Advertisement
Ringworm in children is a skin disease caused by contact with a carrier of the infection, in which the main element of the rash is small itchy nodules and skin rashes.
Every now and then all kinds of rashes appear on the child’s skin. If ordinary prickly heat does not require special therapy and does not pose a danger to others, then lichen is a disease that requires immediate treatment under medical supervision.
Children often get ringworm : especially if left unattended, they strive to cuddle a street cat or dog. And often parents, having discovered a suspicious rough spot on the child’s skin, begin to experiment, trying to get rid of deprivation on their own.
Advertisement
This is a big mistake, because lichen has several varieties, each of which has a specific treatment. Self-medication can lead to very unpleasant and even dangerous consequences.
Symptoms of lichen in children.
If a rash appears on a child’s skin, consultation with a dermatologist or infectious disease specialist is indicated. Without a doctor's examination and scraping, it is impossible to make a correct diagnosis. The analysis will determine which pathogen has affected the skin. The choice of treatment depends on this.
Note: Spots affected by fungus glow in ultraviolet light.
Round or oval spots on the body that are flaky, itchy, or have changed color are symptoms of shingles in children.
Skin disease can be fungal or viral, depending on its causative agent.
Ringworm in an infant begins with a small spot and develops with lightning speed. Before the age of one year, the immune system cannot cope with the infection, the disease becomes chronic, a bacterial infection occurs, and purulent, weeping wounds appear.
Note: If there is any change in the baby's skin, consult a doctor immediately.
Ringworm in a child - which doctor to see, necessary tests
If symptoms of lichen appear on the head, face, or other parts of the body, you should visit a dermatologist, infectious disease specialist, or mycologist.
Basic diagnostic methods:
- general blood test - the presence of an inflammatory process is indicated by an increased level of ESR, normally the indicators should be in the range of 10–15 mm/h;
- PCR diagnostics is one of the most informative research methods; it allows you to determine the presence of infection with almost 100% accuracy, even if there are no obvious signs of the disease;
- luminescent diagnostics - in all forms of lichen, the affected areas are painted in different shades, which makes it possible to determine the type of pathogen;
- iodine test - used to diagnose pityriasis versicolor; when a 2% solution is applied to the skin, the spots become brown;
- bacterial culture of skin scrapings, study of biological material under a light microscope;
- biopsy of the affected area of skin - the procedure can be a little unpleasant and painful for the child.
All tests must be taken in the morning on an empty stomach.
Causes of lichen in children.
Poor nutrition with a lack of vitamins and minerals, hypothermia, stress or overwork reduce the child’s immunity. These factors increase the likelihood of contracting infections, viruses and fungi.
Fungal species live for a long time outside of humans in household items (toys, clothes), so failure to comply with personal hygiene rules (not washing hands, using other people’s things) leads to infection.
Children with weakened immune systems often become infected with lichen from a cat, a stray dog, or in contact with peers.
Subtleties of diagnosis
When the first signs of microsporia appear in a child, parents need to show the baby to a doctor to make sure the presence or absence of the disease. Despite the fact that the pathology is accompanied by specific symptoms, after examination the specialist may prescribe a number of additional studies to clarify the diagnosis.
Help to confirm a preliminary diagnosis:
- Microscopy is a method used to confirm the mycotic nature of the pathology. The material for research is scales taken from the affected areas or hair.
- Luminescent examination - takes place in a darkened room using a Wood's lamp. Before the procedure, the affected areas are completely cleared of crusts.
- Cultural examination is a method used when the results of luminescent and microscopic examinations are positive in order to identify the type of pathogen. To obtain the result, hairs or scales are placed in a nutrient medium, and after 2 days the growth of colonies is observed.
Why is lichen dangerous for children?
With proper timely treatment, the skin disease is not dangerous. When neglected, it goes into a chronic stage and affects large areas of the skin, causing inflammation, itching, and suppuration.
The ringworm type affects the hair follicles. If treatment for deprivation in a child is not started in time, hair stops growing in the affected area.
Failure to comply with personal hygiene rules leads to the addition of a bacterial infection, followed by the prescription of antibiotics and anti-inflammatory drugs.
The shingles type with damage to the facial nerve poses a serious danger. Requires urgent medical attention and hospitalization.
Note: To prevent complications, every parent should know what lichen looks like in children.
How to treat lichen, effective medicines
Treatment of any form of lichen involves the combined use of products for external and internal use, since getting rid of fungal infections is not so easy.
How to treat ringworm
Since ringworm often affects the scalp, you need to purchase a shampoo with an antifungal effect - Mycozoral, Nizoral, you can use tar soap.
Main groups of drugs:
- ointments – Clotrimazole, Terbinafine, sulfur-tar, sulfur-salicylic ointment;
- Fukortsin, iodine can be used to treat affected areas;
- tablets are prescribed for advanced forms of the disease, large areas of damage - Griseofulvin.
Vitamins and agents to improve blood microcirculation and strengthen vascular walls are prescribed as auxiliary therapy. The same treatment regimen is used to eliminate the manifestations of tinea versicolor.
How to treat pityriasis rosea in a child
This form of the disease often goes away on its own, sometimes lasting for years until the true cause of its occurrence is determined. The therapy is radically different from the treatment of ringworm.
For pityriasis rosea, you cannot use antifungal agents or antiseptics with a drying effect to lubricate the rash.
What can be used? Ringworm on the hand, face, and other parts of the body can be lubricated with peach, rose hip, sea buckthorn oil, Chlorophyllipt solution, Romazulan; modern antihistamines - Zodak, Fenistil - will help eliminate itching. If necessary, the doctor can prescribe hormonal medications, but you cannot take them yourself.
Treatment of herpes zoster
The basis of therapy is antiviral drugs - Acyclovir, Famvir, Valtrex; treatment will be effective if you start taking the drugs no later than 72 hours after the first signs of the disease appear.
Additionally, painkillers are prescribed - Ibuprofen, Panadol.
You cannot use ointments and gels with corticosteroids, as they provoke an exacerbation of the disease.
For any form of lichen, it is necessary to take immunomodulators - Polyoxidonium, Cycloferon, Immunal. If the disease is severe and there is a risk of bacterial infection, the doctor may prescribe broad-spectrum antibiotics - Erythromycin, Metacycline.
How long to treat lichen? The duration of the course is determined by the attending physician; if you start therapy when the first signs of pathology appear, then unpleasant symptoms can be eliminated in 7–10 days; in advanced forms, treatment can last for several months; fungal infections are often recurrent.
What does lichen look like in children?
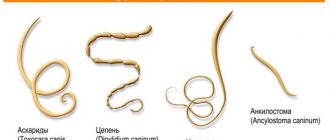
Ringworm in children.
More than 80% of sick children are diagnosed with this type. Caused by fungi. Infection occurs more often from sick animals or human carriers of the microorganism. In the affected area, hair does not grow or is broken off from the root, the skin is covered with scales.
Pityriasis rosea in children.
Poor immunity and allergic diseases are prerequisites for the development of the disease. Not contagious, not transmitted from person to person. The rashes are round, irregular in shape, pink, with clear boundaries, which peel and cause itching. Outbreaks occur in autumn and spring.
Herpes zoster in children.
Causes the herpes virus, which a person suffered from in the form of chickenpox. It settles in the nervous system in a dormant state; with decreased immunity or severe stress, it manifests itself in the form of a massive accumulation of bubbles located in a continuous stripe. Accompanied by severe pain at the site of accumulation of bubbles, burning, itching.
Pityriasis versicolor in children.
Caused by fungi, it affects the entire body. The formation of uneven multi-colored spots with scales inside is characteristic. Causes severe itching and pain in the affected area.
Lichen planus in children.
Difficult to diagnose type, similar to psoriasis. Rarely occurs in children. Occurs when overwork, severe or chronic stress. Locations on the arms and abdomen, rarely on the mucous membrane of the mouth and genitals. Diagnosed by typical bright red spots with scales inside.
Lichen alba in children.
This type is isolated separately and has not been studied. Diagnosed in boys from 3 to 18 years old. Lichen alba in a child is not contagious and appears as white spots in the sunny season of the year. It goes away without the use of medications. The causes have not been established.
Symptoms
There are several stages in the manifestation of symptoms of the disease:
- the initial stage is characterized by the appearance of pink spots. The skin of an infant or older child begins to peel off;
- further, in the absence of treatment, foci of pathogenic activity of the fungus appear on the arms and legs, and abdomen. Signs of lichen are rarely observed on the scalp, face or nails;
- There is an increase in temperature to 39 degrees with subsequent growth of lymph nodes.
How is lichen treated in children?
Note: The therapy complex depends on the type and is prescribed only by a doctor.
Lichen versicolor in children is treated comprehensively:
- Antifungal drugs for topical use. The use of medications containing substances is indicated: clotrimazole (Candide), itraconazole (Zalain), ketoconazole (Sebozol, Mycozoral, Nizoral), terbinafine (Lamisil, Binafin, Exifin, Termicon, Fungoterbin), naftifine (Exoderil, Mycoderil).
- Immunomodulators: Viferon, Isopronisin, Polyoxidonium, Imunorix.
- Multivitamin preparations.
- Regular change of underwear and bed linen followed by boiling and ironing.
- Hormonal ointments (Akriderm, Momat, Advantan, Hydrocortisone, Belosalik) are used for severe disease. Prescribed by your attending physician.
- Antihistamines are indicated for severe itching.
- Isolating the child.
- Systemic antimycotics containing itraconazole, fluconazole, and ketoconazole are used in rare severe cases of the disease.
- The cutting option settles in the hair and requires its removal from the affected area. The treatment option coincides with the pityriasis variety due to a fungal pathogen. On the scalp, the use of antifungal shampoos is indicated: Nizoral, Mycozoral, Sebozol.
Note: Upon completion of treatment for fungal lichen, repeat tests are required.
Shingles requires therapy under medical supervision.
Treatment:
- Antiviral drugs containing active substances: acyclovir, famciclovir, valacyclovir, isoprinosine, tilorone. Duration of treatment is from 7 days.
- Painkillers approved for use by age.
- Caring for rashes, excluding their contact with clothing and aggressive solutions.
The pink type is infectious, but not contagious. It occurs when immunity is reduced due to the body’s allergic reaction to bacteria and viruses that have entered it, and therefore requires taking medications from different groups.
How to cure lichen in a child in 2019:
- Antihistamines to relieve acute reactions of the body.
- Antibiotics to kill bacteria.
- Immunomodulators and antivirals.
- Preparations for local use: antiseptics, anti-inflammatory.
The red variety is diagnosed more often in adults.
Therapy includes:
- steroid ointments based on hydrocortisone, betamethasone, mometasone;
- multivitamins;
- sedatives;
- antihistamines.
Manifestations of the white appearance are eliminated by reducing the time spent in the sun and using products with a high SPF protection factor. The skin is smeared with moisturizing and restorative creams. Taking vitamins, a healthy lifestyle and spa treatment will reduce the likelihood of white spots appearing.
For any variety, a hypoallergenic diet and strengthening of the immune system are indicated.
Note: In case of fungal infection, general cleaning and disinfection of the living space, underwear and bed linen, and towels are recommended.
In case of bacterial complications, the use of combined hormonal agents containing antifungal, antibacterial and anti-inflammatory components is indicated.
Note: The doctor will prescribe what to apply for lichen in a child if bacteria have appeared after examining the affected area.
The use of ointments with antimicrobial action relieves inflammation and prevents the development of suppuration.
Antibiotics for external use:
- Tetracycline;
- Erythromycin;
- Metronidazole (Metrogyl);
- Baneocin powder, ointment;
- Argosulfan;
- Streptocide powder, ointment;
- Zinc paste;
- Gentamicin;
- Betadine solution, ointment
- Triderm, Akriderm GK, Rederm, Belosalik, Betaderm, Diprosalik are combined preparations for external use with antipruritic, anti-inflammatory, antiallergic, antifungal, and antibacterial effects.
Contraindications:
- age up to 2 years;
- herpes;
- increased sensitivity;
- chickenpox;
- cutaneous tuberculosis.
Children from two years of age are prescribed according to strict indications. Treatment is carried out under medical supervision, as severe side effects may develop.
These include: growth retardation, increased intracranial pressure, headaches, delayed weight gain. It is forbidden to use on the mucous membranes of the eyes, mouth and genitals.
In case of severe and extensive damage to the skin with severe inflammation and swelling, on the recommendation of a doctor, highly active corticosteroids are used - Dermovate, Cloveit.
Causative agent of microsporia
The causative agent of ringworm is anthropophilic microorganisms - fungi from the genus Microsporum , localized on the skin.
Penetrating into the layers of the epidermis, the fungal infection forms colonies in the hair follicles, and also affects areas of the skin that are devoid of vegetation, so lesions can usually be seen on the feet or palms.
Important!
Among the fungi of the genus Microsporum there are about 20 species that can lead to the development of a pathological process on the scalp, skin and nails.
Folk remedies.
Note: Home methods will only be effective in conjunction with drug therapy.
Traditional methods of treating herpes zoster :
- compresses with a decoction of burdock leaves;
- fresh white cabbage leaves;
- aloe juice or leaves.
Home therapy for pityriasis versicolor :
- treatment of affected areas with rosehip oil;
- compresses or rubbing with alcohol tincture of calendula;
- decoction of St. John's wort, celandine.
For ringworm , lotions containing 50 grams of fir oil diluted with 50 grams of vodka will help.
The pink type does not require mandatory medical treatment with external agents. Symptoms are relieved by rubbing with chamomile decoction and ointments to relieve itching.
Red view makes it easier :
- warm compresses with sea buckthorn oil;
- celandine decoction.
To relieve white type :
- aloe leaves;
- decoction of birch leaves.
Types of ringworm.
In addition to the two main types of ringworm, the pathology is divided into subtypes, based on the clinical picture as a whole. In addition, the incubation period when the disease does not manifest itself is different for each subspecies.
With a superficial form, the disease is in “sleeping” mode for 5 to 7 days. Symptoms of the disease may be absent or mildly expressed in the form of a slight change in skin color in the affected area, peeling.
The latent period for purulent or infiltrative-suppurative lichen takes about 60 days, although the incubation period can take four weeks. During the suppurative stage, the affected areas of the epidermis are covered with lumpy plaques of a deep red color, inside which pus forms due to inflammatory processes. The stage is characterized by increased temperature, enlarged lymph nodes, general weakness, and in rare cases the child has a fever.
The disease lasts for the longest period in a chronic form, accompanied by either improvement or deterioration of the condition. This stage is more often observed in girls at puberty, as well as in mature women. It occurs as a result of a mild infection that has passed into this subtype due to disturbances in the functioning of the endocrine system, which affects the functioning of the genitourinary system and the ovaries in particular.
If a child catches the infection from a person, the incubation period takes from two to six weeks. In case of infection from animals on the street or at home, this period lasts 5-7 weeks.
Prevention of lichen in children.
Measures to prevent infection with skin diseases:
- Teach your child the rules of personal hygiene. Wash your hands regularly. Do not use other people’s things: clothes, hats, personal items (combs, towels).
- Strengthen immunity. Take vitamins, eat well, exercise.
- Do not contact with strangers or street animals, or persons with signs of skin diseases.
- Have your pets examined regularly by a veterinarian.
Prevention is the main defense
So, no matter what type of lichen your child gets, don’t hesitate! After all, each type has its own nuances, approach and treatment methods. But to avoid trouble:
- observe the rules of hygiene,
- stay less in crowded places with a risk of infection (hospitals, etc.),
- carefully and often examine the child’s skin,
- monitor your child’s contact with unfamiliar animals, and check your pets more often for the presence of lichen,
- disinfect personal hygiene items,
- strengthen your baby's immunity,
- since fungal spores can linger on the comb for a long time and constantly infect the baby.
Well, if you notice something wrong, rush to the doctors. The sooner treatment begins, the better the prognosis.
Diagnostics
Only a doctor can diagnose whether your child is sick. To determine the classification of lichen, various diagnostic methods are used.
Let's take a closer look at each variation of lichen:
- Ringworm is detected using a Wood's fluorescent lamp ; the flickering will be green - emerald in color. Be sure to take a scraping from the affected area for microscopic examination and for inoculating the material;
- Pythiasis is difficult to determine . Tests such as a general blood test, urine test and scraping from the maternal plaque are taken. Afterwards, a differentiated analysis is done to exclude other diseases, such as psoriasis, allergic reactions, eczema;
- Shingles is determined visually . But for children, in order to avoid consequences, it is necessary to consult two doctors, such as a neurologist and an ophthalmologist, and also take an enzyme-linked immunosorbent blood test;
- If pityriasis versicolor is suspected, the study is carried out using 3 methods: Iodine test or Balser test - to carry it out, the skin is lubricated with iodine. The affected skin absorbs iodine quickly, and as a result, the lichen spots stand out in a light color against the background of the skin;
- A skin scraping is taken, which reveals yeast under a microscope;
- Examine the skin under a Wood's fluorescent lamp. The color of the lesions is multi-colored: red-yellow, green-blue or brown;
- General blood analysis;
- Peeling of the stain with “stearic” shavings;
Forms of the disease
The form of the disease can be determined by its external manifestations. Different forms of the disease occur against the background of different pathogens that affect the skin.
Cutting shape
This pathology is more common in children under the age of twelve. The causative agent of ringworm is a certain category of fungi, which is transmitted through contact of a healthy person with an infected person. At the same time, the role of the infected person is not necessarily a person; quite often the disease is transmitted through domestic animals. In some cases, the disease can be transmitted through contact not with the patient himself, but through his personal items.
Fungi belonging to different families can act as pathogens. So, some fungal infections can cause microsporia, while others can cause trichophytosis. Usually, in order to make a diagnosis, the doctor only needs to conduct an external examination of the affected areas, but laboratory tests may be required for an accurate determination.
This form of the disease is most often localized on the head. A little less commonly, ringworm is observed on the face and neck. An advanced form of the pathology can cause the formation of spots in the area of the shoulders, limbs and groin. The development of the disease leads to the appearance of edema. Then, on the swollen places, small spots of regular shape, painted in red tones, appear. The spots have a clear border, and the surface of the damaged area itself is covered with small scales. Most often, the disease occurs in the following situations:
- problems with immunity;
- frequent stress;
- complication of other skin diseases;
- mechanical damage to the integrity of the skin;
- prolonged contact with liquid, which leads to softening of the skin.
Experts note the fact that the cause of the disease may be associated with the presence of problems such as psoriasis, dermatitis and eczema.
In order to confirm or refute the diagnosis, a bacteriological culture procedure is used. This method allows you to get a guaranteed result. The duration of the disease is about one month. But in situations where the infection occurred from an infected pet, the duration of the disease is reduced by an average of one week.
Pink uniform
Pityriasis rosea is a little-studied disease often referred to as Gibert's disease. Usually the causative agent is a virus, which is activated against the background of severe hypothermia and prolonged nervous stress.
This form of pathology most often manifests itself in the upper torso and bends of the limbs. As the disease progresses, oval or round spots with a pinkish color form on the patient’s body. Over time, such spots become covered with scales, merge into a single spot and spread throughout the body in the form of smaller rashes. The rash is accompanied by severe itching, which can be intensified after water procedures or prolonged exposure to sunlight.
The symptoms of the disease are very similar to colds. Children quite often complain of fatigue and frequent migraine attacks. The clinical picture is complemented by symptoms such as a sore throat and redness of the throat.
Shingles form
Treatment of shingles in children is quite difficult, since the disease is caused by the herpes virus. Most often, the symptoms of this pathology occur in children over ten years of age. The virus can be activated during prolonged overwork, constant nervous tension, severe hypothermia, colds and other factors leading to a decrease in the body's protective functions.
In most cases, the rash appears in areas where there is a collection of nerve endings. Quite often, the rash encircles the torso or limb. An advanced form of the disease can lead to the symptoms of lichen appearing on the organs of vision. This pathology is considered quite dangerous, as it can cause partial or complete loss of vision.
At the initial stages, the skin of the infected person becomes covered with red spots; later, rashes appear on the damaged areas, which have a certain similarity with the symptoms of chickenpox. The pathology occurs within two or three weeks. In the second week of the disease, a thin brown crust forms on the rash. The disease is accompanied by severe itching, since the herpes virus has a strong effect on nerve endings.
Each type of lichen has its own specific manifestations
Multi-colored uniform
When you hear about color, versicolor and pityriasis versicolor, you need to understand that these terms hide the same type of pathology. The cause of the disease lies in the entry of a yeast-type fungus into the body. This pathology most often manifests itself in children of high school age. Experts include oily skin, the use of low-quality cosmetics, prolonged exposure to ultraviolet rays and hormonal problems as risk factors.
With tinea versicolor, spots form in the upper body and on the arms. Such spots can be painted in different shades and have different shapes. Small areas of the rash located close to each other can merge into one large uneven spot. In winter, such spots become darker, and in hot months they may become pale. Manifestations of this kind give the skin an unaesthetic appearance, since the affected areas are covered with large scales.
Dermatologists say that quite often the cause of the disease is a failure of the immune system and disruption of the local microflora. In addition, they note the fact that this form of the disease is contagious.
Red flat shape
Signs of lichen in children are pronounced, since the spread of the disease begins from the mucous membrane and nail plates. This disease is extremely rarely observed in preschool children. Despite the fact that the causative agent of the pathology is unknown, doctors trace a certain pattern in the formation of lichen and metabolic disorders. Quite often, symptoms of the disease appear against the background of allergic reactions, viral diseases, diseases of the gastrointestinal tract and diabetes.
Symptoms are most often found in the mouth or genital area. The formations themselves are similar to small nodules, colored pink, gray or purple. Dermatologists note that the rash may take the form of small rings, ulcers, or be similar to warts.
It is quite problematic to cure lichen in a child of this form, since therapy should be aimed not only at eliminating symptoms, but also at preventing the functioning of all of the above organs.
Additional recommendations.
The use of medications and folk remedies will not give the desired result if a number of conditions are not met. The doctor will give you the necessary recommendations. Each parent of a sick child adheres to the following instructions:
- Stick to a diet consisting of plant-based foods. Dairy products are also important. Spicy, salty, sweet are excluded. Products that can cause allergic reactions are excluded from the diet;
- Bathing a child in the bathtub is not recommended. The exception is medical procedures, as they are prescribed by a doctor;
- Walks are postponed to the evening, as heat and sun rays will worsen your well-being and also lead to an increase in the affected areas;
- During the incubation period, protect the baby from contact with other people and animals;
- Preference should be given to clothing made from natural fabrics (linen, cotton). They allow air to pass through, saturating even covered areas of the skin with oxygen;
- When taking a shower, cover the affected areas. And after taking a bath, it is forbidden to wipe the body, therefore you can only get it wet;
- Prepare a comb, soap, and towel for the baby. The disease easily spreads to healthy skin and is transmitted to other family members. Ringworm is a contagious disease;
- Change your baby's bedding daily. Linen is washed, boiled and ironed;
- Toys are treated with boiling water and chlorine-containing substances;
- Daily wet cleaning using disinfectants;
- Eliminate stress.
- The child needs rest, since the nervous system is already weakened from constant itching and pain.
How does infection occur?
Due to the fact that a child learns about the world around him through tactile contact, infection with trichophytosis most often occurs through contact with yard or stray animals.
In addition, you can become infected by:
- tactile contact with a sick person;
- using other people's household items (bed linen, towels, combs);
- upon contact with hay or grass, which may have fur from sick rodents or other animals.
Infection through the soil, which may contain spores of a pathogenic fungus, cannot be ruled out.
The incubation period (from the moment of infection until the first signs appear) when infected from a sick animal is not long - only up to 7 days. But the insidiousness of anthropophilic trichophyton is that after contact with a person suffering from ringworm, it can take from 14 days to 6-7 weeks, so the source of infection is not easy to identify.
Prevention
Prevention of ringworm on a national scale includes the following measures:
- systematic scheduled examinations in children's groups;
- catching stray animals;
- treatment of cats and dogs with lichen;
- mandatory disinfection of water in swimming pools;
- sterilization of instruments in hairdressing salons;
- educational work with the population.
Immunizations against microsporia and trichophytosis are not carried out. Family prevention is based on minimizing the risks of infection:
- limit children’s contact with stray animals, especially during the warm season;
- pets are taken for regular veterinary examinations;
- strengthen children's immunity with the help of a regimen, hardening, and fortification;
- instill in children proper hygiene skills, for example, mandatory hand washing after a walk;
- When bathing your baby, pay attention to any external changes on the skin;
- If there are any suspicious rashes or spots, leave your baby at home. Don't take him to daycare until you've consulted a dermatologist.
- If the child does get sick, he is isolated from healthy children until he recovers.
Home treatment, medications
If you decide to treat your child at home, this does not mean that you do not need to consult a doctor. The doctor will prescribe procedures that you can carry out at home, following simple rules. Various antifungal ointments and drying creams are used in treatment.
These can be drugs and ointments for lichen, such as:
- Sulfuric ointment;
- Micanozol;
- Terbinafine and others.
It is worth regularly changing things, bedding and thoroughly washing dishes and common items. The child should be protected from communication with other children and adults during the treatment period.
Treatment with folk remedies
Folk remedies are quite effective in the fight against various types of lichen.
A few products that have worked well:
- walnut leaves. Boil the leaves for 30-40 minutes and add to the bath;
- sagebrush. Boil the herb and let it brew. Take baths or apply lotions;
- use of propolis. Propolis is infused in alcohol for seven days, then the affected areas can be lubricated;
- castor oil and calendula tincture. Prepare a balm from equal parts of the ingredients and rub into the inflamed areas;
- Apple vinegar. Apply directly to wounds several times a day;
- Infuse garlic with vodka. Leave this remedy for a week, wipe the lesions on the skin;
- Birch tar. This is an excellent natural antiseptic. Relieves itching, fights fungus.
Important! There are quite a few options for traditional methods of treatment, but do not forget about the danger of allergies or other negative consequences. It is best to consult a doctor or dermatologist.
Causes
The fungi of this disease are anthropophilic and zooanthropophilic, so both animals and humans can be carriers. The most dangerous is contact with yard dogs and cats. Children do not understand that a barn cat can be contagious.
Children under 3 years of age are most at risk; they have very weak immunity. Boys are infected five times more often than girls. In the case of children who have a weakened immune system, the main causes of the disease are a lack of vitamin A and poor hygiene.
How to avoid getting shingles
Despite the high contagiousness of depriving the disease, it can be avoided with timely isolation of the patient, pets and strict adherence to personal hygiene and hygiene of household items (use of individual linen, towels, combs, regular cleaning of the room and washing of toys, frequent washing, including after rubbing antifungal ointments and creams, timely cutting of nails, etc.). Prevention of the disease can include strengthening the immune system, hardening, proper and nutritious nutrition.
What's the catch with trichophytosis?
Trichophytosis or, more commonly, ringworm is an infectious fungal infection of the skin and its appendages. The fungus Trichophyton tonsuran, which causes ringworm, is anthropophilic and zoophilic at the same time, so the disease is easily transmitted to humans from a sick animal. Trichophytosis received the name “ringworm” due to damage to the scalp, which is why damaged hair breaks off at the root and the ringworm spots look shorn.
Despite the fact that this disease has been known to mankind for a long time and is mentioned in the culture of Ancient Egypt, it was classified only in the 30s of the 19th century, and it took another hundred years to invent a cure.
Society has developed a stereotype that ringworm affects only disadvantaged and poor sections of the population, but in reality no one is immune from this infection. The disease is highly contagious.
Traditional treatment for lichen
To cure ringworm completely, you will have to consult a doctor and follow all his prescriptions and instructions without deviation.
How long ringworm is treated is an individual question, so after confirming the disease, the doctor prescribes individual treatment. The course of treatment is 1-3 months.
Most often, for superficial trichophytosis, the following treatment regimen is prescribed:
- Inside - Griseofulvin tablets. The daily dose is selected at the rate of 15-20 mg per 1 kg of weight, divided into 3 doses and after each dose it is recommended to drink 1 tsp. vegetable oil. The tablets are taken daily. In this case, epidermal cells are seeded weekly. After no fungus is found in the scraping, the tablets are started every other day (for 2 weeks). After this, the tablets are taken 1 time every 3 days. The reduction in the frequency of administration can last up to 1-2 months.
- Locally - ointments: sulfur-salicylic or sulfur-tar. The drug is rubbed into the skin in and around the affected areas before bedtime, and in the morning these areas are treated with iodine (3-5% alcohol solution).
- Another option for local skin treatment is treating the lesions with antifungal ointments, such as Clotrimazole, Mycoseptin, Terbinafine, Tolnaftate. The procedure is carried out twice a day for 30-60 days (only for children over 3 years old).
- In addition, the ointment can be prepared for you at the pharmacy according to your doctor's prescription. This could be Lassara Paste, consisting of salicylic acid, zinc oxide, petroleum jelly and starch, or Vidal's Milk, which contains salicylic and boric acids, camphor alcohol, sulfur and glycerin.
- If lichen lesions are present on the head, then the hair is shaved and the skin on it is treated with creams and ointments such as Clotrimazole, Mycoseptin, Terbinafine. Shampoos should also contain an antifungal component.
- To strengthen the immune system during treatment, the doctor recommends taking vitamins, especially A, B (the whole group), E and C. Parents can purchase them separately or as part of multivitamin complexes.
- The child’s nutrition during the treatment period should be correct, with a sufficient amount of vegetables, fruits, fish, meat, cereals and a reduction in the consumption of sweets.
- During the treatment period, it is necessary to exclude stress, synthetic underwear and clothing, taking baths (replaced with showers), hypothermia and overheating.
How to treat chronic lichen should also be determined only by a dermatologist, although its treatment is in many ways similar to the treatment of the superficial form: in the morning, treatment of the lesions of lichen with iodine (3-5% alcohol solution), in the evening - with salicylic, sulfur or tar ointment for 1-2 months , in addition, rubbing in antifungal ointments throughout the day.
Only a fully cured child can attend kindergarten, school and other institutions. Children whose laboratory tests confirmed the presence of a fungus, as well as those with visual manifestations of lichen lesions on the skin, should be isolated. After a three-time negative result, taken at intervals of 5-7 days, and the disappearance of external manifestations of lichen, the child is no longer contagious and can be considered healthy. However, even after the child recovers, he should be monitored by a dermatologist for at least another 3 months.
What to do if your child has shingles.
Only doctors can determine the pathology of the fungal genus. This is a doctor - dermatologist, infectious disease specialist and mycologist. Previously, a full examination was prescribed, including a blood test. With the development of high technologies, modern medicine is able to confirm or deny the presence of infection in a short time and with more accurate results.
To do this, scraping is done from the affected area (seeding). Additionally, other, special tests may be prescribed. Inspection of damaged areas using fluorescent diagnostics gives an accurate result (Wood's lamp). Skin exposed to fungal infections glows greenish, while healthy skin glows light blue.
Scraping means taking flakes of skin from the lesion. This analysis allows you to determine whether the skin is affected by the fungus or not. If the presence of a parasitic fungus is confirmed, the scraping is cultured to determine the type of pathogen.
Differential diagnosis is a method of excluding other skin diseases, for example, psoriasis, eczema, and so on, since they have symptoms similar to lichen.
Therapy of various forms of pathology
Knowing how to recognize lichen in a child, you can promptly identify the disease and begin a course of treatment. It is very important that treatment is prescribed by a specialist, since different forms of pathology require different approaches. In order to diagnose the form of the disease, scrapings from damaged surfaces are used, which are then sent for a bacteriological culture procedure.
The main symptoms of deprivation are the appearance of large red or pink spots on the surface of the skin
Cutting shape
When the first symptoms of ringworm appear, you should immediately visit a pediatric dermatologist . Based on the severity of the skin lesion, the doctor prescribes the use of antifungal drugs, which can be in the form of ointments or tablets.
In the treatment of this form of the disease, antifungal agents such as Ketoconazole, Clotrimazole and Lazimil have shown excellent results. Such ointments can only be used if the child is over two years old. In addition to these medications, dermatologists recommend using products containing sulfur, tar or salicylic acid. In some cases, it may be necessary to use quite strong medications that are sold only with a prescription.
To treat foci of inflammation, various solutions that have an antiseptic effect can be used. These medications include iodine and salicylic acid. For internal use, dermatologists recommend using Griseofulvin. The course of use of all of the above medications ranges from two weeks to one month.
To monitor your treatment, you may need to undergo weekly scraping procedures.
As an auxiliary therapy aimed at increasing immunity, experts recommend taking a course of vitamin therapy, using immunostimulating agents and those medications that help strengthen the vascular system.
Pink uniform
Pityriasis rosea usually does not require special therapy, as it disappears as quickly as it appears . But in some cases the disease can persist for many years. In such a situation, it is necessary to identify the cause of the pathology and direct therapy to eliminate it.
Before treating pink lichen in a child, it is necessary to obtain a recommendation from specialists. In this situation, there are a number of specific recommendations. Such recommendations include a ban on the use of any medications that have an antifungal effect. Such drugs can only worsen the disease and increase the number of rashes.
The use of antiseptics is also not recommended, as they have a drying effect, which causes irritation of the affected areas. In addition, you need to avoid taking long baths, hot showers, using a washcloth, rubbing, and prolonged exposure to the sun. Patients with lichen need to wear clothes made from natural fabrics and avoid prolonged physical activity.
Since the disease may be allergic in nature, it is recommended to use the latest generation of antihistamines. To treat the skin, you can use solutions prepared with medicinal herbs. In case of severe inflammatory processes, the use of external hormonal agents is prescribed.
Ringworm is a contagious and dangerous disease; if not treated in a timely manner, the child may develop other unpleasant diseases.
Girdle form
Quite often, the symptoms of the disease disappear on their own, but the appearance of a rash on a child’s skin in any case is a reason to visit an allergist and dermatologist . To treat severe forms of pathology, medications belonging to the group of antiviral and painkillers are used. Antibiotics are used only when ulcers form on the damaged areas and there is a risk of secondary infection.
Multi-colored uniform
When considering the question of how to treat ringworm in a child that has a colored form, it should be mentioned that all therapeutic methods are completely similar to the treatment of ringworm. Antiseptic solutions and antifungal external agents are used to treat damaged areas. If the disease is severe, a specialist can adjust the course of treatment and prescribe special tablets.
Treatment of the disease can be carried out both in a hospital setting and at home. If a fungus is responsible for the formation of the disease, antifungal medications are used. The most common form of lichen in children is ringworm. This type of disease requires special treatment, as complications and spread of the virus are likely.