Types of yellow discharge Possible causes of heavy yellow discharge What to do if yellow discharge appears
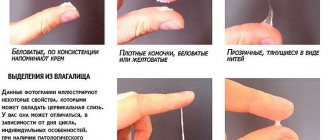
Slight white or light yellow discharge in women during the intermenstrual period is considered normal, unless there are other signs (pain, pain during urination, redness of the mucous membrane). Leucorrhoea cleanses the genital tract of dead epithelium and microorganisms and maintains normal vaginal microbiocenosis. But a change in the color of natural discharge can indicate various disorders in the body, including infectious and inflammatory processes and sexually transmitted diseases.
Causes of yellowish discharge in women
Normally, vaginal discharge may vary depending on your cycle. Sometimes there is yellow discharge in completely healthy women, but it has no odor and is not abundant. This happens at different phases of the menstrual cycle, during the release of the egg or after pregnancy. The nature of the secretory activity of the gonads is influenced by age, the presence or absence of a sexual partner, and the hormonal balance in the body.
If their appearance is accompanied by a stench, foam or a greenish tint, then the following types of pathology can be assumed:
- infections of the genitourinary system, including sexually transmitted infections;
- benign and malignant tumors;
- cysts;
- endometrial proliferation.
Light yellow, odorless discharge in women should not cause alarm. But if they begin to intensify, acquire a different shade or begin to smell unpleasant, then diagnosis of the abnormality and urgent treatment are required. If you start the disease, then you will have to pay with infertility, cycle disruption and other serious complications.
Ovarian cyst
What to do if yellow discharge appears?
If yellow discharge causes discomfort to a woman, she should consult a gynecologist for a full examination and tests. The doctor will conduct an examination using a gynecological speculum, ultrasound, and also take a smear to determine the microflora of the vagina. The results obtained will help make the correct diagnosis and determine the cause of pathological discharge.
In the presence of an inflammatory-infectious process, agents are prescribed that suppress the growth of isolated pathogenic microflora. These may be antibacterial, antifungal or antiprotozoal agents. Depending on the severity of the disease, medications can be prescribed locally or systemically.
At the same time, the doctor will recommend remedies that help restore the correct balance of microflora. If a specific pathogen is identified, treatment should be carried out by both sexual partners, and close contacts should be avoided until the end of therapy.
With or without unpleasant odor
Yellow vaginal discharge may vary in smell. Usually, a secretion that has a specific aroma indicates a disease. An experienced specialist can already recognize the type of disease by this sign:
- A sour odor is observed with thrush; it is also characterized by itching and the presence of a cheesy mass on the underwear. But sometimes the vaginal secretion smells sour when changing partners. Sometimes this feature indicates a decrease in the body's defenses.
- Yellow discharge with an odor in women is often found in the presence of a sexually transmitted infection.
- Putrid notes are given by inflammation in the vagina (colpitis) or infection with Gardnerella. The same phenomenon accompanies advanced cervical erosion or the initial stage of a tumor. At the same time, there is a discharge of ichor and pus.
- With vaginal dysbiosis, the genitals often have a fishy odor. Symptoms intensify after sexual intercourse.
Yellow discharge in women, odorless and in small quantities, is normal. But if they occur for the first time and are accompanied by other signs of inflammation or disorder, then in this case you should visit a gynecologist and get tested.
Sometimes discharge is a symptom of acute gonococcal infection and is accompanied by pain in the lower abdomen and intermenstrual blood loss. Thick, yellowish, odorless discharge occurs with chlamydia.
Causes
The reasons for the appearance of leucorrhoea of an unusual color can be natural or pathological. Yellowish discharge often occurs in diseases of the female reproductive system of an infectious and inflammatory nature. It is impossible to determine at home what triggered such changes. A woman needs to undergo a full examination in a medical facility.
Endometritis
Endometritis of the uterine cavity is an inflammatory disease affecting the inner layer of the reproductive organ. The reason for its occurrence lies in damage to the uterus by an infection (fungal, bacterial or viral). Often the pathology occurs against the background of suppressed immune system.
Initially, the inflammatory process begins in the endometrium, but after a while it penetrates deep into the organ and affects muscle tissue. If the pathology is not treated, then adhesions begin to form in the uterine cavity and peritoneum. One of the most dangerous complications of endometritis is infertility.
In addition to the appearance of copious mucus of an uncharacteristic shade during the development of the disease, the following symptoms are noted:
- nagging pain in the abdominal area;
- general malaise and weakness;
- migraine;
- sudden mood swings and depression.
Among the objective signs of endometritis are the following:
- hyperthermia, which is accompanied by chills and fever;
- vomiting and nausea;
- yellow discharge on panties;
- severe pain in the uterine area, which is felt upon palpation;
- an increase in the size of the reproductive organ.
If the inflammatory process in the uterus occurs in a chronic form, then the clinical manifestations are less pronounced. An increase in temperature is observed only occasionally. In this case, only a doctor can diagnose the pathology after conducting all the necessary studies.
Often, with endometritis, there is a disturbance in the menstrual cycle, the nature of the discharge changes, and there is an increase or decrease in the volume of blood lost. Regardless of the phase of the cycle, the woman experiences pulling pain in the abdominal area.
Vaginitis
Vaginitis is an inflammation of the vaginal mucosa. It occurs due to the penetration of yeast or bacterial infections into the reproductive system, as well as due to mechanical damage, pathologies of the thyroid gland, prolonged use of antibiotics, an allergic reaction to ointments or condoms, decreased immunity and non-compliance with the rules of intimate hygiene. Changes in hormonal levels can also provoke the development of pathology.
In addition to yellow, sour-smelling discharge, women with vaginitis often experience other symptoms. Among the main ones are:
- irritation in the intimate area in women, accompanied by itching;
- pain when urinating;
- discomfort during intimacy and the appearance of an unpleasant odor after it.
There may also be copious discharge with blood . Such symptoms cannot be ignored. You should seek help from a doctor without delay. During therapy, antibiotics and topical drugs are used.
Bacterial vaginosis
If the vaginal microflora is disturbed, the genitals are unprotected from the penetration and active reproduction of pathogenic bacteria. This is what contributes to the appearance of bacterial vaginosis.
Among the reasons that provoke the development of pathology are the following:
- hormonal disorders;
- immunosuppression;
- taking antibiotic drugs;
- diseases of the endocrine and genitourinary systems;
- neoplasms.
The infection is transmitted sexually. The main signs of the disease are profuse yellow-green discharge with a fishy odor. As a rule, this intensifies after intimacy.
During pregnancy, the disease can cause miscarriage or premature birth. If pathogenic bacteria penetrate the cavity of the reproductive organ, there is a risk of developing endometritis.
Salpingitis
With this pathology, the inflammatory process occurs in the fallopian tubes. In the acute form of the disease, mucous discharge has a rich yellow color and becomes abundant. In the case of a chronic course, the volume of secretion decreases significantly. Painful sensations appear during sex, and after sex the discharge sometimes contains blood impurities.
Salpingitis causes symptoms such as:
- pain in the lower abdomen during the period of regulation;
- painful urination;
- lack of appetite;
- flatulence.
If the secretion acquires an unpleasant odor, this indicates that purulent serous fluid has accumulated in the uterine tubes.
The disease needs treatment. In the absence of proper therapy, complications such as the formation of adhesions and scars, as well as infertility, are observed.
STI
Discharge in women that is yellowish in color and odorless appears in diseases that are sexually transmitted. This symptom is nonspecific and does not belong to diagnostic criteria. It is taken into account only in combination with other clinical manifestations, such as:
- abdominal discomfort:
- burning and itching;
- menstrual bleeding outside the period of critical days;
- painful sensations during intimacy;
- liquid discharge after sexual intercourse.
Various sexually transmitted infections can cause similar symptoms:
- Gonorrhea. The first signs of the disease are observed a week after infection, but in some cases the pathology can be asymptomatic for up to one month.
- Trichomoniasis. This disease is considered one of the most common. In addition to the main symptoms, when it develops, swelling of the genitals and pain during urination are noted.
- Chlamydia. A common pathology that annually affects up to 10% of people of reproductive age. In addition to the yellow secretion secreted from the vagina, this disease causes discomfort in the abdomen, itching and burning in the intimate area, a general deterioration of the condition and a slight increase in body temperature.
Cervicitis
Cervicitis is a disease in which the inflammatory process occurs in the cervix. It occurs due to the penetration of infections, bacteria or viruses into the canal. Clinical manifestations directly depend on the form of pathology.
In the acute course of the disease, pain appears in the lower abdomen, itching and viscous, snot-like, yellow discharge, the mucous membranes of the genitals become swollen and inflamed.
Chronic cervicitis manifests itself in the form of a scanty secretion with a yellowish tint and slight swelling of the cervix. In the absence of proper treatment, thickening of the cervical walls and the formation of erosions are noted.
If accompanied by itching
When yellow discharge and itching appear in women, this is almost always a sign of illness. Most often this is observed in the following cases:
- Vaginitis caused by a fungal infection. Candidiasis occurs against a background of weakened immunity, as a result of trauma to the mucous membrane, hormonal imbalance or long-term use of antibiotics. Very often occurs during pregnancy and in women of childbearing age.
- Foamy yellow discharge and itching are often a sign of trichomoniasis infection. At the same time, swelling of the genital organs, redness and irritation occurs.
Control after treatment of discharge
At the end of the course of therapy for a sexually transmitted infection, the patient undergoes tests so that the specialist can monitor the effectiveness of taking the drugs.
If at this stage the pathology does not manifest itself, this does not mean that the patient has recovered.
Some infectious pathologies can take a latent form, and after some time relapse, causing the inflammatory process again.
Even if the infection is latent and does not cause manifestations of the disease in the patient, he still remains dangerous to others.
As a rule, the patient should undergo control tests two weeks after he finishes taking drugs that have a detrimental effect on bacteria.
- If the patient has undergone a course of therapy for ureaplasma and mycoplasma infections, then control should be carried out one month after the last dose of the antibiotic.
- If treatment was carried out due to the presence of gonococcal infection, then tests are taken twice: 2 days after the end of the course of therapy and again two weeks later.
Read also HPV in men: symptoms, types of viruses and treatment
In the event that negative test results for infections are obtained, the doctor declares the patient healthy.
If there is a positive test, you will need to take another course of stronger drugs.
The reasons for obtaining a positive result may be due to the following factors:
- if the patient did not comply with the medication regimen prescribed by the doctor
- development of resistance of microorganisms to drugs
- presence of medical error
Based on this, patient compliance with the rules for taking prescribed medications plays an important role in treatment:
- Compliance with the dosage prescribed by the doctor. The dose is selected by the doctor, and changing it at your own discretion is strictly not recommended;
- No missed medications. During treatment, all medications must be taken on time and at certain intervals;
- The course must be completed from beginning to end. Under no circumstances should you stop taking medications, even if it seems that all the symptoms have already passed;
- If the pharmacy does not have this medicine, then it cannot be replaced with an analogue, even if the pharmacy worker tries to convince the patient that these are the same medicines;
- The medications should be taken in full, and not just those that the patient likes.
Regarding the presence of a medical error, it is better to undergo treatment from experienced specialists.
Copious discharge
In the absence of pathology, an increase in the amount of vaginal secretion occurs during sexual arousal, ovulation and before the onset of menstruation. This phenomenon goes away in a couple of days and is not considered a deviation.
The complete absence of discharge may indicate atrophy of the glands, which is often observed with long-term chronic infections or during menopause. This also happens when a woman abuses hygiene procedures using chemicals and constant douching.
Very profuse yellow discharge is characteristic of the following diseases:
- salpingo-oophoritis;
- salpingitis;
- adnexitis.
All these deviations relate to inflammation of the internal genital organs. The reason for this is pathogenic or conditionally pathogenic flora. Often, high activity of staphylococci accompanies profuse, odorless, yellow discharge. And if a specific infection is added to this, then they begin to smell unpleasant.
Inflammation of the appendages and uterus
Prevention of yellow discharge
Many problems in the field of gynecology can be avoided by following simple recommendations:
- Do not skip preventive examinations with a gynecologist. They should occur every six months.
- Lead a healthy lifestyle, play sports, adhere to the principles of proper nutrition. Many foods, as well as alcohol, negatively affect the condition of the mucous membranes and microflora of the vagina.
- Have sex with a regular partner or use barrier methods of contraception.
- Follow the rules of personal hygiene - take a shower as needed, and also use special products for the intimate area.
- Try to avoid hypothermia, and also take care of the state of your general immunity.
- Wear underwear made from natural fabrics, preferably white, as dyes can cause allergic reactions.
- Do not overuse douching and do not self-medicate. This can lead to the removal of beneficial microflora and the active proliferation of pathogenic ones.
Vaginal discharge of other colors
The above information explains how yellow discharge appears in women, as well as the main reasons for this phenomenon. But they do not always have exactly this color. When does white, brown or green discharge occur?
White
Some women consider the appearance of vaginal secretions as a pathology. However, this is a normal physiological phenomenon, like sweat, saliva or gastric juice. White, cream or light yellow discharge is normal under the following conditions:
- have a faint color;
- the daily volume does not exceed one teaspoon;
- without smell;
- watery consistency.
In the event that it turns into bloody, brown, greenish or bright yellow discharge, acquires an unpleasant odor or begins to resemble curdled flakes, you need to go to the doctor. This often happens with a variety of specific and nonspecific infections. A whitish tint with the addition of gray indicates bacterial vaginosis.
Brown
Secretions from a woman's genitals that are brown or red in color indicate the presence of blood. This is not considered a problem if it occurs a couple of days before or a few days after your period, replacing the usual white or yellow mucous discharge. In some women, this phenomenon may occur after the installation of the IUD or in the middle of the cycle, which corresponds to the ovulation process.
A signal of pathology is excessive smearing or bleeding, the appearance of red, brown or black spots on the underwear, regardless of the cycle. This may be a signal of the formation of a tumor, papilloma or cyst, exacerbation or appearance of endometriosis or cervical erosion. In pregnant women, this may indicate a threat of miscarriage.
Greens
Abundant odorless yellow discharge, as well as unpleasant-smelling discharge with a green tint, clearly indicates the presence of pathological processes. They are often symptoms of chlamydia, trichomoniasis or thrush accompanied by a bacterial infection. They lose their mucous character and become cloudy due to the abundance of white blood cells as a sign of inflammation. At the same time, there is itching, pain in the lower abdomen and lumbar region.
When secretion is normal
Sometimes yellow vaginal mucus occurs after sexual intercourse. If it appears after unprotected sexual relations, then the cause is the mixing of physiological female secretions and the partner’s ejaculate. The discharge returns to normal after about 8 to 10 hours. If the secretion turns yellow after using a condom, the cause is the active activity of the vaginal glands that produce natural lubrication.
Other reasons for the appearance of yellowish leucorrhoea include:
- unbalanced diet - the presence of a large amount of spicy, fatty, acidic foods in the menu can cause changes in the composition of secretion;
- hormonal imbalance;
- the period before and after the end of menstruation;
- ovulation period - the appearance of a thick and abundant secretion of a yellow-transparent color indicates the release of an egg ready for fertilization;
- taking oral contraceptives, accompanied by rapid changes in hormonal levels, a woman often notices scanty yellowish discharge;
- frequent change of sexual partners - such a modification of mucus is a reaction of adaptation of the vaginal environment to the new microflora of the partner.
Treatment
Considering that most of the reasons why spotting appears after sex, as well as white discharge after sex, are quite serious diseases, the doctor determines the treatment after examination and special tests.
If brown discharge after sex is due to mechanical damage to the vagina or this occurs shortly before or after menstruation, then there is no need to take any measures. This may be a normal state of the body in the latter situation. In the case of a mechanical injury, a healthy body is able to quickly recover on its own.
In other cases, treatment is as follows:
- To treat chlamydia, drugs with antibiotic action are used, which are selected individually. Only a doctor can do this. At the same time, we must not forget that both partners must undergo the treatment process to prevent relapse;
- vaginitis, cervicitis and similar diseases require tests to study the composition of the microflora. Some cases of the disease require radio wave exposure in addition to the use of medications;
- if the cause is oncology, then it is necessary to perform a puncture and undergo a number of other tests. A surgeon will most likely be required to remove the affected area.
Leucorrhoea depending on the phase of the female cycle
The nature of leucorrhoea, its structure and quantity depends on the phase of the menstrual cycle. Why does yellow discharge appear in teenage girls? Leucorrhoea without a particular odor appears approximately 10–12 months before the first menstruation, which indicates the beginning of preparation for reproductive activity.
What does white-yellow discharge indicate during ovulation? Moderate leucorrhoea indicates the maturation of the cells; as the date of menstruation approaches, their quantity increases, but at the same time they become more liquid.
The week before menstruation, the amount of leucorrhoea becomes maximum, and if a woman is depressed or stressed, the volume of dark yellow discharge increases noticeably.
Important! Yellow leucorrhoea often occurs as a result of allergies to pads, tampons, underwear, and contraceptives.
Normally, yellow leucorrhoea before menstruation should be uniform, without clots, and their amount should not exceed 4–6 ml. If yellow discharge is accompanied by pain and burning, or its volume significantly exceeds the norm, you should consult a specialist.
Diagnostics
If yellow discharge is detected in women with or without itching, then in any case it is necessary to seek help from a gynecologist. In addition, inoculation of secretions on biological media with determination of sensitivity to antibacterial drugs is indicated, so that upon receiving the results, it is possible to immediately begin treatment, which will be aimed at eliminating the specific pathogen. It should be noted that some STD pathogens cannot be detected by inoculation on nutrient media, and the use of PCR techniques is indicated for their determination.
Another necessary study is ultrasound - it helps to identify the localization of the pathological process, as well as determine the degree of its prevalence.
In what cases will the discharge have a yellow-greenish tint?
- Colpitis is a disease in which there is an inflammatory process on the vaginal mucosa and can have a variety of origins. The discharge can be not only dark yellow, but also green - everything is determined by the etiological factor (in case of an infectious lesion, this color is observed).
- Oophoritis is an infectious pathology in which the process affects the ovaries. Pathogenic microorganisms that provoke the development of this pathology are Trichomonas, gonococci and chlamydia. The cause of the disease may also be the penetration of a nonspecific infection from the abdominal cavity.
Recommendations for home treatment
The patient needs to analyze her diet. Poor nutrition can cause imbalance in the intimate sphere. You should completely avoid fast food, fatty foods and canned foods. Vegetable juices with the addition of herbs - parsley, spinach, sorrel - are useful. Juices even out the pH balance of the vagina.
However, store-bought fruit juices are harmful because they contain large amounts of sugar. Eat more berries, especially sour ones: viburnum, barberry. Strawberries and blueberries are a real storehouse of vitamins.
Intimate hygiene must be carried out competently. It is harmful to wash yourself more than twice a day - this washes away the protective layer of the genital mucosa. Instead of soap, it is better to use special products that contain lactic acid.
Why is it important to come for a follow-up examination after a course of treatment?
In some cases, pathogens are not completely destroyed during a course of antibiotic therapy. A small pool of bacteria remains, and they will already be resistant to the action of the applicable drug. That is why, in order to avoid a relapse of the disease caused by these microorganisms, a repeat visit to the doctor is indicated upon completion of therapy. Even if no greenish discharge or any other symptoms are noted, a follow-up examination is still necessary so that all the treatment performed is not in vain.
Discharge during menopause
During menopause, the activity of hormones decreases, and less natural lubricant is released - this leads to frequent exacerbation of gynecological diseases during menopause. After 55 years, the functions of the ovaries completely decline; the discharge should be transparent, homogeneous and not watery. All discharges of a different nature indicate the presence of pathologies.
Causes of yellow leucorrhoea during menopause:
- sexually transmitted diseases, thrush;
- benign neoplasms of the uterus or cervix;
- hormonal disorders;
- oncological diseases.
With the onset of menopause, a woman should more carefully monitor the condition of her body, regularly visit a gynecologist, and follow all his appointments.
Bloody secretion
Blood after sex can scare anyone. The reasons for the appearance of bloody secretions may be as follows:
- Microscopic injuries. Even with lubrication, the vaginal lining remains vulnerable to damage. In addition, women often have insufficient discharge when there is little sexual arousal. This is especially common during pregnancy, menopause and under stress. Rough sex and the use of low-quality condoms can also damage the vaginal walls.
- Hormonal contraceptives are considered one of the most reliable remedies against unwanted pregnancy. They contain substances that help thin the endometrium. This is done to prevent the fertilized egg from implanting into the uterine wall. Therefore, any impact during intimacy can cause damage, which is accompanied by a brownish secretion. There should be no pain felt.
- Pseudomenstruation. Characterized by intermittent bleeding that appears suddenly. Most often this happens during menopause, pregnancy and hormonal imbalance. Sex only provokes this process. With it, the uterus begins to contract vigorously, throwing out a small amount of blood.
- Ovulatory period. Women who dream of a child specially calculate favorable days for conception. The best time for this is ovulation. Usually it occurs in the middle of the cycle, but there are exceptions. In this case, blood appears due to the rupture of the follicle when the mature egg is released. Sexual intercourse does not affect this process in any way, but may well coincide with it.
- Postpartum period. After childbirth, the uterus is cleared of traces of the fetus. At first, this is accompanied by bleeding. But after a few weeks it decreases and you can start having sex again. It should be borne in mind that after the act, discharge may intensify due to uterine contractions.
- Deviations in men. Men are susceptible to pathologies of the reproductive system no less than women. In some cases, blood is released from the penis. It can enter a woman’s body through unprotected sex. After which it is released along with female secretion, which takes on a pinkish color. In this case, the bloody smear lasts no longer than 1 hour. This phenomenon requires contacting a urologist for a men’s health examination.
- Deflowering. Girls often have bloody discharge after the first act. This is a natural process and occurs due to rupture of the protective film. The spotting after the first sex can last for a couple of hours.
- Anal sex. This type of sexual intercourse is gaining popularity. And this despite the fact that it is accompanied by unpleasant consequences, which also include bleeding. Complications arise due to the fact that the intestine is not designed for this. This process exposes it to tension, which can cause bleeding cracks.
- Orgasm is also thought to be the cause of brown or red discharge. At this moment, the uterus begins to actively contract. If your period is due any day now, orgasm can speed it up.
- Pregnancy. During this period, sexual intercourse often causes the release of bloody mucus. In the early stages, this occurs due to the friability of the endometrium, and in the later stages - due to high susceptibility to injury. In addition, when the water breaks, secretion of a liquid or mucous consistency interspersed with blood is observed.
Skin lesions: curdled discharge with itching
A sharp increase in fungi is the causative agent of irritation of the skin of the genital organs. By attacking the surface of the mucous membrane, microorganisms can cause not only the described discharge, aggravated by itching, burning and swelling, but also changes in the skin in the groin area.
Prolonged ignoring of the problem aggravates the anamnesis with the appearance of small but clearly visible blisters containing a thick, mucus-like substance. Damage to such formations leads to the appearance of impurities in white cheesy discharge, visually similar to blood. These skin defects are a serious reason to contact a specialist.