Pulmonary atelectasis is a rather dangerous disease in which there is airlessness in the lung tissue. This means that there is insufficient expansion or diffuse collapse of the tissues of this organ. There are a large number of predisposing factors that lead to the development of such a disease, ranging from congenital anomalies to many years of addiction to smoking cigarettes.
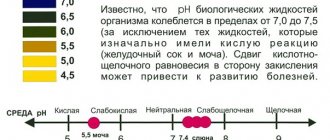
- Etiology
- Classification
- Symptoms
- Diagnostics
- Treatment
- Complications
- Prevention
The clinical picture is dominated by specific symptoms, which are expressed in pain in the sternum, shortness of breath and cyanosis of the skin.
It is possible to make a correct diagnosis based on a physical examination and instrumental examinations of the patient. Treatment of pulmonary atelectasis is often conservative, but in advanced forms surgery may be necessary.
The International Classification of Diseases identifies its own significance for such pathology. The ICD-10 code is J98.1.
Kinds
Congenital
Most often detected in weak and premature children due to immaturity of the lung and bronchial tissue, blockage with mucus or amniotic fluid. If a small area of the lung is involved, then after a certain time it straightens out on its own; with extensive collapse, the prognosis is poor.
Acquired
Develops due to many reasons:
- If it develops as a result of bronchial obstruction, it is called obstructive.
- And if it’s from compression of the lung tissue, then it’s compression atelectasis.
Atelectasis in children. Features in newborns
In children, symptoms and developmental mechanisms are the same as in adults. But when it comes to infants, things are different. Why does atelectasis develop in young children? Most often, this condition accompanies premature babies (children born prematurely) or children with developmental defects (improperly formed organs, such as the lungs).
The occurrence of atelectasis is associated with the entry of meconium (the so-called feces of a newborn), amniotic fluid, and mucus into the respiratory tract. In premature babies, the surfactant layer may not be sufficiently developed (a special substance that covers the structures of the lung and is involved in the act of breathing, helps to hold the frame of the alveoli, preventing them from “collapsing”). Possible head trauma during childbirth and damage to the respiratory center in the brain.
Causes
- Diseases: bronchial asthma, cystic fibrosis, tuberculosis, neuromuscular diseases, cancer, lymphadenopathy, pneumonia, myocardial hypertrophy, anomalies in the development of large vascular trunks, pathology of the inner wall of the bronchi, phrenic nerve palsy, scoliosis, sepsis.
- Other conditions: general anesthesia, a large amount of oxygen in the mixture for artificial ventilation of the lungs, acute lung collapse, increased pressure in the pleural cavity (pneumothorax, pleural empyema, chylothorax, hydrothorax and hemothorax, the presence of effusion), taking a significant amount of sedatives, hypothermia, prolonged immobility, foreign body in the lumen of the bronchus, traumatic injury and much more.
Risk groups include smokers, overweight people, people with chronic obstructive pulmonary diseases, severe forms of tuberculosis, and those who have undergone surgery on the chest organs.
Signs of pulmonary atelectasis
The severity of the symptoms, due to which one can suspect the occurrence of atelectasis in the lungs, depends on a number of reasons:
- The rate of compression of lung tissue (acute and gradually increasing atelectasis are distinguished);
- Volume (size) of the respiratory surface of the lungs turned off from ventilation;
- Localizations;
- The mechanism of occurrence.
Dyspnea
It is characterized by an increase in the frequency of inhalation and exhalation per minute, a change in their amplitude, and arrhythmia of respiratory movements. Initially, the feeling of lack of air occurs during physical activity. With increasing or initially large area of atelectasis, shortness of breath appears at rest.
Chest pain
Optional attribute. Appears most often when air enters the pleural cavities.
Change in skin color
Caused by excess carbon dioxide in tissues. In children, first of all, the nasolabial triangle turns blue. In adults, blueness of the fingers of the extremities (acrocyanosis) and the tip of the nose appears.
Changes in the performance of the cardiovascular system
- Pulse increases (tachycardia);
- After a short-term increase in blood pressure in the initial stages, it decreases.
In children, the indicated symptoms are also observed, which are most clearly manifested in newborns with primary atelectasis. These are accompanied by easily observed retractions of the intercostal spaces when inhaling from the side of the affected lung, as well as retractions of the sternum when air enters the lungs.
Pathogenesis
Compression atelectasis has a more favorable course than obstructive atelectasis. Compression of the lung tissue occurs due to increased pressure inside the pleural cavity (tumors of the mediastinum, accumulation of fluid, blood, pus), while there is no intrabronchial pathology, therefore, when the cause is eliminated, the lung straightens and restores its functions even after prolonged compression.
With obstructive atelectasis, complete or partial closure of the bronchial lumen occurs (sputum, tumor, foreign body, mucus). Congestion develops, blood circulation and lymphatic drainage are significantly impaired, which causes pulmonary edema. Pneumonia and sclerosis of the lung tissue occur at the site of the collapse. This type of atelectasis must be eliminated within three days to restore the function of collapsed lung tissue.
In some cases, there is a mixed mechanism of occurrence (for example, pulmonary atelectasis in tuberculosis around the cavernous cavities), when obstructive and compression components are combined.
Classification of pulmonary atelectasis
Depending on the order of involvement of the lungs in the pathological process:
Primary (congenital)
It occurs in children, most often immediately after their birth, when the lungs do not fully expand with the first breath. In addition to the already described intrauterine anomalies in the development of the lungs and insufficient production of surfactant, the cause of its occurrence can be aspiration of amniotic fluid, meconium. The main difference between this form is the initial absence of air from the environment entering the collapsed area of lung tissue.
Secondary (acquired)
This form of atelectasis occurs as a complication of inflammatory and tumor diseases of organs, both respiratory and other systems, as well as with chest injuries.
Various forms of pulmonary atelectasis
According to the mechanism of occurrence, acquired forms of atelectasis are distinguished:
Obstructive atelectasis
It is observed when the cross-sectional area of the bronchus decreases for the reasons stated above. Obstruction of the lumen can be complete or partial. Sudden closure of the lumen when a foreign body enters requires immediate action to restore the patency of the bronchial tree for the reason that with each hour of delay the likelihood of straightening the collapsed section of the lungs decreases. Restoration of lung ventilation in cases where complete obstruction of the bronchus lasted more than three days does not occur.
Compression atelectasis
Occurs when there is a direct impact on the lung tissue itself. A more favorable form, in which complete restoration of pulmonary ventilation is possible even after a fairly long period of compression.
Functional (distensional) atelectasis
Occurs in areas of physiological hypoventilation (lower segments of the lungs):
- In bedridden patients;
- Those who have undergone severe and prolonged surgical interventions;
- In case of overdose of barbiturates, sedatives;
- With arbitrary limitation of the volume of respiratory movements, which is caused by severe pain (rib fractures, pleurisy, peritonitis);
- In the presence of high intra-abdominal pressure (ascites of various origins, chronic constipation, flatulence);
- With diaphragmatic paralysis;
- Demyelinating diseases of the spinal cord.
Mixed atelectasis
With a combination of different mechanisms of origin.
Depending on the level of bronchial obstruction and the area of lung collapse, the following are distinguished:
- Lung atelectasis (right or left). Compression at the level of the main bronchus.
- Lobar and segmental atelectasis. Lesion at the level of the lobar or segmental bronchi.
- Subsegmental atelectasis. Obstruction at the level of the bronchi of the 4th-6th order.
- Discoid atelectasis. Disc-shaped atelectasis develops as a result of compression of several lobules located within the same plane.
- Lobular atelectasis. Their cause is compression or obstruction of the terminal (respiratory) bronchioles.
Symptoms
Clinical manifestations depend on the size of the affected area and the rate of collapse of the lung tissue.
Small atelectasis, microatelectasis, and also slowly developing ones are often asymptomatic.
With extensive atelectasis with fulminant development, symptoms of acute respiratory failure occur:
- severe, sudden shortness of breath;
- chest pain on the affected side:
- drop in blood pressure;
- cyanosis;
- cough;
- tachycardia.
In addition, during percussion examination, dullness of sound is noted over the focus of atelectasis. Breath sounds in this area are not audible; moist rales, harsh and bronchial breathing may appear. An external examination reveals a lag in the affected half of the chest during breathing.
Prognosis for pulmonary atelectasis
Sudden simultaneous total (subtotal) atelectasis of one or two lungs, which develops as a result of trauma (air entering the chest) or during complex surgical interventions in almost all cases ends in death immediately or in the early postoperative period.
Obstructive atelectasis, which developed due to sudden blockage by foreign bodies at the level of the main (right, left) bronchi, also has a serious prognosis in the absence of emergency assistance.
Compression and distension atelectasis that developed during hydrothorax, with the removal of the cause that caused them, do not leave any residual changes and do not change the volume of the vital capacity of the lungs in the future.
Associated pneumonia can significantly change the prognosis for the restoration of the functions of a compressed lung, which in these cases leaves scar tissue replacing the collapsed alveoli.
Diagnostics
An X-ray of the lungs allows you to fully confirm the diagnosis of atelectasis, establish the exact location of the lesion and the extent of the lesion. Therefore, after examination, collection of complaints and medical history, the patient is first sent for an X-ray examination, which is carried out in two projections.
X-ray: Atelectasis of the lung
Atelectasis of the lung on an x-ray image looks like an area of intense uniform darkening, the root of the lung and mediastinal organs are shifted to the affected side. The diaphragm on the side of atelectasis is raised and the organs located under it are also raised. Unaffected parts of the lung look swollen (cleared), sometimes the lung is swollen on the opposite side.
For example, atelectasis of the upper lobe of the right lung will look like a large focus of darkening on the right, triangular in shape, the apex facing the root of the lung, and the apex facing the chest wall. The unaffected part of the lung tissue has a characteristic clearing, more pronounced in the part immediately adjacent to the pathology zone; the pulmonary pattern is depleted. The upper lobe of the right lung is displaced upward, inward and forward. Atelectasis of the lower lobe of the right lung also has the appearance of a triangular shadow, the apex is adjacent to the root, and the base is facing the diaphragm. The displacement of the lower lobe goes downwards, inwards and backwards.
Small atelectasis (lobular, acinous) are most often multiple; on an X-ray image they are difficult to distinguish from focal pneumonia, especially if they are combined with it.
Sometimes discoid atelectasis occurs; in the picture it looks like a dark transverse stripe located low near the diaphragm.
In severe cases, computed tomography is additionally performed. Atelectasis must be differentiated from oncological processes in the mediastinum, diaphragmatic hernia, pulmonary cysts, and pleurisy. It is important to determine not only the presence of recession, but also to identify the underlying cause.
Causes of atelectasis
The main cause of atelectasis is blockage of the bronchus, which is a branch of the trachea leading to the lungs. Smaller airways may also become blocked. The blockage can be caused by a tumor, mucus plug, or foreign body. Also, the bronchus can be blocked from the outside due to its compression by enlarged lymph nodes or a tumor.
Most often, acquired pulmonary atelectasis can develop with:
- hydrothorax, exudative pleurisy, pneumothorax due to the accumulation of fluid or air in the pleural cavity;
- pulmonary tuberculosis due to compression of the bronchus by enlarged lymph nodes or the breakthrough of caseous masses into it, which clog its lumen;
- malignant neoplasms in the lungs due to compression of the bronchus;
- blockage of the bronchus by a foreign body;
- chronic pneumonia due to reactive enlargement of the lymph nodes of the root of the lung;
- sclerotic bronchitis;
- blockage of the bronchial tube with mucus after surgery in case of disruption of the drainage function of the bronchi (more often occurs after operations on the chest and abdominal cavity);
- injuries due to compression by air or lung blood pouring into the pleural cavity during traumatic pneumothorax;
- in case of traumatic damage to the bronchi due to blockage of the bronchus by aspirated vomit or mucus against the background of a suppressed cough reflex or shallow breathing;
- the rapid movement of a jet plane in pilots due to the closure of small airways.
In adults, microatelectasis may develop due to severe general infection and prolonged oxygen therapy, which can lead to damage to the alveolar mucosa.
Atelectasis of newborns can be caused by inhalation of amniotic fluid, insufficient surfactant, incomplete expansion of the pulmonary vessels, weakened breathing and a weak cry at birth.
In healthy newborns, atelectasis may occur in the first few days of life. Then it goes away on its own, so it is considered physiological.
Treatment
Treatment tactics depend on the type of atelectasis and the cause that caused it. Therapy is aimed at restoring the function of the collapsed area and straightening it out.
If atelectasis is caused by compression, then it is necessary to normalize the pressure in the pleural cavity: drugs that reduce pleural effusion are used, blood, air, pus and other foreign substances are removed. In case of bronchial obstruction, it is cleansed using a bronchoscope: mucus, sputum, blood, foreign bodies, caseous masses in tuberculosis are removed. After which they rinse with a solution of antiseptics and antibiotics, and introduce mucolytic drugs.
Inhalation of a moistened oxygenated respiratory mixture, camphor preparations, caffeine, cordiamine, salbutamol, and therapeutic breathing exercises are prescribed. In severe cases, it is necessary to transfer patients to mechanical ventilation. A course of broad-spectrum antibiotics is required. A special position for the patient is necessary: the head end of the bed is lowered so that the affected area is located above the trachea. After surgery, it is necessary to ensure physical activity as soon as possible.
In some cases, surgical treatment of pulmonary atelectasis is required (for bleeding, suppuration). In this case, the affected area is excised.
Therapeutic tactics for atelectasis
Treatment of pulmonary atelectasis comes down to eliminating the root cause:
- removal of foreign bodies from the bronchus;
- operations for tumors and sclerotic changes;
- suction of the mucous component from the bronchi (in newborns, patients with bronchial asthma);
- surfactant preparations;
- bronchoalveolar lavage (washing the bronchial tree from mucus);
- drainage of the pleural cavity (for hemo-, pneumothorax);
- inhalation of drugs;
- bronchodilators;
- administration of enzymes;
- general methods (massage, breathing exercises, etc.).
Prognosis and complications
The prognosis directly depends on the disease that provoked the appearance of atelectasis, as well as on the localization of the lesion (in the middle lobes it is more difficult to restore oxygenation due to the structural features of the bronchi communicating with them). Total lung lesions are usually fatal.
Compression atelectasis has a favorable prognosis; if the cause is eliminated, the lung quickly expands and completely restores all gas exchange functions. With obstructive atelectasis everything is more complicated, especially if it is associated with the presence of a malignant tumor. The following complications often occur:
- addition of an infectious process;
- the occurrence of bronchiectasis;
- sclerosis, fibrosis, scar changes in lung tissue (if the process persists for more than six months);
- lung abscess;
- pneumonia.
When an infection occurs, a rise in temperature and purulent sputum appear. The incubation period depends on the type of microorganism that caused this inflammatory process. Most often this is a conditionally pathogenic flora, nosocomial infections. A lung abscess is very dangerous, which without timely treatment can lead to generalization of the process and sepsis. Possible formation of a broncho-pleural fistula.
Chronic, protracted microbial processes with multiple relapses lead to changes in the structure of the lung tissue; it becomes denser and cannot carry out full gas exchange. The consequence is a decrease in the usable area of the lungs and the development of chronic respiratory failure.
What is atelectasis?
Atelectasis is a pathology in which the lung or its lobes lose their volume and collapse, reducing (sometimes significantly) its surface area suitable for breathing and gas exchange.
The pathological condition of pulmonary atelecase is directly opposite to emphysema. If with emphysema the lungs are pathologically swollen, then with atelectasis they appear abnormally collapsed. At the same time, the pulmonary vesicles and small bronchi, and in the most intense cases even large bronchi, are deprived of the air they contain.
However, the atelectatic parts of the lungs in their thinner structure are not changed, but are transformed into airless dense tissue. This can occur in the left and right lungs, in the upper, middle and lower lobes.
X-ray of pulmonary atelectasis
Fibroatelectasis is a form of disease in which collapsed lung tissue is replaced by connective tissue.
Determination of discoid atelectasis in the lung, whether it needs to be treated
The word atelectasis has Greek roots, it was formed from two Greek words: “ateles” - incomplete, unfinished, unfinished and “ectazis” - stretching, stretching.
This is a condition when the respiratory organs cannot fully expand after inhalation, they completely collapse, the breathing surface decreases, gas exchange is disrupted, and oxygen deficiency occurs.
The most common form of this disease is discoid atelectasis of the lung. The lumen of the alveoli loses its airiness, collapses, and severe dysfunction of the respiratory organs occurs, including death. The patient needs timely treatment to avoid serious consequences.
Atelectasis should be distinguished from foci of low physiological ventilation, when a person is not sick, is at rest and does not require vigorous oxygen consumption.
DISCID ATELECTASIS OF THE LINGULAR SEGMENTS OF THE LEFT LUNG.
"Otorhinolaryngology / Pulmonologist"
What is tuberculosis?
Since October 2015, there have been complaints of burning pain in the chest. Pain appeared in the area of the right shoulder blade. The pain is not associated with movement. Worsened when swallowing.
11/25/2015 - CT scan of the chest with contrast:
On the left is discoid atelectasis of the lingular segments of the lung.
No focal, infiltrative changes in the lungs were detected. Roots are structural. The pulmonary pattern is not changed. The diaphragm is positioned normally. The lumens of the trachea, main, lobar, segmental bronchi are preserved. The mediastinum is not expanded, not mixed. No enlargement of the lymph nodes of the mediastinum and roots of the lungs was noted. Supraclavicular and axillary lymph nodes are not enlarged. The pleura is not changed. The boundaries of the heart are not expanded. No effusion is detected in the pericardial cavity. The pulmonary arteries are contrasted evenly. The soft tissues of the chest are not changed. No bone destructive changes were detected.
Conclusion: no foci of neoplastic process were identified in the organs of the thoracic cavity.
Blood (general clinical analysis):
Erythrocyte sedimentation rate (ESR) – 4 mm/h;
Red blood cells – 4.24 x109
Blood sugar level – 4.4 mmol per liter
MRI of the brain - without pathologies.
What can be said about this and what other examinations need to be completed?
I am attaching the CT archive. I don’t have previous fluorograms due to the move.
You made me very happy with the absence of atherosclerosis. It’s so interesting to look deep into yourself through the eyes of a specialist, and with such an accessible explanation.
I monitor breast formations on an ultrasound scan every six months - I’ve had them for a long time.
Today's symptoms:
What began in September as right-sided neuropathy, at the end of October it moved to the left - burning (like bee stings) pain in the interscapular region, in the area of both shoulder blades and deep into the chest. They are periodically sharp, and when not sharp, then aching-pressing or a sensation of being pricked by a needle in different places (sometimes as if the needle is picking out something), and then like a crawling sensation. Breathing deeply does not hurt, only sometimes it intensifies the burning sensation in the shoulder blades and upper forearm (when they already hurt).
Burning sensation in both forearms. There were spasms in the muscles of the arms (as if they were petrified and hurt later). Passed after mydocalm.
Sometimes the sacrum hurts - then there is a burning sensation in the thighs, knees and perineum, a burning sensation in the back of the calves (like mustard plaster). There were days when it was a little painful to step on my foot in the morning and there was a tingling sensation in the ankle joint. The next day it could go away and not bother me for a week. Sometimes the muscles of the neck cramp and then the back of the head burns, there is a tingling in the tip of the tongue and in the right throat, the jaw ache. But then he lets go.
These are such broad and incomprehensible symptoms. The neurologist is tired of me - she says we need to look for a neuroinfection. The infectious disease specialist suggested a mixed infection that could have been caused by a tick. He says that, among other things, there may be Bartonella, which gives neurological symptoms. In Ukraine, they do not test for all types of mixed infections (only two types are available). He suggests taking antibiotics preventively.
Thank you very much again. I will now attach the archives of CT 2010 and MRI of the spine 2019.
Risk factors
Factors that increase the risk of atelectasis include:
- Age – under 3 years or over 60 years.
- Any condition that interferes with spontaneous coughing, gaping, and breathing.
- Bed restriction with infrequent position changes.
- Impaired swallowing function, especially in older people - aspiration of secretions into the lungs is a major source of infection.
- Lung diseases such as childhood asthma, COPD, bronchiectasis or cystic fibrosis.
- Premature birth.
- Recent abdominal or chest surgery.
- Recent general anesthesia.
- Weakness of the respiratory muscle due to muscular dystrophy, spinal cord injury, or other neuromuscular disease.
- Any cause of shallow breathing, including medications and their side effects, or mechanical restrictions such as abdominal pain or a broken rib, for example.
Diagnosis of pathology
Primary diagnosis primarily involves taking a medical history along with a physical examination, assessing the condition of the skin, and measuring the patient’s pulse and blood pressure. The main method for diagnosing atelectasis syndrome is x-ray. X-rays show signs of collapse of lung tissue, which include:
- The presence of a homogeneous darkening in the affected area. Its size and shape may vary and depend on the type of pathology. The presence of extensive eclipse detected by x-ray indicates lobar atelectasis of the lung.
- Presence of organ displacement. Due to the pressure exerted by the affected side, the organs located between the lungs are shifted towards the healthy area.
Diagnosis of pulmonary atelectasis is quite simple. X-rays make it possible to detect exactly where organs are displaced during breathing, as well as during coughing. This factor also determines the type of disease. Sometimes x-rays are supplemented with computed tomography or bronchoscopy. The level of lung damage, along with the degree of deformation of the bronchi and the condition of the blood vessels, is determined by bronchography, and in addition, angiopulmonography.
Treatment of pulmonary atelectasis should be comprehensive and timely.
Epidemiology
According to the American Journal of Respiratory and Critical Care Medicine, pulmonary atelectasis after inhalation anesthesia occurs in 87% of cases in American surgical patients, and in 54-67% in Canadian surgical patients. The incidence of this pulmonary complication after open cardiac surgery in developed countries is currently 15% with a patient mortality rate of 18.5%, which is 2.79% of the total mortality from complications of surgical interventions.
Over the past 20 years, the number of premature newborns, according to WHO, has been steadily increasing throughout the world. Premature births (occurring before the 37th week of gestation) account for 9.6% of 12.6 million births per year. However, this indicator differs in different regions, with the highest proportion of preterm births observed in Africa (11.8%), and the lowest in Europe (6.3%).
In the United States, neonatal respiratory distress syndrome is one of the five most common causes of infant death, accounting for 5.6% of deaths.
And congenital atelectasis is the cause of 3.4% of newborn deaths.
Atelectasis is also common in young children because their airways are narrower and many structures are still developing.
Classification of the disease
Atelectasis of the lung can be congenital or acquired. Congenital is a painful condition in which a newborn baby’s lungs do not expand during their first breath. If atelectasis is acquired, then the collapse of the lung tissue occurs in an area that was previously involved in the respiratory process. These pathological conditions must be distinguished from intrauterine tissue compression, when the child’s lungs are compressed while in the womb, and physiological atelectasis, which occurs in some people and represents a certain reserve of lung tissue. These conditions cannot be considered true pulmonary atelectasis.
Based on the size of the area that is excluded from breathing, lobular, lobar, segmental, acinar and total atelectasis are distinguished.
Atelectasis can be unilateral or bilateral. The last case is the most dangerous, as it often leads to the death of the patient.
Doctors classify all atelectasis according to etiopathogenetic factors into the following groups:
Obstructive. Obstructive atelectasis is a mechanical disorder of the bronchial tree. With obstructive atelectasis syndrome, complete closure of the bronchial lumen by viscous mucus or a foreign object is possible; this condition is called distelectasis. Compression. Compression atelectasis of the lung is compression of the lung tissue from the outside, accumulated in the pleural part by air, mucopurulent secretion or blood. Contraction. This pathology occurs due to compression of the alveoli by fibrous tissue. Acinar. Such atelectasis occurs in adults and children with respiratory syndrome. This occurs due to surfactant deficiency.
In addition to this classification, all pulmonary atelectasis are divided into reflex and postoperative. This condition can develop acutely or gradually. Atelectasis can be complicated or uncomplicated, as well as transient and persistent.
Atelectasis is characterized by three successive periods of development:
In the first, the bronchioles and alveoli collapse. In the second, there is congestion of the lung and local edema of a certain area. In the third period, normal tissue is replaced by connective tissue and pneumosclerosis is formed. This condition is called pulmonary fibroatelectasis.
All forms of the disease are accompanied by similar symptoms, only depending on the degree of damage to the lungs, the symptoms are strongly or weakly expressed.
Carrying out prevention
It will be possible to prevent the development of atelectasis of any type if you follow the necessary rules:
- Try to adhere only to a healthy lifestyle.
- As part of the recovery period after suffering bronchopulmonary pathologies, it is necessary to follow all the advice and recommendations of the doctor.
- Constantly monitor your body weight.
- Do not take any medications without a doctor's prescription.
- Be regularly examined for preventive purposes.
The success of therapy directly depends on the reasons that caused atelectasis, and in addition, on timely measures taken. The presence of a mild form of the disease is cured fairly quickly.
Also, as part of the prevention of atelectasis, it is very important to prevent aspiration of gastric contents and foreign bodies. In addition, timely elimination of the causes of external compression of the lung tissue is required, along with maintaining the patency of the respiratory canals. In the postoperative period, patients are prescribed adequate pain relief, exercise therapy, and active coughing up of bronchial secretions. If necessary, the tracheobronchial tree is sanitized. Let us also consider the timing of recovery and treatment of pulmonary atelectasis.
Preparing for your appointment
If you don't need urgent care, you'll probably start by seeing your GP or GP. However, in some cases, when you call to make an appointment, you may be able to see a treatment specialist (pulmonologist) immediately.
Here's some information to help you prepare for your meeting.
What can you do
- Write down any symptoms you experience, including any that may seem unrelated to the reason you made the appointment.
- Think back to when your symptoms started and what you were doing at the time. Ask little children in unimaginable ways about the things they put in their mouths.
- Make a list of all the medications, vitamins, or supplements you take. Some medications, such as antihistamines, can make your secretions thicker and harder to cough up.
- Bring a sample of your sputum into a small container.
- Take a family member or friend if possible to help you remember everything that is said.
- Write down questions to ask your doctor.
Questions to ask your doctor
- What could be causing my symptoms or condition?
- What tests do I need?
- What course of action do you recommend?
- What are the alternatives to the approach you propose?
- I have other health conditions. How can I better manage them together?
- Are there any restrictions that I need to adhere to?
- Are there any brochures or other printed materials that I can take home with me? What sites do you recommend?
Feel free to ask other questions during your appointment if you don't understand anything or need more information.
What to expect from your doctor
Your doctor may ask you several questions, including:
- When did you start experiencing symptoms?
- Were your symptoms constant or occasional?
- How severe are your symptoms?
- Did you have a fever?
- What if something seems to improve your symptoms?
- What if something seems to make your symptoms worse?
Share link:
- Click to share on Twitter (Opens in new window)
- Click here to share content on Facebook. (Opens in a new window)
- Click to share on Telegram (Opens in new window)
Liked this:
Like
Similar
Forecast and timing
The success of lung expansion primarily depends, as noted earlier, on the causes of atelectasis, and in addition, on the timing of the start of treatment. If the cause is completely eliminated in the first three days, the prognosis regarding the complete morphological restoration of the lung area is favorable. In the case of later periods of expansion, the development of a secondary change in the collapsed area cannot be completely excluded. Massive and at the same time rapidly developing atelectasis can lead patients to death.
Complications and consequences of pathology
Against the background of this lung disease (atelectasis), the following complications and consequences are likely:
- The development of acute respiratory failure, in which the breathing process is disrupted with a sharp lack of oxygen in the body.
- The appearance of infection with the occurrence of pneumonia or lung abscess. With an abscess, a cavity is formed at the site of inflammation, filled with purulent masses.
- In the presence of large atelectasis, compression of the entire lung occurs. In addition, against the background of the progressive development of the pathology, death is likely.
Symptoms of the disease
The severity of symptoms directly depends on the area of the lungs where the pathological process has spread. In the case of damage to one segment, as a rule, pulmonary pathology is almost asymptomatic. Only an x-ray will help detect it at this stage. The most noticeable manifestation of this disease is with the development of atelectasis of the upper lobe of the lung on the right. If the middle lobe is affected, doctors will detect elevation of the diaphragm during examination. The main symptoms of the disease are the following:
- The appearance of shortness of breath, which is observed during physical activity, and also at rest.
- The presence of painful sensations on the side where the pathological process occurs.
- The occurrence of increased heart rate.
- Decreased blood tone.
- The appearance of a dry cough.
- The appearance of cyanosis.
It should be noted that the listed symptoms are the same for all patients, regardless of age.
What is the diagnosis of pulmonary atelectasis? Let's look at this next.
Symptoms and diagnosis
The severity of the symptoms depends on the time during which the disease developed and the area of the collapsed area, as well as on the cause of the pathology. Common features are:
Increasing shortness of breath.
Impaired breathing. Difficulty in inhaling or exhaling. Dry or unproductive painful cough. Pain in the area of the affected lobe of the right or left lung. Blue skin tone. Tachycardia – decreased blood pressure, increased heart rate.
If a person has chronic atelectasis syndrome, cor pulmonale is formed, chest pain is possible due to the discrepancy between the required energy and the actual reserves of nutrients and oxygen. Swelling of the lower extremities appears, as blood stagnates in the circulation.
Hypoxia is formed, to which nervous tissue is most sensitive. The patient complains of constant headaches, malaise, chronic fatigue, weakness, and nausea. In newborn children, there is a violation of the shape of the chest, further lag in mental and physical development due to disturbances in metabolic processes.
When diagnosing, the doctor takes into account the symptoms and medical history of the patient; examining the patient, he notes a decrease in the size or deformation of the chest, a decrease in the intercostal spaces. When palpating the chest above the area of atelectasis, vocal tremors decrease.
On percussion, the lower edge of the lung moves upward, a clear pulmonary sound is replaced by a pronounced dullness. During auscultation, breathing is weakened and cannot be heard at all over the affected area. Sometimes moist rales are heard.
An objective research method is a plain chest x-ray. The X-ray shows:
- darkening of areas of the lungs; displacement of mediastinal organs; the presence of a foreign object or tumor; scoliosis; changes in the diaphragm dome; level of damage, that is, atelectasis of the upper, middle or lower lobe.
For better image quality and layer-by-layer study, magnetic resonance and computed tomography are used. Most patients undergo bronchoscopy – endoscopy of the bronchial wall. Additionally, tissue biopsy and mucus collection for microscopy are performed.
Spirography is necessary to clarify volumes and capacities, assess ventilation and respiratory failure. In case of cardiac dysfunction, ultrasound examination and electrocardiography are prescribed.
How does pathology develop?
Atelectasis occurs:
- primary (congenital);
- secondary (acquired).
Congenital atelectasis is observed in newborns, when the first breath does not fully expand and fill the lungs with air. The causes of such atelectasis:
- intrauterine malformations;
- lack of surfactant;
- ingestion of amniotic fluid or meconium (an analogue of feces excreted by the fetus during intrauterine development) into the respiratory tract.
Acquired atelectasis occurs at different ages due to the reasons described above. According to the development mechanism, it is:
- obstructive (due to bronchial blockage);
- compression (due to external pressure on the airways)
- functional (in the case when the “ventilation” of the lungs decreases, but pathology as such is not observed);
- mixed.
The degree of atelectasis due to blockage depends on whether the bronchial lumen is partially or completely blocked. If blockage occurs, bronchial patency must be restored immediately. The point is not only in the sudden oxygen starvation of the body due to a decrease in oxygen supply: the longer air does not enter through the bronchus into the collapsed fragment of the lung, the greater the likelihood that this area will stick together and not straighten out. If the lumen of the bronchus is completely blocked for more than 3 days, ventilation in the corresponding part of the lung will not be restored.
Atelectasis due to pressure on the lung tissue has a more favorable outcome than due to blockage. Even after a long period of compression of the lung, there is a chance of complete restoration of lung ventilation.
Functional atelectasis develops in the lower parts of the lungs. It occurs in the following cases:
in bedridden patients - most often during a long postoperative period, after strokes, spinal injuries, in patients in a coma, and so on;
- if there has been an overdose of sedatives (calming) drugs or barbiturates (used to suppress the nervous system);
- when breathing is limited to reduce pain (chest injuries, inflammation of the pleura, acute surgical diseases of the abdominal organs);
- due to increased intra-abdominal pressure, which is facilitated by constipation, ascites (free fluid in the abdominal cavity), bloating;
- with paralysis of the diaphragm;
- due to certain diseases of the spinal cord.
Mixed atelectasis occurs due to the summation of various reasons described above.
The severity of atelectasis depends on the level of blockage of the bronchus and the area of collapse of the lung - its degree varies from lobular atelectasis, when the terminal bronchioles (the smallest bronchi) are affected, to collapse of the entire lung, when the main bronchus is involved in the pathological process.
Diagnosis of central malignancy
Now let's look at what lung cancer looks like on an X-ray, if we are talking about its central location. The tumor will appear as follows:
The appearance of a dark area (infiltration). Poor ventilation. Adjacent sections are characterized by compensatory airiness. It occurs because when a section of the lung is severely damaged, the organ requires compensation to normalize the process of supplying oxygen to the surrounding tissue.
If a patient has central cancer of the main bronchus, then the tumor has typical symptoms, and therefore an experienced radiologist can easily recognize the onset of the development of pathology. The central cancer on an x-ray image appears as a shadow having an inhomogeneous structure with a tuberous outline. On one side, such a shadow is often covered with ulcers.
If the tumor compresses other organs, fluid may appear in the pleural cavity.
If the neoplasm has developed in the upper part of the lung, it is often mistaken for a tuberculous infiltrate. However, if we are really talking about cancer, then foci of destruction are clearly visible on the x-ray. The darkening created by the tumor is characterized by an uneven scalloped contour.
A tumor is benign if it has the following features:
A circle of regular shape. Clear contours.
How does central lung cancer appear on x-ray?
Such a lung tumor in the first stages manifests itself in the form of the following changes:
A blackout appears. With atelectasis, there is no differentiation of the boundaries between the heart and the diaphragm.
In addition, their position may change somewhat in relation to each other. But the main sign of the disease is the presence of darkening, which can have different shapes and sizes. The spot can also be oval in shape if it is located on the periphery.
We can talk about a malignant formation if the following signs are present on the x-ray:
The vessels deviate, causing their distal approach. The intensity of the darkening is reduced due to the fact that the blocked bronchus suffers from a lack of ventilation. Atelectasis of the lung area (collapse process) is observed.
Cancer of the exobronchial type appears on x-rays with the following distinctive features:
Presence of hypoventilation; there is a bumpy formation in the root zone; the spot has radiant contours; there is a narrowing of the bronchial lumen; enlargement of root lymph nodes.
The presence of at least one of the above characteristics indicates that the patient should undergo a CT or MRI to confirm the diagnosis. The procedures should be carried out as quickly as possible, since the tumor can quickly grow and, after a short period of time, metastasize to nearby organs. Even within a month, significant tumor progression is possible.
How does peribronchial formation appear on x-ray?
With a peribronchial tumor, the following symptoms are noticeable on x-rays of lung cancer:
The bronchi have thickened walls; there is no hypoventilation; the presence of rough strands running from the edge to the root; the tumor grows along the wall of the bronchial tree.
In cases where lung cancer on X-ray does not have the above-described signs, it is necessary to conduct some additional studies. An MRI or CT scan is prescribed if the radiologist cannot make an accurate diagnosis. A diagnostic thoracotomy may also be prescribed. It is carried out as a result of a meeting of oncologists and radiologists.
Cancer in the upper part of the lung can occur due to a Pancoast tumor. This formation is round in shape and is located in the clavicular region, affecting the ribs and upper vertebrae. Such a lesion in lung cancer can be diagnosed only after bronchoscopy has been performed, the results of which can show the patency of the upper lobe bronchus.
If the malignant formation is characterized by a mixed form, then an x-ray of the lungs can reveal a number of pathogenic signs, among which the following stand out:
- infiltrative node; bronchial stump; presence of effusion in the pleural cavity; large size of lymph nodes located in the sternum area; bronchial patency is impaired; development of perifocal pneumonia.
If there is a suspicion that a patient has a mixed form of cancer, then in most cases a CT scan is prescribed.
Only tomography allows us to fully study how widespread the process has reached and assess the condition of the tissues surrounding the tumor.
Causes of the disease
A lung can collapse for various reasons; they can be identified in the following list:
- Bronchial obstruction. In this case, a complete blockage of the bronchus occurs, and the air begins to dissolve slightly lower than the blocked area. The appearance of a large pleural effusion, which puts pressure on the lung tissue from the outside. A blood clot in the lung that formed as a result of pulmonary hemorrhage. Stagnation of thick secretion in the bronchi, which is formed due to acute and chronic diseases of the respiratory tract - bronchitis or pneumonia. Strong pressing of lung tissue by a tumor, inflamed lymph node or foreign inclusion. Impaired ventilation of the lungs and abundant accumulation of viscous mucus in the bronchi, due to general anesthesia or surgery.
Pulmonary atelectasis can also occur with prolonged bed rest if the body position does not change for a long time. This pathology is typical for bedridden patients.
Sometimes atelectasis begins as a result of bronchospasm and bronchial edema in pathologies of an allergic nature.
Features of the disease
This type of atelectasis appears first in the pleural membrane of the lung, and then spreads directly to the lungs. Some pathological volume begins to grow in the pleura; it can be pus, blood, fluid or air.
Pulmonary atelectasis
Most often, pus can accumulate in the pleural membrane as a residue from the inflammatory process. This fluid begins to put pressure on the lung, after which air comes out of it, and the alveoli, the walls of which have a layer of surfactant on the inside, stick together. Factors that can compress the lungs during compression atelectasis include:
- A large amount of any inflammatory fluid. This fluid contains many leukocytes, which constantly increase the volume of fluid. Fluid in the pleural membrane can accumulate due to diseases such as pneumonia, tuberculosis or systemic diseases that affect the entire body or are caused by immunodeficiency. These diseases include chronic bronchitis and rheumatism.
Hydrothorax. Hydrothorax is caused by poor heart function. This symptom occurs when the heart does not pump blood well, and congestion occurs in the veins of the lungs. After some time, blood accumulates around the lungs, which gradually compresses the lungs.
- Pneumothorax. When atmospheric pressure comes into contact with the internal pressure of the lung, the second begins to compress the respiratory organ, pneumothorax occurs. If the necessary manipulations are not carried out in time, a person may suffocate from simply not being able to breathe.
- Hemothorax. Accumulation of blood in the pleural lining of the lungs due to excessive bleeding.
- Compression of the lungs from the inside by a significant tumor located on the lungs or bronchi. The most common malignant tumor, which can affect both the lungs and the bronchial tree, is lung cancer.
Lung cancer can occur against the background of any inflammatory processes that occur in the lungs. Pneumonia, tuberculosis, chronic bronchitis - all this can lead to the development of pathological lung cells. In the early stages of diagnosing the disease, surgical intervention can be used. At later stages, only palliative care can help.
Symptoms of compression atelectasis
It is worth noting that the symptoms of different types of atelectasis vary. Some types can be practically asymptomatic, and a person will not even suspect the mortal danger.
As a rule, already on the 3rd day, atelectasis turns first into an inflammatory process, and only then into pneumonia, which proceeds much faster than a normal disease, and already on the 4-5th day a person can die for no apparent reason. That is why timely diagnosis of any type of atelectasis can save tens, or even hundreds of lives.
The main symptoms of compression atelectasis are:
shortness of breath (occurs gradually, against the background of any disease);
- difficulty breathing;
- cough;
- pain and heaviness in the affected lobe of the lungs;
- cyanosis of lips, skin and limbs;
- in the part of the chest where collapse occurs, swelling forms, including intercostal tissue;
- when performing a respiratory act, one side of the chest noticeably lags behind.
Thus, some symptoms of compression atelectasis can be seen with the naked eye.
It is worth noting that during the course of this syndrome, collapse can occur - a sharp drop in blood pressure, which can lead to loss of consciousness, coma and even death.