How does the disease manifest itself?
Obstruction of the biliary tract is more common in women. This pathology is found in every fifth resident, so it is considered quite common.
There may be several reasons:
- GSD (gallbladder stones);
- JVP (biliary dyskinesia);
- intussusception of the gallbladder;
- neoplasms of the biliary system;
- inflammatory process of the organs responsible for the synthesis and secretion of liver secretions;
- scars and strictures in the main duct.
If one of the reasons is present, symptoms of bile duct obstruction may occur.
These include:
- nagging pain on the right side of the body under the ribs;
- yellowing of the skin, sclera and mucous membranes;
- change in color of stool and urine;
- increase in the amount of bilirubin in a blood test.
Blockage of the bile ducts can cause subhepatic jaundice. The appearance of signs of the disease is often preceded by colic associated with the movement of the stone.
If the extrahepatic bile ducts are blocked, urgent medical intervention is necessary, as the condition threatens the life and health of the patient.
Blockage of the bile ducts does not happen on its own. It is preceded by a certain pathology:
- acute cholecystitis (cholelithiasis or biliary);
- cholangitis;
- history of chronic inflammatory diseases of the duodenum;
- benign (cyst, calculus) and malignant (cancer) neoplasms of the biliary system;
- strictures and scars in the common bile duct (main duct of the liver);
- infection by worms or protozoa.
The inflammatory process present in the bile formation and excretion system can spread to neighboring organs. This is how cholecystitis spreads to the ducts, causing swelling in them. This causes stenosis of the biliary tract, resulting in stagnation of liver secretions.
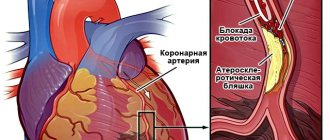
Stones formed in the gallbladder can come out with a flow of bile and clog the common bile duct. An intrahepatic calculus follows the same path. Dropsy or epiema occurs. This starts the process of damage to hepatocytes. Then dangerous substances neutralized in the liver enter the bloodstream, causing symptoms of intoxication.
Other sources of pain: external pressure
In addition to internal, the causes of biliary tract obstruction can also be external, independent of the properties and structure of the biliary tract and bladder. Quite often, blockage of the bile ducts leads to:
blockade of the liver gates by enlarged lymph nodes (metastases of a malignant tumor from another organ);- mechanical pressure of the head of the pancreas during its cancerous degeneration;
- echinococcus, localized in the gates of the liver,
or similar “suffocating” diseases and conditions.
A common cause of bile duct obstruction are conditions leading to swelling of the large duodenal (Vater's) papilla.
The severity and nature of the pain also depend on the size of the blocked duct: if there is a blockage of the common bile duct, the pain will be much more intense and the consequences will be more serious.
Diagnostics
A blood test when the outflow of bile is blocked will show hypothrombinemia (reduced coagulation), an increase in acute phase proteins of inflammation (C-reactive) several times in the presence of an infectious process.
Based on complaints and examination, a set of diagnostic measures is prescribed. In addition to the blood test, it includes:
- Ultrasound (ultrasound diagnostics);
- RCP (retrograde cholangiopancreatography);
- MRI (magnetic resonance imaging);
- CT (computed tomography).
The last two methods involve large financial costs, are available only in large cities (Moscow, St. Petersburg, regional centers) and are prescribed in extreme cases. The identified changes allow us to draw a conclusion about the severity of the disease, the degree of occlusion and possible treatment options.
In some cases, diagnostic endoscopy is indicated, after which pneumobolism of the bile ducts persists for some time.
Treatment of narrowing of the bile ducts is based on the data obtained during a diagnostic study and consists of expanding the lumen. If obstructive changes have led to deep intoxication of the patient, he is transferred to the intensive care unit until his condition is stabilized and the symptoms of poisoning with intrahepatic poisons are relieved.
If an ultrasound shows that the gallbladder or the main hepatic canal is clogged with stones, the stones are extracted, an artificial outflow (nasobiliary drainage) is installed using a probe for formations and fluid, and a choledochostomy/cholecystostomy is performed. During treatment, the patient is prescribed choleretic drugs to speed up recovery and increase the effectiveness of therapy.
Methods of therapy
If the bile ducts are blocked, then the blockage will need to be cleared and the obstruction removed. When stones are present, they will need to be removed from the bladder. The stones are destroyed using an endoscope during a special procedure.
In some cases, it is necessary to remove the bladder if there is a risk of dangerous complications. When tumors are present, endoscopic treatment methods are required.
Quite often, doctors prescribe drug therapy. In particular, antispasmodics such as No-shpa, Drotaverine, Papaverine and Baralgin are prescribed. In addition, choleretic agents are often required: Flomin, Allochol and Holosas. Anti-inflammatory drugs may be needed, for example, Ibuprofen, Ketorolac and Ursafalk. In certain situations, doctors prescribe antibiotics.
Treatment methods should also be considered depending on what disease you are dealing with:
- Chronic cholecystitis. First of all, the patient will need to follow a strict diet. During periods of exacerbation, bed rest is prescribed. Therapy includes the use of antibacterial agents, enzyme preparations, and antisecretory drugs. To relieve symptoms, doctors prescribe antispasmodics.
- Acute cholangitis. To eliminate pain, you will need to use antispasmodics and painkillers. The doctor also prescribes broad-spectrum antibiotics, enzymes and anti-high fever medications.
- Conglomerates in the hepatic ducts. You will need to follow a special diet to be able to improve the condition of the organ. A person will need to monitor his weight so that it is within the normal range. The person will be prescribed special medications based on ursodeoxycholic acid. To eliminate pain symptoms, you will need to use analgesics or anti-spasm medications. Antibiotics are prescribed according to indications.
- Biliary dyskinesia. In such a situation, choleretic drugs, as well as herbal remedies, will be prescribed. A diet must be prescribed to normalize well-being. In addition, antispasmodics and sedatives may be required.
If we talk directly about diet, then it will definitely be needed for problems with the bile ducts. First of all, you will need to exclude from your diet foods containing large amounts of fat and cholesterol. In addition, you will need to avoid fried, spicy, salty and pickled foods. You will need to exclude coffee and strong tea.
Preference should be given to fruits, berries, and low-fat varieties of fish. Vegetables will also be useful, as they have a good effect on the digestive system. In any case, you need to observe how the body perceives various foods.
It is also necessary to treat pathology using folk remedies. For example, a mint-honey mixture that can be stored in the refrigerator will be useful. To prepare it, you will need to take dry peppermint, as well as flower honey. All components will need to be mixed, and the product should be taken once a day, a teaspoon. In addition, it is recommended to use herbal decoctions. Tinctures made from corn silk, sage, oats and speedwell will be useful.
If you choose the right treatment regimen, it is imperative to undergo a full medical diagnosis. In this case, you will be able to understand exactly what you are dealing with.
Causes of blockage
Bile is produced in the liver, stored in the gallbladder, and used in the duodenum and small intestine. After each meal, a small portion of bile from the duodenum goes directly into the intestines, where it must digest fats, especially animal origin and vitamins. The rest of the bile remains in the gallbladder.
Partial or complete obstruction of the biliary tract is distinguished. The following may be responsible for the development of blockage of the intrahepatic ducts:
- cysts and stones in the bile ducts, stuck in them and partially or completely clogging the lumen;
- scars and strictures in the ducts;
- parasitic infestations.
Biliary tract obstruction can also be caused by:
- cholangitis and cholecystitis;
- chronic pancreatitis;
- pancreatic tumors;
- infections of the liver, bladder and intestines;
- recent operations on these organs;
- injuries to the right half of the abdominal cavity.
Fluctuations in body weight, both obesity and too rapid weight loss can also cause blockage of the common bile duct.
Obstacles inside the duct
The outflow of bile may become difficult (or stop altogether):
- due to an obstruction inside the duct;
- due to changes in its wall;
- due to mechanical compression from the outside.
The first group of causes of obstruction includes stones, the presence of individual large parasites (roundworms) or their clusters in the bile ducts. It could also be a tumor growing into the lumen of the duct and impeding the outflow of bile, or a powerful inflammatory process occurring in the mucous membrane of the bile duct, leading to a narrowing of its internal diameter.
Blockage can be caused by stones inside the ducts.
Changes in the structure of the wall of the ducts themselves - their cysts, scars of any etiology (arising from trauma, surgery, cirrhosis of the liver), strictures should also be equated to causes of an “internal” nature.
The intensity and severity of pain depend on the speed of onset of biliary tract obstruction. If an obstacle to the movement of bile appears suddenly, completely blocking the lumen of the bile duct, the pain will be intense and acute.
When an obstacle is created slowly, minimal clearance remains for movement. Bile also accumulates slowly above the obstruction, causing a gradual stretching of the pathways that carry it out, and then the pain is less pronounced and more smoothed out. Such gradually “accumulating” pain will not lead the patient to the doctor immediately.
An example of such an obstacle is an incomplete bend of the neck of the gallbladder, or its stricture, or adhesions, strictures of the ducts. It could also be a plug of thick mucus, bile and desquamated epithelium that does not completely block the duct.
Pathogenesis of bile duct obstruction
Bile, passing through blocked ducts, can no longer move at normal speed. It begins to accumulate in the place where there is an obstacle, stretching the walls of the elastic tube. Often, inflammation soon develops here, as a result of which the mucous membrane thickens, which in turn also helps to reduce the diameter of the ducts.
Next, bile is absorbed into the bile ducts and a serous-mucous liquid, called white bile, begins to be released from their mucosa.
This phenomenon indicates severe damage to the liver tissue, resulting in:
- dysfunction of this organ;
- disorder of fat and carbohydrate metabolism;
- pathological changes in internal organs, for example, in the kidneys and heart.
In the liver itself, if a blockage occurs in it, the accumulated bile has a toxic effect on its cells - bilirubin and bile acids cause their destruction. Long-term stagnation of bile in the liver can cause severe pathologies of this organ, including liver failure. Also, bile substances can enter the blood and cause intoxication and damage to both the blood vessels themselves and body organs.
Anatomy and structure
For the full functioning of the digestive tract, bile produced by the liver is necessary. Transport of secretions into the gastrointestinal tract is carried out by the bile ducts. If their work is disrupted, digestive problems appear.
The bile ducts are conventionally divided into two groups. Classification is carried out depending on the location of the channels. There are:
- Intrahepatic bile ducts. The ducts are located inside the tissue of the organ, arranged in neat rows of small ducts. Small vessels form a system reminiscent of a tree. The system is similar to a circulatory network. The function of these ducts is to collect bile in the liver. Liver cells secrete bile, which penetrates into the space of small bile passages, and through the interlobular canals enters the large ones. Gradually copulating, the canals form a segmental duct extending beyond the organ.
- Extrahepatic bile ducts. Located outside the organ. The system includes the left and right lobar canals, which unite into the common hepatic duct. It removes bile from the organ.
The cystic duct acts as a link between the liver and gallbladder. The common bile duct originates from the place of copulation of the hepatic and cystic ducts and flows into the duodenum. A certain part of the bile goes to the common bile duct, without entering the gallbladder.
The longest is the common bile duct, which consists of 4 sections. The first section (supraduodenal) has a length of up to 4 cm and stretches from the entrance of the cystic duct to the upper border of the 12 signets of the intestine. The next section (retoduodenal) has a length of 1 to 2 cm and passes behind the 12 rings of the intestine.
The bile ducts form a network and function in two directions. When food does not enter the gastrointestinal tract, the sphincter, which is a muscle bundle, closes.
As a result, the produced bile accumulates in the bladder. At this time, bile acquires a dark olive color, the percentage of enzymes increases several times. After food enters the intestines, the outlet opens, the bile valve contracts and fluid is released into the gastrointestinal tract.
Through the common bile duct, liver secretion enters the digestive system, where the digestive bolus is broken down with the participation of bile acids.
Obstruction of the bile ducts provokes a violation of the digestive tract, which is detected by various pathological conditions.
Symptoms of bile duct obstruction
Symptoms of bile duct blockage include many components.
This:
- skin itching, rashes;
- yellow discoloration of the skin, sclera and mucous membranes;
- bitterness in the mouth and coating on the tongue;
- bad breath;
- pain in the right hypochondrium;
- headache;
- enlarged belly;
- slowing and decreasing heart rate;
- slowing down blood clotting;
- light-colored and unpleasant-smelling stools;
- dark, bilirubin-stained urine.
In advanced cases of the disease, swelling and sweating, as well as intellectual impairment, may be observed. Since these are symptoms that can also manifest themselves in other gastrointestinal diseases, the diagnosis is established only after special diagnostic measures have been carried out.
Signs of chronic cholangitis
- recurrent fever
- muted pain of low intensity in the right hypochondrium
- feeling of "bloating" in the upper abdomen
- at a severe stage it may be accompanied by obstructive jaundice
- low-grade body temperature (within 37-38 degrees)
- frequent fatigue
The symptoms of sclerosing cholangitis are similar to the acute and chronic subtypes. But sometimes it can be aggravated by the development of multiple abscesses (purulent inflammation of tissue) of the liver, sepsis (“blood poisoning”), and toxic shock.
Diagnosis of bile duct blockage
To diagnose patients, they take a biochemical blood test, the results of which exclude cholecystitis, cholangitis, and establish the level of bilirubin, liver enzymes and alkaline phosphatase.
Hardware research methods are prescribed:
- Ultrasound, which makes it possible to determine whether there are stones in the bile ducts and pneumobilia of the bile ducts, that is, the presence of air in them, which can occur as a complication of hepatic and biliary diseases.
- Laparoscopic or endoscopic examination. With their help, the presence of cysts and stones in the bile ducts is determined. They are prescribed if the symptoms of the disease are not very pronounced and there is an assumption that the disease is still in a mild form. The diagnostic tool is also used to take a piece of tissue (if there is a suspicion of cancer), as well as for treatment - it is used to remove stones in the ducts.
- MRI and CT scans provide detailed images of the ducts of the liver, pancreas and common bile duct.
If the diagnosis of “biliary tract obstruction” is confirmed, then therapy is prescribed based on the results of the studies.
Treatment
The main specialists involved in the fight against pathology are a surgeon and a gastroenterologist. Treatment of biliary obstruction consists of surgical and conservative measures. Surgical intervention comes first in importance. Therapeutic treatment is auxiliary in nature and includes detoxification, anti-inflammatory, and antibacterial therapy.
A patient with urinary tract obstruction is not always initially in a stable condition. In such situations, take gentle measures:
- Gallbladder puncture;
- Cholecystostomy;
- Choledochostomy;
- Percutaneous transhepatic drainage (ensuring the outflow of bile through the drainage system that has accumulated above the blockage);
- Removal of stones during RCP;
- Nasobiliary drainage for GCHD (installation of a catheter in the bile ducts).
After stabilization of the patient's condition, treatment of the bile ducts is carried out more radically. If possible, all manipulations are performed through laparoscopic access. If for some reason it is impossible (for example, due to complications), they resort to laparotomy. Some types of interventions:
- Bougienage of the bile ducts. When they are obstructed due to strictures and scars.
- Biliary tract stenting. Installation of a special tube at the site of stenosis.
- Cholecystectomy. Removal of the gallbladder.
- Expansion of the sphincter of Oddi. Used when its patency is impaired.
Treatment of bile duct obstruction
Treatment of blocked ducts aims to partially or completely free them from the blockage. One of the possibilities for removing stones from the ducts is the use of an endoscope during endoscopic cholangiopancreatography, as well as endoscopic papillosphincterotomy. These operations are prescribed if the narrowing of the bile flows is slight or they are clogged with small stones.
The patency of the ducts is also restored using a stent - a hollow tube that is installed in the clogged ducts. It also helps to expand the duct if its narrowing is caused by a tumor. After some time, another operation to replace the stent may be necessary.
If the blockage is caused by stones in the gall bladder, then it is removed (cholecystectomy). Ductal sphincterotomy is used if stones are present simultaneously in the gallbladder and ducts.
In addition, traditional medicine is also used.
To improve bile flow, patients can take:
- 1 glass of apple juice with 1 tbsp. l. apple cider vinegar;
- 1 glass of water with 4 tbsp. l. lemon juice;
- decoction of mint;
- juice from 1 cucumber and beets, 4 carrots.
Any of these medications must be taken daily for at least 2 weeks to feel the results. But traditional treatment is not a replacement for traditional treatment, but only complements it.
Gallbladder blockage - symptoms.
The main symptoms of blockage of the gallbladder duct should be known in order to recognize a dangerous pathology in time. Blockage of the bile duct is a blockage of the channel that comes from the organ by a stone that comes out of it along with the flow of bile. It is worth considering a description of the signs and methods of treatment of this pathology.
Bile is a yellow-green substance that is produced in the liver and stored in the gallbladder. From there it penetrates through the pancreas into the small intestine. The main task of this liquid is to digest lipid structures that come with foods. After eating food, this substance comes from the gall bladder, which begins digestion and cleansing the liver of toxins and breakdown products.
How to diagnose bile duct blockage?
The clinical picture of this pathology at an early stage of its development resembles the symptoms of cholecystitis or hepatic colic.
These external signs may lead to hospitalization of the patient.
Initial diagnosis is carried out using an abdominal ultrasound procedure. If gallstones are detected, magnetic resonance cholangiography or computed tomography may be prescribed to search for them in the bile ducts.
In order to clarify the causes that cause obstructive jaundice, as well as to determine the location of the stone and the degree of blockage of the lumen of the duct, the technique of percutaneous transhepatic cholangiography and the method of dynamic scintigraphy of the biliary system are used. These instrumental diagnostic methods make it possible to identify disturbances in the dynamics of bile and bile outflow.
The most informative method for diagnosing biliary tract obstruction is considered to be the method of retrograde cholangiopancreatography, which involves simultaneous endoscopic and x-ray examination of the bile ducts. If stones are detected in the lumen of the bile duct, during such a procedure it is possible to extradite the stone from the common bile duct, and if a tumor is detected compressing the duct, it is possible to take a biopsy from it.
If we talk about laboratory diagnostic methods, they can reveal the following:
- biochemical liver tests reveal elevated levels of direct bilirubin, transaminases, alkaline phosphatase, blood lipase and amylase;
- a general blood test determines leukocytosis, in which the leukoformula shifts to the left;
- this analysis also makes it possible to detect a decrease in the level of platelets and red blood cells characteristic of this pathology;
- The coprogram in this disease is characterized by a significant content of fat in the feces and the absence of bile acids.
Why does the gallbladder duct become blocked?
Blockage of the gallbladder duct occurs due to various reasons that have a direct connection with the organ and its pathways, the liver, and the small intestine:
- the presence of stones in the gall bladder;
- inflammation in the ducts;
- neoplasms;
- scarring of tissue and narrowing of the lumen;
- injuries;
- pancreatitis;
- an increase in the size of lymph nodes in the liver;
- the appearance of strictures;
- neoplasms in the pancreas or other organs of the gastrointestinal tract;
- hepatitis;
- helminthic infestation;
- cirrhosis of the liver.
These provoking factors can cause blockage of the bile duct with all the ensuing symptoms;
Normal and enlarged gallbladder - how they differ
The gallbladder is a temporary reservoir for bile.
It is constantly produced by the liver and flows through the bile ducts into the bladder, where it should remain for several hours (before the first meal). As soon as food enters the lumen of the duodenum, the gallbladder contracts and bile is released into the intestine. This should be normal and necessary so that bile participates in digestion only when needed. It should not irritate the duodenal mucosa when there is no food mass in its lumen. Average sizes of a healthy gallbladder in an adult:
- Length – 14–15 cm;
- Width – 2.5–4.0 cm;
- Volume – 20–30 ml.
An enlarged gallbladder is an excess of the specified normal parameters. This means that he:
- Expanded – the size and volume are larger than expected;
- Full of bile;
- Unable to fully contract;
- Turned off from digestion - accumulated bile stagnates in it;
All these changes can be either a dangerous deviation from the norm or a temporary adaptive reaction of the body.
The first symptoms of a blocked gallbladder duct
Symptoms of blockage of the gallbladder duct are characterized by increasing character. But in some cases, symptoms may occur over a short period of time and increase rapidly. In many cases, symptoms of blockage appear after the bile ducts are affected by an infectious process. A person rarely immediately pays attention to the symptoms of the first stage of the disease, starting treatment only when the blockage has reached a serious stage.
Often a person consults a doctor when symptoms such as blockage of the bile duct, elevated body temperature and severe pain appear. At this stage of the disease, symptoms are accompanied by sudden weight loss, as well as severe paroxysmal pain in the lower abdomen on the right. The skin becomes yellowish, the person notices that he has severe itching of the skin of a systematic or periodic nature. This signals that the gall blockage has developed into a serious stage.
You should also pay attention to the fact that if there is a lack of bile acids in the intestines, further consequences of this condition may occur:
- Lack of color in stool.
- Bilirubin begins to be actively excreted by the kidneys, so the urine becomes intensely dark in color.
- If the canals are partially blocked, there is a high probability of periodic alternation of discolored feces with a substance of a specific shade.
- At the initial stage of bile duct blockage, symptoms that resemble jaundice often appear. Among them is a yellowish tint of the epidermis and the whites of the eyes.
- All mucous membranes on the human body can acquire a yellowish tint.
- At a serious stage of development of the pathological process, symptoms such as tremors of the limbs and intense sweating often occur.
If a person with such a diagnosis is not provided with timely medical care, medical prognosis is not very favorable. Therefore, it is important to know the risk factors that increase the likelihood of developing this pathological condition:
- Pain in the right hypochondrium. The etiology of pain can be different, the pain can be sharp or paroxysmal, stabbing or weakly pulling.
- Urine is dark in color, this sign should cause concern immediately after its appearance.
- Hyperthermia, tremors of the upper and lower extremities, intense sweating.
- Itching of the epidermis.
- Signs of jaundice are yellowness of the skin, sclera of the eyes, yellowness of the mucous membranes.
- Regular nausea, periodic vomiting with bile, which does not bring the desired relief.
- Discoloration of stool, in which undigested lipid structures are clearly visible, this sign indicates a deficiency of secreted bile.
Bile ducts
I
Bile ducts (ductus biliferi)
a system of ducts that drain bile from the liver and gallbladder into the duodenum. There are intrahepatic and extrahepatic bile ducts, which include the right and left hepatic ducts, the common hepatic duct, the cystic duct, and the common bile duct ( Fig. 1 ). The common hepatic duct is formed by the fusion of the right and left hepatic ducts, which drain bile from both lobes of the liver. The cystic duct arises from the neck of the gallbladder and merges with the common hepatic duct to form the common bile duct. The latter is divided into 4 parts: supraduodenal, retroduodenal, retropancreatic and intramural, which opens on the large papilla of the duodenum (papilla of Vater), forming the common mouth of the common bile and pancreatic ducts - the hepatic-pancreatic ampulla ( Fig. 2 ). These features of the anatomy of the general pancreas make it possible to compress it with the development of obstructive jaundice with tumors of the head of the pancreas and the papilla of Vater.
The bile ducts are innervated by branches of the hepatic nerve plexus. The blood supply comes from the hepatic artery proper, and the blood flows into the portal vein. Lymphatic drainage is directed to the lymph nodes located along the portal vein, which are closely connected with the lymphatic tracts of the gallbladder, liver, and pancreas. Bile moves into the gallbladder as a result of the secretory pressure of the liver, the motor function of the gallbladder, sphincters, and the tone of the walls of the gallbladder.
Research methods . Duodenal intubation (see Duodenal intubation) allows you to detect signs of inflammation of the biliary tract (presence of leukocytes, duct epithelium in bile), tumor cells, Giardia, Echinococcus larvae, etc.; the presence of blood may indicate hemobilia (see Liver). To assess the condition of the gastrointestinal tract, radiocontrast research methods are of primary diagnostic importance - intravenous (including infusion) cholangiography, fistulography, retrograde pancreatocholangiography, percutaneous transhepatic cholangiography. Ultrasound examination (see Ultrasound diagnostics) and computed x-ray tomography can also assess the condition of the liver and pancreas. Despite the great information content, an accurate diagnosis using these methods is established in approximately 70% of observations. Therefore, a comprehensive intraoperative examination of the gastrointestinal tract (measurement of their diameter, transillumination, probing, telecholangioscopy and cholangiography, as well as choledochoscopy - examination of the lumen of the gastrointestinal tract using a special device - choledochoscope) is of decisive diagnostic importance.
Pathology. Malformations of the ducts include atresia (absence of the lumen of the ducts), hypoplasia (narrowing of the lumen of the ducts), cysts, diverticula and doubling of the ducts, displacement of their mouth. Malformations of the stomach are characterized by obstructive jaundice, which appears with atresia and hypoplasia in the first days of a child’s life. Jaundice increases, skin itching occurs, the content of bilirubin in the blood increases (usually direct), stercobilin is absent in the feces, and the urine darkens. Hepatomegaly quickly develops, and then the symptoms of portal hypertension (Portal hypertension) - splenomegaly, gastrointestinal bleeding. With cysts and diverticula of the stomach, obstructive jaundice appears at the age of 10-15 years and is not permanent.
The diagnosis of atresia and hypoplasia of the pancreas is based on data from laparoscopic or intraoperative cholecystocholangiography. With a cyst, diverticulum, and displacement of the orifice of the gastrointestinal tract, the leading role in diagnosis belongs to intravenous or retrograde cholangiography. Treatment is only surgical: as a rule, the formation of an anastomosis between the dilated sections of the duct and the duodenum.
Damage to extrahepatic glands can be closed or open. Closed isolated injuries to the pancreas are rare. Open injuries to the stomach are usually combined with injuries to the liver, stomach, and intestines. Damage to extrahepatic glands is possible during surgical interventions (cholecystectomy, gastrectomy), as well as during their intraoperative instrumental examination.
Damage to the gallbladder is diagnosed by the resulting leakage of bile into the abdominal cavity or out through a wound. In the case of ligation of the gastrointestinal tract after surgery, as a rule, obstructive jaundice appears. Damage to the gland leads to the development of peritonitis, external biliary fistulas (Biliary fistulas), and strictures of the gland. The latter usually appear after 4-6 months. after damage. Glandular strictures are recognized based on the symptoms of recurrent cholangitis, intermittent obstructive jaundice or non-closing external biliary fistula, as well as data from intravenous or retrograde cholangiography, fistulography. Treatment is always surgical.
Diseases. The most common disease of gallstones is choledocholithiasis (see Gallstone disease). Gastrointestinal dyskinesia occurs as a result of neurohumoral disorders of the mechanisms regulating the function of the biliary tract. Clinically, dyskinesia of the stomach is manifested by dull or sharp pain, usually short-term in the upper abdomen, radiating to the back and right shoulder blade. Body temperature does not rise, chills, fever, hepatomegaly are not observed. The diagnosis is made on the basis of characteristic clinical symptoms and the exclusion of the organic nature of the disease (see Biliary dyskinesia).
Cholangitis often develops as a result of an inflammatory process in the gallbladder or ascending infection of the gallbladder from the intestine. The clinical picture is especially pronounced with purulent cholangate - fever, chills, jaundice, hepato- and splenomegaly, and progressive liver failure are observed. The most effective method of treating purulent cholangitis is adequate drainage of the general gastrointestinal tract, which, due to the serious condition of patients, is preferably done using endoscopic napillosphincterotomy. If it is impossible to perform it, surgical intervention is indicated - choledochotomy and drainage of the lumen of the common bile duct. Subsequently, an antibiotic is injected into the lumen of the bile ducts.
Parasitic infestations of stomachs are common. In the ducts, protozoa (giardia, etc.) helminths (roundworms, whipworms, cat and liver flukes, bovine and pork tapeworms, broad tapeworms, larvae and cysts of echinococcus, etc.) can be found. Parasitic invasion of the stomach can be asymptomatic, sometimes accompanied by purulent cholangitis with severe intoxication, which may require surgical intervention.
Tumors of the stomach are rare. They can be benign (fibroma, neurofibroma, cholangioma, lipoma, myxoma, papilloma, fibroids, etc.) and malignant (cancer). Benign tumors, as they grow, cause a narrowing of the lumen of the gallbladder and disruption of the outflow of bile. This is accompanied by pain in the right hypochondrium, sometimes like hepatic colic, and obstructive jaundice. The clinical picture resembles cholelithiasis. Diagnosis is difficult, even during surgery. Differential diagnosis should be made with stones and a malignant tumor. Benign tumors G. pI. subject to removal due to the risk of developing obstructive jaundice and the possibility of malignancy. For this purpose, sometimes they resort to resection of the duct segment along with the tumor and the imposition of a biliodigestive anastomosis.
Malignant tumors are localized more often in the ampullary section of the common gastrointestinal tract, as well as at the confluence of the cystic and common hepatic ducts. An early symptom is increasing obstructive jaundice that occurs without a previous painful attack. The content of bilirubin in the blood serum quickly reaches high levels (300 µmol/l or more), the level of cholesterol and alkaline phosphatase in the blood increases. Excruciating skin itching appears. With the development of cholemia, subcutaneous hemorrhages and gastrointestinal bleeding are observed. Weight loss and general weakness progress, the liver is enlarged and dense. When a malignant tumor is localized distal to the confluence of the cystic duct and its occlusion of the common gallbladder, jaundice is observed, biliary hypertension and distension of the gallbladder develop, which reaches a significant size and is easily palpated through the anterior wall (Courvoisier's symptom).
The diagnosis of a malignant tumor of the pancreas is difficult even during surgery. The pronounced clinical picture allows one to suspect it, especially in the presence of Courvoisier’s symptom. The diagnosis is clarified using laparoscopic and percutaneous (transhepatic) cholangiography (Cholangiography).
Treatment of malignant tumors of the pancreas is only surgical, but radical surgery (resection of the pancreas with tumor) is possible in rare cases. Palliative interventions are biliary operations (cholecystoduodeno- or cholecystoenteroanastomosis).
Operation on the gastrointestinal tract. To access the extrahepatic gastrointestinal tract, various incisions are used: oblique in the right hypochondrium, longitudinal (including the upper median), transverse, and angular. The most common oblique subcostal incisions are on the right. Operations on the bile duct are performed to remove stones from their lumen (choledocholithotomy), for tumors (resection of the ducts), in case of damage to the bile duct (suture of the duct) and to restore the outflow of bile - biliodigestive anastomoses: for example, anastomosis of the common bile duct with the duodenum (choledochoduodenostomy) or jejunum (choledochojejunostomy). After removing the stones, the choledochotomy opening is sutured and the common bladder is drained through the stump of the cystic duct or a T-shaped drainage is left in its lumen, which is removed after 14-16 days. Patients are discharged after surgery on the 15-20th day. The period of disability after discharge is usually 1-1.5 months.
Bibliography: Vinogradov V.V., Zima P.I. and Kochiashvili V.I. Obstruction of the biliary tract, M., 1977; Vishnevsky A.A., Ulmanis Ya.L. and Grishkevich E.V. Biliary anastomoses, M., 1972; Galperin E.I., Kuzovlev N.F. and Karagyulyan S.R. Cicatricial strictures of the bile ducts, M., 1982, bibliogr.; Clinical surgery, ed. Yu.M. Pantsyreva, p. 298, M., 1988; Lindenbraten L.D. Radiology of the liver and biliary tract, M., 1980; Milonov O.B. and Timoshin A.D. Complex study during operations on the biliary tract, M., 1981, bibliogr.; Nechai A.I., Stukalov V.V. and Zhuk A.M. Non-operative removal of stones from the bile ducts during their external drainage, L., 1987, bibliogr.; Niederle B. et al. Surgery of the biliary tract, trans. from Czech, Prague, 1982; Pantsyrev Yu.M. and Gallinger Yu.I. Operative endoscopy of the gastrointestinal tract, M., 1984; Tskhakaya Z.A., Vinogradov V.V. and Mamamtavrishvili D.G. Surgery of choledocholithiasis, Tbilisi, 1976; Shalimov A.A. and others. Surgery of the liver and bile ducts, Kyiv, 1975.
Rice. 2. Diagram of the connection of the common bile and pancreatic ducts with the formation of a common hepatopancreatic ampulla: 1 - common bile duct; 2 - accessory duct of the pancreas; 3 - pancreatic duct; 4 - duodenum.
Rice. 1. Diagram of the typical location of the cystic and common hepatic ducts: 1 - gallbladder; 2 - cystic duct; 3 - common hepatic duct; 4 - common bile duct; 5 - duodenum.
II
Bile ducts (ductus biliferi)
ducts that drain bile from the liver and gallbladder into the duodenum.
Extrahepatic bile ducts are bile ducts located outside the liver; include two hepatic ducts, the common hepatic duct, the cystic duct and the common bile duct.
Intrahepatic bile ducts are bile ducts located in the liver tissue; include bile and interlobular ducts.
Bile ducts are interlobular - see Interlobular ducts.
Source: Medical Encyclopedia on Gufo.me
- Blog
- Jerzy Lec
- Contacts
- Terms of use
© 2019 Gufo.me
Therapeutic measures
The key goal of treating a blockage is to free the bile duct from the obstruction or to significantly improve the patient’s well-being. Stones stuck in the gallbladder are often removed through the use of an endoscope during a diagnostic procedure, which includes examination of the abdominal organs.
Sometimes treatment of the disease is carried out exclusively through surgery to remove the obstruction that has blocked the ducts. If the obstruction is caused by a stone, the gallbladder is surgically removed. After the operation, the patient will need to undergo a course of antibacterial agents, which the doctor selects individually for each patient. Antibiotics are prescribed if the doctor suspects an infectious process.
The most common methods of treating obstruction:
- Complete removal of the gallbladder through surgery.
- Treatment with an endoscope is used to remove small stones or to install a stent, which will subsequently expand the ducts.
- Sphincterotomy is used by the doctor if stones are found in multiple quantities both in the bile ducts and in the organ itself.
It is important to consult a doctor in a timely manner for treatment. It should be remembered that self-medication for such a pathological condition is unacceptable.
Folk remedies
The use of traditional medicine makes it possible to maintain the results of a therapeutic course, prevent the occurrence of pathological conditions associated with disruption of the bile ducts, and strengthen the biliary system.
St. John's wort decoction
The healing drink has an anti-inflammatory effect. You need to take 1 tbsp. l. St. John's wort, pour 200 ml of boiling water and put on low heat for 15 minutes. After time, the composition must be filtered. You need to drink ¼ cup of the decoction a few minutes before meals 3 times a day.
1 tbsp. l. dry herbs are poured with a glass of boiling water, left for an hour, then filtered. Take ¼ cup 30 minutes before meals 3 times a day.
1 tbsp. l. mint, pour 200 ml of boiling water and leave in a closed container for half an hour. Should be taken 3 times a day in small sips.
Lemon juice
Every day, every 2 hours, it is recommended to take two tablespoons of freshly squeezed lemon juice.
Hercules flakes
You need to infuse Hercules flakes in hot water, cool and take half an hour before meals - morning and evening.
Melon seeds
You need to make flour from dried melon seeds. Pour 1 cup of flour with 1 cup of boiled milk. Leave for 1.5 hours, strain and drink half a glass on an empty stomach in the morning. The method is effective for dyskinesia.
Prevention
Following the rules of a healthy diet and lifestyle will help you avoid a pathological increase in gallstones. Compliance with food intake, avoidance of alcohol, and emotional well-being will help you avoid diseases of the digestive system. Regular examination of the gastrointestinal tract will reveal pathological processes in time.
An enlarged gallbladder is a symptom of digestive diseases. In the absence of timely treatment, the pathology causes life-threatening complications.
Symptoms
The clinical course is directly related to the degree of obstruction, its duration and the main cause. Symptoms of blocked bile ducts:
- Pain syndrome. The most typical localization is the area of the right hypochondrium. The complaint is pronounced and may be cramping in nature.
- Jaundice. The color of the skin and sclera changes. With prolonged disruption of the outflow of bile, skin itching is often a concern.
- Change in color of stool and urine. The feces become discolored and the urine becomes darker. If the obstruction is transient, their change may be periodic.
- Hyperthermia. Occurs against the background of inflammation of the gallbladder and gallbladder.
- Asthenovegetative syndrome. Weakness, increased fatigue, drowsiness.
As congestion progresses, severe toxic damage to almost all organs and systems is possible. Therefore, measures to eliminate biliary obstruction should be taken as early as possible.
Important! Vitamin K deficiency is one of the pathological causes of decreased blood clotting. With prolonged obstruction of the gallbladder, there is a tendency to bleeding.
Normal Ultrasound Characteristics in Adults
Ultrasound scanning is one of the most informative methods for studying the condition of the common bile duct. It is performed simultaneously with an ultrasound of the gallbladder. During the examination, the main duct is not completely visualized - this is normal. On transverse scanning, it is determined as an oval hypoechoic structure.
Age-related changes lead to thickening of the duct wall, so in older people the degree of echogenicity increases. Removing the gallbladder does not affect the size of the biliary tract in any way. The exception is damage to the ductal system during surgery. Normally, the bile duct has an elastic structure without additional formations.
The diameter of the common bile duct differs in different places, which means that it is advisable to carry out measurements in several areas:
- in the area of the porta hepatis – 4–6 mm;
- at the level of the retroduodenal region, the common bile duct is from 4 to 8 mm;
- in the area of the distal third it narrows to 2–5 mm.
Scientific articles on professional medical websites contain comments from doctors about the use of a new improved technique - endoscopic ultrasound diagnostics. This is a study of the ductal system using an endoscopic probe with an ultrasound probe at the end. It is introduced through the duodenum and allows you to examine sections that are not visible with the traditional method. This invention is valuable for accurate diagnosis of choledocholithiasis and tumor lesions in the retroduodenal part of the canal.
Causes of gallbladder enlargement in children
Even infants can encounter a pathological condition, but often in childhood other causes lead to the problem. It is important to determine the presence of a specific pathology in order to understand why the gallbladder is enlarged.
Common reasons:
- Scarlet fever.
- Hepatitis or obstructive jaundice. They are caused by small stones in the ducts.
- Dyskinesia of the bile ducts. It can be diagnosed even in infants.
- Gastroenteritis and pancreatitis.
- Helminths and infection of the digestive system with E. coli.
- Twisting of the bile ducts.
An enlarged gallbladder can occur with abnormal development of the organ, as well as with the appearance of polyps. Infants often encounter similar problems when consuming artificial formulas, poor diet, or excessive feeding. In childhood, the problem is provoked by fatty and low-quality foods, which are harmful even for an adult.
Possible complications
If left untreated, an enlarged gallbladder can cause dangerous pathologies. Secretions accumulate in the organ, expanding the walls, which gradually become thinner. There is a threat of perforation, as a result of which bile enters the abdominal cavity, causing peritonitis. This condition poses a threat to the patient's life.
If the gallbladder is enlarged for a long time, stagnation of the secretion, changes in composition, and the threat of stones appear. Dysfunction of the organ leads to disruption of the housing and communal services. Food is not digested, the body does not receive the necessary nutrients. A person may lose weight and suffer from vitamin deficiency. To avoid dangerous complications, it is necessary to treat an enlarged gallbladder.
Determination of gallbladder diseases on ultrasound
Gallstones, due to their significantly higher density compared to bile and due to the reflection and absorption of ultrasound by them, are manifested echographically by two phenomena: echo-positive, which looks like bright “flares,” and echo-negative, in the form of a so-called acoustic shadow. A characteristic feature is their displacement when the patient’s body position changes. Stones that are suspended or surrounded by bile on three sides are better detected. The minimum size of stones detected by echography is 1.5-2 mm. But they give a small echo signal and do not form an acoustic shadow, so the only evidence of the presence of small stones in these cases is the mobility of the “flares” when the patient’s body position changes. The task is significantly easier with larger stones, starting from 3-4 mm, when in addition to “exposure” they provide an acoustic track. Small stones are usually slightly convex, while large stones are curved. As the size of the stones increases, the curvilinearity increases. Single stones have the appearance of separate echo-positive formations with acoustic tracks corresponding to them in width. In the presence of a large number of stones adjacent and layered on top of each other, a wavy summary echo signal appears with a wide continuous acoustic shadow shielding the rear wall of the bubble. A gallbladder completely filled with stones is not visualized. Instead, a band of bright lights with wide echo-shadow reflected from the stone conglomerate is revealed - a “corona symptom”. Despite the unity of the pathomorphological process and the fundamental commonality of the ultrasound signs of chronic cholecystitis, its holistic echographic display is not uniform. There are 5 options for the echographic picture of chronic calculous cholecystitis: a functioning gallbladder with preserved contractile function. It is always visualized well, all the signs characteristic of chronic cholecystitis, including stones, are clearly revealed; a gallbladder completely filled with stones: its cavity and walls are not revealed, but an area of continuous “exposure” with a wide acoustic shadow is determined; scar-wrinkled gallbladder: its cavity and walls are also not visualized, but at the same time, unlike the second option, the image of the stones is unclear, since they are masked by “exposure” from the sharply thickened, compacted walls of the bladder and putty-like pathological contents; blockade of the gallbladder: an increase in the size of the gallbladder, an increase in its tone and, most importantly, loss of contractility. Evidence of bladder blockage is the normal state of the common bile duct; blockade of the entire biliary system: the fundamental difference of this option is the localization of the obstruction zone of the biliary system, due to which new specific signs appear: dilation of the extra- and intrahepatic bile ducts with the presence of stones in them. In general, chronic calculous cholecystitis manifests itself with a fairly characteristic echographic picture and is diagnosed with 95-99% confidence.
- Symptoms of acute cholecystitis on ultrasound:
- enlargement of the gallbladder
- thickening and separation of the wall
- blurred contours
- increased bladder tone
- inhibition of contractile function
- the appearance of pathological inclusions in the gallbladder bile
- sharp local pain sensitivity
Destructive forms of cholecystitis are characterized by: more significant thickening of the walls (up to 10 mm); the presence of echo-negative stripes throughout their image; pronounced blurred external and internal contours with detachment of part of the mucous membrane; the presence of multiple echogenic pathological inclusions in the gallbladder bile; local peritonitis in the form of a strip of fluid around the gallbladder. A frequent complication is the formation of paravesical infiltrates and abscesses. Infiltrates look like areas of uniformly reduced echogenicity with uneven, fuzzy contours. The echostructure of abscesses is unevenly reduced, and the contours become clearer over time. In the case of perforation of the gallbladder, the image of its wall is torn. Cholesterosis of the gallbladder has two forms: focal polyposis and diffuse reticular. Focal polyposis cholesterosis has the appearance of clearly defined echo-positive formations, protruding from the bladder cavity, intimately connected to its wall, not shifting when the patient’s body position changes and not giving an acoustic shadow. Diffuse reticular cholesterosis is determined by the presence of multiple small echo-positive inclusions in the wall of the bladder, detected when the operating mode of the device is reduced. Benign tumors are displayed as pathological formations of medium echogenicity, round in shape, usually no more than 2.5 cm in diameter, not giving an acoustic shadow and not moving. In contrast to focal polyposis cholesterosis, when the operating mode of the device is reduced, their image disappears. * Gallbladder cancer, depending on its shape, is displayed in two versions of the echographic picture: with a nodular form of the process, a pathological formation with uneven contours and a wide base is determined by heterogeneous echogenicity (in this place the bladder wall is poorly differentiated); with diffusely infiltrating cancer, the gallbladder is not differentiated, and in its zone a poorly contoured area of heterogeneous echostructure is revealed. Compression or invasion of the common bile duct causes dilatation of the intrahepatic bile ducts. Indirect signs of a malignant tumor are the presence of metastases, primarily to the liver, enlarged lymph nodes, and ascites. The bile ducts are examined simultaneously with the liver and gallbladder. Intrahepatic ducts are not normally visualized. When expanded, they have the appearance of tubular echo-negative formations, which should be differentiated from the hepatic and portal veins. Unlike the bile ducts, the hepatic veins are fan-shaped at an angle to the anterior surface of the liver and join together at the entrance to the inferior vena cava, and the branches of the portal vein run almost parallel to the abdominal wall and have thick walls. In addition, during deep inspiration, the veins dilate, but the bile ducts do not. The common bile duct normally has a diameter of up to 6 mm and is located in front of the portal vein. Due to the fact that its various sections often do not lie in the same plane, it is difficult to obtain a one-time image of the duct along its entire length. Its retroduodenal section is often shielded by the gas contained in the duodenum. Cysts and diverticula of the common bile duct are defined as echo-negative pathological formations of round and oval shape, having a direct connection with the duct. They often contain stones. Congenital ectasia of the intrahepatic ducts (Caroly's disease) is reflected by the uneven expansion of their lumen. Primary sclerosing cholangitis is characterized by diffuse narrowing of both extra- and intrahepatic bile ducts with the development of cholestasis and cirrhosis. Echographically, there is a significant increase in the echogenicity of the intrahepatic periportal zones, narrowing of the ducts with thickening and compaction of their walls. Tumors of the intrahepatic ducts are echographically indistinguishable from tumors of the liver parenchyma. When the extrahepatic ducts are affected, a poorly demarcated formation with a heterogeneous structure of lower density is revealed compared to the surrounding tissues. Cholestasis often develops. Bile duct stones in an echographic image are not fundamentally different from gall bladder stones, that is, they appear as an echo-positive signal with an acoustic shadow behind it. In addition to these direct signs, choledocholithiasis is also manifested by a number of indirect symptoms: dilation of the intrahepatic ducts, dilation of the common bile duct proximal to the stone and narrowing of its distal part, deformation and breakage of the image of the duct. Stones in the retroduodenal part of the duct are not detected, since they are shielded by gas in the duodenum. In such cases, one should try to move the stone to a clearly visible part of the common bile duct or to achieve passage of gas into the small intestine, which can be achieved by changing the position of the patient’s body, in particular, if the study is carried out on a trochoscope of an X-ray machine with the head end down (Trendelenburg position) , the stone will move to the proximal part of the common hepatic duct, which is usually clearly visualized. Difficulties in diagnosing choledocholithiasis are sometimes due to the fact that bile duct stones have not yet formed and are lumps of so-called putty, which does not give one of the main symptoms - an acoustic shadow. Biliary tract stones must be differentiated from liver calcifications of various origins and air bubbles entering the ducts after biliodigestive anastomoses and papillosphincterotomy, as well as in the presence of internal biliodigestive fistulas.
general characteristics
Bile is an auxiliary enzyme, it is secreted in the human liver to improve digestion. In humans, the bile ducts are a system of channels through which bile is discharged into the intestine. The bile ducts of the liver open into the duodenum, which leads to the stomach. The system of pathways and bile ducts vaguely resembles the image of a tree: the crown of the tree is the small channels located in the liver, the trunk is the common hepatic duct connecting the duodenum with the liver. The movement of bile is carried out using pressure, it is created by the liver.
Jaundice
Jaundice is a syndrome caused by an increase in the concentration of direct or indirect bilirubin in the blood, which is accompanied by a yellow coloration of the mucous membranes and skin. There are three types:
- hemolytic (suprahepatic);
- parenchymal (hepatic);
- mechanical (subhepatic).
The cause of the development of suprahepatic jaundice is the active breakdown of red blood cells against the background of the occurrence of hereditary disorders, Rh - conflict between mother and newborn child, the development of malaria, systemic inflammatory response syndrome. The clinical picture includes an increase in the size of the spleen and liver, discoloration of the skin in a lemon-yellow color, and general malaise. Urine and feces acquire a darker, richer hue. With malaria, symptoms are supplemented by fever, excessive sweating, and chills.
Parenchymal jaundice indicates structural changes in the gland. It is a consequence of diseases such as hepatitis, cirrhosis, leptospirosis, cancer, hepatosis, infectious mononucleosis. The patient acquires an orange-yellow color of the mucous membranes and skin, the clinic includes pain in the right hypochondrium, enlarged spleen, the appearance of spider veins on the body, ascites, dilation of the veins of the esophagus and anterior abdominal wall.
Obstructive jaundice is caused by blockage of the ducts with stones or neoplasms. The cause of development may be metabolic disorders in the body, congestion in the gallbladder. There are no symptoms without inflammation. With cholecystitis due to cholelithiasis, the patient complains of acute pain in the right hypochondrium, nausea, and possible vomiting of bile. The clinic is complemented by a rise in temperature and a deterioration in the general condition of the body. The color of the skin is greenish-yellow.
Any of the described conditions requires emergency hospitalization and qualified medical care.
Anomalies of the bile
An anomaly in the development of the gallbladder ducts is diagnosed in almost 20% of people. Much less common is the complete absence of channels intended for the removal of bile. Congenital defects entail disruption of the biliary system and digestive processes. Most congenital defects do not pose a serious threat and can be treated; severe forms of pathologies are extremely rare.
Duct anomalies include the following pathologies:
- the appearance of diverticula on the walls of the canals;
- cystic lesions of the ducts;
- the presence of kinks and partitions in the channels;
- hypoplasia and atresia of the biliary tract.
Anomalies of the bubble itself, according to their characteristics, are conventionally divided into groups depending on:
- localization of the bile;
- changes in organ structure;
- deviations in shape;
- quantities.
An organ can be formed, but have a different location from the normal one and be located:
- in the right place, but across;
- inside the liver;
- under the left hepatic lobe;
- in the left hypochondrium.
The pathology is accompanied by disturbances in bladder contractions. The organ is more susceptible to inflammatory processes and the formation of stones.
A “wandering” bubble can occupy various positions:
- inside the abdominal region, but almost not in contact with the liver and covered by abdominal tissues;
- completely separated from the liver and communicating with it through a long mesentery;
- with a complete lack of fixation, which increases the likelihood of kinks and torsion (lack of surgical intervention leads to the death of the patient).
It is extremely rare for doctors to diagnose a newborn with a congenital absence of the gallbladder. Gallbladder agenesis can take several forms:
- Complete absence of the organ and extrahepatic bile ducts.
- Aplasia, in which, due to underdevelopment of the organ, there is only a small process that is not capable of functioning and full-fledged ducts.
- Bladder hypoplasia. The diagnosis indicates that the organ is present and capable of functioning, but some of its tissues or areas are not fully formed in the child in the prenatal period.
Functional excesses go away on their own, but true ones require medical intervention
Agenesis in almost half of cases leads to the formation of stones and dilation of the large bile duct.
An abnormal, non-pear-shaped shape of the gallbladder appears due to constrictions, kinks in the neck or body of the organ. If the bubble, which should be pear-shaped, resembles a snail, then there has been a bend that has disrupted the longitudinal axis. The gallbladder collapses towards the duodenum, and adhesions form at the point of contact. Functional excesses go away on their own, but true ones require medical intervention.
If the pear-shaped shape changes due to constrictions, then the vesical body narrows in places or completely. With such deviations, stagnation of bile occurs, causing the appearance of stones and accompanied by severe pain.
In addition to these shapes, the pouch can resemble a Latin S, a ball or a boomerang.
The biliary bile weakens the organ and leads to dropsy, stones and tissue inflammation. The gallbladder may be:
- multi-chamber, in which the bottom of the organ is partially or completely separated from its body;
- bilobed, when two separate lobules are attached to one bladder neck;
- ductular, two bladders with their ducts function simultaneously;
- triplicative, three organs united by a serous membrane.
Cholangitis
Cholangitis is inflammation of the bile ducts. It occurs most often in elderly or middle-aged people, that is, at fifty to sixty years old. Depending on the structural changes, tissues are divided into several types:
- catarrhal;
- purulent;
- necrotic;
- fibrinous or diphtheritic.
The cause of the pathology is usually a bacterial infection, namely staphylococci, streptococci, Escherichia coli or Pseudomonas aeruginosa, mycobacteria. Sometimes an autoimmune process can act as an etiological factor, when the body produces antibodies against its own healthy cells. In this case, systemic lupus erythematosus, vasculitis, and rheumatoid arthritis may be concomitant diseases of cholangitis.
At first, the patient may experience the so-called Charcot triad: fever, pain and jaundice of the skin. The inflammation is acute, the patient complains of general weakness, malaise, headaches, loss of appetite, that is, typical signs of intoxication of the body. In addition, itching may occur, intensifying at night, resulting in scratching in the form of ordinary scratches or shallow wounds covered with a crust.
In severe cases, the Reynolds pentad becomes a distinctive feature: fever, pain in the right hypochondrium, jaundice, impaired consciousness and toxic shock, which is indicated by a decrease in blood pressure.
Complications of cholangitis can include cirrhosis, abscess, acute or chronic functional failure, systemic inflammatory response syndrome (sepsis).
Organ functions
The liver is a kind of chemical laboratory responsible for many biochemical processes in the body. Its main functions are:
- Synthesis. In the cells of the organ, the synthesis and accumulation of bile occurs, which is necessary for the breakdown of fats and the activation of certain enzymes in the cavity of the duodenum. In addition, some hormones, cholesterol, glycogen, phospholipids and other compounds are formed here.
- Neutralization. The organ takes an active part in cleansing the body of toxic metabolites, excess sex hormones, some vitamins, microelements, medicines and poisons received from the outside.
- Accumulation and production. In case of insufficient nutrition or diseases that exhaust the body, the gland releases complex carbohydrates into the bloodstream for the purpose of further breakdown and formation of energy, iron, copper, cobalt, ascorbic acid, calcitonin and other biologically active substances.
- Hematopoiesis. During the growth, development of the fetus and the still unformed red bone marrow, the liver performs a hematopoietic function, that is, it replenishes the blood with red blood cells, platelets, and leukocytes.
- Thermoregulation. Hepatocytes play some role in chemical thermoregulation. They control the balance between anabolism and catabolism, regulate the amount of energy received and expended in the process of human life.
The body needs the gallbladder only to accumulate secretions. For this reason, the operation for resection or removal of this organ does not have any special complications and does not lead to disability of the patient.
Symptoms and manifestations
Pathology associated with an enlarged gallbladder may not bother a person for a long time. The main symptom is pain of a different nature. They can be aching, periodic, mild or sharp, unbearable, characteristic of an acute inflammatory process.
Their location is the right hypochondrium. The patient may complain of nagging pain radiating to the right shoulder blade and arm. Chronic processes are accompanied by discomfort after eating, especially if the menu included harmful foods: fatty, salty, smoked, alcohol, carbonated water, snacks and other foods high in preservatives and carcinogens.
The following symptoms may accompany an enlarged gallbladder:
- bitter taste in the mouth not associated with food intake;
- yellow color of the skin, whites of the eyes;
- bowel dysfunction - both constipation and diarrhea;
- bloating, flatulence, belching;
- temperature increase;
- causeless nausea and vomiting that does not lead to relief;
- skin irritation;
- physical activity aggravates the condition and increases pain;
- feces become light, whitish in color, urine darkens.
The presence of several signs is a reason to consult a therapist and gastroenterologist.
Classification of pathologies
According to the International Classification of Diseases, Tenth Revision (ICD 10), liver pathologies are encoded under the numbers K70-K77, gallbladder and biliary tract - K80-K83. They are divided into the following sections:
| Liver | Gallbladder |
| Alcohol disease (K70) | Cholelithiasis (K80) |
| Toxic damage (K71) | Cholecystitis (K81) |
| Functional impairment (K72) | Other pathologies (cholangitis, fistula and others) (K82, K83) |
| Connective tissue changes (cirrhosis and fibrosis) (K74) | Pathologies not classified elsewhere (K 87) |
| Hepatitis (K73) | |
| Other types of inflammatory process (K75) | |
| Other pathologies (heart attack, peliosis, etc.) (K76) |
Some diseases are worth talking about in more detail, since their prevalence has increased over several decades, and the age of patients suffering from them has decreased by ten to twenty years.
Disease research methods
Due to the fact that almost all diseases of the biliary system have the same symptoms, diagnosing diseases is a labor-intensive process. Every competent specialist will advise the patient to take a blood, urine and stool test. You also need to do an ultrasound of the liver, gallbladder and canals. You should not refuse a liver biopsy. It makes sense to take an x-ray of the abdominal cavity. This will help determine what deformations the disease led to. Depending on the situation, the doctor prescribes a computed tomography scan of the abdominal organs. Diagnostics takes a lot of effort and money, but it is necessary in order to make a diagnosis. Only after studying the results of all tests, a qualified specialist is able to make a correct, adequate diagnosis. This determines what therapy to prescribe.
Cleaning the gallbladder using traditional methods
Lemon juice and olive oil are used to cleanse the gallbladder at home.
Traditional medicine offers a huge number of different recipes for cleaning the gallbladder and ducts. Narrowing, accumulation of stones, compaction - all this can be treated if you clean the ducts at home. Cleansing with lemon juice and olive oil is the most effective remedy. Recipe:
- In the morning, have a hearty breakfast (vegetarian food).
- Until 16:00, drink only apple-beetroot juice (1:5).
- From 16:00 to 20:00 do not drink or eat anything.
- At 20:00, take a glass of fresh lemon juice and a glass of vegetable oil (preferably olive).
- Take turns drinking from two glasses with short breaks. Both glasses should be empty within 40-60 minutes.
- After this, apply a warm heating pad to the right hypochondrium and go to sleep on your right side.
- The next morning you need to do a cleansing enema (chamomile). Don't worry if you end up with a strange mass with an unnatural color and smell.
Do not self-medicate; proper treatment should only be prescribed by a specialized doctor. The use of folk remedies can sometimes only aggravate the situation or lead to relapse. You should listen to your doctor’s advice, strictly follow the prescribed diet and lead a healthy and active lifestyle. This is enough to get your digestion in order.
Pathological changes
There are a number of pathological changes in the common bile duct. One of them is dilatation of the common bile duct. Dilatation from the Latin dilatation - expansion of the lumen of the duct. Occurs due to mechanical narrowing of the lower part of the organ.
- Congenital and acquired malformations (hypoplasia, cysts).
- Benign diseases of the gallbladder (cholelithiasis, bile duct strictures).
- Inflammatory processes (cholecystitis, cholangitis, pancreatitis).
A number of natural questions arise. How does the common bile duct change? What might this entail? In such cases, a number of clinical studies are prescribed to establish the cause of changes in the lumen and select a method of further treatment.
Anatomy
The gallbladder is a small sac consisting of epithelium, smooth muscle cells and connective tissue. The bile that is not spent during the digestion process accumulates in this organ, and then, as needed, is released into the cavity of the duodenum.
The liver is the largest gland, its weight reaches one and a half kilograms. Located in the area of the right hypochondrium. It consists of two lobes separated from each other by a large connective tissue ligament. It has several surfaces: diaphragmatic (smooth, flat), visceral (lumpy). It is from the latter side that the portal of the organ is visible, consisting of an artery, portal vein, common hepatic duct, and the gallbladder, which lies in the fossa of the same name.
The gland is covered on top with a fibrous membrane, to which all nerve endings go. With active inflammation and an increase in the size of the organ, this capsule stretches, and the patient feels a sharp, aching or nagging pain.
Histologically, liver tissue consists of cells called hepatocytes. They are combined into peculiar groups or plates - lobules. Through a microscope you can see a peculiar pattern: in the center there is a central vein, from it hepatocytes are located in the form of strands or beams, and blood and bile capillaries pass between them.
Small vessels responsible for the flow of secretions (bile) unite along their course and form larger intrahepatic ducts: right and left. Next, the common hepatic duct is formed. Connecting with the cystic duct, the common duct exits into the duodenum.
Knowledge of anatomy when diagnosing and treating pathologies of the liver and gallbladder is necessary, since all operations performed are based on this information. Any mistake during surgery can cost the patient's life.
Parasitic infestations
As the popularity of an omnivorous raw food diet grows, the incidence of pathologies caused by parasites increases: round or flatworms, protozoa. The liver and bile ducts are a favorite place for organisms such as flukes, roundworms, flukes, and amoebas.
Worm eggs and protozoan cysts enter the gastrointestinal tract through the fecal-oral route. Most of them are found in water, on blades of grass near the lake, and in poorly cooked meat and fish. In the development cycle of parasites, humans are most often the definitive host.
Disorders of the digestive system during the active growth and development of worms are caused by the release of toxic products of their vital activity and the consumption of nutrient reserves of the macroorganism, that is, humans.
Symptoms are initially mild, perhaps a feeling of weakness, malaise, but nothing more. Over time, a clinical picture develops, including itching of the skin, upset stool, decreased appetite, weight loss, and fever.
Sometimes deworming medications do not provide adequate treatment and surgery is required.
Symptoms
Symptoms of bile duct blockage usually appear gradually; acute onset is quite rare. Typically, the development of clinical biliary obstruction is preceded by a biliary tract infection. The patient complains of fever, weight loss, and cramping pain in the right hypochondrium. The skin becomes jaundiced, and the patient is bothered by itching of the skin. The lack of bile acids in the intestines leads to discoloration of stool, and increased excretion of direct bilirubin by the kidneys leads to the appearance of dark-colored urine. With partial blockage, alternation of discolored portions of feces with colored ones is possible.