Gangrene of the lower extremities is one of the diseases that is one of the most severe surgical pathologies. This process is characterized by necrosis, that is, tissue death. How long people live after the onset of gangrene directly depends on how quickly and efficiently the treatment is received. Of course, it is impossible to cope with gangrene of the limbs at home; using folk remedies will not give any result.
Although some reviews may talk about the effectiveness of such home, folk treatment, in reality, amputation of dead tissue is often the only solution. The longer no action is taken, the more gangrene will spread throughout the limb, and the more tissue will have to be removed. It is necessary to understand how and why gangrene develops in order to prevent such an outcome. If you notice signs and symptoms of any form of gangrene, immediately contact the clinic for timely examination and diagnosis of the disease.
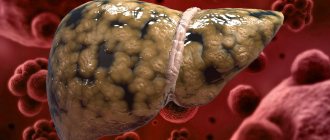
Spoiler with a slight shock photo of an example of the early stage of development of gangrene on the big toes.
This is what gangrene looks like in the initial stages of its development. [collapse]
Types of gangrene of the extremities
Besides the lower extremities, gangrene can occur almost anywhere. It affects the arms, torso, sometimes the face and even internal organs such as the intestines or lungs. Moreover, each zone is characterized by its own type of disease, and the course of the pathology and methods of its treatment depend on it.
Most often, the following types of diseases are distinguished:
- Dry gangrene of the lower extremities . It is one of the most favorable forms. This is due to the fact that the pathology does not spread to neighboring tissues, but remains where it originally appeared. The affected tissues look dense and slightly wrinkled.
Expand the spoiler to view a creepy photo of dry gangrene of the right leg.
Many doctors consider dry gangrene to be a great success for the patient, since, unlike other types, dry gangrene does not spread to other tissues [collapse]
The photo shows the gradual development of dry gangrene on the leg, in three stages, from the normal state.
- Wet gangrene of legs and arms . Here the rotting occurs much more pronounced. The affected tissues become soft, they swell and swell, and a rotten smell appears.
Photo example of wet gangrene of the skin of the thigh, arm and foot.
Expand the spoiler to view a creepy photo of wet gangrene of the left leg.
Rotting of soft tissues occurs much more pronounced than with dry gangrene, which, naturally, is accompanied by a corresponding odor. [collapse]
- Gas gangrene of the leg . In fact, this is another wet gangrene, but it is usually considered a separate disease. The International Classification of Diseases assigned it the ICD 10 A0 code. This type of pathology is diagnosed only if the tissues are infected with clostridia microbes. The gas form differs in the speed of distribution through healthy tissues, and the process is accompanied by severe intoxication.
The photo shows gas gangrene of the left lower limb.
Expand the spoiler to view a creepy photo of gas gangrene of the right leg.
At its core, gas gangrene is practically no different from wet gangrene, but it was identified as a separate type for the reason that its development is actively promoted by bacteria, which not only create severe intoxication of the body, but also spread infection at great speed throughout all tissues of the body. [collapse]
- Bedsore . It is not gangrene in the classical sense; it affects only the very top layers of tissue. This develops due to prolonged pressure on the same place. The appearance of bedsores is typical for bedridden patients who are unable to frequently change the position of their body.
Spoiler with a slight shock photo of bedsores on the heels of the feet.
Although a bedsore cannot be called gangrene in the classical sense and it does not belong to the previous three types, but due to necrosis of the upper tissues, it was added to this list. [collapse]
There is another type of disease called noma. It can also be classified as a type of wet gangrene, but there is one feature. This develops only in people with insufficiently strong immunity, most often in children. This is often due to the presence of a positive HIV test in the medical history. With such gangrene, areas of the face, as well as fatty tissue, are usually affected. As a rule, it is not possible to live with such a diagnosis for long.
Main complications and prevention
The most dangerous complications include extensive sepsis and intoxication of the body, both due to the products of rotting soft tissues and as a result of infection of the lesions. A common complication of gangrene is renal failure. A decrease in kidney function is indicated by an increase in the level of creatinine and urea in the patient’s blood. The main complication of dry gangrene is its progression, development and transformation into a wet and then anaerobic form. Preventive measures include eliminating factors that provoke the development of gangrene. Timely treatment of chronic diseases, avoidance of frostbite, injuries, burns, adherence to a healthy lifestyle and protective regime.
The prognosis for dry gangrene is usually favorable. With the development of the pathological process, not only the limb, but also all organs and systems suffer. It is impossible to predict in which organ necrotic changes will begin, so you should not lead to wet or gas gangrene. In late stages of the disease, the prognosis is unfavorable. In almost 60%, disability occurs, in almost 20% the patient dies after some time.
Why does dry gangrene develop?
The causes of gangrene are very diverse. Although numerous films suggest that this occurs after some serious injury, such as a gunshot wound, in reality the situation is completely different. In simple terms, it is all due to ischemia, that is, a condition characterized by a sharp weakening of blood circulation in a certain area, which leads to the development of a certain type of gangrene.
However, why this weakening occurs and how ischemic gangrene begins is another question. Each type of this pathology has a number of potential causes. First, it’s worth finding out why dry type of gangrene develops :
- Atherosclerosis of the lower extremities . Because of this disease, blood clots begin to form on the walls of the arteries, which can completely block the blood flow. Most often this occurs under the knee or in the thigh area, although atherosclerosis can also lead to gangrene of the arms due to damage to the brachial artery.
- Vibration disease . This disease is classified as an occupational one. It develops in those who constantly deal with exposure to vibration. For example, this applies to people who operate jackhammers, pavers, or concrete mixers. Such an effect means constant vasospasm. This disrupts the nutrition of nerves and tissues, which leads to pathological changes and the development of a dry form of gangrene.
- Raynaud's disease . This pathology is characterized by the destruction of nerves or blood vessels in the limbs, due to which they can no longer function normally.
- Polyneuropathy . The peculiarity of this pathology is a disruption in the supply of tissues and organs with nerves. Most often, problems with communication with the central nervous system manifest themselves in the lower extremities.
Another reason leading to the development of the dry form of gangrene is typhus. Sometimes it affects not the limbs, but the skin. In this case, the lesion spreads mainly along the sides of the body.
Often the problem lies in pathologies or diseases resulting from work or a sedentary lifestyle.
General characteristics of the disease
Gangrene of the leg, or in other words - necrosis, necrosis, is a pathological process in which the death of living tissue occurs. This process develops under the influence of external or internal factors, when the required amount of oxygen does not reach the tissues of the organ, and blood circulation is disrupted. This pathological process leads to extensive tissue damage, disruption of the functioning of the limb, which acquires a pale tint at the onset of the disease and a blue-brown or black color later in its development.
With the development of gangrene to the lower extremities, the transportation of blood, which normally supplies the tissues with the necessary amount of oxygen and useful substances, is disrupted. With insufficient blood supply to tissues, organ cells begin to die, which can cause the development of gangrene. People at risk for developing such a serious disease include people with diabetes, vascular atherosclerosis, pathologies of peripheral arteries, as well as those who abuse alcohol, smoke, or have suffered various types of limb injuries.
Reasons for the development of other forms of gangrene
One of the most pressing topics is gangrene of the lower extremities in diabetes mellitus. The so-called “diabetic foot” is a potential cause of the development of the wet form of the disease. It has its own code in ICD 10 - E10-E14. With this type, the entire foot or toes are affected. This is due to the fact that blood circulation occurs most intensely here, but immunity in this zone is weak.
A photo of gangrene of the lower extremities in diabetes mellitus, the treatment of which is very difficult, is always an extremely unpleasant sight. However, it is still possible to live with such a diagnosis if you start treatment in time. Diabetic gangrene of the lower extremities is quite common, but it is also necessary to consider other causes of the development of the wet form.
Spoiler. Photo gallery of examples of gangrene of the lower extremities with diabetes. Creepy photos.
[collapse]
What causes the disease to develop? The causes of gangrene are as follows:
- Deep burns or severe frostbite.
- Strangulated hernias . This can also cause intestinal damage.
- Cholecystitis and appendicitis . If they are not treated in time, gangrene may develop.
- Arterial thrombosis , if mesenteric, that is, feeding the intestines, is affected.
- Pneumonia . If the disease is caused by microbes like Pseudomonas aeruginosa or Clostridia, and the patient has problems with the immune system, this can lead to gangrene, including affecting the lungs.
With the gas, or so-called anaerobic type, everything is somewhat simpler. There is only one reason why the gangrenous process begins. This will happen if clostridia get into a deep wound, especially a wet one. However, there are several conditions. First, the microbes must reach fatty tissue or muscle tissue. Secondly, there should be a poor blood supply in this area. Thirdly, the wound must be closed, which will cause the parasites to begin to multiply faster.
The causes of bedsores have already been discussed above. It is worth noting that approximately 70 hours are enough for them to appear. People suffering from heart, liver or cancer diseases are more susceptible to bedsores. As for noma, the reasons for its appearance in children include pathologies such as rubella, meningitis and measles.
Gangrene is always a consequence of some kind of protracted illness, so you should never neglect even small symptoms
Prevention of pathology
Prevention of gangrene is as follows:
- Careful care of the wound to avoid the penetration of pathogenic microflora into it.
- Treatment of diabetes mellitus.
- Prevent skin exposure to high or low temperatures.
- Timely treatment of diseases of the body that can cause necrosis of the limbs.
- Strengthening the immune system.
- Maintaining a healthy lifestyle.
Gangrene is a disease that can be very life-threatening if you do not get rid of it in time. Therefore, you should immediately contact a medical facility if the slightest signs of pathology occur, and not try to cure the disease on your own.
How to notice the development of dry gangrene?
It is important for any patient to notice in time that gangrene is beginning. The earlier the onset of the disease is determined, the lower the likelihood that you will have to think about removing a leg or part of it. As with the causes, the signs of gangrene also depend on its form. The beginning of the pathological process in the dry type can be suspected by the following factors:
- In the entire painful limb, or in its individual parts, such as fingers, goosebumps or tingling will be felt. Severe pain may be present when moving.
- The infected limbs will experience weakness, especially noticeable after exertion such as long walking or running.
- Due to insufficient blood supply, the tissues will begin to turn pale and become cool to the touch.
- The disease is characterized by the so-called intermittent claudication (intermittent claudication is the periodic occurrence of paresthesia and pain in the legs (usually in one) when walking, forcing the patient to stop; the main symptom of diseases manifested by chronic occlusion of large and medium-sized arteries of the extremities).
There is a way to check whether the blood supply to the lower extremities is normal. To do this, you need to lie on your back and raise your outstretched legs at an angle of 45 degrees. Firstly, patients will not be able to maintain this position for more than 25 seconds. Secondly, they will begin to experience characteristic symptoms, such as goosebumps and weakness, and their skin will turn pale.
On video: TV program - Health. Gangrene. How to avoid amputation? (from 05/13/2018)
If you do not notice the problem at this stage, then in the near future you will have to deal with tissue necrosis. At this phase, their blackening will begin. It is this color that indicates dry type gangrene, since in the case of noma the shade may differ. The process of tissue necrosis will also be accompanied by:
- Reduction of the affected limb.
- Feeling of dryness, cessation of sweating.
- Increased density of diseased tissue.
- Nails and hair will not grow in the area affected by gangrene.
The most important thing to pay attention to is that at this stage of dry gangrene, a person does not feel pain in the limbs, since the nerves have already died along with other tissues. However, in this case there are new symptoms of gangrene associated with intoxication. These include fever, dizziness, poor appetite, nausea and other similar manifestations.
Photo of gangrene of the lower extremities at the initial stage:
Spoiler with a slight shock photo of gangrene of the toes at the initial stage.
The photo shows gangrene of the lower extremities, toes, in the initial stage. You can determine the presence of problems with blood flow at home, but tests and consultation with a specialist are still a necessary measure for your own peace of mind. [collapse]
Diagnostic methods
Examination of the foot
When the first symptoms appear, which may indicate the development of gangrene of any type, it is necessary to urgently consult a surgeon. The doctor examines the leg and a separate area that is suspicious and interviews the patient. During palpation, the surgeon will be able to determine the thickening of the skin, evaluate the color; when pressing on the affected area, when gas gangrene develops, a specific crunching sound will be heard due to the bubbles.
If the fears are confirmed, the doctor may prescribe additional testing: wrap a thread around the affected area to monitor swelling of the foot. As swelling increases, the thread begins to dig into the skin. During the diagnostic process, the following tests must be performed:
- General blood analysis.
- Biochemical analysis.
- Blood test for contamination.
- Bacteriological analysis of wound discharge.
- X-ray of muscle tissue.
- Analysis of urine.
Most often, after a preliminary examination, the patient is prescribed a referral to a hospital, where the most effective treatment tactics are selected.
Signs and symptoms of other types of gangrene
Wet gangrene of the legs
In the case of wet gangrene, the color of the affected tissue will gradually change to bluish or dark purple. Unlike the dry type, it is impossible to see clear boundaries between diseased and healthy areas, since the microbes will continue to spread throughout the tissues. Soon the smell of rot will be added to the color, and the affected limb will begin to swell.
Note. The wet, wet type of gangrene of the legs will also be accompanied by pastiness, the so-called pre-edema state, which is characterized by paleness of the tissues and a decrease in the degree of their elasticity. They feel like dough to the touch.
The wet type of gangrene of the lower extremities is characterized by constant acute pain . As with dry gangrene of the legs, there will be a decrease in temperature in the affected tissues. All the same symptoms of gangrene are observed in the case of noma development.
Gas gangrene of the legs
In addition to pallor and swelling, gas gangrene is characterized by the release of a cloudy green or brown liquid with an unpleasant odor. Also, muscle fibers are sometimes visible through the wound. If gas gangrene develops, they become pale, whitish and seem to be stratified. When palpating the lower limb, a specific crunching sound occurs.
Most people with gas gangrene die because they have severe poisoning. Weakness develops so much that the person cannot move, and the temperature rises to 41 degrees. Patients with gas gangrene begin to experience delirium, constant vomiting and nausea, severe pressure surges and tachycardia.
The appearance of bedsores during gangrene
As for bedsores, they, to one degree or another, are characterized by all the same symptoms as other types. The difference is that they develop very slowly and very locally. Fortunately, this is the easiest way to deal with this problem. It is enough to regularly change the position of the patient and massage areas where bedsores may appear.
It is much more difficult to determine wet gangrene, because... even skin color is not always a clear sign of the active development of microbes
Stages and features of localization
The International Classification of Diseases (ICD 10) considers the condition under code R02.
Necrosis of the lower extremities is distinguished by location and stage of the process. There are 4 stages of gangrene.
| Stage | Peculiarities |
| 1 | At the initial stage, shallow lesions appear. The bone tissue is not affected or up to 10% is affected. The patient feels some discomfort, but this does not affect the full functioning of the limb. The condition is reversible, but requires qualified intervention. |
| 2 | Bone tissue suffers - cracks and destruction occur. The patient is accompanied by painful sensations. Movement and limb functionality are limited. Urgent surgical intervention is required. |
| 3 | The decomposition process is quite deep. The bone is affected by 40 - 50%. The patient suffers from severe pain in the affected area. The functionality of the leg is absent or significantly limited. |
| 4 | Complete destruction of soft tissue and bone. The person's condition is critical. High probability of sepsis. Urgent amputation of the affected area is necessary. |
Tissue decomposition can affect the entire limb.
The disease develops in the hip area, at the knees, on the legs, and in the foot area - due to severe stress. In patients with diabetes, gout, kidney or liver failure, necrosis in the foot area is observed - frequent damage to the toes, upper arch and heel. Wearing tight shoes promotes the development of the process. If a necrotic lesion occurs on one finger, gangrene will spread to others. The main problem with foot decomposition is partial or complete restriction of movement. The patient cannot wear shoes, the irritation causes acute pain.
In severe cases, in order to avoid toxic poisoning of the body and the spread of necrosis, it is necessary to amputate the diseased area along with a small healthy area.
What to do with gangrene, how to treat it?
Any patient who is ill will, first of all, be interested in treating gangrene of the lower extremities without amputation. If the prognosis is favorable, then doctors will try to save the legs, but it is worth understanding that the affected tissue will have to be removed in any case.
Note. Alternative treatment for gangrene of the legs cannot be effective against this disease, especially in advanced stages of development of the pathology.
The stages of exposure will include the removal of tissue with the accompanying use of strip incisions, which provide additional air flow. The patient will then be prescribed a course of antibiotics, an infusion of crystalloid solutions and anti-gangrenosis serum. If such treatment does not have the desired effect, the limb will have to be removed.
The sooner the problem is detected and measures taken, the greater the chance that the limb will remain unharmed, i.e. amputation of the leg or arm will not be required.
On video: Gangrene of the legs. Rescue from amputation. Medical center Sofia, Anapa
Forecast
The prognosis after surgery is not very comforting; even intestinal resection does not save half of the patients.
If conservative methods help and there is a chance to restore the damaged areas, then the survival rate is greater. But this is only at the early stage of the disease, and only a few seek help during this period.
For everyone else, the chance of recovery is less than 50%, of which another 30% may develop complications.
External signs of necrosis at the initial stage
In order not to miss the development of gangrene, it is necessary to pay attention to such possible manifestations as:
- loss of sensation in the legs;
- numbness or tingling sensation;
- limbs often freeze as a result of poor circulation;
- pale skin color on the feet, later the leg turns red or blue;
- legs often get tired;
- the color and structure of nails changes, their fragility and susceptibility to fungal infections increases;
- an unsteady gait with pronounced lameness appears;
- Fever and nausea may occur.
Having discovered such signs, you should immediately undergo examination and begin treatment.
By changing the color of the skin of the legs, you can notice how necrotic damage to the tissues of the extremities begins.
With dry necrosis, the following changes occur:
- redness of the fingers is observed;
- the redness subsides and the skin turns pale;
- a bluish tint appears;
- dying fingers turn black;
- a clear boundary between affected and healthy tissues is visible.
Progressive pathology can no longer go unnoticed.
Signs of dying become pronounced:
- against the background of normal health, pain in the legs bothers you;
- limbs become insensitive to external influences;
- Dying and healthy tissues are more clearly distinguished;
- the pulse in the leg disappears;
- deformation of the foot and its drying out occurs.
Wet gangrene manifests itself somewhat differently:
- a venous network becomes noticeable on pale skin;
- limbs become swollen;
- at the initial stage there is no difference between diseased and undamaged areas.
Advanced wet gangrene manifests itself as clearly noticeable symptoms:
- intense pain that cannot be relieved;
- the skin turns black and becomes covered with blisters containing pus;
- an unpleasant odor appears from ulcers and wounds;
- high temperature and low pressure are observed, tachycardia increases;
- vomiting, tremors in the legs, and seizures occur.
Video about the stages of development of necrosis in diabetes mellitus:
Treatment
Treatment of intestinal necrosis is carried out in the following areas:
- Conservative therapy.
- Relieving therapy.
- Surgical intervention.
The first two directions are mandatory, but surgery is prescribed according to indications, but since necrosis at an early stage is detected only in small quantities, most patients will still need it.
Conservative therapy
A patient with necrosis is given:
- antibiotics;
- protein solutions;
- anticoagulants;
- electrolytes.
All this is done to reduce blood clotting, reduce the amount of thrombosis, eliminate infection and support the body.
Relief therapy
To reduce the load on the intestines, the patient’s stomach and entire intestinal tract are washed from all sides. If there is no accumulation of feces and undigested food, the likelihood of squeezing blood vessels will decrease. They can also, if necessary, intubate the large or small intestine, bringing the tube to the anterior wall of the abdomen, which will allow feces to be excreted through it in the future.
Surgical intervention
Most patients are indicated for intestinal resection (the necrotic part), but even this does not always provide a chance of survival. The patient has the damaged part of the intestine removed and the healthy ones stitched together; if this is not possible, then a colostomy is performed.
Laparoscopy may help if necrosis has just begun. Then such a small operation will eliminate the resulting defect without performing a full-fledged operation, which will significantly reduce the risk of infection.
Video about gangrene of the leg
Elena Malysheva will talk about gangrene:
Gangrene of the lower extremities is one of the diseases that is one of the most severe surgical pathologies. This process is characterized by necrosis, that is, tissue death. How long people live after the onset of gangrene directly depends on how quickly and efficiently the treatment is received. Of course, it is impossible to cope with gangrene of the limbs at home; using folk remedies will not give any result.
Although some reviews may talk about the effectiveness of such home, folk treatment, in reality, amputation of dead tissue is often the only solution. The longer no action is taken, the more gangrene will spread throughout the limb, and the more tissue will have to be removed. It is necessary to understand how and why gangrene develops in order to prevent such an outcome. If you notice signs and symptoms of any form of gangrene, immediately contact the clinic for timely examination and diagnosis of the disease.
This is what gangrene looks like in the initial stages of its development.
How long does recovery take?
After removing dead fingers, the wounds usually heal within 3-4 weeks without any additional operations. If a foot resection is performed, the ability to walk appears about a month after the removal of dead tissue. With diabetic infected gangrene, healing is 2-3 times slower.
We save the leg during gangrene! Call (free in Russia)
The same patient 3 weeks after transplantation of a vascular pedicle flap. The wound defect is closed. The foot is preserved.
A 55-year-old patient with diabetes mellitus, thrombosis of the popliteal artery and an extensive necrotizing circular ulcer of the leg. Endovascular surgery was performed - Rotarex thrombectomy, balloon angioplasty and popliteal artery stenting. The blood flow was restored in full. Subsequently, reconstructive surgery with islet muscle grafting was performed to cover the exposed bones and a split-thickness skin flap was transplanted.
A month after the vascular and reconstructive plastic surgery, the wound was completely healed, blood circulation in the leg was compensated.
A patient with critical ischemia secondary to thrombosis of the iliac artery. In another medical institution, hip amputation was proposed. He was admitted to the clinic with severe pain in his left leg, which could only be relieved with epidural anesthesia.
The patient underwent balloon angioplasty and stenting of the iliac arteries. View of the wound 3 days after surgery. The wound has cleared and is healing. Skin grafting is expected. The question of amputation has been removed.
A patient with severe circulatory failure in the leg with the formation of a necrotic wound in the heel area. He was treated in other vascular surgery institutions without success due to damage to small vessels. He was admitted for microsurgical bypass surgery of the arteries of the leg.
Photo one month after surgery to restore blood flow. The wound has completely healed.
Photo of gangrene against the background of atherosclerosis. A 68-year-old female patient was admitted with subtotal dry gangrene of the foot. Before admission, she was treated for a long time in the vascular surgical department at her place of residence with a diagnosis of obliterating atherosclerosis. Endovascular intervention was attempted but without success. We performed a microsurgical femoral-anterotibial shunt using our own vein. Blood circulation was restored.
After restoring blood flow, we removed the foot with the formation of a supporting stump of the leg according to Pirogov. Such a stump allows the patient to walk without a prosthesis, and the prosthesis itself is a comfortable boot-type design.
Consultations with a vascular surgeon
Moscow, Leninsky Prospekt, 102 (metro station Prospekt Vernadskogo)
Make an appointment
Questions and answers
Hello! Initially, I hit my toe on a step in the dark) I initially applied iodine to the bruise, but it didn’t help that the toe began to swell and twitch for a month.. I went to a paid clinic: Examination by a surgeon - he says it looks like an ingrown toenail, I.
Answer:
Call me back on the phone
Hello! I would like to know from you! My grandmother, she is 84 years old, gangrene of her left leg began; she underwent surgery on blood vessels at the Gorbacheva Pathological Clinic in St. Petersburg, but nothing good was done.
Answer:
We are doing this successfully. Send research data, a medical statement and a photograph of your leg in the “Correspondence with the Doctor” section. It is advisable to do this as quickly as possible, as gangrene progresses. You can come to the nearest one.
gangrene or other.
Hello! My father has this problem. 3 6 days ago I tore off a callus on my toe, the toe turned blue with a bruise, went to the surgeon for a dressing, the ichor and leg began to come out.
Answer:
Urgently see a vascular surgeon and be sure to do an ultrasound of the blood vessels.
Atherosclerosis and gangrene
hello, my father (71 years old) has atherosclerosis of the vessels of the arteries of the lower extremities, gangrene has begun on the toe of his right foot, there are pictures, tests, we hoped for an operation, but we were told that it was too late to save the leg.
Answer:
It is necessary to send ultrasound data of the arteries and photographs of the leg in the “Correspondence with the doctor” section.
Diabetic foot gangrene
My husband developed a black spot on his right foot, his big toe did not turn so quickly and the floor of his foot turned dark purple. They were admitted to surgery for treatment with a diagnosis of wet gongrene of the lower extremity.
Answer:
We deal with such pathology. Bring the patient directly to the clinic for a consultation; if space and indications are available, we will hospitalize him. Contact the chief physician A.V. Sedov. regarding hemodialysis and places.
gangrene of the thumb of the lower extremities
Hello. I am 35 years old. On April 30, 2014, I had surgery to ligate the femoral artery. I can’t walk, there is swelling in my lower legs, and I have no feeling in my foot. An ultrasound showed phlebitis of the superficial and deep veins of the lower limb, endarteritis of the arteries of the lower limb with stage 3 urinary tract. I have unbearable pain, I can’t sleep. They appeared.
Answer:
Come to the clinic urgently, we have every opportunity to help. Amputation at 35 years old, maybe. produced only in a hopeless condition. Phone number of the chief physician, Alexey Valerievich Sedov.
critical ischemia of the lower extremities
Good afternoon Dad is 75.5 and has diabetes. Currently, he was treated in surgery, the diagnosis was polyneuropathy, critical ischemia of the lower extremities. The feet burn, the joints on them become inflamed, and abscesses form.
Answer:
You need to see a surgeon, that's their job.
Leriche Gangrene Syndrome
Hello! My father (57 years old) was diagnosed with Leriche syndrome. Due to gangrene, three toes of the right foot were amputated, starting with the big one. At the moment they say that there are no other options other than amputation.
Answer:
Send medical reports on blood vessels, ECHO data, photographs of legs. We may be able to perform endovascular treatment.
Good afternoon. My father is 84 years old. He is diagnosed with gangrene. Doctors refuse to perform surgery, citing his age and health. Now he is being treated with medication - they give him IVs, pain-relieving injections and apply ointments to his foot, but his condition has improved.
Answer:
Send in the “Correspondence with the Doctor” section photographs of your leg and ultrasound data of the arteries. After that I will be able to answer this question for you.
Gagrene in the legs of a 75-year-old grandmother after a heart attack
Hello. I want to ask you, my grandmother was admitted to the hospital with gangrene of her leg and we were told that it was necessary to amputate the leg above the knee. She is after a heart attack and she is 75 years old. Costs.
Answer:
There are 2 treatment options: reconstructive surgery on blood vessels (bypass surgery or stenting through a puncture), or amputation for health reasons.
© 2007-2019. Innovative vascular center - vascular surgery at a new level
Causes of the pathological condition
The list of provoking factors that lead to necrosis are divided into three main groups:
- thrombotic;
- embolic;
- non-occlusive.
Thrombotic causes include thrombosis of the arteries or mesenteric veins. Basically, thrombosis is located in the mesenteric artery, namely in the upper mouth. The following pathologies lead to a similar condition: peritonitis, intestinal obstruction, polycythemia, tumor, hormonal contraception, various injuries, heart failure, high blood clotting.
The embolic type is possible during blockage of the mesenteric vessels with the help of thromboembolus, which migrates from the proximal part. Causes include improper coagulation, aortic aneurysm, and myocardial infarction. These diseases provoke migratory ischemia.
The non-occlusive variety relates to decreased blood flow to the visceral vessels. Provoking factors include dehydration, sepsis, mesenteric thrombosis, arrhythmia, spasm of mesenteric vessels, and reduced cardiac ejection fraction.
In some cases, the listed provoking factors are combined with each other, so the disease occurs with subcompensation, compensation and decompensation of blood flow. During the infarction stage, necrosis of this organ is observed, the protective functions of the intestine weaken, and bacteria attack the deeper layers in the abdominal cavity. When the stage of peritonitis occurs, the intestinal walls begin to disintegrate.
Specifics of therapy
The goal of treatment is to eliminate any pathogenetic parts of the pathology. The patient is hospitalized, after which infusion therapy is administered to help compensate for the lack of blood, restoring the perfusion of the necrotic intestine. Conservative therapy is used only in the absence of peritonitis. The effectiveness of treatment is observed if all recommendations and prescriptions of the doctor are followed. If there is no effect, urgent surgery is necessary.
In the case of such a pathology, surgical intervention on the vascular bed is considered radical. When the operation is performed within 24 hours of the onset of the disease using laparotomy, irreversible consequences in the intestine can be confirmed in 95% of all cases. Regarding radical resection, we can say that it does not guarantee the absence of death.
This disease requires urgent surgery. The prognosis is usually unfavorable. This is due to the fact that the pathology is extremely rarely diagnosed at the initial stage. Late treatment may not give the expected result.
Exodus
The significance of the consequences of tissue necrosis for the body is determined based on the functional characteristics of the dying parts. Necrosis of the heart muscle can lead to the most severe complications. Regardless of the type of damage, the necrotic focus is a source of intoxication, to which the organs respond by developing an inflammatory process (sequestration) in order to protect healthy areas from the harmful effects of toxins. The absence of a protective reaction indicates suppressed immune reactivity or high virulence of the causative agent of necrosis.
- Internal hemorrhoids in women: symptoms and treatment
- How to treat bedsores
- Erysipelas of the skin
An unfavorable outcome is characterized by purulent melting of damaged cells, complications of which are sepsis and bleeding. Necrotic changes in vital organs (kidney cortex, pancreas, spleen, brain) can lead to death. With a favorable outcome, the dead cells melt under the influence of enzymes and the dead areas are replaced with an interstitial substance, which can occur in the following directions:
- organization - the place of necrotic tissue is replaced by connective tissue with the formation of scars;
- ossification - the dead area is replaced by bone tissue;
- encapsulation – a connecting capsule is formed around the necrotic lesion;
- mutilation - external parts of the body are rejected, self-amputation of dead areas occurs;
- petrification - calcification of areas that have undergone necrosis (replacement with calcium salts).
Reviews
Katerina Volova, 33 years old, Moscow
My mother was 68 years old and had type 2 diabetes for more than 30 years. We learned that she had gangrene on her left leg when she was 66 years old. It all started with a small spot on my little finger, which no one paid much attention to. Then my mother began to complain of pain in her leg and numbness. Literally a week later, a small spot affected the entire little finger, we went to the doctor, who said that it was gangrene and necrosis was already present, so the only way was to have surgery to remove the finger. But not everything is so simple, the doctor refused to perform the operation, he said that the heart would not withstand anesthesia, so he was admitted to the hospital for maintenance therapy. The doctor immediately told me that I could prepare for the worst. A month after the treatment, my mother’s whole foot and toes had already darkened, she was suffering from severe pain, she was injected with narcotic medications to reduce the pain. In general, after 5 months, my mother passed away! The doctor told me that if they had contacted me earlier, when the spot first appeared, perhaps there would have been a chance, but alas!
Valentina Sviridova, 46 years old, Voronezh
My husband is 55 years old, but he was able to overcome gangrene, although he suffered for more than 2 years. In general, the cause of the disease is not known to us; he does not suffer from diabetes. It all started with the appearance of a small dark spot on the big toe, we immediately went to the doctor, who was “pleased” that it was gangrene and if we wanted to save the limb, we needed to amputate the toe. The operation was successful, but after 2 months there was a relapse and another operation. In total, in 1 year we had to undergo 4 operations, each of which deprived my husband of part of his leg. More than a year ago, the doctor said that the last chance was if we amputated the entire leg, 20 cm above the knee, we agreed. After this operation, there was severe pain, but as the doctor explained, this is good, since there are “living” vessels and tissues. More than a year has passed since that operation, the disease has not progressed further, my husband experienced severe depression, but everything turned out okay. Three months ago they ordered him a prosthesis. Now he is learning to walk again, and last week he even got behind the wheel of a car. We really hope that this will be the end of our troubles!
Sergey Kosynov, 48 years old, Sverdlovsk
A year ago, I suffered a severe leg injury at work, a large hematoma formed, followed by tissue necrosis. The doctor said that there is a risk of gangrene and if treatment measures are not taken in time, then the prognosis could be disastrous. I spent more than a month in the hospital, took a lot of medications, antibiotics, had surgery, the wound did not heal well, it was constantly oozing, and only after a month did improvements begin. The doctor said that there should be no gangrene, but still advised to monitor the condition of the skin on the leg, as well as general well-being. The doctor said that I was lucky that I did not have diabetes. I feel good so far, but I’m still very worried!
Kristina Rogova, 38 years old, Krasnodar
My grandfather died of dry gangrene 3 years ago, but as the doctors later said, if he had sought help sooner, he could have lived to this day. The mistake was that he was treated with various herbs, lotions, infusions, and only when the pain became unbearable did he turn to the doctors, who immediately said that there was no chance, and he might not be able to endure the operation. He was given only 3 months, but he lived a little more than six months, although he suffered very much! I would like to advise that gangrene cannot be treated with traditional methods, because in this way a person wastes time!
Prevention of gangrene of the leg
To prevent the disease, it is necessary to minimize the likelihood of damage to the skin as a result of various injuries, and also to avoid getting soil or dust into the wound. If such a situation occurs, you should immediately wash the wound with 3% hydrogen peroxide and consult a specialist.
Patients with diabetes should be especially careful to avoid skin damage, punctures or other injuries. The regeneration function in such patients is impaired, so the likelihood of developing gangrene is increased.
In addition, it is recommended to balance the diet, replenish the deficiency of nutrients, and strictly observe the rules of personal hygiene.
Additionally, doctors recommend that patients with varicose veins, thrombophlebitis, obliterating endarteritis, atherosclerosis, diabetes mellitus, and vibration disease regularly visit a medical facility so that a specialist can assess the condition.
This will minimize the risk of developing gangrene and also improve the patient’s general condition.
Diagnostic measures
It is enough to make an accurate diagnosis based on the patient’s complaints, the results of a visual examination and palpation of the limb. Laboratory research methods are carried out only to clarify the general condition of the patient and determine the sensitivity of microorganisms to antibiotics.
To assess health status, a number of the following studies are carried out:
- blood biochemistry for the degree of inflammation (leukocyte level, urea/creatinine, reactive protein and other indicators);
- urine analysis (protein and glucose content, density);
- smear from the site of gangrenous changes;
- Bethe test (placing a piece of tissue in 6% sodium chloride to determine anaerobic gangrene - if the tissue floats, then we can talk about gas gangrene).
If there are doubts about determining the degree of gangrenous lesion of the limb, then an x-ray or ultrasound is performed. The anaerobic process is confirmed by the presence of gaseous bubbles on the image or computer monitor. All diagnostic measures are carried out quickly to immediately prescribe therapeutic or surgical treatment.