Sections and functions of the small intestine
The small intestine is the longest part of the digestive tract, ranging from 6.5 to 8 m in length, with an absorption surface area of more than 16.5 square meters. m, since it increases due to villi and outgrowths.
The small intestine has three sections: the duodenum, which extends from the stomach, as well as the jejunum and ileum. The latter ends in connection with the cecum, which is already part of the large intestine.
After passing through the stomach, the food mass enters the duodenum, where a mucous secretion is produced that promotes the breakdown of nutrients. The ducts of the liver and pancreas also open here. In the following sections, the breakdown of complex substances and their absorption continues.
Food chyme enters the small intestine within four hours due to the contraction of muscle fibers, which mix it and move it into the lower parts of the digestive tract.
Thus, the main functions of the small intestine are digestive, absorption and motor-evacuation.
Description of the disease
The small intestine is located between the stomach and large intestine. It is in this area that the most important digestive processes take place. The small intestine includes the following sections:
- duodenum. It is the initial part of the small intestine. It begins immediately after the stomach. It is associated with the following digestive glands: liver, pancreas, gall bladder;
- jejunum. It is represented by the middle part of the small intestine. This area is located between the duodenum and ileum. The loops of this intestine occupy a place in the left upper abdomen;
- ileum. It is the lower part of the small intestine. This section begins after the jejunum and ends in front of the cecum. This area has thick walls, a large diameter, and many vessels. It is located on the right lower abdomen.
Pain in the small intestine occurs with the following pathologies:
- maldigestion syndrome;
- Crohn's disease;
- intestinal dysbiosis;
- enteritis;
- celiac disease;
- intestinal obstruction;
- malabsorption syndrome;
- intestinal dyskinesia;
- duodenal ulcer;
- tumor of the small intestine;
- intestinal diverticula, volvulus;
- ischemia, intestinal infarction.
https://youtu.be/rl_57zHgexc
Symptoms and signs of diseases of the small intestine. Diagnosis of pathology
Diseases of the small intestine do not have any special, specific symptoms. Therefore, to clarify the diagnosis, the patient may be referred for various examinations, especially for most ailments, it is important to know that the signs are similar - abdominal pain, unstable stool, vomiting, nausea...
The most effective method is capsule endoscopy. The patient swallows a miniature camera, which, passing through all parts of the intestine, takes pictures. Unfortunately, the examination is not carried out in all clinics.
More accessible are intestinal or ileocolonoscopy, as well as radiography of the small intestine. Before an X-ray examination, the patient drinks a barium mixture, a contrast agent, the progress of which determines the functional state of the intestine - peristalsis, narrowing of the lumen, the presence of diverticula, polyps.
If a tumor is suspected, irrigoscopy is performed, identifying bleeding, fistulas, and diverticula. Finally, ultrasound provides data on the integrity of the walls of the gastrointestinal tract, inflammatory processes, and cancer.
In addition to these examinations, laboratory tests of blood and stool are prescribed to identify signs of malabsorption, for example, deficiency of vitamins and microelements, as well as internal bleeding and other pathologies.
Basics of a rational diet
Products containing hard-to-digest carbohydrates are excluded: cereals, including pasta, brown bread, legumes. Rice, potatoes, bananas and yogurt should be present in your diet as often as possible.
Meals are divided into at least six meals. Food should be chewed thoroughly and not washed down. Separate consumption of carbohydrates and proteins is effective. It is better to replace tea and coffee with mint infusion.
It is important to adhere to the rule: “When I eat, I am deaf and dumb.” This prevents air from being swallowed along with food. The consumption of gas-forming foods (cabbage, asparagus, corn, legumes) should be reduced. You cannot mix proteins, fructose, and starch when eating at the same time. Limit consumption of dairy products. Dishes should not be too cold or hot.
Diseases of the small intestine
Diseases of the small intestine can be congenital, functional, inflammatory, or tumor. Congenital ones appear in children in the first years of life, tumor ones, as a rule, develop in older people.
An elevated temperature indicates an infectious disease. The disease can be triggered by injury, surgery, smoking (especially on an empty stomach), infection, addiction to fatty or spicy foods, alcoholism, chronic stress, and certain medications. I will focus on the main diseases of the small intestine.
Enteritis
Inflammation of the mucous membrane of the small intestine is caused by bacteria, viruses, and helminths that enter with food or liquid. As pathogens multiply, they release toxins, which leads to inflammation and swelling of the wall of the small intestine.
The disease can occur against the background of medication, radiation therapy, and poisoning with arsenic and sublimate. Sometimes the disease is diagnosed simultaneously with colitis (inflammation of the colon) or pancreatitis (inflammation of the pancreas).
Enteritis can appear several hours or days after the pathogen enters the intestines and lasts about a week.
Symptoms of enteritis
Pain in the navel area, mushy diarrhea up to 5 times a day, vomiting, and sometimes fever. After defecation, weakness occurs, a drop in blood pressure, tachycardia, dizziness, and tremor are possible.
The disease most often occurs in a mild form, so the doctor does not prescribe any additional examinations. For moderate enteritis, you should drink more fluids and stop taking antidiarrheal (anti-diarrhea) medications, this will slow down the elimination of toxins.
Conservative treatment of enteritis
In the acute form of the disease, it is necessary to urgently rinse the stomach with a weak solution of baking soda and take a laxative, for example, 30 ml of castor oil or 25 g of magnesium sulfate with 100 ml of water.
On the first day of illness, completely refuse food and drink plenty of boiled water and strong tea without sugar. On the second day, include low-fat broth, pureed porridge with water, and crackers in the menu. Then, taking into account the condition, the diet can be expanded.
Drug therapy includes antidiarrheal drugs - rehydron or glucosolan ; antispasmodics - besalol, no-shpu or papaverine ; antimicrobial drugs - phthalazole or ersefuril .
To improve digestion, enzymes are prescribed - mezim forte, festal ; to normalize the intestinal flora - Hilak Forte, Linex, Bactisubtil , as well as Bificol, Lactobacterin.
Complications of enteritis
In the chronic form of enteritis, extraintestinal manifestations cannot be excluded - vitamin deficiency, osteoporosis, dystrophy, which are associated with impaired absorption function of the intestine.
If the disease occurs with rapid loss of fluid, dehydration may develop. In this case, treatment will be in a hospital. Complications of the disease are chronic diarrhea, irritable bowel syndrome, lactose intolerance.
Traditional recipes for enteritis
Mix 6 tbsp. spoons of chamomile flowers, 2 tbsp. spoons of peppermint leaves and valerian roots. Pour 4 tbsp. collection spoons 1 liter of water, boil for 15 minutes, leave for an hour. Drink 150 ml 3 times a day after meals to relieve cramps and a feeling of heaviness in the stomach. Store the prepared infusion in a thermos for 2 days.
Prevention of enteritis involves strict adherence to personal hygiene rules. Wash fruits and vegetables thoroughly, eliminating expired products and green potatoes.
Dyskinesia
This diagnosis is made if the peristalsis of the walls of the small intestine is weakened or strengthened. The disease develops against the background of other pathological processes (cirrhosis, pancreatitis, gastritis, cholecystitis), as well as as a result of malnutrition and prolonged stress.
Symptoms of intestinal dyskinesia
With increased peristalsis, mild spastic pain occurs, the stool is liquid, and undigested food is noticeable in it. Weakened peristalsis leads to dull pain in the navel, bloating, and a feeling of heaviness. The diagnosis is confirmed after X-ray contrast examination.
Treatment of dyskinesia
In addition to the medications prescribed by the doctor, decoctions of cinquefoil or oak bark . Pour 2 tablespoons of raw material into 300 ml of water, boil for 15 minutes, let it brew. Drink a decoction of cinquefoil 100-150 ml 3 times a day, oak bark - twice.
Diverticula
Bag-like protrusions of the intestinal walls, diverticula, can be congenital, resulting from connective tissue pathology, or acquired, which are formed due to poor nutrition, in particular, insufficient consumption of fiber, fruits and vegetables. Provoking factors are constipation, obesity, sedentary lifestyle.
Symptoms develop only with inflammation (diverticulitis) - the temperature rises and abdominal pain appears. Diverticulitis can lead to intestinal bleeding, perforation, adhesions, or fistulas. Diverticula are removed surgically.
Dysbacteriosis
Also a very common disease, it occurs while taking antibacterial drugs, intestinal infections, and an unbalanced diet. Symptoms are general, characteristic of diseases of the small intestine. The diagnosis of dysbiosis is confirmed by testing for dysbacteriosis and stool culture.
To restore normal microflora, probiotics ( bactisubtil, enterol, linex ), as well as agents that promote the growth of beneficial microflora, so-called prebiotics ( lactulose, duphalac, normase ), are prescribed. Patients should eat properly and lead an active lifestyle and exercise.
Peptic ulcer
According to statistics, duodenal ulcers are diagnosed four times more often than gastric ulcers. The disease is caused by the bacterium Helicobacter pylori, which is able to survive in the acidic environment of the stomach, as well as drug therapy, especially the use of non-steroidal anti-inflammatory drugs.
Smoking, stress, alcohol abuse, and poor diet increase the risk of developing the disease. Gastroscopy allows you to identify not only the localization of the ulcer, but also bleeding and scar changes.
Symptoms and signs of the disease
Signs of the disease are dull pain in the abdomen, which subsides after eating or taking medications that reduce the concentration of hydrochloric acid in the stomach, and intensifies after 3-4 hours. Characterized by “hungry” and “night” pain, sour belching, vomiting, and flatulence.
Peptic ulcer disease is dangerous due to bleeding, which can be hidden and is only revealed by increasing anemia. Blood may be in the vomit or stool. Minor bleeding is stopped during endoscopy by cauterizing the ulcer; severe bleeding is eliminated by surgery.
When the ulcer perforates, peritonitis develops, which is accompanied by acute stabbing pain and fever.
Treatment
Treatment involves taking medications that suppress the secretion of hydrochloric acid and prevent the proliferation of Helicobacter pylori. The patient must follow a diet.
Crohn's disease
This is the name of a chronic inflammatory disease that occurs in the inner mucous membrane and submucosal layers of the intestine. The diagnosis is made after a colonoscopy and computed tomography.
Symptoms
Symptoms of Crohn's disease - in addition to the general manifestations, blood in the stool or hidden bleeding, weight loss, inflammation of the joints, eyes, skin, pathology of the liver, biliary tract.
Treatment
Therapy consists of reducing the inflammatory process, preventing relapses and complications. Patients are prescribed a diet, anti-inflammatory drugs, immunosuppressants, corticosteroid drugs, and symptomatic therapy. In emergency cases - surgical treatment.
Allergy
This immune disease is associated with changes in the intestinal mucous tissue. Symptoms are characteristic of most diseases of the small intestine; skin rash, itching, swelling, shortness of breath, weakness, and atopic dermatitis are also possible. In severe cases, anaphylactic shock cannot be ruled out.
To confirm the diagnosis, special tests are performed to identify the allergen. Treatment is taking antihistamines.
Celiac disease
Another name for the disease is gluten enthropathy. The disease develops as an immune response to the consumption of gluten, a protein found in wheat, rye, and barley. With pathology, damage to intestinal tissue occurs and the process of absorption of nutrients is disrupted.
Signs
Symptoms of celiac disease include abnormal consistency and frequency of stool, flatulence, vomiting, as well as the development of anemia and osteoporosis, headaches, and heartburn.
Children may experience delayed physical development, hyperactivity, and poor coordination. Usually the disease manifests itself by 1.5 years. In adults, the first symptoms of the disease may occur after surgery or an infection; in women, during pregnancy.
Diagnostics
To determine pathology, blood tests and genetic testing are done. If necessary, endoscopy of the small intestine is performed with tissue sampling to determine the degree of villous atrophy.
Therapy
The only way to avoid exacerbation of the disease is to exclude gluten-containing foods from your diet. In severe cases of the disease, corticosteroid drugs are prescribed. To eliminate the effects of inflammation - vitamins and minerals. It may take up to 6 months for the intestinal mucosa to recover.
If symptoms persist even during a gluten-free diet, tests are ordered to rule out a tumor. Patients with celiac disease are at risk for colon cancer.
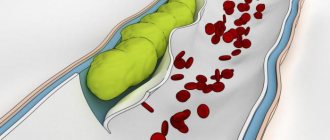
Ischemia
In case of circulatory disorders of the small intestine - thrombosis or narrowing of the lumen of the arteries, atherosclerotic plaques - ischemia may occur. In severe situations, when blood stops flowing to the cells, even intestinal infarction is possible.
Symptoms
Signs of chronic ischemia are abdominal pain after eating for 1-3 hours, which intensifies over several days. Diarrhea, nausea, vomiting, and weight loss develop. Signs of acute ischemia are sharp abdominal pain, aggravated by pressure, blood in the stool, vomiting, hyperthermia.
Diagnostics
The diagnosis is confirmed using computed tomography and magnetic resonance imaging, colonoscopy, endoscopy, Doppler ultrasound, and clinical blood tests.
Treatment
Drug therapy includes medications that dissolve blood clots and prevent them from forming again, as well as vasodilators that improve blood circulation. In acute ischemia, shunting and thrombus removal are sometimes performed.
Malabsorption syndrome
The disease develops when digestion in the small intestine is disrupted and it loses its ability to absorb nutrients. In addition to general signs of dysfunction, systemic symptoms develop - weight loss, weakness, anemia, osteoporosis, swelling, dermatitis.
Diagnostics
A blood test indicates a lack of vitamins and microelements. The coprogram detects muscle fibers and starch in the stool, and changes in acidity. To accurately determine the cause of the disease, an X-ray examination, ultrasound of the abdominal cavity, and other examinations are performed.
Therapy
Treatment is aimed at restoring the absorption function of the intestine, eliminating the pathologies that led to malabsorption syndrome. The patient is given a drip with vitamins and microelements; to normalize the microflora, probiotics and prebiotics and an appropriate diet are prescribed.
If necessary, surgical intervention is performed.
Whipple's disease
This is a fairly rare disease that develops when there is a bacterial infection of the small intestinal mucosa, which leads to impaired absorption of nutrients.
Symptoms of Whipple's disease include diarrhea, cramping pain that intensifies after eating, and sudden weight loss. Extraintestinal manifestations also occur, for example, damage to the skin and eyes. To confirm the diagnosis, a biopsy of the small intestinal mucosa is prescribed.
The disease is treated with antibacterial drugs; therapy is long-term, more than a year, despite the fact that the symptoms subside a couple of weeks after starting medication.
Neoplasms
In the small intestine, benign neoplasms more often occur - lipomas, neurofibromas, fibromas, leiomyomas. The tumor is small and usually has no symptoms.
Signs of intestinal tumors
In other cases, blood appears in the stool, and partial or complete intestinal obstruction occurs. Then surgical treatment is performed. Small benign tumors can be removed by endoscopy.
Tumors with uncontrolled growth and the ability to affect neighboring organs develop less frequently, usually adenocarcinoma, lymphoma, sarcoma. The causes of such malignant formations are genetic disorders, celiac disease, Crohn's disease, smoking, and alcohol abuse.
Diagnostics
Older people are most susceptible to small bowel cancer, with men more likely than women. Oncology is manifested by abdominal pain, blood in the stool, and other symptoms of intoxication.
The diagnosis is confirmed by fluoroscopy with contrast, endoscopic examination, video capsule endoscopy, computed tomography and magnetic resonance imaging. The type of tumor can be determined only after examining the biopsy specimen under a microscope.
Treatment
Treatment involves surgical removal of the tumor followed by chemotherapy or radiation therapy.
Intestinal obstruction
It develops in the process of blockage of the intestinal lumen by a tumor or hernia. This pathology is called mechanical obstruction. When the cause is weakening or disappearance of peristalsis, which happens as a result of peritonitis, after surgery or injury, they speak of dynamic obstruction.
Signs
Symptoms of the disease are abdominal pain, accumulation of gases, lack of bowel movements, nausea, fecal vomiting. Fluoroscopy of the abdominal cavity helps clarify the diagnosis.
Therapy
Dynamic obstruction is eliminated conservatively - the patient is prescribed motilium or itomed, drugs that stimulate intestinal contraction. Mechanical obstruction requires surgery.
Drug therapy for flatulence
Treatment of the disease should be comprehensive and include several areas:
- Selection of diet in accordance with digestive disorders.
- Normalization of intestinal microflora.
- Improved motor skills.
- Preventing excessive gas formation and ensuring the release of gases naturally.
Since bloating is usually a symptom of an intestinal disease, it is diagnosed first and appropriate treatment is prescribed. Usually after this the flatulence goes away. If you treat only bloating, then after a course of taking such drugs, the symptoms will return again. Therefore, it is necessary to identify the cause of flatulence and only then begin treatment.
To normalize the microflora, pro- and prebiotics are prescribed. Probiotics are medicines containing beneficial bacteria. These include Linex, Bifi-form, Acylact, Enterol. Prebiotics contain indigestible fibers, which activate the growth of your own beneficial microorganisms. These are lactofiltrum, hilak forte, duphalac.
There are several medicinal groups that affect gas formation and their natural elimination:
- Defoamers complicate the formation and ensure the destruction of formed gas bubbles in the intestinal cavity. The released gases are absorbed by the mucous membrane and eliminated by contraction of the gastrointestinal tract muscles. These are espumizan, simethicone, disflatil, meteospasmil.
- Enterosorbents “pull out” toxic substances and gases (smecta, sorbex).
- Medicines that improve motor skills (Motilium, Domstal, Motilak, Passazhix).
conclusions
I believe that, now knowing at least briefly what diseases of the small intestine are, symptoms and signs of the disease, which often manifest themselves, as they say, “just diarrhea,” you will consult a doctor in a timely manner and, by starting the necessary treatment, will stop the development of a serious illness.
Do not self-medicate. Similar symptoms and manifestations sometimes make it difficult to make a diagnosis, and self-medication, blurring the picture of the disease, further complicates the diagnosis. This can lead to progression of the disease, atrophy of the mucosa, and other negative consequences.
Only after an accurate diagnosis will the doctor prescribe drug therapy that will help avoid relapses and prolong remission.
Author: Anatoly Vanin, Candidate of Medical Sciences
Treatment
If any disease has affected the small intestine, symptoms will appear that will be very difficult for the patient not to notice. If abnormal bowel movements, characteristic abdominal pain, nausea, vomiting, headaches, flatulence, or belching occur, you should seek specialized help.
Treatment of diseases arising in the small intestine is considered a rather complex process. The main thing is to strictly follow the doctor’s instructions during the treatment process and follow the prescribed diet.
Intestinal bloating is accompanied by additional unpleasant symptoms. This can be a temporary disorder of the digestive system, or signal the onset of serious diseases - from simple gastritis to pancreatitis and cancer. Some pathologies without timely treatment can even lead to death.
Colonoscopy
Colonoscopy is a research method based on the use of a special device - a fiber colonoscope - a plastic tourniquet with an optical system. Such a study is recommended for preventive purposes to be performed every five years for people over forty years of age and those whose heredity is burdened with oncological pathologies of the intestine.
Before the procedure, it is necessary to cleanse the intestines with the help of medications. Typically, a colonoscopy lasts no more than 30–40 minutes, but is a rather unpleasant procedure. The patient may experience discomfort due to the fact that the intestines fill with air, and the person feels bloated.
Methods for examining the intestines with a fiber colonoscope also allow for the collection of biomaterial for histological analysis. In addition to diagnostic functions, colonoscopy allows you to remove polyps or small benign formations. Using this technique, it is also possible to identify adhesions in the intestines. The results of the study are usually ready immediately after the manipulation.
Virtual colonoscopy of the intestine (MSCT) is the reconstruction of a three-dimensional image of the intestine during computed tomography in a special way. During the procedure itself, air is pumped through a tube in the rectum and then, after the patient holds his breath, the abdominal organs are scanned. Visually, the result of MSCT differs from classical colonoscopy only in a clearer image.
Reviews about virtual colonoscopy of the intestine
Advantages of virtual colonoscopy:
- There is no need to introduce endoscopic instruments into the patient's body.
- It can be performed on patients with severe heart failure and those suffering from poor blood clotting.
- The procedure is gentle and comfortable for the patient, so there is no need for anesthesia or sedation.
- The risk of damage to the colon during MSCT is significantly lower than during conventional colonoscopy.
- In parallel with the examination of the intestines, other organs of the abdominal cavity and pelvis can be examined.
Virtual colonoscopy is prescribed in the following cases: advanced inflammatory processes in the digestive tract, suspicion of the development of a malignant tumor, peptic ulcer of the stomach and duodenum, frequent disruptions in the gastrointestinal tract of unknown etiology. The list includes regular pain and cramps in the abdomen of unknown origin, bleeding that occurs in the lumen of the small or large intestine, patients over 40 years of age.
During virtual diagnostics, it is impossible to take a biopsy sample for research, so it will not be possible to confirm the malignancy of the tumor in this way.
Painkillers
It is possible that intestinal inflammation will pass painlessly, so NSAIDs, analgesics and antispasmodics are used to eliminate discomfort. Antispasmodics such as No-shpa, Duspatalin, Papaverine and Drotaverine have proven themselves especially well.
Since the disease often occurs with severe pain, painkillers are also prescribed during treatment.
- Especially often in such situations, eubiotics like Enteroseptol, Mexase or Intestopan, Enterofuril, etc. are prescribed.
- These products contain hydroxyquinoline, due to which their effectiveness increases significantly.
- They normalize stool, reduce bloating and eliminate abdominal pain.
Such drugs are practically free of side effects if taken for a short course; only a small number of patients experienced headache and mild nausea. But with long-term therapy, it is possible to develop or damage the optic nerves, etc.
Therefore, you should not get too carried away with these drugs; they are usually prescribed in 10-day courses. If the treatment needs to be repeated, then at least a month should pass between the courses.
Preventing bloating
Prevention of flatulence includes giving up bad habits, especially smoking and constant chewing of gum. If signs of bloating occur periodically, you need to find out what caused it.
To identify foods that are not right for you, you can keep a so-called “food diary” in which you write down all the foods you eat during the day. After some time, you will be able to identify a “harmful” product. A half-hour walk after a meal will help reduce the manifestations of flatulence. It is important to remember that bloating is a very common symptom. Therefore, it is important to identify the cause of its appearance, because sometimes flatulence indicates serious pathologies of the gastrointestinal tract.
Antimicrobials
The advisability of prescribing one or another group directly depends on the severity of the symptoms of the disease.
Aminosalicylic acid and its analogues. Of this group, mesalazine-based drugs are most often prescribed. They are produced in the form of tablets or granules for internal use. They are endowed with special shells that allow the drug to dissolve throughout the colon without being destroyed in the acidic environment of the stomach.
The maximum concentration of the active substance in the blood is detected 5 hours after the first use. These drugs are used for exacerbation and for the prevention of ulcerative colitis and Crohn's disease.
Trade names of mesalazine:
- Mesacol;
- Salofalk;
- Mezavant;
- Pentasa;
- Asakol.
Sulfasalazine is also widely used. It has anti-inflammatory and antimicrobial bacteriostatic effects. Reaches maximum concentration 3-12 hours after application. It has found application in ulcerative colitis (treatment of exacerbations and maintenance during remission), mild and moderate Crohn's disease.
Produced under the same name by different manufacturers. There are different coatings for these tablets: film and enteric. The drug coated with the second type is considered better.
It is more toxic to the body compared to mesalazine. A prerequisite for use is the combination with folic acid (vitamin B9). The fact is that the drug inhibits its absorption in the small intestine, so you need to additionally take drugs with a high content of vitamin B9.
We recommend reading:
Cryptitis: definition of pathology, symptoms and treatment methods
Corticosteroids. The second group, which is also used for inflammatory bowel diseases, when previous drugs did not relieve symptoms or Crohn's disease has systemic manifestations. Prednisolone tablets are usually used. It has an antiallergic and anti-inflammatory effect, reduces capillary permeability, and reduces the formation of scar tissue. It acts on all stages of inflammation and increases the resistance of cell membranes to the destructive effects of various factors.
The maximum concentration is achieved an hour and a half after internal use. Used for ulcerative colitis, local enteritis, Crohn's disease. Produced under the same name.
There are drugs that are injected directly into the rectum. They have less systemic effects on the body and are easier to tolerate. Rectal forms are divided into the same pharmacotherapeutic groups as oral ones.
Preparations based on mesalazine:
- Suppositories (Kansalazin, Pentasa, Salofalk). Used for exacerbation of ulcerative colitis of the lower rectum or during remission.
- Rectal suspension (Pentasa, Salofalk). Used for inflammation of the sigmoid colon and left-sided ulcerative colitis. It is administered using a ready-made enema with a solution once a day at night, preferably after bowel movement naturally.
- Foam for rectal use (Salofalk). It is used for the same symptoms as the candles of the same name. Usually administered into the rectum at night, the daily dose is 2 presses on the bottle pump. If a person cannot hold this amount of foam inside, the dose is divided into 2 times: at night and at night/early in the morning. The uniqueness of the foam lies in its adhesive properties; it stays on the mucous membranes for a very long time.
Other drugs for rectal use:
- Proctosan. Treats inflammatory processes in the rectal area. It contains a local anesthetic component, which can temporarily bring relief by suppressing pain symptoms. Available in the form of ointments and suppositories.
We recommend reading:
Duodenitis (inflammation of the duodenum): symptoms and treatment methods
- Methyluracil. Used for erosive and ulcerative colitis and inflammation in the sigmoid colon. Accelerates epithelization processes, which allows wounds to heal faster.
- Ultraproct. Contains a glucocorticosteroid and local anesthetic, used for proctitis. It has anti-inflammatory, antipruritic and analgesic effects.
Antimicrobial agents that are used in the complex treatment of intestinal inflammation include the group of nitrofurans (furazolidone, nifuroxazide) and 8-hydroxyquinoline derivatives (enteroseptol). These drugs are active against gram-positive and gram-negative microorganisms. In low concentrations they can have a bacteriostatic effect, and in high concentrations they can have a bactericidal effect.
Prescribed for prolonged constipation. Drugs in this group include Bisacodyl, Guttalax, Senadexin, Senade. If you have hemorrhoids and anal fissures, it is better to use Senade. Guttalax is a universal remedy, as it is used for constipation of various origins.