Intestinal obstruction is a syndrome that occurs against the background of complete/partial disturbances in the motor activity of an organ or mechanical blockage (obstruction) in one of its sections, creating difficulty for the further movement of food. Many diseases lead to this complication. Intestinal obstruction is a serious problem that leads to changes in metabolic processes and poisoning of the body. Treatment is carried out under the supervision of a doctor in a hospital.
Types of intestinal obstruction
Before moving on to the symptoms of intestinal obstruction, let's first look at its types. Types of acute intestinal obstruction can be divided into two large groups:
- dynamic (spastic and paralytic);
- mechanical (mixed, obstructive and strangulation).
- Dynamic obstruction is a violation of the motor function of the intestinal wall without a mechanical obstruction in the intestine.
Spastic obstruction is a violation of passage through the intestines due to persistent spasm of the muscular layer of the intestinal wall.
Paralytic obstruction is a consequence of decreased tone and loss of the ability of the muscle cells of the intestinal wall to contract.
- Mechanical obstruction occurs when there is a mechanical obstruction at the level of the large or small intestine. It can be caused by intestinal volvulus, tumors, external compression of the intestines and other reasons.
Mixed (intussusception) is when one intestine is inserted into another. It is possible to introduce one loop of intestine into the lumen of another over a considerable distance (from 20 cm to 1 m and even more). In this case, due to the intestine, obstruction of the lumen of the other intestine begins (obstructive obstruction). There is strong compression of the intestine itself and its mesentery, it is poorly supplied with blood (stangulating obstruction).
Obstructive occurs when there is a mechanical obstacle that interferes with the movement of the intestinal contents that are in its lumen. In 96% of cases, obstructive obstruction is caused by intestinal tumors (colon cancer). Sometimes there are gallstones, cicatricial strictures of the intestines, and foreign bodies.
Strangulation obstruction appears from squeezing and twisting of the intestine with the mesentery, which causes not only compression of the intestinal lumen itself, but also a disruption of its blood supply due to compression of the mesenteric vessels.
A classic example of strangulation intestinal obstruction is intestinal volvulus, strangulation in the hernial orifice, and nodulation.
The peculiarity of such obstruction is the rapid necrosis of the intestines, the presence of painful shock and a generally severe course.
Consequences of intestinal obstruction
The development of obstruction triggers a cascade of pathological processes that affect the body systemically. With tumor obturation, the onset, as a rule, is blurred due to incomplete occlusion of the intestinal lumen, but as the tumor grows, the situation worsens. Acute obstruction, as a rule, develops due to complete obstruction of dense feces in the area of the intestine narrowed by the tumor.
In the first time after the development of obstruction, there is an increase in intestinal peristalsis. It's as if he wants to overcome an obstacle. As intestinal contents accumulate, the intestinal wall becomes overstretched, water-electrolyte and metabolic disturbances occur, motor function sharply weakens, and then intestinal paralysis occurs.
At the second stage, disturbances in the secretory-resorptive activity of the intestine and disturbances in parietal digestion develop, the enzymatic activity of enterocytes is blocked, as they are rejected, and the regenerative activity of the crypts is first inhibited and then completely stopped.
Under such conditions, the activity of intestinal bacteria and the so-called symbiont digestion is activated. It is not physiological and is inferior in efficiency to normal, parietal digestion. As a result, rotting and fermentation occurs, as well as the accumulation of a large number of products of incomplete breakdown of proteins, some of which have a toxic effect.
As the process progresses, the immune defense mechanisms are disrupted, which leads to the active proliferation of anaerobic bacteria that secrete exo- and endotoxins. They act systemically on the body - they disrupt tissue microcirculation, lead to central nervous system disorder, and disrupt cellular metabolism. Due to these effects, the permeability of the intestinal wall to bacteria increases, and they can spread into the abdominal cavity, blood and lymph flow, causing peritonitis and even sepsis.
Water and electrolyte disturbances also progress. Due to disruption of the intestine, increased filtration of fluid occurs; it is not absorbed back and accumulates in the afferent loop of the intestine. Under normal conditions, about 10 liters of liquid enter the gastrointestinal tract per day (including food, drink, saliva and secretions of the digestive glands). About 8-9 liters should be absorbed back, but this does not happen due to impaired reabsorption. Fluid accumulates in the adductor section of the intestine, causing it to expand. This, in turn, leads to reflex vomiting, which further worsens dehydration. Against this background, electrolyte disturbances quickly develop, which ultimately lead to renal and heart failure.
Book a consultation 24 hours a day
+7 (495) 151-14-53
What causes intestinal obstruction?
What is this pathological condition? This is the presence of obstacles to the passage of the food bolus through the intestines. The reasons are as follows:
- the intestinal lumen can be compressed by tumors (malignant or benign), which are localized internally or externally;
- Foreign elements may enter, hematomas may appear, and worms may accumulate;
- it happens that the intestinal muscles are paralyzed;
- overgrown scars or adhesive disease may be present;
- there is a volvulus;
- Gallstones may accumulate in the intestinal lumen.
The causes of intestinal obstruction in children are the same, but often the underlying cause lies in the accumulation of feces or the presence of a foreign object.
Doctors recommend!
Monastic stomach tea - for gastritis, ulcers, heartburn and for general health promotion!
Find out more>>>
Diagnostics
The initial task of the surgeon is to distinguish intestinal obstruction from diseases with similar symptoms. To do this, differential diagnosis is carried out with appendicitis, organ perforation, peritonitis, afferent loop syndrome, pleurisy, renal colic, heart disease, pancreatitis, cholecystitis.
To recognize intestinal obstruction, the doctor analyzes the patient’s complaints and conducts an external examination of the abdomen. By palpation and tapping, the most painful areas and the presence of volumetric compactions are identified. To analyze noises inside the abdomen, specialists use a phonendoscope, a special device that helps evaluate peristaltic sounds.
Instrumental examination of the abdominal cavity includes:
- X-ray. Using this method, you can see the accumulation of gases and transverse levels of liquid in the loops of the organ. This information is recorded on the x-ray. To detect a blockage and determine its location, a person is given a contrast agent to drink. This method is called the “half-glass Schwartz test.”
- Tube enterography. The survey is carried out to document the area where there is an obstacle.
- Colonoscopy. The method allows you to assess the condition of the colon. Sometimes a colonoscopy can clear the blockage.
- Ultrasound diagnostics. The study helps to distinguish intestinal obstruction from other pathologies, detect tumors, and inflammatory formations.
To make a diagnosis, women may need a gynecological examination and pelvic ultrasound. Such measures are necessary to exclude ectopic pregnancy and diseases of the genital organs.
How does this pathology manifest itself?
To avoid serious consequences from the condition described above, it is necessary to know the symptoms of intestinal obstruction in both adults and children. Understanding this issue is very important.
It must be said that in medicine the clinical picture of the disease consists of three stages. Each of them has specific characteristics.
At the first stage
It lasts twelve hours and is characterized by the presence of pain. If intestinal obstruction occurs due to mechanical blockage, then the pain will be paroxysmal. She disappears from time to time.
Often, if you consult a doctor at this stage, he will diagnose an incomplete blockage. In this case, the patient will be prescribed a diet for partial intestinal obstruction.
If a torsion, loops or other changes have already formed, the pain can be very severe. It rarely passes, and in certain situations its intensity provokes painful shock and loss of consciousness.
At the first stage of the disease, nausea and vomiting occur infrequently, only in a situation where the small intestine is blocked by some object.
Many patients at the first stage of pathology progression take painkillers, antispasmodics, and try to improve their well-being with their help.
Unfortunately, this does not help, and the signs of adhesive intestinal obstruction, on the contrary, become even more intense.
At the second stage
It lasts from twelve to twenty-four hours from the onset of intestinal obstruction. At this time, a person has severe pain attacks, and the intestines cease to cope with their functions. Abdominal bloating begins, constant vomiting begins, and dehydration of the body also rapidly increases.
It is too late to seek medical help at this stage, because complications still cannot be prevented. And yet the chances of recovery and restoration of functionality are quite good.
At the third stage
At this phase everything is very difficult. In the patient:
- there is no urine at all;
- tachycardia and rapid breathing are observed;
- there is hyperthermia (increased body temperature).
Doctors, examining such a patient, may note symptoms of sepsis and peritonitis. Feces and gases do not pass.
The third stage is very difficult and fast. Often the patient quickly develops toxin poisoning, sepsis progresses, which disrupts the functioning of all organs and systems of the body. In almost every case, the person dies at this stage.
So, you already know what intestinal obstruction is and symptoms in adults. Now let's move on to diagnostics.
Symptoms of the disease
- Stomach ache. Initially, the unpleasant sensations are cramping in nature, attacks of pain occur along with the activation of intestinal motility. When pain occurs, the patient may scream, thrash, squat, kneel, or press his legs to his stomach. In these positions, sensations become less pronounced, but the overall intensity of pain changes little.
- Vomit. Intestinal obstruction is characterized by repeated vomiting, which is not accompanied by a feeling of relief. Pathological masses are released abundantly. Their character may change over time. Initially, the remains of undigested food come out, then the patient vomits bile. Later, the discharged masses may acquire a fecal character.
- Retention of stool and gases. In case of intestinal obstruction, defecation is completely absent until therapeutic measures are carried out. As a result, food masses accumulate in the gastrointestinal tract, which leads to severe bloating and asymmetry of the abdomen. Unlike other pathologies, there is no flatulence or intense release of gases in this condition.
- Intoxication syndrome. With prolonged presence of obstruction, severe intoxication of the body develops, which can be manifested by increased temperature, pallor, and sweating. If the patient's condition is serious, signs of damage to the shock state appear - lack of urine output, metabolic disorders, increased respiratory rate. Most often, such symptoms occur in the later stages, when intestinal obstruction is complicated by peritonitis and sepsis.
Table 1. Characteristic differences between constipation and intestinal obstruction.
| Intestinal obstruction | Constipation |
| There is no stool discharge at all | Defecation is possible, but bowel movements may not be complete |
| Severe abdominal pain | Pain syndrome is not typical |
| No flatulence | Often accompanied by flatulence |
| There is pronounced asymmetry of the abdomen | Abdominal asymmetry is not typical |
| Nausea and repeated vomiting are always present | Nausea and vomiting are practically not typical, in rare cases - single vomiting |
| Symptoms of intoxication are expressed | General symptoms are not typical |
How is diagnosis carried out?
Obstruction in the intestine is diagnosed in the surgical department. The gold standard for diagnosis is a survey radiography of the abdominal cavity, which determines the pattern (Kloiber's cups).
Additional research tools:
- colonoscopy;
- barium passage (x-ray contrast study);
- CT scan of the abdominal cavity;
- Ultrasound of the abdominal organs, pelvic organs and urinary system;
- fibrogastroduodenoscopy.
How should common intestinal obstruction be treated?
Rarely do doctors provide therapeutic interventions. This decision is made only at an early stage of pathology development and with timely diagnosis.
The conservative method is used to cure intestinal obstruction in elderly people who are prohibited from surgery, but only at the initial stage of the disease.
Therapeutic treatment consists of:
- pumping out the contents of the stomach and intestines through a special probe;
- performing siphon-type enema;
- use of antispasmodics.
Also, conservative treatment in this case is a colonoscopy, in which doctors eliminate the cause of the development of the acute condition. For example, a gallstone is removed or a loop of intestine is straightened.
How is acute intestinal obstruction treated? As mentioned above, there is only one solution: an operation is performed immediately and the root causes of the pathology are eliminated.
Forecasts depend on the speed and correctness of the operation. After surgery, the obstruction no longer bothers the patient, but he needs a long rehabilitation. During this period, the patient is recommended:
- be periodically examined by a doctor (to avoid relapses);
- take a course of antibiotics;
- strictly limit your diet.
The result of obstruction of the small intestine, like the large intestine, can be quite serious. If it is too late to seek medical help, surgeons remove part of the intestine, which cannot but affect the patient’s future life.
Classification
Since a set of symptoms associated with impaired peristalsis can be a consequence of a whole list of diseases, there are many types, forms, and types of this syndrome.
Depending on the genetic causes, congenital and acquired intestinal obstruction are distinguished. The pathological process occurs in acute or chronic form. The disorder extends completely to the entire organ or a separate part of it.
The cause-and-effect relationship, as well as the features of the course, are the basis of the classification. Based on these characteristics, mechanical, vascular, and dynamic forms are distinguished. Each of them has its own subspecies.
Mechanical
This form is associated with the appearance of some obstacle. The closure of the area occurs gradually or suddenly. Mechanical intestinal obstruction can occur due to:
- Obturation – blockage of one of the areas. The lumen of the organ is pinched due to inflammatory processes, tumor growth, enlarged spleen, foreign bodies (fecal solids, a lump of parasites, bile coprolites).
- Intestinal strangulation (strangulation). Mechanical intestinal obstruction of this type occurs with hernias, adhesions, torsions, and nodular formations. In such cases, the local blood supply is disrupted. Ischemia of the intestinal muscles provokes necrosis.
- Mechanical blockage in combination with compression of mesenteric vessels. This combination is referred to as mixed intestinal obstruction. Most often, this type occurs with invagination of loops (when one part of the organ is wedged into another), internal and external hernias, and adhesions.
Dynamic
Food moves through the gastrointestinal tract using contractile movements of a certain strength and frequency. This mechanism is disrupted when the muscle layer of the organ for some reason fails to cope with its functions.
Peristalsis slows down greatly or stops completely. In the dynamic form of the pathology, obstruction and strangulation of the intestinal mesentery are not detected.
Based on the cause that caused the condition, there are 2 types of syndrome:
- Paralytic obstruction of organ loops. The complication is associated with a decrease in the tone of myocytes - the main cells that form the intestinal muscles. These changes are caused by metabolic failures, disorders of the nervous system, surgical diseases of the tissues of the chest and abdominal cavity, leading to peritonitis. Smooth muscles lose motor function. Complete paralysis of the intestinal tract occurs. The loops with this type of pathology are equally tense and swollen.
- Spasmodic obstruction. The muscle tissue of the intestines contracts. This process is caused by an increase in the tone of the cells lining the walls of the organ. The spasm occurs due to a lack of calcium, parasites, hysteria, and heavy metal poisoning. Over time, the spastic form is replaced by total paralysis of the organ.
Vascular
Intestinal obstruction in this case is caused by cessation of blood flow in the mesenteric arteries. This condition is associated with the formation of blood clots, embs (clogging particles). After 2-3 hours, intestinal motor function fades away and gangrene begins. Tissue death due to vascular obstruction is a complication of diseases of the circulatory system and heart.
According to the level of the pathological process, high and low obstruction are distinguished.
This classification assumes the anatomical location of the obstacle to the movement of food. Small intestinal obstruction corresponds to a high level. The obstacle in this type of pathology is located away from the muscle connecting the duodenum to the diaphragm. The anatomical border that conventionally separates the upper and lower obstruction is the Bauhinian valve. It connects the small and large intestines. High obstruction occurs in most cases.
The length of the small intestine is about 5 meters. The loops of the organ are fixed on the abdominal wall by two-leaf ligaments - the mesentery.
Obstructions located below the connecting valve are referred to as colonic obstruction. It is diagnosed in 20-30% of cases.
Other important nuances
When the intestines have already been washed, antispasmodics and drugs that enhance peristalsis are used.
In case of intestinal obstruction for mechanical reasons, an operation is performed to remove the obstruction (the foreign body is removed, adhesions are removed, deintussusception is performed, the loops are untwisted, etc.). The necrotic section of the intestine is removed. An intestinal anastomosis is created between viable parts of the intestine.
If the contents of the intestine have ruptured into the abdominal cavity and peritonitis develops, then drainage must be installed during surgery.
Possible complications and prognosis
Complications of intestinal obstruction include:
- peritonitis - inflammation of the peritoneum;
- ischemia and necrosis of the intestinal area;
- state of shock;
- sepsis.
If the patient consults a doctor in a timely manner, the prognosis is favorable. In most cases, the patient makes a full recovery. With late hospitalization, the likelihood of an unfavorable outcome increases. The risk of complications is higher; in 25% of cases, severe obstruction ends in death. Therefore, timely hospitalization of the patient is so important.
Prevention
To prevent such a serious health problem, you need to:
- get rid of helminthic infestations in a timely manner;
- lead an active lifestyle, if possible walk at least three kilometers a day;
- drink at least two liters of water daily (juice or tea does not count);
- switch to fractional meals;
- give preference to healthy food: the diet must consist of various spices and vegetables;
- if surgery is needed, it is better to choose laparoscopy;
- closely monitor the condition of the intestines and promptly treat all identified diseases: adhesions, tumors, inguinal hernias, etc.
Doctors recommend!
Monastic stomach tea - for gastritis, ulcers, heartburn and for general health promotion!
Find out more>>>
Clinical picture
Mechanism of formation of acute intestinal obstruction
The clinical picture of the acute form of obstruction manifests itself very clearly - a gradual increase in the intensity of symptoms is not typical for the disease. The disease is expressed by symptoms of intestinal dysfunction:
- nausea and vomiting;
- intense pain syndrome;
- flatulence and increased peristalsis (the intestine itself tries to push through the barrier that blocks its lumen);
- impaired excretion of feces and gases. A person usually experiences constipation.
The pain syndrome in acute intestinal obstruction is very intense. The pain is localized in the navel area, but does not radiate. Has a cramping character. At the time of an attack, a person takes a forced position, which allows him to slightly reduce the manifestation of pain. During this period, the patient may show signs of shock - increased heart rate, pale skin, cold and sticky sweat, etc. Already when this symptom is expressed, it is necessary to take the patient to a doctor and carry out a diagnosis that will make it possible to determine the true cause of the condition.
The second symptom is vomiting. Based on its character, the doctor can even tell at what level the intestinal lumen was blocked. For example, if the vomiting is profuse and particles of food that a person consumed the day before are visible in it, then in this case the small intestine is affected. But it also happens that first vomit with food particles is released, then it turns yellow due to the admixture of bile, and then dark green - fecal vomit. This indicates damage to the large intestine.
Impaired excretion of feces and gases. At first, this process may not be disrupted, since the lower parts of the intestine are reflexively emptied. But after this, persistent constipation and bloating develop. A visual examination can reveal that the patient’s abdomen is enlarged, but asymmetrically. In addition, enhanced peristalsis can be noted on it.
If such signs are expressed, you cannot hesitate - you need to take the patient to a medical facility to a surgeon who can carry out a full diagnosis and treatment of acute intestinal obstruction.
It is important to follow the following diet
How to cleanse the intestines of toxins? Colon cleansing at home. These are very popular queries on the Internet, so let's deal with them.
To restore normal functioning of the gastrointestinal tract, you cannot do without a therapeutic diet. After surgery, you should not eat at all for twelve hours, because you need to allow the intestinal walls to heal.
Then (depending on the severity of the disease and the patient’s condition) the nutrient solution can be administered intravenously.
After a successful operation, the following diet is prescribed:
- mucous decoctions of flax, oats, starch;
- vegetable decoctions and low-fat broths.
After a person has suffered from intestinal obstruction, he should not eat foods that cause constipation and cause flatulence. Let's also find out how to cleanse the intestines.
To begin with, you should give up:
- apples;
- fresh bread, pastries;
- fermented milk and dairy products;
- chocolate, alcoholic drinks, coffee;
- baked, marinades, salted, spicy, smoked;
- legumes;
- poorly digestible cereals;
- fatty fish and meat.
The diet should include bran and rye bread. Every day you need to consume at least one tablespoon of vegetable oil. Products such as oatmeal, beets, and prunes are especially beneficial for the body.
Symptoms
The first signs of the disorder in adults are cramping pain in the pit of the stomach, near the navel. The attack begins suddenly. The pain may subside temporarily or be permanent, depending on the cause. Usually attacks are repeated at intervals of 10-15 minutes. The pain intensifies during the peristaltic wave. Without treatment, they go away within 2-3 days from the first episode. This is an alarming sign indicating a complete cessation of motor function.
Obstruction associated with intestinal paralysis is characterized by dull arching pain. A person does not feel any overflows or noises in the abdominal cavity that indicate the digestive process.
Characteristic symptoms by which intestinal obstruction is recognized:
- external asymmetry;
- swollen abdomen with visible peristalsis;
- vomiting is combined with stool retention.
The patient has visible bulges on the sides or anterior wall of the peritoneum. This sign is used to determine acute intestinal blockage. Severe bloating is associated with expansion of intestinal loops. The increase occurs due to stool retention, gases, and fluid accumulation. With intestinal obstruction, pain occurs as a result of damage to nerve endings. Against the background of obstruction and extinction of peristalsis, the receptors are pinched and their integrity is disrupted.
Small intestinal obstruction at an early stage does not manifest itself as stool retention. The contents of the lower sections are promoted. There may even be multiple stools during therapeutic procedures. Defecation is not difficult.
Stool retention is a characteristic manifestation of an obstruction in the large intestine. The mechanism of development of this symptom depends on the cause of the disorder. The obstacle is a foreign body, decreased motor activity, and lack of blood supply.
Symptoms of intestinal obstruction associated with intoxication of the body:
- nausea;
- weakness;
- headache;
- cardiopalmus;
- low pressure;
- dyspnea;
- dry mouth.
Such signs appear as a result of gradual poisoning of the body.
When the obstacle is located high, vomiting is repeated. It does not alleviate the patient's condition. Vomit contains food debris, then bile. After some time, the discharged masses acquire a brown color and a putrid odor.
Colon obstruction is characterized by vomiting 1-2 times.
If the patient is not provided with medical assistance in a timely manner, peritonitis develops - inflammation of the peritoneum.
The chronic form of intestinal obstruction appears due to adhesions and tumor growth. Most often, a sluggish process is observed after surgery on the gastrointestinal tract. The chronic form is manifested by stool disturbances (diarrhea alternating with constipation), increased gas formation. When the tumor grows to a certain size or the adhesions completely block the intestinal loop, the process becomes an acute form of obstruction. In this case, the pathology develops rapidly and requires emergency care.
Symptoms of spastic obstruction
With this type of dynamic intestinal obstruction, the main manifestation of the pathology is cramping intense pain in the abdomen without a specific localization. During spasms, the patient screams, cannot remain still and rushes about in bed. Painful attacks do not last long. Some patients may experience a slight increase in temperature.
Digestive disorders with spastic intestinal obstruction are not typical. Lack of stool is not detected in all patients, and it is rarely persistent. The general condition of the patient suffers slightly. When examining the abdomen, it has a normal appearance or the abdominal wall is slightly retracted and has a scaphoid shape.
A plain X-ray image reveals a spastic atonic state of the intestine. In some patients, along the course of the small intestine, small Kloiber cups are identified, lined up in a chain along the mesentery. Images with a barium suspension show clear areas of swelling and slow passage of the contrast agent.
Obstruction in a child
Obstruction in children is of the paralytic type. The reason may be:
- surgical interventions;
- pneumonia;
- intestinal disorder;
- infectious diseases.
The onset of the disease is expressed by intense pain and vomiting. The contents of the intestines return back to the stomach, causing sharp pain, and a foul odor is noted in the mouth. The abdomen swells and becomes inelastic. Upon subsequent examination in the hospital, tachycardia is detected, body temperature increases, and intestinal loops dilate.
Infants may develop intussusception, a type of obstruction. In this case, one part of the intestine enters the space of another.
Postoperative period
Surgeries for intestinal obstruction are volumetric interventions with a long postoperative period. It is determined by the time of complete healing of the wound and the maximum possible restoration of the body. The main treatment tactics during this period:
- control and restoration of the normal functioning of internal organs (respiratory and cardiovascular systems);
- adequate pain relief;
- gastric and intestinal lavage;
- restoration of normal peristalsis;
- surface treatment of the surgical wound;
- in the case of a colostomy, teaching the patient how to care for it.
Gastric lavage is performed daily using a tube. Continuous suction of intestinal contents is possible. The greatest effect is observed from the use of a probe inserted during surgery through the nose into the intestines. It allows you to remove liquid contents of the intestine and gases during this period, which reduces the effects of intoxication and helps restore peristalsis. As a rule, in the middle of the postoperative period the probe is removed (day 5).
Peristalsis is activated by the introduction of small quantities (up to 40 ml) of hypertonic solutions of 10% sodium chloride, and the introduction of cholinesterase inhibitors (Proserin).
Gradually, as intestinal motor function is restored, the patient is allowed to eat. During this period, food should be as gentle as possible mechanically and thermally. Food must be pureed or chopped using a blender. The temperature should correspond to the human body temperature.
Dishes should not contain salt, substances that affect peristalsis, herbs and spices should be excluded. Meals up to 8 times a day, in small portions. Vegetable decoctions, pureed porridge, boiled and chopped fruits (apples, pears), lean veal, and chicken are acceptable. It is recommended to drink up to one and a half liters of fluid per day.
Diagnosis of pathology
In case of dynamic obstruction, the doctor conducts an oral interview, finds out the symptoms, and collects anamnesis. A visual examination necessarily includes palpation, which allows you to determine the intensity of pain and the cause of its occurrence. Laboratory tests may then be prescribed. First of all, this is a general and biochemical blood test - to assess changes in the composition and to determine the general health of the human body.
Rectal examination is also mandatory when diagnosing this disease. Using this technique, you can detect the presence (absence) of blood or mucus in the stool.
Still, the main diagnostic methods are instrumental. Here are the main ones:
- Ultrasound;
- irrogography;
- radiography;
- colonoscopy.
When diagnosing a child, consultation with a pediatric surgeon is required. It is he who will determine the techniques that will need to be used to make the correct diagnosis.
The main goal of rapid diagnosis is to determine the type of intestinal obstruction. If mechanical rather than dynamic obstruction is diagnosed, then immediate surgical intervention is required.
Any delay in this case can lead to serious complications and even death. Diagnostics also makes it possible to differentiate this disease from others, for example, pancreatitis, perforated ulcers, acute appendicitis. All pathologies have similar symptoms, but different treatment methods, so it is important to diagnose on time.
It is worth noting the fact that it is very difficult to diagnose this disease in newborns and infants, so the mortality rate here in this case is at a high level.
Preparing for surgery
Depending on the cause of development, timeliness of diagnosis, and general condition of the patient, surgical intervention can be urgent or planned. Before the intervention, the patient is prepared. In the case of a planned operation, it can be started at home and continued in the hospital; in case of an urgent operation, it can be done for several hours in a hospital.
Main components of the preparatory stage:
- a special diet for the intestines with enough water, excluding vegetables, fruits and bread;
- prescribing laxatives daily (Fortrans, magnesia solution, petroleum jelly);
- cleansing enemas every evening;
- the use of medications to reduce spasms (drotaverine, baralgin);
- intravenous administration of solutions to normalize the level of electrolytes, the amount of fluid, acid-base indicators, energy metabolism, protein composition of the blood;
- consultations with specialists regarding concomitant diseases, treatment with the aim of maximum correction of changes.
The amount of fluid that needs to be consumed during the day is calculated based on the daily urine output (normally - about 1.5 liters). The recommended volume is adjusted depending on the weight and functional state of the cardiovascular system, kidneys and urinary organs.
Simultaneously with preparation, it is necessary to conduct a full comprehensive examination of the patient. As a result of analyzing all the data obtained, a decision is made on the method of operation.
Indications for surgery for intestinal obstruction
Help is sought when the main symptoms of the disease in adults are observed.
In addition, the following conditions are considered indications for surgery:
- growths on the intestinal walls;
- obstruction of the intestinal lumen with stones;
- adhesive disease of the intestines and torsion;
- intussusception.
The cause of the disease is associated with a nervous disorder. In this case, treatment is treated with drug therapy. If complications arise, surgery is performed.
When medications are prescribed, the main goal of therapy is to prevent further development of obstruction. The drugs help soften, restore the peristalsis of the organ and remove the obstruction in the lumen.
Prolonged inability to push through digested foods activates the process of rotting. Therefore, sometimes the patient is diagnosed with injury to blood vessels and nerves in the area of the small or large intestine. Because of this, a process of epithelial necrosis occurs. This becomes the main reason for surgical treatment when medications are not able to help.
Definition
Often, dynamic obstruction is a deviation accompanying the underlying disease. Rarely is such a deviation independent. A lot of pathologies contribute to the occurrence of obstruction of the intestinal contents - this can be a separate serious symptom that cannot be ignored. The main cause of the disease is a violation of intestinal motor functions. Most often this is a temporary condition that goes away on its own. In other cases, if it takes a long period of time, the pathology can be fatal. It is very important to take action in time.
Possible complications
In the absence of timely and adequate treatment, the disease can lead to the development of several serious complications:
- development of peritonitis - provided that it was not the cause of the disease. Its appearance is facilitated by necrosis of the walls of the affected organ;
- intussusception - the introduction of one part of the intestine into the lumen of another;
- blood poisoning, which can occur during surgical intervention.
This development of the pathological process can be prevented if, at the first symptoms, you seek competent medical help and do not self-medicate.
Causes
The main factors in the formation of this disease remain unclear. Experts in the field of gastroenterology agree that the causes may be circulatory disorders and changes in the excitability of certain nervous systems. The following factors may predispose to the development of these conditions:
- peritonitis and other acute inflammatory processes (for example, acute pancreatitis, appendicitis);
- abdominal injuries with hemorrhages into the mesentery;
- complicated course of chronic pathologies of the digestive system;
- blockage of blood vessels;
- consequences after surgical interventions;
- fractures of the spine or pelvis;
- CNS lesions: traumatic brain and spinal cord injuries, ischemic stroke, mental trauma, uremia, etc.;
- acute mesenteric infarction;
- acute intoxication: poisoning with heavy metal salts, intestinal infections, food intoxication;
- complicated course of certain diseases of the chest and abdominal organs (for example, myocardial infarction, urolithiasis, pleurisy, etc.).
The main risk group includes people with some stage of obesity, as well as the elderly.
Treatment
Treatment of dynamic intestinal obstruction does not depend on its form; therapy is aimed at eliminating the cause.
The spastic form can be cured with conservative methods:
- drug treatment – to relieve symptoms and the main factor of the disease. To stimulate muscle peristalsis, potassium and sodium chloride and glucose are administered intravenously. Proserin, Aminazine will help start the intestines;
- cleansing enemas - for gastric lavage;
- physiotherapy.
Such measures are enough to eliminate the disease, especially for children.
Therapy for the paralytic form is carried out using surgery. A laparotomy is performed with manual alignment of the intussusception or dissection of the pathological area. You will also need to constantly probe to eliminate stagnation.
After surgery, you need to eat right. When disinvagination is performed, 6 hours after it, it is allowed to drink warm tea. On day 2 you need to adhere to dietary nutrition. In case of a cut, the liquid can be taken on the second day.
How is the operation performed?
The surgeon's task is to find and eliminate constipation, which interferes with normal bowel function. He performs an enterotomy, removes all the contents, performs a bowel resection, and creates bypass routes for food. The surgeon not only eliminates the source of inflammation, but also takes care of the general condition of the intestines. He analyzes all organs and ensures that they function well together.
Finding a mechanical obstacle is not always easy. This is especially true for the adhesive process. The surgeon and his assistant have to go through each loop manually. The following methods are used to identify obstacles:
- Extending the wound with mirrors without removing internal organs. This is the easiest way. It guarantees fast work. The assistant uses his hands or mirrors to move other organs away so that the surgeon can do his job.
- Removing internal organs and carefully examining them. The method is used in cases where the doctor cannot find the problem. The assistant tries to open the wound wide and free the necessary organs from the adjacent ones. Stretched loops are removed to create more space. The surgeon slowly moves along the tracks until a mechanical obstacle occurs.
- If the loops are very stretched, then to minimize risks, work starts from the high sections. The action begins with the Treitz connection.
- When the first methods do not help, it is worth moving from the ileocecal angle along the collapsed efferent colon. This is a convenient method, as it makes it possible to quickly sort through organs and return them to their place.
- If there is an adhesive process, it is necessary to examine the entire intestine, since there may be several obstacles.
The next stage of the operation is to extract the problem. When it comes to a food bolus or gallstone, it is important to hold it at all times. This guarantees its stability. After all, further inspection may lead to a change in location.
When eliminating a volvulus, the surgeon must carefully hold and fix the adductor and efferent colon. If there is a knot, the surgeon carefully unties it, and his assistant holds the loops so that they do not stretch.
When the problem has been eliminated, you need to take care of intestinal decompression. The Zhitnyuk method is most often used. Passing a tube through the intestines is difficult work. It requires extra care to avoid damaging anything. It is impossible to determine in advance how the tube will be inserted. He is chosen on the spot after assessing the situation. There are several rules in this regard:
- It is impossible for there to be large loops in the lumen of the cecum;
- the tube should be springy and slightly curved;
- once the tube has passed, it needs to be fixed;
- if the tube does not pass, then a more complex design is used - a uterine probe.
Enteroplication should be considered separately. This is an operation that is used for complex adhesions. Its task is to correctly position the intestinal loops so that there are no relapses in the future. The main process is resection of the greater omentum, from which the adhesive process most often begins.
Intestinal constipation can only be eliminated with professional help. There is no point in postponing a trip to the hospital, as the development of intestinal obstruction occurs very quickly.
Description of the disease
Dynamic obstruction is considered a separate type of this pathology. Very rarely, this anomaly is independent; it mainly occurs due to the presence of some kind of illness (peritonitis, infectious pathologies, pneumonia). Specialists consider the disease only when there is a need to exclude mechanical obstruction, which usually requires surgical intervention.
This deviation provokes a neurohumoral disorder in the human body and disrupts the functioning of the small and large intestines. The main reason is a change in intestinal motor function.
In most situations, this is a short-term condition that resolves spontaneously. But sometimes it is longer and can lead to death if left untreated.
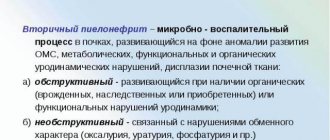
Etiology
in order to cause stasis of intestinal contents and clinical manifestations of dynamic intestinal obstruction, it is enough that not the entire intestine is paralyzed, but only some part of it. The absence of a propulsive peristaltic wave causes stagnation in the afferent segment of the intestine. Paralytic intestinal obstruction develops as a complication of various diseases and injuries of the abdominal organs. All peritonitis leads to the appearance of symptoms of paralytic obstruction. Often, paralytic intestinal obstruction complicates non-surgical diseases of the thoracic and abdominal organs, retroperitoneum (myocardial infarction, acute pleuropneumonia, pleurisy, urolithiasis, etc.).
A separate and severe group of dynamic paralytic obstruction consists of those types that arise due to acute circulatory disorders in the mesenteric vessels (thrombosis and embolism of the superior mesenteric artery)
Clinic and diagnostics
The main symptoms of dynamic paralytic obstruction are pain, vomiting, persistent retention of stool and gas, and bloating. The pain is dull, bursting in nature, and has no clear localization or irradiation. They are, as a rule, permanent; the cramping component seems to fade into the background.
Vomiting, the second most common symptom of paralytic obstruction, usually repeated, is combined with regurgitation of stagnant, foul-smelling gastric contents. The vomit is profuse, with a large admixture of duodenal and intestinal contents. Vomiting is often hemorrhagic in nature due to diapedetic bleeding from the stomach wall, as well as from acute ulcers and erosions. The abdomen is distended evenly. There is no asymmetry of swelling characteristic of mechanical obstruction. Palpation determines the rigidity of the abdominal wall. In thin patients, it is possible to palpate the loops of the small intestine stretched in the form of cylinders. Peristalsis is either sharply weakened or absent, and upon auscultation of the abdomen, instead of intestinal sounds, respiratory and cardiac sounds are heard (Lotheissen’s “deathly silence” symptom).
If paralytic obstruction is not combined with the development of peritonitis, in the first hours the general condition of the patients suffers little from it, but then, after 3–4 hours, hypovolemia, severe metabolic disorders, and cardiac dysfunction quickly begin to increase.
The diagnosis of paralytic obstruction is made on the basis of the characteristic signs of dynamic obstruction and the presence of symptoms of the underlying disease that led to its development.
Stages of the disease
A disease such as intestinal obstruction develops in three stages:
- Initial – its duration is 2–12 hours, accompanied by pain in the abdomen, flatulence and increased peristalsis.
- Intermediate – lasts 12–36 hours. The pain syndrome decreases, a period of imaginary well-being begins, meanwhile, signs of dehydration and intoxication increase.
- Terminal – occurs 2 days after the formation of the disease. The patient's condition worsens significantly, there is an increase in signs of damage to internal organs, dehydration and damage to the nervous system.
Stages of acute intestinal obstruction