Treatment of the disease is mandatory, as it can become chronic and cause complications.
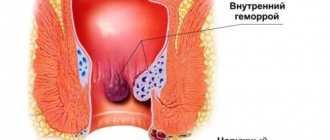
Photos of paraproctitis that occurs in children and adults will help you understand what this disease is. To understand the etiology of the disease, it is necessary to understand the structure of the mucous membrane, as well as the fiber surrounding the rectum.
This organ of the gastrointestinal tract is located so that there are several spaces around it:
- ileo-rectal;
- pelvic-rectal;
- retrorectal;
- submucosal (in the intestinal wall);
- subcutaneous (near the anus).
Inflammatory processes can occur in one or several areas at once.
The structure of the mucosa also has a number of features. In the area of the anorectal line, it creates depressions (pockets) - Morgani's crypts. The mouths of the ducts of the anal glands are located at their bottom. It is worth noting that paraproctitis is very often a complication of cryptitis - inflammation of the Morganian crypts.
Reasons for the development of paraproctitis in children
There are several factors that provoke the disease, but the main one is infection. These can be different pathogens:
- streptococci;
- staphylococci;
- Proteus;
- anaerobic flora;
- coli.
Typically, the infection enters the cellular spaces from the rectum, for example, through the hematogenous and lymphogenous route from infected cracks and microtraumas of the mucosa. The latter are caused by constipation and hemorrhoids.
The infection can penetrate into the perirectal tissue due to blockage of the anal gland duct. Initially, inflammation is observed only at the mouth of the gland and the intestinal crypt.
The bacteria then spread to her body, located in the deeper layers of the intestinal wall. Then it moves to the adjacent pararectal tissue, provoking paraproctitis.
It is worth noting that microbial pathogens can penetrate into the cellular spaces from any foci of chronic infections (tonsillitis, caries, sinusitis). Most often, the cause of the development of this pathology in children is intestinal infections, which weaken the immune system, as well as a violation of the intestinal microflora.
Etiology of the phenomenon
Paraproctitis in children and adults is caused by infection.
If in adults the main causative agent of the disease is E. coli, then in children the pathology is most often provoked by staphylococcus. Pathogenic microorganisms enter the fiber through the damaged rectal mucosa. Microcracks, damage and inflammation of the rectum can occur:
- with frequent constipation;
- when the baby has to strain hard during bowel movements;
- violation of hygiene rules for child care;
- improper feeding;
- constant wearing of diapers;
- but more often damage occurs as a result of infant maceration (softening) of the skin: loss of integrity as a result of diaper rash and diarrhea.
In newborns, the development of paraproctitis can be caused by the abnormal structure of the anal glands. They are often excessively branched, which creates an environment for the accumulation of infection.
The immune system in infants has not yet been formed, and this becomes an additional stimulus for the vital activity of bacteria.
One more important factor cannot be ignored: injury to the anal area. It can be external (due to impacts, friction, scratching, etc.) and internal, caused by small solid bodies swallowed by the child.
Chemical damage to the skin and mucous membranes can be caused by overly aggressive detergents.
Acute paraproctitis in children under one year of age
This form of pathology occurs suddenly and is accompanied by severe symptoms, which depend on the location of the inflammatory process, its size, the type of pathogen and the level of body resistance.
Characteristic signs of the disease:
- Fever with an increase in temperature to 38-39°, chills;
- Manifestations of intoxication – malaise, weakness, headaches, muscle and joint pain, loss of appetite;
- Disorders of urination and stool (constipation), painful urination and defecation;
- Pain of varying intensity in the rectum, lower abdomen, pelvis, which intensifies during stool.
However, different forms of the disease have their own characteristics. For example, subcutaneous is accompanied by swelling, thickening and redness of the tissues near the anus, pain on palpation, and the inability to take a sitting position. The source of inflammation is visible to the naked eye.
The pelvic-rectal form is more difficult to diagnose, since the pathology is located deep in the pelvis and manifests itself only in general symptoms.
- Often, parents do not attach importance to the child’s condition, attributing them to a common respiratory infection.
- There is no improvement when using cold medicines.
- The child's condition worsens, manifestations of intoxication become more pronounced.
- Problems with bowel movements and urination become worse.
- Sometimes the patient’s condition improves sharply, the temperature drops, but profuse purulent discharge mixed with blood comes out of the rectum.
- The reasons for this phenomenon are hidden in the independent breakthrough of the abscess into the intestine after the melting of its wall.
The ileorectal form is rarely diagnosed at the initial stage. Only by the end of the first week are specific symptoms visible:
- red skin;
- swelling;
- asymmetry of the buttocks.
It is worth noting that opening an abscess on your own, as well as inadequate treatment, can lead to complications - the disease becomes chronic or causes serious complications.
What should parents be wary of?
The first signs of paraproctitis in children under one year of age appear at the end of the first day of development of the disease. On the second or third day, possible purulent discharge from the formation or directly from the anus. At the same time, during the process of defecation, a large amount of mucus is released along with feces, which promotes tissue healing.
The subcutaneous form of the disease is easy to diagnose by external signs. The submucosal variant is accompanied only by a slight increase in temperature, which parents often perceive as a decrease in immunity or teething. Therefore, they do not immediately seek help from a doctor. This is dangerous due to the breakthrough of the abscess and the development of sepsis. In this case, the temperature rises to 40 degrees. The child's heart rate increases and vomiting occurs. Urgent medical attention is required. If the listed symptoms appear, parents should call an ambulance.
Chronic paraproctitis
This form is accompanied by the formation of a fistula, a canal whose internal opening opens into the anal crypt. The outer one extends to the skin of the perineum and usually does not exceed a centimeter in diameter.
- The infection constantly circulates between the rectum and perirectal tissue, supporting the inflammatory process.
- With normal patency of the fistula, secretions are discharged regularly, otherwise infiltrates and purulent cavities are formed.
- Symptoms of the chronic form occur in accordance with periods of remission and exacerbation. But purulent discharge is always observed, which, with normal patency, does not cause discomfort.
When the fistula becomes clogged with dead tissue, pus, and granulations, the outflow from the perirectal tissue becomes difficult, and inflammation with its accompanying symptoms occurs again. As a rule, the abscess opens on its own. Then the patient’s condition improves, and remission occurs for some time.
Prevention methods
To prevent paraproctitis in children after one year and in the first 12 months of life, it is necessary to follow basic hygiene rules and promptly treat diseases associated with intestinal dysfunction. If a child is prone to constipation or diarrhea, the problem cannot be ignored. The appearance of painful sensations during defecation requires immediate consultation with a doctor.
An advanced form of the disease can cause not only unpleasant symptoms, but also surgical intervention. This is additional stress for an immature organism.
Prevention of paraproctitis includes compliance with the following recommendations:
- Prevention of constipation and diarrhea. To do this, you need to improve your diet and not forget about your drinking regime.
- Compliance with the rules of personal hygiene from the first hours of a child’s life. The baby should be washed after each act of defecation, and air baths should be given periodically. When diaper rash appears, you need to use special creams.
- Timely treatment of intestinal disorders under the guidance of a pediatrician.
- Strengthening the immune system. Hardening, daily walks in the fresh air, establishing the correct feeding and sleeping schedule - all this has a positive effect on the functioning of the body's defenses.
In the photo, paraproctitis in children under one year old looks quite unpleasant. Therefore, parents themselves should examine the baby daily for redness in the anal area. If specific signs of the disease appear, you should immediately contact your pediatrician.
Treatment of paraproctitis in adults and children
- The most effective method of eliminating pathology is surgery, which is used in both acute and chronic forms. The operation is performed under intravenous, epidural anesthesia or mask anesthesia.
- The action consists of opening and draining the abscess, removing the inflamed crypt and blocking the passage through which the infection circulates. Only such measures will allow you to completely get rid of the acute form of paraproctitis.
- An operation for a chronic disease is performed in exactly the same way, if according to the photo, an opening and drainage occurs. However, treatment should continue after surgery.
- If infiltrates are detected along the fistula, intensive antibiotic therapy and physiotherapeutic treatment are prescribed. After the acute manifestations have stopped, a planned operation to excise the fistula is performed.
Radical treatment for rectal fistulas is carried out only in a specialized department of a medical institution by qualified, experienced coloproctologists.
Features of therapy
According to medical reviews, treatment of acute paraproctitis in children under one year of age is carried out exclusively through surgical intervention. The operation is performed on the day of visiting the doctor, since there is a risk of infection spreading throughout the body if the tumor breaks through into the intestine. The intervention is carried out using general anesthesia. It lasts no more than 20 minutes. If there is a fistula, the operation is carried out in 2 stages:
- The neoplasm is opened, cleaned of purulent secretions, washed and drainage is installed. To prevent infection, young patients are prescribed antibiotics. The duration of treatment is 7 days.
- If the child’s condition improves, the drainage is removed after 3-4 days. After the first bowel movement, daily baths using a manganese solution are recommended.
A slag-free diet is used for three days after the intervention. Additionally, physiotherapy may be prescribed on an individual basis. Typically, the child is discharged 2 weeks after surgery. At home, treatment continues for some time using drugs that restore intestinal microflora.
The chronic form of the disease requires conservative therapy (antibacterial drugs, anti-inflammatory suppositories, Levomekol). If such methods are ineffective, which most often happens, surgical treatment of paraproctitis in a child is prescribed. At 1 year or even 2 years, surgery is usually performed; in the absence of a clear threat, intervention is not recommended.
Complications of the disease
Serious consequences can be caused by both acute and chronic paraproctitis.
The acute form most often provokes the following complications:
- Opening an abscess on the surface of the skin;
- Melting with pus of the rectum, vagina in females;
- Damage to the pelvic tissue;
- Melting of the intestinal wall above the anorectal region, release of pus into the perirectal tissue, spread of inflammation;
- Breakthrough of the abscess into the abdominal cavity or beyond it, development of peritonitis;
- Melting of the walls of the urethra;
- Spread of infection from one cell to another.
The chronic form is accompanied by repeated inflammation and the appearance of scar tissue. As a result, the anal canal narrows and becomes deformed. This also applies to the rectal sphincter.
Symptoms of deviation
The main signs of paraproctitis in a child are constipation or, conversely, loose stools. In addition, it is possible to have:
- pain during bowel movements;
- decreased appetite;
- increased body temperature;
- tearfulness;
- child's worries.
There is severe swelling in the anal area. Most often, children have an acute form of pathology. In the presence of this type of deviation, the child cries during bowel movements due to unbearable pain.
Acute childhood paraproctitis is accompanied by constant pain in the anal sphincter area. There are bumps and redness near the anus. All new growths are warm to the touch. The skin of the buttocks changes color.
One of the signs of the disease is poor appetite
The folds of the mucous membrane become smooth. In the presence of an acute form, purulent discharge is possible. Necrotic tissue destruction is present. In the presence of an acute form of pathology, body temperature increases. The condition is rapidly deteriorating. Irritability appears and performance decreases. The patient feels discomfort when urinating. There is a fever.
The child may have a false urge to defecate. There is weakness and apathy. The baby complains of a painful sensation in the abdomen. On palpation the symptom intensifies significantly. Purulent and bloody discharge is possible.
Chronic paraproctitis in newborns is manifested by the presence of a fistula.
There is an external and internal through defect. Depending on its location, neoplasms are:
- full;
- incompletely open;
- incompletely closed.
The disease often provokes a false urge to go to the toilet.
With an exacerbation of the chronic form, the symptoms are similar to the acute type of the disease. The condition worsens quite often. Deviation cannot disappear on its own. The child must be taken to a medical facility for diagnosis and selection of therapy.
Treatment with antibiotics
Doctors prescribe intravenous antibiotic therapy for children who exhibit signs of a systemic disease secondary to infection, for example:
- pallor;
- lethargy (the baby will not be as energetic as usual);
- fever;
- violation of feeding, sleep, bowel movements.
However, the need for intravenous antibiotic treatment is extremely rare.
Concept and characteristics
Paraproctitis is an inflammation of the tissue that surrounds the lower part of the rectum. In most cases, this disease is diagnosed in adults, but cases of its occurrence in children are no exception.
Infants under one year of age and preschool children are at risk.
The main symptoms of the pathological process are pain during defecation and certain external signs of irritation of the skin around the anus.
Features of the disease:
- paraproctitis is an inflammation of the anal gland;
- the localization of the pathological process has clear boundaries;
- the development of the disease is accompanied by the formation of a purulent abscess;
- in the absence of timely treatment, the inflammatory process spreads rapidly.
Diagnostics
The doctor examines the rectum by palpation, determines the location of the formation, its size, the degree of compaction (in the initial stage it is higher, when an abscess forms, the tissue becomes softer). When paraproctitis is located on the inner wall of the rectum, external examination is ineffective; anoscopy is performed to examine the rectum. If a fistula has formed in a baby due to paraproctitis, an ultrasound and probing are performed to determine the location of its course.
When conducting a general blood test, signs of an inflammatory process in the body are revealed: an increased content of leukocytes and a high erythrocyte sedimentation rate. Additionally, a biochemical blood test and urine test are performed. If pus is released, the bacteria that causes the infection are determined from it in order to prescribe antibiotic therapy. To find out the cause of the pathology, it is necessary to show the baby to an immunologist to rule out lactose intolerance and infectious diseases.
Difference from hemorrhoids
Similar signs are observed when a baby develops hemorrhoids, but due to the non-infectious course of the disease, the child does not have a fever. He is quite active, there is no malaise, and his general health is normal.
Hemorrhoidal bumps appear after physical activity. The disease develops over several months, in contrast to paraproctitis, in which inflammation turns into an abscess in about 7 days (the timing varies from person to person). If left untreated, hemorrhoids can become inflammatory, causing paraproctitis.
The essence of pathology
Paraproctitis is an inflammatory reaction in the tissue located around the lower rectum. Paraproctitis in children is less common than in adults, but unfortunately, it also occurs. Newborns and babies under 6 months are more susceptible to childhood paraproctitis (about 65% of all manifestations in a child).
Somewhat less often, it is recorded in children in the interval of 0.5-1 year (about 20-22% of all cases of the disease). The incidence rate decreases sharply with age.
Another pattern is also emerging: boys get sick much more often than girls. This feature is associated with the anatomical structure: in girls, the pressure in the rectum is noticeably lower, which reduces the risk of damage.
Paraproctitis has an infectious etiology. It originates when pathogenic microorganisms penetrate the loose adipose tissue (fiber) surrounding the rectum. The main routes are the anal glands and the damaged rectal mucosa.
In infants, the increased risk of infection is due to the fact that the tissues of the body are easily damaged, and any prolonged constipation can compromise their integrity, opening the way for infection.
Acute inflammation is provoked first in the anal crypt (sinus) or glands. As the disease progresses, the pathogen enters the tissues, as a result, the affected areas are separated from healthy tissues, which forms an abscess (ulcer).
If timely and adequate measures are not taken, the purulent focus breaks through and opens through the skin to the outside, forming a fistula. The acute course of the pathology becomes chronic.
Taking this into account, paraproctitis is divided into 2 forms: acute and chronic pathology.
Mechanism of the disease
Paraproctitis in infants has features in the mechanism of development. Children are exposed to the elimination of monomicrobial microflora. The development of inflammation occurs in stages. For the disease to appear, a damaged rectal mucosa is required. Otherwise, stagnation of feces occurs.
An obstruction occurs in the rectum, causing a growth to form. If the formation is damaged or opened, the infection spreads to the perianal region. Purulent masses can spread to other organs and tissues. This represents the mechanism for the development of acute paraproctitis.
Making a diagnosis from a doctor
Diagnosis of paraproctitis in infants takes place in several stages. First, the doctor examines the baby. To suspect a disease, the doctor observes the following signs in the anus:
To finally confirm suspicions of paraproctitis in an infant, he is sent for laboratory and instrumental examination methods. The baby is required to undergo a general and biochemical analysis of blood and urine.
Sometimes rectal probing is done. To identify tumors and other problems, radiographic and ultrasound diagnostic methods are used.
Symptoms of acute illness
Primary paraproctitis in a child begins brightly. He is capricious, refuses to eat, and the temperature rises to 37.5°-39° C. The baby becomes more anxious during swaddling and hygiene procedures. Children aged 2-3 years and older complain of pain in the anus, which manifests itself especially sharply during bowel movements and in a sitting position.
Infants under 1.5-2 years old cannot talk about their problems, so parents should pay attention to the following conditions:
- causeless tearfulness
- lethargy, drowsiness, general weakness;
- crying during bowel movements and urination;
- hyperthermia;
- lack of appetite;
- redness of the skin around the sphincter;
- swelling and compaction of tissue in the anus;
- purulent discharge in stool;
- hyperemia (overflow of blood) of the vessels near the anus;
- sharp anxiety when palpating the perineum;
- swelling of the buttocks;
- anal deformation.
Characterized by retention of stool or, conversely, its dilution. In children over 1.5 years old, the gait may change - the child walks with his legs wide apart. The child prefers to sit on one, least painful buttock, or does not sit at all. While lying down, he chooses the healthy side of the body and pulls his legs towards his stomach.
The complicated form often develops gradually, and noticeable external symptoms do not appear immediately. At first there are no changes in the skin; after 5-7 days, swelling and redness of the skin of the perineum are visible. Palpation (feeling) does not give clear pain reactions from the baby.
Paraproctitis in infants can be diagnosed late due to untimely detection of fluctuations (signs of liquid contents in the infiltrate). Severe swelling of the perineum makes it difficult to determine the presence of a deep, small abscess.
An accurate diagnosis during this period can only be made by a doctor using a digital examination of the anal area.