Causes
The reliable causes of this disease have not been established, but it is known that erythema nodosum is a form of allergic vasculitis. The disease is based on allergic reactions and immune disorders, which lead to vascular inflammation.
The appearance of erythema nodosum is in no way related to the gender and age of the patient. Adults and children are equally affected, but the prevalence of the disease among women is higher than among men.
Erythema nodosum in children is often caused by infectious diseases, allergic reactions, and gastrointestinal disorders. The disease is mainly diagnosed after reaching 6 years of age.
Causes of erythema nodosum in adults:
- infectious diseases caused by streptococcus;
- tuberculosis, yersiniosis, trichophytosis, inguinal lymphogranulomatosis, coccidomycosis, syphilis, hepatitis B, chlamydia, histoplasmosis and others;
- sarcoidosis, oncology;
- acute rheumatic fever, Behcet's disease, ulcerative colitis, paraproctitis, Crohn's disease;
- allergic reaction, including those caused by medications (the most dangerous are antibiotics, salicylates, bromides, iodides, sulfonamides and vaccines).
Erythema nodosum may appear during pregnancy.
Chronic erythema nodosum often occurs in patients with vascular pathologies (varicose veins, atherosclerosis), chronic infectious diseases (tonsillitis, sinusitis, pyelonephritis), hereditary predisposition, as well as in people who suffer from allergic reactions such as bronchial asthma or atopic dermatitis.
Erythema nodosum and pregnancy
This disease during pregnancy, according to various sources, is diagnosed in 2-15% of women. It is believed that the same mechanisms underlie its development. Pregnancy is a unique state of a woman's body. It is possible only if there is a balance between nonspecific and specific types of immunity. It is these factors that direct the immune response along a certain “channel”.
The restructuring of the endocrine and immune systems during gestation is a vulnerable link, which creates the conditions for the occurrence of erythema nodosum. Acute or activation of chronic infection during gestation against the background of physiological immunosuppression (suppression of immunity) to an even greater extent includes the mechanisms of the latter, which contributes to the sensitization of the vascular network of the dermis and hypodermis and leads to the threat of miscarriage.
How, during what period, and with what to treat erythema nodosum during pregnancy are always difficult questions for doctors, who must take into account the negative impact not only of the disease itself, but also of medications on the fetus. Antibiotics and antibacterial drugs have a particularly adverse effect during the formation of organs and systems of the unborn child (in the first trimester of pregnancy).
Thus, the main role in the etiology and pathogenesis of the disease is given to the body’s immune response to the influence of an infectious or non-infectious damaging agent. The role of the human body’s reactivity in this process, as well as all the links in the mechanisms of its interaction with aggressive agents, remain sufficiently unexplored.
The predominant localization of the pathological process on the legs is also not entirely clear, which is associated mainly with slow blood and lymph flow, with the structural features of muscle tissue and the vascular network of the lower extremities and with stagnation in them.
Symptoms
With erythema nodosum, redness appears on the surface of the skin. It has a dense texture, and upon palpation the patient experiences pain. In some cases, the nodes disappear on their own, but if this does not happen, they begin to increase in size.
These formations are located in the lower parts of the dermis or in the subcutaneous tissue. Their size is 0.5-5 cm. The skin over the nodes turns red, but its structure does not change. The skin is smooth to the touch, but visually you can notice elevations that are caused by swelling.
More often, erythema nodes on the legs are localized in the lower leg area and on the inner side of the thigh. There is symmetry of the lesion.
The nodes grow quickly. As they reach a certain size, their growth stops, but the symptoms become more pronounced:
- pain increases, which can occur not only during palpation;
- on days 3-5 of illness, the nodes become even denser;
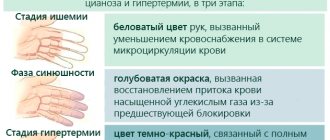
- the skin acquires a brown and then bluish tint, reminiscent of a bruise, and over time the skin becomes green or yellow.
If the cause of erythema nodosum is an infectious disease, then local symptoms are supplemented by general malaise. The initial stage is accompanied by increased body temperature, fever, chills, weight loss, joint pain and stiffness.
Joint syndrome with erythema occurs in a third of patients. The symptoms are similar to arthritis.
After a month, clinical manifestations gradually subside and recovery begins.
The first symptoms of erythema in children appear 5 days after the development of the disease. The baby becomes capricious, the child’s body temperature rises, headaches, muscle and joint pain appear, and the stomach hurts. Local symptoms are similar to those in adults.
Features of the course and danger of the disease
The appearance of erythema is preceded by a period during which a person feels extremely weak, quickly gets tired, fever, swelling in the joints, pain, and stiffness appear. Symptoms often resemble those of the onset of influenza. Pain in the legs and joints continues for some time after the rash.
Erythema manifests itself as sudden rashes. If the course is acute, it is accompanied by fever, abdominal pain, vomiting, and diarrhea. Nodules appear symmetrically on the legs, in the anterolateral part. In rare cases, they spread over the surface of the arms, neck, and shoulders.
Externally, the nodules are soft, warm thickenings, from 1 to 5 cm in diameter. At first they have a bright red color, and then change it to blue-yellow. The boundaries of the nodes are unclear because the surrounding tissue is swollen. The nodes may be painful upon palpation. The rashes remain on the skin for several weeks or months, then the nodules heal without atrophy or scars.
In children
Erythema nodosum in childhood is acute. It is characterized by painful rashes that appear on the lower extremities, in the area of the legs, which can merge with each other.
Cause:
- reaction to tuberculosis;
- streptococcal infection of the upper respiratory tract.
- reaction to antibiotics, sulfonamides.
The course of the disease is accompanied by symptoms:
- pain in muscles and joints;
- feeling overwhelmed;
- heat;
In adults
Currently, the leading cause of erythema in adults is sarcoidosis. The frequency of occurrence is up to 65% in various regions. Erythema nodosum is often combined with joint damage.
Other symptoms accompanying erythema developing against the background of sarcoidosis:
- severe swelling of the lower extremities;
- arthralgia of the ankle joints
- large size of nodules, their fusion;
- cough, chest pain, shortness of breath.
Common causes of the syndrome are inflammatory bowel diseases and the use of medications. Tuberculosis is not currently a common cause of erythema nodosum.
During pregnancy
During gestation, when a restructuring of the endocrine-immune cascade occurs, women carrying a child may develop erythema nodosum. This occurs in 8% of pregnant women. During this period, it is extremely important to be promptly examined for infectious markers. The presence of herpes simplex viruses, mycoplasmosis, and chlamydia contributes to the development of erythema syndrome.
Classification
There are 3 forms of this disease, which differ in symptoms:
- Acute erythema nodosum. Nodes measuring 0.5-5 cm in size form symmetrically on the limbs. They are dense and painful, rising above the surface of the skin. Having reached their maximum size, the nodes stop growing. After 2-4 weeks they disappear. Relapses do not occur. The skin in their place may remain reddish for some time and peel off a little. Along with external manifestations, articular syndrome also disappears.
- Chronic. This form of the disease is rare, mainly in women over 40 years of age who are diagnosed with a tumor of the pelvic organs or chronic infectious diseases. With this form of erythema, the nodes do not disappear a month after their appearance. They may decrease, but then reappear in larger numbers. Exacerbations are observed in the autumn-spring period. There are no symptoms of intoxication, there are signs of chronic arthropathy, but the joint is not deformed.
- Migratory. The symptoms of the disease are mild. General symptoms come to the fore - weakness, malaise, increased body temperature up to 38 ° C, muscle and joint pain. Local signs are represented by one node, which is localized on the anterior surface of the leg. Over time, a plaque forms, in the center of which there is a white depression, the edges are red. Then more nodes appear.
Symptoms of erythema nodosum
Depending on the severity, nature of the course and duration of the inflammatory process, the following forms of the disease are distinguished:
- Spicy.
- Migrating.
- Chronic.
Acute erythema nodosum
It is a classic type, but not the most common variant of the course, the development of which is usually preceded by an acute infectious disease (tonsillitis, ARVI, etc.).
It is characterized by the sudden appearance on the legs in the area of the anterior and lateral surfaces of the legs (sometimes the thighs) of typical multiple elements in the form of subcutaneous nodes with a diameter of 5 to 60 mm or more, which can merge with each other, forming red plaques, and are never accompanied by itching . The occurrence of rashes is accompanied by pain of varying intensity, both at rest and when palpating them.
The nodes have a dense consistency and unclear outline (due to tissue swelling), and slightly rise above the surrounding healthy skin surface. They quickly grow to a certain size, after which their growth stops. The skin located above them is smooth and red. Regression of granulomas can occur on their own within 3 (in mild cases) or 6 (in more severe cases) weeks.
Their reverse development is never accompanied by the formation of ulcers and atrophic or hypertrophic scars. The nodes disappear without a trace, but sometimes peeling of the epidermis and/or hyperpigmentation may temporarily remain in their place.
Erythematous lesions are usually located symmetrically, but occasionally on one side, or are represented by single nodes. Very rarely, granulomas appear on the arms, neck and face, where they can merge with each other, forming erythematous (red) plaques, and sometimes extensive, merging lesions.
Localization of the process on the palmar and plantar (plantar) surfaces is usually unilateral and is more common in children, very rarely in adults. Plantar localization of erythema nodosum must be distinguished from the so-called plantar traumatic urticaria, which looks like areas of reddened skin on the soles. The latter occurs in children as a result of significant physical activity. Dynamic observation makes it easy to distinguish erythema nodosum from plantar erythema, in which the redness disappears within a few hours to 1 day.
Quite often, the onset of the acute form of erythema nodosum is accompanied by high body temperature (up to 39°) and general subjective symptoms - weakness, malaise, headache, abdominal pain, nausea, vomiting and diarrhea, pain in the joints and muscles. Approximately 32% of patients have symptoms of an inflammatory process in the joints - intra-articular effusion, the presence of skin hyperemia and tissue swelling in the joint area.
1. Plantar localization; 2. Localization of erythematous nodes on the legs
Acute form of the disease
Migratory form
It occurs with similar clinical manifestations described above, but, as a rule, has an asymmetrical nature and a less severe inflammatory component. The disease begins with the appearance in a typical area (anterolateral surface of the leg) of one flat node of pasty consistency and cyanotic (bluish) color.
The node quickly grows due to its peripheral zones and transforms into a deep, large plaque with a sunken and pale central part. Its peripheral sections are surrounded by a richly colored ridge. The main node can be accompanied by single small nodes. The latter are often located on both legs. General symptoms are also possible - low fever, joint pain, general weakness and malaise. The duration of the migratory form ranges from several weeks to months.
Late stage of erythema nodosum
Chronic form
Usually develops in women in middle and old age, more often against the background of cardiovascular (chronic heart failure, obliterating atherosclerosis and varicose veins of the lower extremities), allergic, infectious-inflammatory (adnexitis, etc.) or tumor pathology, for example, uterine fibroids.
This form of erythema nodosum is characterized by a long, persistent course. It occurs with relapses that occur in the spring and autumn periods and last for several months, during which the reverse development of some nodes occurs and the emergence of new ones.
There are usually several nodes, they are dense, have a diameter of about 40 mm, bluish-pink in color, are localized on the anterolateral surface of the leg, are accompanied by mild pain and moderate intermittent swelling of the leg and/or foot. At the initial stage of their appearance, the color of the skin may not change, and the granulomas themselves can only be determined by palpation. General symptoms may be mild or absent altogether.
Diagnostics
A preliminary diagnosis is made based on a visual examination, patient complaints and medical history. Next, the patient is prescribed a number of additional examinations.
Diagnosis of erythema includes laboratory and instrumental research methods:
- clinical blood test - the inflammatory process is visible;
- bacterial culture from the mucous membranes of the nose and throat - to identify pathogenic microflora;
- rhino- and pharyngoscopy - to exclude chronic infectious diseases;
- blood test for rheumatoid tests - rheumatoid factor is detected;
- biopsy - to determine the nature of the erythema;
- stool culture - to exclude yersiniosis;
- fluorography – if tuberculosis is suspected;
- X-ray or CT scan of the chest - to exclude systemic diseases;
- Ultrasound of the veins of the lower extremities.
A set of diagnostic techniques for erythema is selected individually for each patient.
Differential diagnosis plays an important role in making the correct diagnosis. Erythema is differentiated from thrombophlebitis, Bazin's erythema, Christian-Weber disease and erysipelas.
What is erythema nodosum
The name “erythema nodosum” was introduced by the British dermatologist Robert Willan in 1807. For a long time, the disease was classified as a specific nosological entity. After some time, dermatologists conducted studies that proved that erythema nodosum is one of the variants of allergic vasculitis. Erythema nodosum differs from systemic vasculitis by its characteristic local vascular involvement, which is mainly limited to the lower extremities.
People of different age groups can get erythema nodosum, but it is more common in 20-30 year old patients. Both boys and girls can get erythema nodosum before puberty, and after puberty, the likelihood of the disease in men becomes several times less than in women. Cases of erythema nodosum become more frequent in the spring and winter.
Treatment
If erythema nodosum appears on the legs, treatment should be started immediately. You can get by with traditional therapy - systemic and local medications, physiotherapeutic procedures.
The treatment regimen and choice of medications depend on the patient’s age and individual characteristics. First of all, therapy is aimed at eliminating the underlying disease that led to the appearance of erythema nodosum.
In adults
Depending on the cause of the appearance of nodes, the following remedies can be used for treatment:
- antibacterial - Erythromycin or Penicillin;
- antiviral - Aflubin, Anaferon;
- antifungals – Ketoconazole, Nystatin;
- non-steroidal anti-inflammatory drugs - Nimesulide, Diclofenac, Celecoxib;
- hormonal – Prednisolone;
- aminoquinols (more often prescribed for the chronic form) - Delagil and Plaquenil;
- antihistamines – Suprastin, Cetirizine.
To treat the disease, physiotherapeutic procedures are used - plasmapheresis, phonophoresis, ultraviolet irradiation with hydrocortisone and laser therapy.
Locally, the use of anti-inflammatory and hormonal creams, for example, Elokom, is indicated.
In children
Erythema nodosum in children can only be treated in a hospital. If the cause is any systemic disease, then it is necessary to cure it. Rashes that appear as a result of infections, viruses or fungi are treated respectively with antibacterial (Cefazolin, Erythromycin), antiviral (Anaferon, Influcid) or antifungal drugs (Nystatin, Potassium iodide).
Erythema caused by an allergic reaction should be treated with antiallergic (Suprastin) or corticosteroid (Dexamethasone) drugs. Anti-inflammatory gels, such as Voltaren, are suitable for topical use. Heparin ointment has a warming effect.
Along with medications, physiotherapeutic procedures are effective - magnetic therapy, ultraviolet irradiation, phonophoresis and laser therapy.
To get rid of erythema, a small patient must follow the following clinical recommendations:
- adhere to bed rest, limbs should be higher than body level;
- apply warming compresses of 10% ichthyol solution to the nodes;
- Drink plenty of fluids; choleretic infusions (lemon balm, mint) are especially useful.
In pregnant women
Erythema during pregnancy cannot be treated with medications. A pregnant woman should be regularly observed by an obstetrician-gynecologist and examined by other specialists.
Erythema does not affect the ability to become pregnant and bear a child.
It is important for a woman to maintain bed rest and keep her legs above body level.
Treatment of erythema nodosum
If there is a pronounced picture of the disease, it is necessary to adhere to bed rest for a week, which helps reduce swelling of the lower extremities and the intensity of pain. In this case, it is recommended to give the legs an elevated position, and in case of severe symptoms, use elastic stockings or bandaging with elastic bandages.
Drug therapy
- For moderate and mild forms of erythema nodosum, treatment begins with the use of one of the drugs from the class of NSAIDs (non-steroidal anti-inflammatory drugs) - Ibuprofen, Paracetamol, Indomethacin, Ortofen, Diclofenac, Naproxen, Ibuklin, Meloxicam, Lornoxicam, Nimesulide, etc. They are taken for 3-4 weeks.
- Antibiotics, antibacterial and virusostatic agents. If possible, it is advisable not to prescribe them to pregnant women in the first trimester. The safest antibiotics for the fetus are penicillin group antibiotics (Ampicillin and Oxacillin), cephalosporins (Cefalizin, Ceftriaxone, Cefoxitim) and macrolides (Azithromycin, Erythromycin). But it is better to use them and other antibacterial agents in the second trimester, and in the second half of pregnancy the range of antibiotics used can be expanded.
- Aminoquinoline drugs Delagil or Plaquenil, which have anti-inflammatory, antiplatelet, antimicrobial, analgesic, antioxidant and other effects. Their administration to pregnant women is undesirable.
- Iodine-containing preparations (potassium iodide solution) and iodine substitutes that promote the release of heparin by mast cells, which suppresses delayed-type hypersensitivity reactions, reduces thrombus formation and improves microcirculation.
- Short courses of subcutaneous administration of Heparin or Fraxiparine (better) - in severe cases.
- Antiallergic drugs (Fexofenadine, Loratidine).
- Angioprotectors that dilate small vessels and increase their tone, reduce swelling and permeability of their walls, improve the rheological properties of blood and microcirculation (Pentoxifylline, Curantil, Vazonit, T rental, etc.).
- Vitamins “C” and “E”.
- Glucocorticoids (Prednisolone, Metipred, Dexamethasone, Diprospan) are indicated for erythema nodosum, especially associated with sarcoidosis, in the presence of an intense inflammatory process and in case of insufficient effectiveness of the treatment. They can be prescribed in low doses even at any stage of pregnancy.
- Plasmapheresis or hemosorption - in case of particularly persistent and protracted course of the disease.
Local therapy
Local treatment is carried out with applications with Dimexin solution or Ichthyol solution, Dimexin gel in combination with Heparin, indovazin cream in combination with ointment or cream with corticosteroids - Beloderm containing betamethasone, Belogent (betamethasone with gentamicin), Belosalik (betamethasone with salicylic acid) .
After stopping the acute manifestations of the inflammatory process, it is possible to use physiotherapeutic procedures in the form of ozokerite applications, phonophoresis with liquid ointment (liniment) containing dibunol, with heparin, with lidase or hydrocortisone. Inductothermy, magnetic therapy, ultra-high frequency currents, laser treatment, etc. are also used.
Unified standards and treatment regimens for erythema nodosum have not been developed. The main drugs currently used are antibiotics. At the same time, their widespread use can contribute to the transition of an acute process to a chronic one. This is explained by the lack of influence of antibacterial agents and antibiotics on viruses and even on many strains of bacteria. At the present stage, treatment of both idiopathic and secondary diseases, unfortunately, is aimed primarily at reducing the severity of local inflammatory processes and reducing the duration of the disease.
Traditional therapy
Treatment with folk remedies:
- Ointment or infusion with arnica. To prepare the ointment you will need 100 g of dry plant root. It needs to be ground into powder, add pork fat and cook for 3 hours. Lubricate the affected areas 3 times a day. Drink the infusion up to 5 times a day. To prepare 1 tbsp. l. dried flowers pour 200 ml of boiling water.
- Baths with potassium permanganate. It is necessary to prepare a weak solution. The duration of the procedure is 15 minutes, after which apply Ichthyol ointment.
- Sage tea. You need to drink 100 ml 2 times a day. Brew 2 tbsp. l. in 100 ml of boiling water.
- Red elderberry tincture. You need to fill the container with berries and fill it to the top with vodka. Leave for 40 days. Drink before bed, dosage depends on weight. If the patient weighs up to 70 kg, then you need to take 20 drops, if more than 70 kg - 30 drops.
- Compresses with Ichthyol ointment. The product should be applied to a bandage and applied to the affected area overnight.
- Infusion of horse chestnut and sweet clover leaves. You will need 1 tbsp. l. crushed leaves. Pour 200 ml of hot water over the herb and boil in a water bath for 15 minutes. Leave for 30 minutes. Take 1 tbsp. l. 3 times a day.
Folk remedies for erythema can be used for children and pregnant women, but only after consultation with a doctor.
Erythema nodosum of the lower extremities - causes
The exact causes of erythema nodosum are unknown. It is believed that the disease can develop against the background of systemic pathologies (leprosy, sarcoidosis, tuberculosis, tonsillitis, streptococcal infections, rheumatism).
In addition, the development of erythema can be provoked by mycoplasmas, chlamydia, some viruses and fungal microorganisms. In some cases, the trigger is the use of certain medications (bromides, antibiotics, contraceptives and a number of others).
The cause of the disease can be tumors (both benign and malignant) or inflammatory diseases of the gastrointestinal tract.
In women, pregnancy can trigger the development of the disease. In some cases, the cause of erythema cannot be determined.
Nutrition
Proper nutrition is important for erythema nodosum. When following a diet, you need to exclude the following foods from your diet:
- fried, fatty, salty and spicy foods;
- canned food and pickles;
- smoked meats;
- alcohol;
- strong tea and coffee;
- chocolate;
- products with any food additives (dyes, preservatives).
For this disease, it is useful to eat offal, chicken meat, walnuts, dairy products, egg yolk, vegetable oil, berries (especially black currants and raspberries), rose hips, and citrus fruits.
When treating erythema, the patient’s body must receive a sufficient amount of vitamin P, PP, E and C.
Fresh vegetables cleanse the intestines and reduce allergic reactions. These are root vegetables, onions, garlic, nightshades, legumes, spices (dill, basil, fennel, cumin). To normalize digestion during erythema, porridge and cereals are useful.
Complications and prevention
The main danger of erythema nodosum is the transition to a chronic form and complications of severe pathologies that caused the disease. Timely health care, adherence to diet and rest regimen reduces the risk of the disease and its complications.
Bad habits, such as drinking alcohol, smoking, and spending long periods of time at the computer, adversely affect emotional and mental health, which in turn reduces the body's defenses. At the first suspicion of the occurrence of an erythema nodosum rash, photos of which are presented on the website, you should immediately contact a specialist.
What it is
Erythema is a pronounced vascular reaction on the skin caused by a strong rush of blood to its surface.
This phenomenon can be physiological (natural), for example, appear on the face during severe emotional stress in adults or during prolonged crying in a child.
Erythema can also be a consequence of sunburn, trauma and scratching of the skin, or insect bites. Usually in such cases it does not require treatment. As soon as the provoking factor is eliminated, the redness on the body disappears.
Pathological erythema is caused by toxic effects on the body, endocrine disorders, bacterial, viral or fungal infections. Their symptoms and treatment vary depending on the type of disease.
The manifestations of erythema are very diverse, they vary from slight redness to the formation of large lesions, with thickening of the epidermis, nodular changes in peripheral vessels, profuse rash in the form of papules, pustules, plaques, roseola, blisters, etc.
Erythema nodosum in children
In infants, the appearance of erythema nodosum is often a consequence of the body's allergic response to intoxication with the causative agent of tuberculosis.
In older children and adolescents, the cause of the disease may be:
- staphylococcal or streptococcal infection;
- candidiasis;
- taking certain medications (antibiotics, iodine, sulfonamides and a number of others).
The clinical picture in children resembles the symptoms of erythema in adults. In addition to the above clinical signs, defecation disorder is added. Sometimes the nodules begin to soften and fester, but there will be no consequences from this. After some time they will dissolve without leaving a trace.
If erythema nodosum is suspected, children are advised to go to bed. Testing for tuberculosis is mandatory. If it is not detected, then antibiotic therapy is prescribed for 10-15 days.
For severe erythema with severe inflammation of the skin, glucocorticosteroids are used. In addition, the administration of vitamins B, C, A, calcium chloride and sodium salicylate is indicated.
Warm cotton bandages, compresses with ichthyol, and physiotherapy (UV irradiation, Sollux, microwave currents) are used as local treatment.
Children who have had erythema nodosum in infancy should be under medical supervision for six months after recovery.
Erythema nodosum chronic
Who successfully cured demodicosis
The term chronic erythema nodosum combines a number of forms of deep skin vasculitis, characterized by common etiological, pathogenetic, clinical and morphological signs.
Etiology and pathogenesis
insufficiently studied. Like the acute version, chronic erythema nodosum is an allergic vascular process of a polyetiological nature. In its pathogenesis, chronic focal infection (especially strepto- and staphylococcal) and previous infectious diseases are important. Occupational factors (working on your feet, in cold rooms, etc.) may play a certain role.
Clinic
. The main forms are nodular allergic vasculitis, migratory erythema nodosum, subacute migratory hypodermatitis. Manifestations of different forms can be observed sequentially at different times in the same patient or combined simultaneously.
Nodular allergic vasculitis
observed mainly in women 30-40 years old with good general condition. Soft, slightly painful nodes, ranging in size from beans to plums, form, most often on the outer surface of the legs, grouped along the superficial vessels. The skin over them is bluish-red, sometimes with symptoms of hypertrichosis. The nodes can exist for up to several months; they resolve without leaving a trace and without a “blooming” bruise, as happens with acute erythema nodosum. Relapses occur more often in the spring and summer over several years.
Erythema nodosum migrans
. This option is characterized by a longer (up to 1.5-3.5, sometimes even up to 10-11 months) subacute course and a tendency to relapse. The nodes are few in number, slightly painful on palpation, in most cases from the very beginning of the disease with a tendency to peripheral growth and resolution of infiltrates in the center. It affects the legs, feet, thighs, and rarely the torso and upper limbs. An asymmetrical arrangement of elements is often noted. Occasionally, instead of nodes, the formation of spots growing peripherally and resembling erysipeloid is observed. Some patients have low-grade fever and increased ESR; There are no arthralgias. Mostly women aged 30-40 years suffer.
Subacute migratory hypodermatitis
. Single small (the size of a pea or a cherry) dense nodes appear, located in the subcutaneous tissue of the anterior outer surface of the legs and the lower third of the thigh. They are not fused with the surrounding tissues, usually painless, the skin over them is not changed. Within one to several weeks, the nodes, increasing along the periphery, turn into flat, varying density (sometimes scleroderma-like) infiltrates up to 10-20 cm or more in diameter, which gradually, without sharp boundaries, pass into healthy tissue. The skin over the infiltrates also gradually acquires a red color of varying intensity. In some patients, hypertrichosis develops on the surface of the lesions. The general condition does not suffer, very rarely mild arthralgia is possible. The process is resolved within several weeks - three months without atrophy and scars. Women aged 20-30 almost always suffer.
Treatment
. Sanitation of foci of chronic infection, antibiotics, calcium preparations, vitamins C, P, E, non-steroidal antiphlogistics, in case of incomplete resolution of foci after the use of antibiotics - iodine preparations, in case of insufficient effectiveness of therapy - corticosteroids in small doses, dry heat.
B.D. Elkin
- Erythema rheumatica
- Erythrosis perioral pigmentosa
- All information on this issue
Principles of diagnosis
Often patients have a question about which doctor to contact for a woman or a man who is faced with such changes in the body.
Diagnosis depends on the cause of the disease and is often complex. It takes place with the participation of several specialists.
At the initial stage you will need:
- Donate blood and urine for general and biochemical analysis to the laboratory.
- Get examined by a therapist, check your blood pressure, do an ECG.
- Submit biological material for analysis and make sure that there are no hidden infections in the body.
The key is to palpate the nodules for pain and mobility. If required, the doctor gives a referral for an ultrasound examination of the formations in order to clarify their nature of appearance and characteristics.
The diagnosis will be carried out under the supervision of a doctor, and its direction will be determined by the doctor. He selects the necessary procedures that can help make the patient the correct diagnosis and prescribe treatment.
Treatment regimen
The success of treatment of erythema nodosum depends on the effectiveness of treatment of the disease that caused its development.
Patients with erythema nodosum are prescribed bed rest, and the affected limb must be elevated. To relieve pain and relieve inflammation, it is recommended to use non-steroidal drugs that have an anti-inflammatory effect.
Systemic glucocorticosteroids are quite effective, however, they should be prescribed with extreme caution, as they can negatively affect the course of the underlying disease.
If the underlying disease is infectious in nature, intensive antibiotic therapy is carried out. For general health, vitamins and angioprotectors are prescribed.
Local treatment for this disease consists of using physiotherapy methods - ultraviolet irradiation, UHF. Apply compresses using ichthyol ointment.
Patients are recommended to adhere to a hypoallergenic diet during treatment, abstaining from fatty, smoked and fried foods.
Erythema nodosum - treatment
How to treat erythema nodosum? In order for therapy to be effective, it is necessary to first find out the cause of the disease. Treatment may include both the use of medications and folk remedies.
Treatment with drugs
If the disease began against the background of an infection, then, depending on the type of pathogen, antifungal, antibacterial or antiviral drugs are prescribed.
If the cause of erythema has a non-infectious etiology, then the following groups of drugs can be prescribed:
- antiallergic drugs;
- corticosteroids;
- aminoquinoline drugs;
- NSAIDs.
Anti-inflammatory ointments are prescribed locally. Physiotherapy has a good effect.
Treatment with folk remedies
As mentioned above, for erythema nodosum it is possible to use traditional medicine. It should be remembered that they can only be used with the permission of the attending physician, strictly following his recommendations.
Below are several recipes that are used in the treatment of erythema:
- Take birch buds, blackberry, raspberry and plantain leaves, chop them and mix them in a 50:50 ratio with castor oil. After this, the mixture is simmered in a water bath for an hour, filtered, cooled and rubbed into the lesions twice a day.
- Take nettle leaves, chop them and pour a tablespoon of the mixture into a liter of boiling water. Leave for 15 minutes and pour the liquid into a filled warm bath, which must be taken for 15 minutes.
- For erythema nodosum, it is useful to take baths from a decoction of raspberry branches, linden flowers, willow and oak bark.
In conclusion, I would like to note that a timely visit to a doctor will help to start treatment on time and will not allow the disease to become chronic, in which a complete cure is almost impossible. However, the prognosis for the disease is favorable; erythema nodosum does not pose a threat to life.
Introduction to Basic Concepts
Erythema is a broad group of skin diseases in which there is an intense rush of blood to the capillaries. Erythema nodosum or erythema nodosum is a complicated form of these diseases in which pathological changes in the skin and fatty tissue are observed. The following photos are dedicated to erythema nodosum of the lower extremities.
What causes erythema nodosum? Causes
The causes of erythema nodosum can be very diverse. Most often, the disease appears under the influence of such factors:
- The appearance of the described erythema may indicate that a disease such as tuberculosis is beginning or progressing in the body.
- Also, with sarcoidosis and ulcerative colitis, erythema nodosum may appear.
- Another cause of the disease may be infectious diseases (coccidioidomycosis, histoplasmosis, and yersiniosis).
- In the same way, an inflammatory nodular process appears after taking certain medications. Because of them, an allergic reaction will begin, accompanied by erythema.
- With streptococcal infections (tonsillitis, scarlet fever), there is a possibility of the appearance of affected areas of the skin.
Methods of influence
Therapy depends on the cause of the disease and has several directions:
- Preference is given to antibiotics, they are able to “extinguish” the inflammatory process, without consequences for the body, rid a person of the manifestations of the disease.
- Since erythema nodosum is considered to be a consequence of an allergic reaction, antihistamines are prescribed. This is done by an allergist, but a therapist can also prescribe it.
- If there are problems with the immune system, then specific therapy is selected, including taking immunostimulants and immunosuppressants. This treatment is carried out with the participation of an immunologist.
- If the culprit is a disease of vascular origin, then medications are prescribed to improve blood flow in the lower extremities. So, for varicose veins and thrombosis, specific medications are prescribed, and wearing compression garments is recommended. A phlebologist treats the patient.
If the disease is a consequence of taking medications, then they are canceled or replaced with others. Which helps to easily relieve a person from health problems. This procedure is called therapy adjustment. It is carried out by a doctor who has previously been involved in prescribing medications.
Complex treatment is less commonly carried out; it includes the use of drugs that improve joint mobility, normalize blood flow in the extremities and eliminate pain.
It is not possible to choose medications and solve problems on your own. Such treatment will take time and cause serious complications.
Conclusion
Erythema nodosum is not a reason to panic, but rather a reason to go to the doctor and undergo a comprehensive examination. You should take the appearance of nodules as an alarming sign, but do not forget that competent treatment will correct the current situation and solve the problem as soon as possible.
Treatment with traditional methods
Since erythema nodosum is often accompanied by a decrease in immunity, it is recommended to use herbal treatment recipes aimed at generally strengthening the defenses.
- For erythema nodosum, it is useful to drink vitamin tea made from raspberry leaves, lingonberries, currants, and rose hips. You can add orange peels or a slice of lemon to your tea.
- A good result in the treatment of erythema nodosum is obtained by using horse chestnut leaves and sweet clover herb. Plant materials can be used individually or in a mixture. An infusion is prepared from the herb, which is taken up to four times a day, a quarter glass.
- Aloe leaves are an excellent remedy for erythema nodosum. A fresh leaf, freed from thorns and skin, is applied to the node and secured with a plaster. It is recommended to make such a compress at night. For oral administration, the leaves (without thorns) are ground in a blender, mixed with an equal amount of honey, and a few chopped walnut kernels are added. Take a dessert spoon before each meal.
Reasons for the development of the disease
Erythema nodosum is of an allergic nature, and the main causes of increased sensitivity of the body are infections, primarily streptococcal and tuberculosis.
Less commonly, a similar reaction is caused by lymphogranulomatosis, coccidioidomycosis, and trichophytosis. Sometimes erythema nodosum is caused by drug sensitization. Most often, the cause of an allergic reaction is antibiotics, bromides, iodides, salicylates, and sulfonamides.
Less commonly, the development of erythema nodosum is caused by non-infectious diseases - ulcerative colitis, ankylosing spondylitis. Often, a tendency to develop erythema nodosum is observed among blood relatives, that is, high sensitivity to infectious agents and medications is inherited.
The risk group for the development of erythema nodosum includes patients with various vascular diseases and vascular pathologies. For example, varicose veins.