Main pathologies of the female breast: types and forms
Symptoms of breast diseases in women depend on the specific disease. The international classifier identifies several categories of breast pathology:
- a group of benign dysplasias (adenosis and its sclerosing form, fibrous and cystic mastopathy, a mixed version of the disease);
- hypertrophy of glandular tissue;
- malignant neoplasms;
- inflammation;
- unrefined neoplasms and other pathologies;
- anomalies (absence of the pectoral muscle or gland/accessory gland, absence of the nipple/accessory nipple, unrefined and other anomalies).
This classification is convenient in that it allows us to identify the leading symptoms for each group. But it is not informative for patients. Because the diagnosis written by the doctor on the card will be more precise. For example:
- adenoma;
- atrophy;
- papillary tumor;
- galactorrhea (outside labor);
- nodular/diffuse mastopathy;
- fat necrosis;
- invasive ductal carcinoma;
- cyst;
- lactostasis;
- mastitis;
- mammalgia;
- mycoses (actino-, candidomycosis);
- hereditary cancer;
- anomalies;
- cancer tumor;
- Paget's disease;
- fistula;
- syphilis of the mammary glands;
- cracked nipples;
- injuries;
- mammary tuberculosis;
- fibrolipoma;
- fibroma, including leaf-shaped.
These are the main diseases that affect the female bust. The reasons for the development of many pathologies have not been fully determined. Exceptions are infectious and inflammatory pathologies for which the causative agent is known (for example, actinomycosis, candidiasis, tuberculosis, herpes virus or mastitis), mammary gland injuries, fistulas and cracked nipples.
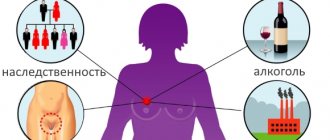
The causes of other pathologies may be a genetic predisposition stimulated by unfavorable factors:
- disturbances in the production of hormones, associated diseases of the female sphere (including STDs) or pituitary disorders;
- bad habits;
- inactive/hyperactive sex life;
- frequent termination of pregnancies or lack thereof;
- neglect of breastfeeding;
- late pregnancy and childbirth;
- environmental problems in the place of residence;
- industrial hazards;
- poor diet;
- consumption of milk from cattle affected by viral leukemia.
And there are many more known and unknown factors that can cause the transformation of normal bust cells into pathological ones.
Causes
A common cause of mastitis during lactation is infection with Staphylococcus aureus. Less commonly, pathology is caused by streptococcus, fungi and E. coli. The infection enters the milk ducts through the blood or lymph flow if there is an inflammatory focus in the body (dental caries, sore throat, sinusitis, cystitis, tonsillitis, etc.). Pathogenic microorganisms can also penetrate from the external environment. Often, mastitis covers a large area of the breast (several lobes), which is due to active blood flow and the rapid spread of infection.
The presence of cracks in the chest and non-compliance with personal hygiene rules increases the risk of developing pathology. Often the cause of mastitis is lactostasis: the mammary glands produce more milk than the baby needs, which provokes stagnation.
The pathology develops mainly in primiparous women. This is due to the fact that the breasts and milk ducts are not sufficiently prepared for lactation.
A history of mastopathy, cystic and tumor formations in the mammary glands, hypothermia and reduced immunity increase the risk of developing lactation mastitis. The provoking factor is the mother’s lack of proper rest, frequent stress, emotional distress and overwork.
Signs of benign dysplasia
This is a whole group of pathological processes in the glandular tissue of the breast, which are characterized by:
- proliferation;
- regression of glands;
- tissue imbalance: epithelial/connective.
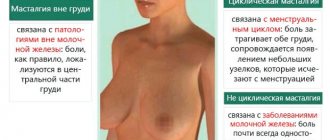
The main symptom for this group of pathologies is pain that intensifies before or during menstruation and decreases until it disappears completely after bleeding. Pain syndrome can be:
- intense;
- medium-intensive;
- unbearable.
The pain is localized most often in both glands, less often in one gland, sometimes radiating to the armpit, shoulder, under the scapula, simulating signs of a heart attack. When palpated in the tissues of the gland, compactions may be felt.
Changes in the size of the mammary glands or their shape occur only in the advanced stage of the disease. At the same time, during menstruation, the nipples become hard, the breasts increase in volume (fill out). Light, translucent discharge from the nipple may appear.
At the initial stage of the disease, treatment is conservative; at later stages, surgery may be suggested.
Symptoms
The first signs of inflammation of the mammary gland appear at the early stage of the disease - serous. Its symptoms are:
- enlargement and thickening of the mammary gland;
- soreness and feeling of fullness of the breasts, which do not disappear (and sometimes intensify) after feeding the baby and expressing milk;
- increase in body temperature up to 380C.
Lack of treatment leads to the fact that the woman’s condition sharply worsens, and the symptoms increase:
- temperature rises above 390C;
- upon palpation, an inflammatory compaction is felt in the depths of the gland - infiltration;
- the skin over the area of inflammation turns red;
- migraines and severe weakness appear.
With ineffective treatment of the infiltrative form of mastitis, the disease turns into a purulent form with the formation of an abscess, the symptoms of which become threatening:
- the breasts significantly increase in size, swell, there is severe redness and pain;
- body temperature reaches 400C and above, often it changes abruptly: it drops sharply with profuse sweating, then rises again to high numbers;
- symptoms of intoxication increase: nausea, vomiting, severe headaches;
- Regional lymph nodes enlarge.
In the phlegmonous and gangrenous form of mastitis, infection spreads to the entire area of the gland. The symptoms of the purulent form are complemented by:
- persistent increase in heart rate to 120-130 beats per minute;
- the entire breast becomes hard and sharply painful;
- the appearance of a purplish-bluish tint of the skin of the chest (with phlegmon), then the appearance of blisters with bloody contents (with gangrene) - tissue necrosis.
The woman's health and life are in serious danger - only urgent surgical intervention can save her.
The clinical picture of the chronic form of inflammation of the mammary gland is not clearly expressed:
- the breasts are slightly enlarged in size, moderately painful;
- low-grade fever (up to 37.80C);
- to the touch a dense infiltrate is detected in the area of the gland;
- the lymph nodes are slightly swollen;
- the general condition of the woman was slightly disturbed.
Mastitis usually develops in one mammary gland, less often in both (10% of women).
Signs of hypertrophy
Hypertrophy or excessive growth of glandular tissue, in some cases together with the growth of fat cells, can be congenital or acquired. There are three stages of hypertrophy from a slight increase in the bust to a change in volume by 8-10 sizes with the development of pronounced mastoptosis. Main symptoms of the pathology:
- noticeable change in bust size;
- back pain, development of osteochondrosis, in the case of unilateral hypertrophy - scoliosis;
- discomfort during active exercise;
- increased fatigue;
- difficulty breathing;
- discomfort during sleep.
Treatment is mainly surgical:
- mastopexy;
- reduction mammoplasty;
- restoration of the position of the nipple and areola.
When diagnosing the disease in teenage girls, mammologists try to resolve the issue using conservative methods. And only after reaching 18 years of age can such patients be offered a surgical solution.
How to treat mastitis
You should not delay the treatment of mastitis; it is better to contact a mammologist as soon as the nursing mother feels something is wrong. After all, the sooner you provide help during the development of the disease, the faster the recovery stage will begin, and the lesser the risk of complications will appear. Treatment of mastitis in a medical institution is especially important if the disease has been going on for a couple of days and there is no improvement.
First aid
First you need to try to eliminate the stagnation of the ducts. Frequent latching of the baby will help with this, because nothing will achieve complete emptying of the breast better than the natural process of feeding. Establishing lactation will lead to a speedy recovery. In order for the baby to completely and quickly eliminate congestion, you need to point his head with his chin towards the affected area. At the same time, you should remain calm, relax as much as possible, and devote time to yourself and your baby.
Treatment of mastitis without surgery
No woman wants to be away from her baby for a long time, much less interrupt feeding. But if there is a risk of ending up on the operating table, then the nursing mother must first do everything possible, including using medications, to prevent such a development of events. take antibiotics for mastitis if:
- signs of illness do not go away within 24 hours,
- the situation does not change, but the painful sensations remain as they are throughout the day,
- During the first 12 hours, the woman’s condition deteriorates sharply.
But only a doctor should prescribe treatment; you should not take antibiotics without permission while breastfeeding. You can harm not only yourself, but also your child. Antibacterial agents that fight Staphylococcus aureus are considered an effective method of treatment. There are drugs such as:
, Amoxiclav,
, Cephalexin,
, Ciprofloxacin and others.
At the same time, there are drugs that do not affect the baby, so the mother can continue breastfeeding, even resorting to such drugs. But only if the attending physician agrees with this decision.
During and before breastfeeding, a nursing woman suffering from milk stagnation would benefit from self-massage. Massage for mastitis is carried out with light movements, directing the flow of milk from the edge of the breast to the nipple. If cracks or abrasions have already formed on the nipples, then in order to avoid infection, it is worth additionally treating the breasts with healing agents. For example, they use Bepanten, a wound-healing ointment for mastitis.
Physiotherapy for mastitis is considered a fairly effective method of treatment . In this case, all kinds of compresses, UHF and heating pads are used. This method, supplemented with massage, improves blood circulation, relieves pain and relieves swelling. Sometimes, even an ultrasound procedure can affect the seals and “break” the ducts a little.
Surgery for mastitis
In a particularly difficult situation, with purulent mastitis, it is extremely difficult to do without surgery. A minimal intervention is considered to be only a puncture to examine purulent formations, then antibiotics are injected directly into the mammary tissue. The situation is more complicated if you have to resort to drainage. Then the affected breast is opened and the canals are cleaned, while supplementing the treatment with the same antibiotics.
If it comes to surgery, then, unfortunately, you will most likely have to forget about continuing to breastfeed the baby naturally.
Because physically, breastfeeding after surgery is very painful. Expressing is also practically impossible, so medication is often used to complete lactation.
Traditional methods of treating mastitis
If the process of developing the disease is not too advanced, then it is possible to try treating mastitis at home. But it is better to discuss prescriptions for such medications with a mammologist, because there are cases when, for example, heating can only harm a nursing mother. Often young mothers use the following procedures:
- Compresses with rice starch. Dilute the powder with water until a semi-liquid state is formed (like sour cream), apply to the chest, and leave for some time. Such lotions ease the physical condition of a woman, relieving pain.
- Fresh vegetables or plants. Cabbage leaves or coltsfoot, or grated carrots help relieve breast condition. The ingredients are applied to the chest, fixed with a towel or bandage, and held until the discomfort is relieved.
- Natural mixtures of herbs, oils and other plants will also improve the condition of a nursing mother with mastitis. Narcissus bulb plus pureed rice gruel, or rye flour plus milk with the addition of butter, cakes are prepared from these products and applied to the chest.
- Infusions, herbal decoctions, which are used both internally and in the form of compresses. For example, a mixture of licorice and tangerine peels is mixed with boiling water, infused and drunk throughout the day.
- Rubbing or alcohol lotions.
- Warm drink. Herbal teas or vitamin teas will help the body from the inside, for example, a decoction of mint, sage, rose hips (fruits), and viburnum.
Signs of malignant neoplasms
The symptom that usually sends us to the hospital is pain. With these diseases, pain begins only in the later stages of the disease, sometimes at the time of tumor disintegration. That is, when any treatment gives a minimum of results and causes maximum harm to the body. Therefore, it is important to regularly conduct self-examinations and palpation of the breast, paying attention to the following symptoms:
- the appearance of compactions;
- immobility of the node/adhesion with surrounding tissues;
- change in shape/size of the areola;
- disturbances in the nipple area (its retraction, formation of cracks, ulcers, wounds, scabs);
- changes in the skin over the seal (hyperemia, peeling, ulceration, formation of lemon peel and other disorders);
- enlargement of the gland, deformation;
- discharge from the nipple (from clear to bloody);
- rapid growth of formations without clear boundaries.
Even if painless lumps appear that are not prone to growth, you should visit a mammologist. As you age, your likelihood of developing cancer increases. After 60 years of age, malignant oncology in the breast area in women is 400 times more common than the number of sick girls aged 20 years.
With this pathology, the surgeon’s scalpel comes to the aid of patients, sectoral resection of the mammary glands and mastectomy are performed.
Treatment and prevention
Nursing mothers should follow measures to prevent lactation mastitis. Even before the birth of the baby, the expectant mother should attend courses for pregnant women, where she will be told how to properly attach the baby to the breast to avoid cracks.
Particular attention should be paid to personal hygiene. Take a shower every day, change your underwear, and don’t forget about physical activity. Wash your hands thoroughly before each feeding. There is an opinion that it is also necessary to wash your breasts with warm water and soap every time. However, this can compromise the protective layer of skin and only increase the likelihood of cracked nipples. Therefore, it makes sense to limit yourself to a daily shower.
After feeding, you should take air baths for 10-15 minutes. If cracks do appear on the nipples, they are lubricated with Bepanten cream or ointment and treated with Panthenol spray. Products containing lanolin also speed up healing. It is better to stop feeding until the cracks are completely healed, as they become deeper during sucking.
Milk should be carefully expressed and fed to the baby from a spoon. If the cracks are shallow, you can try using silicone nipple covers
They will help minimize the impact on the damaged breast during breastfeeding. If the first symptoms of mastitis occur, you should immediately consult a doctor who will prescribe treatment. Each stage requires a special approach.
Breastfeeding in the initial stages can be continued, this will help alleviate the woman’s condition. But any decision related to the continuation of lactation should be discussed with a doctor. He will also select medications approved for nursing mothers. If the abscess stage of mastitis has begun, it is necessary to stop breastfeeding until the end of treatment. To maintain lactation, you can use a breast pump.
In severe cases, lactation should be stopped. Special medications, for example Parlodel, can help with this. It reduces the production of the hormone responsible for milk production, prolactin. When treating this disease, it is necessary to use antibacterial drugs. To combat serous or infiltrative mastitis, antistaphylococcal drugs (oxacillin, lincomycin, dicloxacillin, methicillin, fusidine) are used.
At the stage of abscess and phlegmonous mastitis, the following is prescribed to destroy the anaerobic flora:
- chloramphenicol;
- lincomycin;
- rifampicin;
- clindamycin;
- erythromycin;
- rifampicin;
- metronidazo;
- benzylpenicillin.
Simultaneously with the use of antibacterial drugs, measures are taken to strengthen the immune system.
To increase the body's resistance, intramuscular injections of antistaphylococcal gamma globulin are used, toxoid and antistaphylococcal plasma are also prescribed. Women with intoxication require infusion therapy. They are prescribed:
- polypher;
- rheopolyglucin;
- polyglucin;
- rheomacrodex;
- sodium bicarbonate solutions;
- glucose;
- potassium chloride;
- sodium chloride.
Treatment of lactation mastitis should include taking antihistamines. Diphenhydramine, suprastin, and diprazine may be prescribed. Physical methods are also used in treatment, such as ultraviolet radiation, microwave therapy, and ultrasound. At the stage of serous and infiltrative mastitis, ultrasound or microwave therapy in the centimeter or decimeter range is used.
Abscess and phlegmanous mastitis require mandatory surgical intervention. Opening of purulent blisters occurs in stationary conditions. After this, laser therapy and intravascular ultraviolet radiation are used.
The health of a nursing mother requires special care and attention. If a woman follows all the recommendations of doctors regarding the organization of breastfeeding, she will be able to avoid such troubles as lactostasis and mastitis. And if treatment begins at the first signs of the disease, then soon you will again be able to enjoy all the joys of motherhood without suffering from the consequences of mastitis.
Mastitis: main signs
Inflammation in the area of the mammary glands is often associated with postpartum lactostasis; less often, it can develop after injury, hypothermia of the gland, or penetration of an infectious agent. Characteristic symptoms for this disease are:
- local temperature;
- tissue hyperemia;
- fever;
- pain;
- the breast becomes dense and may increase in size.
If you consult a doctor in a timely manner, treatment will be conservative, including antibiotic therapy, physical therapy, etc. methods. If abscess formation occurs, conservative therapy is ineffective and surgery will be required.
Stages of flow
The acute course of lactation mastitis is characterized by a sequential change of phases. These phases include:
- Serous phase. This stage is characterized by the formation of primary pathological changes in the breast tissue. At this stage, the woman’s body tries to independently eliminate the source of inflammation. If general and local immunity decreases, mastitis moves to the next stage.
- Stage of infiltrative changes. This stage is characterized by the rapid spread of the pathological process throughout the entire internal area of the mammary gland.
- Stage of pus formation. The course of purulent mastitis can occur in the form of gangrenous and phlegmonous forms.
Other diseases
This is a large group of ailments, including mastodynia (pain in the gland area). Galactorrhea, the main symptom of which is the release of milk or a similar fluid outside of lactation. Fissures and fistulas differ in: pain, the appearance of ichor (and in the case of a fistula, purulent discharge) and increased temperature.
This group also includes fat necrosis. The following symptoms are characteristic of this disease:
- regional lymphadenitis;
- change in nipple shape;
- cyanotic skin of the affected breast;
- the appearance of a specific formation of a round shape.
Atrophy or a sharp decrease in the volume of glandular tissue is accompanied by mastoptosis. The pathology is congenital; malnutrition can be acquired. Corrective therapy (endoprosthetics and mastopexy) is possible for this disease.
Treatment with folk remedies
Along with conservative therapy, doctors recommend using traditional medicine. At the initial stages of the disease, you can include procedures for washing the affected breast with a special infusion. To prepare it, you need two tablespoons of a dry mixture of chamomile and yarrow flowers (1:4) poured into 0.5 liters of boiling water. This infusion has a disinfectant and anti-inflammatory effect.
To relieve swelling, you can prepare a honey cake. To do this, you need to mix a tablespoon of honey with two tablespoons of flour and knead the dough. The cake must be applied to the affected area and covered with gauze on top. Such a compress must be kept for at least 10 hours.
Mastitis in non-lactating women, the symptoms of which are described in this article, requires qualified treatment. Warming compresses should not be used. High temperatures can cause suppuration. The use of traditional recipes is permissible only after consulting a doctor.
Anomalies
Of the main indicated anomalies, psychological discomfort is caused by the absence of the pectoral muscle, glands and extra nipples located along the milk lines. Physical discomfort is caused by:
- excess mammary glands appearing along the milk lines;
- inverted nipples or their absence, making feeding impossible.
Accessory glands are usually bilateral. The pathology is called polymastia. In addition to aesthetic ones, problems can arise during lactation, when additional lobules in the axillary region or glands along the milk lines are cut, hurt, and sometimes secrete.
Diagnostics
Timely diagnosis is the key to successful treatment of mastitis in nursing women. To identify this disease, the following diagnostic techniques are used:
- a clinical blood test to identify markers of inflammation, such as an increase in the number of leukocytes and acceleration of ESR;
- ultrasound examination of the mammary glands;
- bacteriological examination of fluid discharged from the nipple;
- studies aimed at excluding diseases such as actinomycosis and tuberculosis;
- mammography (X-ray) of the mammary glands, which allows to exclude benign and malignant neoplasms;
- If necessary, a biopsy can be performed to exclude carcinomatous mastitis.
Treatment of inflammation of the mammary glands
Mastitis in the first two stages responds well to conservative treatment. In this case, the woman does not even have to stop breastfeeding. Doctors recommend stopping breastfeeding only during antibacterial therapy, and only in cases where the drug can harm the baby.
It is strictly forbidden to self-medicate, since the transition from a relatively safe to a life-threatening state takes no more than 4-5 days. In destructive forms, as well as in specific mastitis, surgical intervention is required, the consequences of which are cessation of lactation and scars on the chest.
The use of folk remedies does not provide a 100% guarantee of relieving inflammation of the mammary gland. You need to contact a mammologist as soon as possible and undergo an ultrasound to determine the stage of the inflammatory process and select the optimal treatment tactics.