Evgeny Zhilyaev says:
professor, doctor of medical sciences, doctor of the highest category.
Systemic scleroderma is a medical term for a group of connective tissue diseases that are characterized by damage to the skin, blood vessels and tissues of internal organs.
Causes and mechanisms of development of systemic scleroderma
The exact causes of systemic scleroderma have not been established today. Scientists suggest that the disease develops under the influence of many external and internal factors combined with a genetic predisposition to the disease. Along with the role of infection, vibration, cooling, stress, injury and endocrine disorders, special attention is paid to the effects of chemical agents (household, nutritional, industrial) and certain medications.
The central links in the mechanism of development of systemic scleroderma are excessive fibrosis, disorders of the immune system and microcirculation. An imbalance of cellular and humoral immunity leads to activation of the production of specific antinuclear antibodies, interleukins (mediators of inflammation and immunity), antibodies to the endothelium and connective tissue.
In the inner layer of the vascular wall, the number of smooth muscle cells increases and mucoid swelling occurs. The lumen of the vessels narrows, microthrombosis develops. Over time, blood supply to tissues decreases. The degree of endothelial damage is indicated by an increase in the concentration of von Willebrand factor and cellular soluble adhesion molecules.
T-lymphocytes and fibroblasts accumulate in the dermis (the skin itself). They overproduce collagen types I and III. Activated mast cells produce transforming growth factor B and histamine. This stimulates the proliferation of fibroblasts and the formation of components of the intercellular matrix.
Description
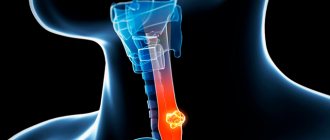
Systemic scleroderma.
Diffuse pathology of connective tissue, which is characterized by fibrous-sclerotic changes in the skin, joints and muscles, internal organs and blood vessels. Typical signs of systemic scleroderma are Raynaud's syndrome, skin thickening, mask-like face, telangiectasia, polymyositis, joint contractures, changes in the esophagus, heart, lungs, and kidneys. Diagnosis of systemic scleroderma is based on a set of clinical data, determination of scleroderma autoantibodies, and skin biopsy. Treatment includes antifibrotic, anti-inflammatory, immunosuppressive, vascular agents, and symptomatic therapy.
Types of systemic scleroderma
There are diffuse and limited clinical forms of systemic scleroderma. In 2% of cases, scleroderma without scleroderma is registered (damage to internal organs only). There are cross-forms of the disease in which systemic scleroderma is combined with rheumatoid arthritis, inflammatory myopathies, and systemic lupus erythematosus).
The following variants of the clinical course of scleroderma are distinguished:
- Acute, rapidly progressive course - generalized fibrosis of the skin (diffuse form) and internal organs develops during the first two years from the onset of the disease;
- Subacute, moderately progressive course - there are clinical and laboratory signs of immune inflammation (dense swelling of the skin, myositis, arthritis), there may be cross-syndromes;
- Chronic, slowly progressive course - vascular pathology predominates; at the beginning of the disease, Raynaud's syndrome is observed for a long time, then the skin and internal organs are gradually affected.
Prevention
To prevent exacerbation of systemic sclerosis, it is recommended to follow certain measures:
- Give up bad habits - smoking, caffeine abuse and medications that cause vasospasm.
Try to avoid cold and vibrations, wear warm clothes.- Eliminate psycho-emotional overload.
- If the gastrointestinal tract is affected, follow small meals, excluding fatty foods and drinking alcoholic beverages.
- Get a good night's sleep on a raised bed at the head end.
- Regular examination by a doctor once every six months.
- Do not change the dosage of prescribed medications on your own without consulting your doctor.
- Perform physical therapy, conduct massage courses.
- Try to spend more time outdoors.
Symptoms of systemic scleroderma
The clinical picture of systemic scleroderma includes a wide range of manifestations. It is characterized by polymorphism in terms of symptoms, severity and prognosis of the disease. One of the first symptoms of systemic scleroderma is a syndrome of symmetrical paroxysmal spasm of arteries, precapillary arterioles, cutaneous arteriovenous anastomoses under the influence of cold and emotional stress.
Skin lesions in systemic scleroderma are characterized by stages. In the initial stages of the disease, dense swelling of the skin and underlying tissues occurs. Due to swelling of the fingers, the hand is difficult to clench into a fist in the morning. Sometimes diffuse hyperpigmentation develops at the onset of the disease.
As the disease progresses, skin induration occurs - an increase in density and a decrease in elasticity. The skin can hardly be gathered into a fold. It is much thicker than normal skin. At the atrophy stage, the skin acquires a bluish-brown color due to hyperpigmentation and dyspigmentation, and becomes thinner. It has a characteristic shine. The skin becomes rough, dry, hair disappears. Small subcutaneous and intradermal deposits of calcium salts may appear in soft tissues. If they open, a cheesy mass is released and long-term non-healing ulcers are formed.
In the advanced stage of the disease, the “purse string” symptom appears - when radial folds form around the mouth. Late signs of systemic scleroderma are telangiectasia - dilated venules and capillaries grouped in a bundle. The number of telangiectasias increases over time. They are located on the hands, face, and décolleté. These symptoms of systemic scleroderma are visible in the photo.
Damage to the musculoskeletal system is manifested by polyarthralgia; polyarthritis with severe synovitis and tenosynovitis may develop. In the chronic course of systemic scleroderma, sclerosing tenosynovitis and damage to other tissues located around the joints predominate. These processes, together with skin thickening, lead to the formation of sclerodactyly (local thickening and hardening of the skin of the fingers), flexion contractures of small and large joints. A typical manifestation of systemic scleroderma is acroosteolysis - resorption of the terminal sections of the terminal phalanges of the hands due to prolonged ischemia.
The manifestations of scleroderma are the following lesions of internal organs:
- Hypotension of the esophagus;
- Erosion and ulcers of the esophagus;
- Damage to the small and large intestines;
- Malabsorption syndrome;
- Interstitial lung disease;
- Pulmonary hypertension;
- Acute or chronic nephropathy.
With scleroderma damage to the heart, fibrosis develops involving both ventricles. In patients, the balance of the immune system is disturbed, autoimmune disorders occur with the formation of antinuclear antibodies. Almost all patients have antinuclear factor.
The most important blood test for systemic scleroderma is the detection of anticentromere antibodies (ACAs), antibodies to topoisomerase 1 (Scl-70) and to RNA polymerase III. All of these autoantibodies are directed to soluble nuclear proteins. Autoantibodies in systemic scleroderma appear already at the preclinical stage. Each person with systemic scleroderma usually has only one type of autoantibody, which does not change as the disease progresses.
What is fiber sarcoidosis?
Fiber sarcoidosis is a chronic non-infectious disease that primarily affects the skin and lungs.
In rare cases, the disease is accompanied by ulcers, psoriasis-like changes, baldness and nail damage. In a chronic course, pathological processes in the skin lead to disfigurement of a person.
The pathological process includes 3 parts:
- Damage to small vessels.
- Changes in tissues and cells.
- Dysfunction of connective tissue, which leads to its excessive deposition in tissues and organs.
Diagnosis of systemic scleroderma
Rheumatologists at the Yusupov Hospital make a diagnosis of systemic scleroderma based on the clinical picture of the disease, data from instrumental and laboratory studies, which allow one to assess the degree of involvement of internal organs in the pathological process and the severity of pulmonary hypertension. For this purpose, I use the following research methods:
- Electrocardiography;
- Echocardiography;
- Six-minute walking test;
- X-ray and computed tomography of the chest;
- Spirometry;
- Body plethysmography;
- Ventilation-perfusion lung scintigraphy;
- Angiopulmonography.
If indicated, catheterization of the right heart is performed. Patients are prescribed a clinical, biochemical, immunological blood test, and a coagulogram. In a general blood test for systemic scleroderma, an increase in the erythrocyte sedimentation rate, a change in the amount of hemoglobin and red blood cells can be detected. A general urine test reveals hyposthenuria (decreased urine density), proteinuria (protein in the urine), decreased specific gravity of urine, and casts. A biochemical blood test includes determination of the level of AlT, AST, total protein and fractions, glucose, creatinine, urea, and cholesterol. In the blood of a patient suffering from systemic scleroderma, an increase in the titer of the following antibodies is detected:
- Antinuclear;
- Anticentromeric;
- To topoisomerase-1 (Scl-70).
Rheumatologists use clinical guidelines from the American Rheumatological Association to make a diagnosis of systemic scleroderma. The “major” criterion is proximal scleroderma. It is characterized by symmetrical thickening, thickening, and induration of the skin proximal to the metacarpophalangeal and metatarsophalangeal joints. Changes characteristic of scleroderma can be located on the neck, face, chest, and abdomen. “Minor” criteria include sclerodactyly (the skin changes listed above are limited to the fingers), small scars on the fingertips or loss of fingertip tissue, and bilateral basal pneumofibrosis on radiographic examination. The diagnosis of systemic scleroderma is established in the presence of a “major” criterion or two “minor” criteria. Rheumatologists use these criteria to identify severe systemic scleroderma. They do not cover early limited, crossed and visceral systemic scleroderma.
Classification and forms
There are several types of limited scleroderma. They mainly differ from each other in the localization and shape of the spots, but, in general, they do not pose a threat to life.
- The most common form is plaque scleroderma. It got its name from the characteristic round or oval shape of the spots. Their size can vary quite widely - from 2 to 15 cm.
- The spot at the first stage has a purple-red hue due to the inflammatory reaction. Later, the plaques become yellow or grayish, acquire shine and high density - like “wooden”. A lilac ring is held around the spot. Spots can appear on any part of the body, including the scalp.
- At the next stage, the hairs on the plaque fall out, the sebaceous glands disappear, and the skin completely loses its elasticity, which is caused by collagen hypertrophy. Then the lilac ring disappears and the plaque resolves.
- The third stage, as a rule, is marked by atrophy of the skin in the damaged area: it becomes thin and acquires a characteristic parchment color. However, there are often cases when the plaque form resolves without leaving a trace and heals spontaneously.
- Ribbon or strip - has a clear localization. The disease manifests itself in the form of a line running from the scalp above the forehead to the tip of the nose, as if dividing the face in two, a vertical strip along the chest or along the nerve trunk - the Ged zone. This form is specific and indicates that scleroderma has affected the nerve endings. Quite often, the appearance of such a stripe precedes the atrophy of half the face. Most often, the strip-like form is observed in children.
- “White spot” disease – the lesions look like small spots – up to 1 cm in diameter, white, bordered by a red-brown rim. The spots are grouped and have a shiny surface. Their color is always lighter than the color of the skin or mucous membranes. The plaque may rise above the skin or sink, which serves as a distinctive sign of the disease during diagnosis - lichen has the same shape and color. Plaques can appear in the mouth, on the genitals, on the chest, shoulders and neck. Other localizations are rare.
- Superficial is the mildest form of the disease. It is characterized by the formation of small spots of a gray-brown hue. The plaques do not have a clear boundary and are located slightly below the skin level. Spots usually appear on the back and legs. This form of the disease practically does not progress. The surface of such a plaque is dense, but in the center the skin becomes so thin that small blood vessels are visible. The likelihood of skin damage is very high, which, however, does not lead to the development of the disease or complications.
- Romberg's hemiatrophy of the face is noticeably different in symptoms from other types, but also refers to limited scleroderma. The disease usually appears before the age of 20; women and men suffer from it equally often. In this case, the skin of the face is damaged, and the subcutaneous tissue is immediately involved in inflammation. Spots form on the cheekbones, around the eyes, near the lower jaw; in these areas there is increased activity of the sweat and sebaceous glands. The sclerotic stage in this case is essentially absent, but hemiatrophy leads to severe neuralgic pain. Following skin atrophy comes muscle atrophy. Because of this, the face loses symmetry, proportions and sizes are distorted. Hair, eyelashes and eyebrows fall out.
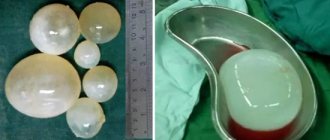
- Bullous - also refers to focal. In this case, in addition to connective tissue, lymphatic vessels are affected. The disease is characterized by the appearance of blisters on the surface of the skin along with other sclerotic foci.
Treatment of systemic scleroderma
Rheumatologists for systemic scleroderma prescribe drugs with an antifibrotic effect in combination with arterial vasodilators, antiplatelet agents, cytostatic and anti-inflammatory drugs. B-penicillamine (cuprenil) is the most effective among the group of antifibrotic agents. Nonsteroidal anti-inflammatory drugs and glucocorticosteroids are used.
Nonsteroidal anti-inflammatory drugs are prescribed for the treatment of muscular-articular manifestations of systemic scleroderma and low-grade fever. Glucocorticosteroids are used according to indications, taking into account their effect on the cellular and humoral components of inflammation, as well as on fibroblasts.
In the treatment of complex therapy of pulmonary hypertension in systemic scleroderma, oxygen therapy, vasodilators and angiotensin-converting enzyme inhibitors are effective. Calcium channel blockers dilate blood vessels, which leads to a decrease in pulmonary artery pressure. Prostacyclin is a powerful endogenous vasodilator. It also has antiaggregation, cytoprotective and antiproliferative effects. Alprostadil is also used intravenously to treat patients with pulmonary hypertension. Treatment is often combined with long-term use of calcium channel blockers. Vasodilators are prescribed together with antiplatelet agents and angioprotectors.
In the chronic course of systemic scleroderma, hyaluronidase preparations have a positive effect. They are prescribed in the form of courses of intramuscular or subcutaneous injections, electrophoresis or applications to the area of contractures and inductively altered tissues. With the progression of pulmonary fibrosis and the development of severe respiratory failure, scleroderma renal crisis, and the development of severe heart failure, treatment is carried out in the intensive care unit.
To prevent the development of systemic scleroderma, doctors recommend avoiding emotional stress, prolonged exposure to cold, smoking, and drinking coffee and drinks that contain caffeine.
People often ask the question: “How many people live with symptoms of systemic scleroderma?” The prognosis depends on the form of the disease, course, severity of damage to internal organs and the adequacy of therapy. If you have the first signs of illness, call the contact center.
Treatment of patients with systemic scleroderma at the Yusupov Hospital is carried out by rheumatologists. In case of development of dysfunctions of internal organs, specialists from other medical specialties (cardiologists, nephrologists, pulmonologists, gastroenterologists) are involved in the treatment process. Severe cases of the disease are discussed at a meeting of the Expert Council with the participation of professors, associate professors and doctors of the highest category. Leading rheumatologists specializing in the treatment of systemic diseases collectively determine further tactics for patient management.
Author
Liliya Rashitovna Garayeva
Obstetrician-oncogynecologist, candidate of medical sciences, doctor of the highest category
Treatment during pregnancy
Faced with scleroderma and pregnancy at the same time, every woman wonders what to do now.
There is currently no safe way to treat this disease during pregnancy. Therefore, it is important that medications are prescribed only by a doctor and in cases of extreme necessity.
Self-medication and the use of folk remedies are excluded in this situation.
If the treatment of scleroderma occurs during pregnancy planning, then it is worth postponing the treatment until it is cured.
This is due to the fact that many drugs cause congenital pathologies and fetal development defects. During pregnancy, special attention is paid to the treatment of systemic scleroderma, since it can cause significant harm to both the body of the mother and the child.
To treat it, drugs such as:
- Medicines that lower blood pressure;
- Medicines to help cope with heartburn;
- Corticosteroid drugs that reduce the manifestations of the disease;
- Medicines that suppress the immune system.
Pregnant women who suffer from scleroderma disease, in addition to a gynecologist, must be observed by the following doctors:
- Dermatologist;
- Cardiologist;
- Pulmonologist;
- Gastroenterologist;
- Nephrologist.
Causes
The cause of the disease is unknown. Provoking factors may include the following:
- hypothermia is a very common cause, since scleroderma forms more quickly in areas with damaged or traumatized skin;
- disorder in the functioning of the endocrine system;
- the cause may be vaccination or blood transfusion - the entry of a “foreign” protein into the body often causes an allergic reaction, and then a change in the connective tissue;
- A number of external factors can also provoke the disease: silicon dust, if the patient is constantly in contact with it, vibration that accompanies the workload, vapors of certain organic solvents;
- in some cases, medications were the provoking factor.
The effectiveness of traditional methods of treatment
Non-traditional remedies help if other methods of treatment are carried out and are an integral but auxiliary part of complex therapy.
Ointments for focal form
A common method of treatment is the use of ichthyol ointment with the addition of aloe juice.
When applying the drug to the steamed dermis, the therapeutic effect is more pronounced.
The most unexpected means are used to prepare ointments - for example:
- baked onion;
- honey;
- kefir.
To prepare, mix honey, baked onion, grated on a sieve, and Vaseline in equal proportions. Mix everything and store in the refrigerator, applying cloth overlays to the affected area for 2-3 hours a day.
Traditional methods of treatment for children
In childhood, an ointment made from visceral fat with the addition of wormwood extract helps well, but long-term use is necessary for a pronounced effect.
How is skin scleroderma treated?
Therapeutic tactics depend on the stage and form of the disease. There are developed treatment protocols, to which the necessary adjustments are made when additional symptoms are detected or existing symptoms intensify.
Long-term antifibrotic drugs
There are basic drugs like cuprenil (D-penicillamine), diucifon, colchicine that can suppress excess collagen synthesis caused by autoimmune pathology. They become the main method of treating scleroderma, because they are able to bind and remove copper from the body, as the main inhibitor of collagenosis.
Massage
Massage is one of the recommended methods of physiotherapy, a way to soften scar tissue and restore the functionality of joints and skin.
Electrophoresis
Electrophoresis is used to introduce medications that have an enzymatic, absorbable or anti-inflammatory effect into the affected tissues.
Laser therapy
It is prescribed for physical treatment for many types of scleroderma, however, as with vacuum compression and magnetic therapy, high activity of the pathological process and some types of systemic lesions can be an obstacle.
Acupuncture
Sometimes it is recommended as a method of treatment, but such courses require the help of a qualified specialist.
Hydrogen sulfide and carbon dioxide baths
The leading method of balneotherapy, used as a means of sanatorium-resort consolidation of achieved results. It is considered effective if prescribed taking into account the characteristics of the disease and contraindications. Self-medication of pathology is considered unacceptable.
Forecast
Limited scleroderma has a very favorable prognosis if all recommendations are followed, of course. The disease cannot be ignored. Unfortunately, it is impossible to eliminate areas of scar tissue that have already appeared, but it is quite possible to prevent the appearance of new ones and prevent its formation in the future.
Limited scleroderma is an inflammatory skin disease of an autoimmune nature. The exact causes of the disease are not yet known, but its localized form is treatable and is not life-threatening.
What drugs are used to treat systemic sclerosis?
Antibiotics:
- penicillins,
- fusidine sodium - 500 mg three times a day for 2-3 weeks;
- cuprenil - 150 mg per day, the dose is gradually increased to 1500-1800 mg per day, and after 2 weeks - gradually reduced to 300-600 mg per day, treatment duration - 2-3 years.
Corticosteroids:
- prednisolone - 30-40 mg per day for 2-4 weeks with a gradual dose reduction. A
Anticoagulants:
- Complamin - intramuscularly, at a dose of 0.3-0.6 g 1-3 times a day;
- mydocalm - starting with 50 mg 2-3 times a day, gradually increasing the dose to 150 mg 2-3 times a day;
- doxium - prescribed individually;
- heparin - prescribed individually.
NSAIDs:
- indomethacin - 25 mg 2-3 times a day, if necessary, the daily dose can be increased to 100 mg, divided into 4 doses;
- naproxen - at the beginning of treatment and in acute conditions, 500-1000 mg per day in 2 divided doses (morning and evening), the maintenance dose is 500 mg per day in 1 or 2 divided doses;
- diclofenac sodium - 25-50 mg 2-3 times a day.
Antimalarial:
- delagil - prescribed individually;
- Plaquenil - minimum effective doses are indicated, not exceeding 6.5 mg/kg per day (calculated based on “ideal” rather than actual body weight) and can be either 200 or 400 mg per day.
At-risk groups
The focal type of scleroderma develops more often in women, and this is due to the individual characteristics of the body:
- The activity of cellular immunity in women is less pronounced;
- Immunoglobulins, on the contrary, are more actively produced;
- The influence of sex hormones on blood circulation in the skin is higher than in men.
Also at risk include:
- Representatives of the Negroid race;
- People who suffer from other types of autoimmune diseases;
- Builders;
- Those who have close relatives with any autoimmune diseases;
- Sellers who work in open markets in winter;
- People who regularly interact with refrigeration units and freezers;
- Food storage guards;
- People in contact with chemicals;
- Those who are regularly exposed to cold.
Contraindications for scleroderma
The disease imposes its restrictions on the lifestyle of patients. Physical therapy exercises and feasible physical activity are recommended for all patients to prevent congestion and improve blood circulation. Intense physical activity should be avoided. Contraindications for scleroderma are some cosmetic procedures that can cause an exacerbation of the disease: plasma lifting (treatment with your own platelet-rich plasma), biorevitalization (introduction of hyaluronic acid).
Classification of focal scleroderma
There is a classification of pathology that was developed by S.I. Dovzhansky, it is most often used in medicine:
- White spot disease , also called guttate scleroderma.
- Linear. It has three varieties: “saber strike”, zosteriform and stripe.
- Pasini-Pierini disease ( superficial large patchy skin atrophy with hyperpigmentation )
- Plaque. There are the following varieties: deep, superficial, indurative-atrophic, bullous, nodular, generalized.
- Parry-Romberg syndrome.