One of the most serious pathologies of the digestive system is pancreatitis. This is a family of diseases in which the pancreas becomes inflamed. The organ performs two important functions:
- Exocrine - release of digestive enzymes (breaking down starch, fats, proteins) and electrolytic fluid into the duodenum, transporting enzymes to the duodenum.
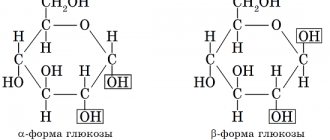
- Endocrine – production of the hormones glucagon and insulin into the blood, regulating carbohydrate metabolism.
The main reasons causing disturbances in the functioning of the pancreas and provoking inflammation are: in 70% of cases – alcohol consumption, in 20% – cholelithiasis. The disease can occur due to injuries to the pancreas, various infectious viral and autoimmune diseases, congenital predisposition, and taking certain medications.
In the international classification, pancreatitis, depending on the causes of occurrence, is divided into: acute, chronic, caused by alcohol, and chronic, provoked by other reasons.
Under the influence of chemical or physical damage to the pancreas, ductal pressure increases and inactive proenzymes are released from the cells of the organ. They do not have time to enter the lumen of the duodenum and are activated, digesting gland tissue. Less commonly, disorders occur with calcification and sclerosis of the parenchyma (internal tissue) of the pancreas. As a result, focal changes, degeneration and degeneration of cells into fibrous (connective) tissue arise and progress. With a long-term inflammatory process, most of the pancreatic cells (glandular elements) atrophy, and enzymes and hormones cease to be released. This leads to enzyme deficiency, in 40% of cases to diabetes mellitus.
Diabetes with pancreatitis
Diabetes with pancreatitis is accompanied by digestive disorders, abdominal pain and impaired carbohydrate metabolism. More often than not, blood sugar levels are quite high. This is because the pancreas cannot secrete enough insulin, lowering glucose levels. Type 1 diabetes occurs.
In type 2 diabetes, the breakdown of carbohydrates is impaired. When insulin levels are high, cells do not respond to the hormone. This forces the pancreas to work harder. As a result, inflammation and atrophic pancreatitis progresses.
Symptoms
First of all, a person is bothered by cutting pain in the area of the left hypochondrium. Their appearance is associated with food consumption. They appear after about 2 hours, when food enters the intestines and needs pancreatic juice. In the first months, pancreatitis is expressed by a periodic change in exacerbation of pain and calm. If you do not monitor your diet, pain begins to appear regularly and the disease becomes chronic.
Then very unpleasant symptoms begin that are associated with the gastrointestinal tract. These are flatulence, heartburn, nausea, diarrhea, and loss of appetite. This is due to the fact that the disease affects many pancreatic cells that secrete juice, the lack of which leads to indigestion of food.
Medical nutrition
Pancreatitis and diabetes mellitus must be treated comprehensively. In parallel with drug therapy, patients are required to adhere to dietary nutrition. This approach will help avoid complications, achieve stable remission, and improve the quality of life of patients.
Basic principles of nutrition for pancreatitis and digestive disorders
The basic rules of nutrition for pancreatitis are to balance the nutritional value of the foods consumed. It is necessary to increase the amount of protein, reduce the consumption of simple carbohydrates and optimize the number of plant and animal products. Food containing protein has a beneficial effect on the course of pancreatic diseases. Proteins are found in foods: meat, fish, soybeans, egg whites and nuts. Regardless of the presence of diabetes in the anamnesis, split meals are important. The regimen involves 6 meals a day in portions weighing no more than 300 g.
For the treatment of aggravated and chronic inflammatory processes of the pancreas, a special diet table No. 5p has been developed. For diabetes, table No. 9 is used.
For patients with pancreatitis, it is important not to provoke strong secretion of gastric juice, as with a stomach ulcer. An increased content of hydrochloric acid causes the production of gastrin. The hormone stimulates the secretion of the pancreas, its digestive enzymes and insulin. It is necessary to exclude spicy and sour foods, fried and smoked foods from the diet. Drinking alcohol is prohibited.
The diet for ulcers, as for pancreatitis, involves steaming or boiling dishes, grinding them and serving them warm. Mechanical stress and temperature changes have an adverse effect on the gastric mucosa, causing inflammation and the production of pancreatic enzymes.
Do's and Don'ts for Pancreatitis and Diabetes
The diet of patients in each case is selected individually, taking into account concomitant pathologies. The diet for pancreatitis and diabetes mellitus should also take into account taste preferences and intolerance to specific foods and at the same time is designed to compensate for the lack of nutrients. This deficiency occurs as a result of insufficient absorption of proteins, fats and carbohydrates. The menu should take into account the body's glucose tolerance level.
In case of diabetes, the diet of patients includes a sufficient amount of protein foods. Protein-rich foods break down slowly and do not cause spikes in blood sugar and are recommended for diabetics.
When the chronic inflammatory process worsens, rice, oatmeal and semolina porridges are excluded from the diet. Preference is given to buckwheat. The bread should be chosen gray, and before eating it, it should be dried. Fresh and rich baked goods, especially with gastritis with low acidity, cause rotting of poorly digested food. This complicates the breakdown of carbohydrates, increases the load on the pancreas and leads to spikes in blood sugar. For mild diabetes and chronic pancreatitis, it is allowed to eat crackers and bagels. These products are relatively low in calories. It is better to soak bagels and dryings in tea. Such gentle nutrition does not irritate the mucous membrane and enriches the patient’s menu.
In case of severe diabetes, the patient is prohibited from eating sweets and sweet fruits. But with low sugar levels and chronic pancreatitis, you can include a small amount of sweets in your diet.
Vegetables and fruits during exacerbation of diseases must be heat treated. During remission, it is allowed to eat raw. Sour fruits: apples, plums, etc. are contraindicated in the acute phase of the disease. In addition to the fact that these fruits stimulate the production of gastric and pancreatic juices, plums for pancreatitis increase diarrhea and worsen the course of diseases. During stable remission, you can eat sour fruits in small quantities. They contain a large amount of fruit acids, vitamins and minerals that have a beneficial effect on the body and its regenerative functions.
Drug treatment of pancreatitis in adults: tablets and drugs
- About the development mechanism
- About type 2 diabetes
- About treatment and diet
Chronic pancreatitis is one of the forms of the inflammatory process that occurs in the pancreas. This process is characterized by a fairly long course of the disease, with changes observed in the area of its cells and tissues, which cannot be reversed or improved by marshmallows.
Especially if the person’s condition is aggravated by diabetes mellitus, both type 1 and type 2. In the complicated course of diabetic pancreatitis, experts observe the regeneration of healthy tissue, which is replaced by either adipose or connective tissue. More details about what the disease is and how to deal with it, what the diet is further in the text.
The primary stage of pancreatitis, with possible stages of remission and periods of exacerbation, during which the pancreas becomes inflamed, is accompanied by painful sensations of varying degrees of intensity and their occurrence in the case of oat deficiency. This stage can last about ten years. If any diet is used, the period may increase, but the onset of the second stage is inevitable without constant preventive measures.
When the next stage occurs, the symptoms of the so-called impaired function of the digestive tract come first:
- flatulence;
- heartburn (relieved by semolina);
- diarrhea;
- loss of appetite.
As specific conditions, when pancreatitis develops and, along with it, diabetes mellitus, a minimal, but still destabilization of carbohydrate metabolism is manifested.
In this case, a strict and constant diet containing buckwheat is necessary.
During the formation of all processes that are associated with chronic pancreatitis, the cells of the gland present begin to destroy, and stable tolerance to glucose is formed. In this regard, the sugar ratio on an empty stomach is normal, and after eating it is increased. The same applies to the permissible duration of hyperglycemia, which becomes “active” after eating food, in particular millet.
The final stage is aggravation of diabetes mellitus, which occurs in more than 30% of people with a history of long-term pancreatitis. At the same time, a diabetic very often encounters such specific conditions as: ketoacidosis, macro- and microangiopathy, as well as many others.
As is known, the first is destabilization in the field of carbohydrate metabolism, which is provoked by insulin deficiency. The presented symptom is not typical for the symptomatic type of the disease and diet in this case may also be effective.
Further, damage is likely to occur not only to medium vessels and large arteries, but also to arterioles and capillaries. The second phenomenon occurs much more rarely than even with diabetes of any type. Therefore, pancreatitis and developing diabetes mellitus should be treated as quickly as possible.
At the primary stage of diabetes mellitus, medications that reduce the glucose ratio are effective. In the subsequent treatment process, the presented therapy will not be effective. The need for insulin therapy in such a situation is extremely small, but a special diet is required.
About type 2 diabetes
Quite often, against the background of developing pancreatitis, people are faced with an illness such as type 2 diabetes. It is known to be characterized by the fact that when inflammation is detected, an increase in the blood sugar ratio occurs. The formation of the presented disease is accompanied by acute painful sensations in the abdominal area and destabilization of digestive processes.
Experts identify several stages of the formation of the presented disease:
- deterioration of pancreatitis and recovery, which alternate with each other;
- destabilization of carbohydrate metabolism due to irritation of beta cells in the pancreas (in this case, a vitamin-protein diet will be needed);
- formation of type 2 diabetes.
In general, 35-40% of people develop diabetes mellitus against the background of pancreatitis. Each of these ailments enhances the impact of each other on the human body.
A diet must be followed, otherwise full recovery may never occur.
About treatment and diet
The process of treating pancreatitis in diabetes mellitus is labor-intensive and lengthy; it takes several rather long stages. Each of them must be observed. Thus, pancreatitis and developing diabetes mellitus can be cured using replacement therapy not only to optimize carbohydrate-type metabolism, but also to eliminate enzymatic-type insufficiency.
In the presented situation, it is necessary to use not just specialized enzymatic, but also hormonal drugs. It should be noted that most often the use of any drugs in the form of tablets does not bring the expected good results. However, a well-structured diet was and remains necessary.
Thus, it is extremely important to maintain optimal nutrition during the treatment of both pancreatitis and diabetes. This means excluding foods that are dangerous to the pancreas from the menu. It is vitally important to stop eating fatty and spicy foods, and also to minimize flour products and sweet foods in your diet. In addition, it is not recommended to eat:
- meat-type broths;
- apples;
- cabbage;
- mayonnaise, ketchup and sauces.
This is explained by the fact that such food can have the most irritating effect on the epithelium in the intestinal area. In this situation, if the two presented illnesses go away simultaneously, doctors insist that the following diet be maintained for every day: vegetables and fruits 300-400 grams, dressing for food - no more than 60 g, food of protein origin - from 100 to 200 G.
Taking into account everything presented, you can count on the fact that pancreatitis in diabetes mellitus will be cured as soon as possible. It is important to follow absolutely all the specialist’s recommendations and not forget about compensation for diabetes.
As you know, the pancreas is responsible for the production of necessary enzymes that take part in the digestion of food, including peas. In addition, it is this gland that is necessary to break down not only proteins, fats and carbohydrates, but also their components. Its normal functioning also ensures the production of insulin, which is impaired in diabetes mellitus. Read more about how changes occur in the body of each diabetic and whether recovery is possible.
About hardware
The pancreas simultaneously has two functions: endocrine and exocrine glands. The part that carries out endocrine functions includes approximately a million clusters of cells known as the islets of Langerhans. The presented islands, in turn, consist of four types of cells:
- alpha cells produce glucanone (and increase the blood sugar ratio, just like sauerkraut);
- beta cells are responsible for secreting insulin (reduce the amount of glucose);
- gamma cells develop somatostatin and further regulate the degree of activity of both alpha and beta cells;
- PP cells enable interaction with pancreatic polypeptide.
Also, being part of the exocrine system, the pancreas has another function, namely helping in the functioning of the digestive system. After all, it is she who produces pancreatic fluid containing the necessary digestive enzymes, as in corn. They are necessary for humans to break down food. This also affects blood glucose levels.
It is worth noting that in addition to the pancreas, the endocrine gland is also important. After all, a poorly functioning endocrine gland and diabetes mellitus are interconnected.
About sugar levels
The effect of the pancreas, like lemon, on sugar levels is an obvious process. In the human body, the transformation of glucose, which comes from eating food, into energy for the interaction of cells with each other is noted. As you know, glucose in general form is found in all sweets - for example, in confectionery or ice cream.
After eating food, the amount of glucose in the blood suddenly increases, and at the same time insulin is created. When the blood sugar ratio decreases—for example, as a result of physical exercise—then the amount of insulin also becomes less.
Another hormone that is produced by the pancreas is glucagon. If there is such a need, it directly affects the liver, and therefore:
- the sale of glucose reserves is noted;
- Due to this, the ratio of sugar in human blood increases.
Insulin, remarkably, is processed and stored in the pancreas, which is a lobular organ. It is located transversely in the space behind the peritoneal region. This gland is often thought of as two organs in one. This occurs due to the fact that it has been established that, in addition to insulin, the gland produced also produces enzymes that should be considered vital for the process of digesting the food received.
This list also includes lipase, which helps digest fats, as well as amylase, which is responsible for the digestion of carbohydrates. In addition, the pancreas develops a substance such as sodium bicarbonate, which neutralizes excess acidity in the stomach area. After all, it is known that it is he who is capable of destroying the original structure of the walls in the intestinal area. This also affects blood glucose. What can be said about the treatment and restoration of the described gland?
About treatment
- Stabilizes sugar levels for a long time
- Restores insulin production by the pancreas
Forecast and general advice
Clinical studies have shown that in order to obtain stable remission in chronic pancreatitis and diabetes, patients must, first of all, eat right. It is also important to drink enough water. It promotes better digestion of food, normalizes water-salt balance and helps remove waste products from the body.
A balanced diet and replacement therapy improve the quality of life of patients. The doctor will tell you what foods are allowed for pancreatitis and diabetes, select a diet and prescribe a course of treatment. These measures lead to long-term remission in 80% of cases.
Diseases of the pancreas lead to disruption of the gastrointestinal tract and endocrine system. Diabetes mellitus is a chronic pathology that affects all external and internal systems of the human body.
The disease originates in the pancreas, as a result of which it is the pancreas that suffers first. Sugar and the pancreas are a hot topic not only for the elderly age group, but also for young people.
Pancreatitis is an inflammatory process in the pancreas and a high glucose level, an increase in acetone in the urine - precursors to a pathogenic process called diabetes mellitus and the pancreas.
Can sugar increase with pancreatitis, how much diabetes aggravates inflammation of the pancreas, how two pathologies are treated - this is a range of topical issues that concern diabetics when there is inflammation of the organ.
Diet for high blood sugar - types of foods
When hyperglycemia is diagnosed, the first step, regardless of the cause of this syndrome and its mechanism, is to prescribe a diet. Prescribes diet No. 9, which is “classical” in the CIS countries and in endocrinology hospitals. Its peculiarity is the complete balance of products, while the standard daily diet has the following ratio: 330 g of carbohydrates + 95 g of proteins + 80 g of fat.
The following features should be taken into account:
- Of the 90 g of fat per day, you should consume about 30 g of vegetable and unsaturated fats.
- Sweets and pure sugar are completely excluded. Instead of sugar, sweeteners are used: the most popular are “Xylitol”, “Sorbitol”, “Fructose”.
- Be sure to include a large amount of vitamins in your diet, especially B1, A, C and E, as well as fiber.
- Refusal of sweet sodas, flour products and alcohol.
Development of diabetes with pancreatitis
Pathological anatomy of the pancreas is quite simple. However, this cannot be said about the functionality of the internal organ. The pancreas is located between the stomach, spleen, liver and duodenum.
Performs two main functions. It secretes pancreatic juice and also produces a unique hormone called insulin. It is this substance that helps bind glucose, as a result of which it is absorbed at the cellular level.
High sugar with pancreatitis, an imbalance in the chemical balance of pancreatic juice are the key symptoms of developing diabetes mellitus. Depending on the concentration of sugar in the blood, the severity of the pathological process is determined.
It is possible to trace a two-way relationship - diabetes is the culprit, contributing to the disruption of the functionality of the pancreas, and a failure in its functioning worsens diabetes, leading to a severe clinical picture.
This is an established fact. About half of diabetics who are registered at a medical institution sooner or later begin to complain of significant discomfort in the pancreas. They are worried not only about abdominal discomfort, but also about other specific manifestations of pancreatitis. These include nausea, vomiting, and heartburn.
The negative effect of sugar on the pancreas has been proven, which leads to the development of not only acute, but also chronic pancreatitis. We can also say, on the contrary, that inflammation of the pancreas contributes to insulin deficiency. The main causes of gland destruction:
- The beta cells of the internal organ change pathologically.
- Changes are observed outside the parenchyma, have no cellular connection with the pancreas area, and develop as a result of severe poisoning, trauma, or surgery.
Insulin production sharply decreases due to a deficiency of mineral components - silicon, potassium and zinc - these are the substances that “keep” the hormone in the body. If excess calcium is detected, it is deposited on the mucous membranes, which leads to inflammation of the gallbladder (cholecystitis) or the formation of stones in it.
Cancer makes a deadly contribution - cirrhosis of the liver and malignant tumors irreversibly stop insulin production.
Blood sugar and cholesterol: normal for women and men, tests, risk groups
- Sugar norm
- Norm for men
- Norm for women
- Hyperglycemia
- Hypoglycemia
- Analyzes
- The relationship between cholesterol and glucose in the blood
- Classification of lipoproteins
- Beneficial properties of cholesterol
- Cholesterol standards
- Taking tests
- At-risk groups
To maintain good health, every person must eat properly and variedly. For the normal functioning of the body, it is necessary to consume a sufficient amount of proteins, fats, carbohydrates, vitamins, minerals, etc.
But due to an incorrect lifestyle, an unbalanced diet and a number of other features, the content of certain vital components may be overestimated or underestimated. This article will discuss the normal levels of blood sugar and cholesterol.
Sugar norm
Doctors call blood sugar the glucose contained in it. It is simply necessary for the normal functioning of the body, as it is one of the main sources of energy. Glucose enters the body through foods containing sugar or carbohydrates. The processing and absorption of glucose is carried out with the help of insulin, a special enzyme.
Blood sugar levels for men and women of different ages are slightly different. This is due to the characteristics of the body of men and women. In addition, over the years, sugar gradually accumulates in the body, so the level of its content in the blood only increases with age.
Norm for men
For newborns less than a month old, the normal blood sugar level is only 2.8 to 4.4 millimoles per gram.
For children aged from one month to 14 years, the normal level is from 3.3 to 5.6 millimoles per gram. The normal blood sugar level from 14 years to the end of life is 4.6 - 6.4 millimoles per gram.
Bad habits (drinking alcohol, smoking), unbalanced diet, eating fatty, spicy or highly salty foods can lead to a lack or excess of glucose in the blood. In men, this problem can lead to infertility or impotence.
Norm for women
- The normal blood sugar level for female children under one month is 2.8 - 4.4 millimoles per gram.
- At the age of one month to 14 years, this figure can vary from 3.3 to 5.5 millimoles per gram.
- For girls and women from 14 to 50 years old, the norm is 3.3 - 5.6 millimoles per gram.
- After the 50th birthday, this figure drops again to 5.5 millimoles per gram.
Women's sex hormones actively participate in the metabolism and absorption of carbohydrates. That is why glucose is eliminated from a woman’s body several times faster than from a man’s body. But after menopause, the level of sugar content can jump sharply. This is due to the cessation of the production of sex hormones.
Hyperglycemia
An excess of sugar (glucose) in the blood is called hyperglycemia. It may be caused by the following factors:
- Disorders of the thyroid gland;
- Poor nutrition;
- Lack of regular physical activity;
- Wrong lifestyle;
- Diabetes;
- Insufficient synthesis of insulin, the hormone responsible for processing glucose;
- Prediabetes.
The main symptoms of hyperglycemia are:
- Frequent urination;
- Weakness, inability to work;
- Drowsiness;
- A sharp decrease in vision;
- Rapid weight loss;
- Constant dry mouth.
There are several ways to maintain glycemic levels at the proper level. This issue should be approached comprehensively. It is necessary to balance your daily diet, fill it with healthy foods and exclude those foods that contain excess glucose. These include sweets, jam, sweet baked goods, etc.
Hypoglycemia
A lack of sugar in a person's blood is called hypoglycemia. It can be caused by:
- Pancreatic cancer;
- Diseases and disorders of the adrenal glands;
- Insulinoma, etc.
The main signs of hypoglycemia are:
- Constant feeling of hunger;
- Weakness, fatigue;
- Constant feeling of fear;
- Cardiopalmus;
- Irritability;
- Chills;
- Headache and migraines;
- Sweating;
- A sharp decrease in vision.
The main problem with treating hypoglycemia is that it is difficult to diagnose. Failure to act in the presence of this violation can lead to the death of a person.
Analyzes
There are several features of taking tests to determine blood levels. Tests must be taken in the first half of the day, before 11 o’clock.
Blood sampling is carried out only on an empty stomach. Approximately 15-20 minutes after eating, the level of glucose in the body increases significantly. After a few hours, this indicator returns to normal. This process is called nutritional hyperglycemia. It does not affect human health in any way. Blood is taken from a finger or from a vein.
A glucometer is used to determine blood sugar levels at home.
The relationship between cholesterol and glucose in the blood
The processes of carbohydrate and fat metabolism are closely related. Excessive consumption of carbohydrates can lead to the accumulation of excess sugar in the body. This one way or another leads to rapid deposition of fat cells. Due to disturbances in the process of lipid metabolism, blood vessels lose their former elasticity, and cholesterol plaques begin to form in them.
Many medical scientists claim that all patients with type 2 diabetes suffer from hypertension. It is caused by high cholesterol levels.
In addition, elevated cholesterol and blood levels have exactly the same prerequisites:
- Lack of regular physical activity;
- Wrong lifestyle;
- Unbalanced diet;
- Overweight.
Classification of lipoproteins
At the end of the 20th century, there was a huge amount of debate about the benefits and harms of cholesterol in the body. Many argued that cholesterol is an extremely harmful substance that can cause hypertension and a number of other diseases. Others divided cholesterol into “bad” and “good.”
None of the above classifications are completely correct. Lipids play a huge role in the life of the body. They have a significant impact on the functioning of many organ systems. But some of them can also lead to bad consequences (plaque deposition, hypertension). The further fate of lipids depends not on their structure and composition, but on which protein they will be attached to. Lipoproteins are responsible for this.
They are divided into several types:
- Low density level. They transport particles from the liver to other organ systems. An increased content of such lipoproteins can lead to cardiovascular diseases.
- Increased level of density. The complete opposite of the previous variety. Such lipoproteins help avoid cardiovascular diseases. They transport lipids from all organ systems to the liver.
- Triglycerides. They are the body's energy resource. They are deposited when consuming dietary fats. In case of food shortage, the body will use triglycerides as the main source of energy.
Beneficial properties of cholesterol
Cholesterol is a very important element that is necessary for the normal functioning of the body. It performs many tasks and has a number of useful properties. The first of them is that cholesterol takes an active part in the processing and absorption of food. Without such an element it is impossible to imagine the production of the necessary salts and digestive juices.
The next property is that cholesterol is very important in such a process as the production of sex hormones in male and female bodies. These hormones include, for example, estrogen or testosterone. Without cholesterol, human reproductive function would be seriously impaired.
Cholesterol is also involved in the production of vitamin D. With a lack of lipids, weak immunity, frequent viral diseases, etc. are observed.
You can control your cholesterol levels on your own. To do this, you need to completely reconsider your diet, make it more varied and balanced.
Cholesterol standards
The cholesterol index largely depends on a person’s gender and age. It is worth considering this indicator for women and men of different age categories.
Cholesterol standards for women
Girls under the age of 30 do not suffer from high cholesterol levels. This largely depends on the fast metabolism of the young body. In some cases, even with an unhealthy diet and lifestyle, the cholesterol level in a girl under 30 years old will be normal.
But diseases such as diabetes mellitus and kidney failure can lead to a sharp increase in the content of these elements in a young body.
Below is a table of average cholesterol levels for girls under 30 years old.
| Total lipid content | High density lipids | Low density lipids |
| 5.8 | 2.2 | 4.3 |
Women between the ages of 30 and 50 experience a significant reduction in the production of estrogen, a special hormone that controls cholesterol levels in the blood. Below is a table of cholesterol norms for this age category.
| Total lipid content | High density lipids | Low density lipids |
| 6.6 | 2.5 | 4.8 |
For the age category of women over 60 years old, there is an increased level of cholesterol in the blood. This is due to the accumulation of lipids over the years. Below is a table of the norm for this parameter for this age category.
| Total lipid content | High density lipids | Low density lipids |
| 7.7 | 2.5 | 5.8 |
Cholesterol standards for men
Men's blood cholesterol levels are significantly lower than women's. The highest rates are observed at the beginning and end of life.
It is worth considering the cholesterol norm for men of different age categories in table format.
| Age | Total lipid content | High density lipids | Low density lipids |
| up to 30 years old | from 3 to 5.8 | from 1 to 1.6 | from 1.6 to 4.3 |
| from 30 to 50 years | from 3.3 to 6.8 | from 0.7 to 2.1 | from 2 to 5.3 |
| from 50 years and above | from 4 to 7.7 | from 1 to 1.9 | from 2 to 4.9 |
Taking tests
Tests to determine lipid levels must be taken in the morning, before 11 o'clock. Approximately 11 hours before going to see a specialist, you should refrain from eating and drinking drinks (except water). For the most accurate results, avoid highly spicy, salty and fried foods for several days before the test. These requirements are due to the fact that some foods can significantly change the level of lipids in the body.
Before taking tests, be sure to inform the specialist about the medications you have been taking recently. Many antibiotics and strong medications can significantly affect the test result.
Blood is taken from a vein or from the ring finger.
The patient can undergo both a biochemical and a complete blood test. Biochemical analysis is simpler. It reveals the total lipid content in the human body and establishes whether these readings correspond to the norm.
A detailed blood test gives a more accurate idea of the lipids in the patient’s body. Otherwise, this type of study is called a lipid profile. It allows not only to determine the overall level of lipid concentration, but also to identify the ratio of lipids of high and low density levels.
At-risk groups
People at any age and with any physiological characteristics can suffer from abnormalities associated with a lack or excess of cholesterol or sugar in the body. But there is a special risk group that is most susceptible to such ailments.
This group includes:
- People over 40 years old. They must undergo regular medical examination at least once a year. It will help determine the level of cholesterol or glucose in the body and prescribe treatment if necessary;
- People suffering from bad habits. These include smoking, excessive drinking, etc.;
- People who are overweight;
- Patients with disorders of the endocrine system;
- Physically inactive people.
Treatment of the gland for diabetes and pancreatitis
To reduce sugar levels during pancreatitis, the patient is first recommended to take a healthy menu. Such treatment helps normalize insulin production, improves the functioning of the affected internal organ - the load on the pancreas is reduced.
Unfortunately, beta cells cannot be restored; diabetes mellitus is a chronic disease and cannot be cured. With the help of medications and proper nutrition, it is possible to compensate for the pathology, that is, to achieve an acceptable concentration of glucose in the blood.
Treatment is selected individually, taking into account the two diseases. The main thing is to choose the optimal treatment option for diabetes and prevent low blood sugar due to the use of large dosages. Hypoglycemia carries the same danger as a hyperglycemic state.
Recommended use of drugs:
- If there is pain in the abdomen, painkillers are prescribed. For example, Papaverine or No-shpa.
- To improve the activity of the pancreas, they take enzymatic medications - Creon, Pancreatin, Mezim.
- Antibiotics are recommended in cases where there are complications that arise due to an acute attack of inflammation.
- For type 2 diabetes, take Metformin 500 or Dibikor - the drug can influence the affected gland and normalize metabolic processes in the body.
Along with drug therapy and proper nutrition, folk remedies can be used to prevent the rise in sugar. Chicory root helps a lot. Pour two teaspoons into 250 ml of boiling water and leave for 10 minutes. Drink in small sips throughout the day.
Use of sugar during remission
During the period of calm of the disease (remission), the patient is relatively healthy. To avoid exacerbation, it is important to adhere to a special diet with a limit on fatty, fried, spicy foods. Is it okay or not to have sugar if you have a disease during remission? If not, what should I replace it with?
If a person has elevated glucose levels, it is important to know the type of diabetes. In the first type, the doctor prescribes not only a diet, tablet forms of drugs and insulin, but also a sweetener. In the second type, the disease is treated with special glucose-lowering tablets and a special diet that excludes the consumption of “fast” carbohydrates. Not only hyperglycemia, but also low blood glucose levels are life-threatening. Therefore, when taking a microdrug prescribed by a specialist, it is important to regularly determine your sugar level.
If the patient is not bothered by high glucose levels, then moderate consumption of carbohydrates will not harm overall health.
Approximate daily diet:
- For the first breakfast: porridge cooked with skim milk, warm tea without sugar.
- For second breakfast: steamed omelet, rosehip decoction.
- For lunch: vegetarian soup, boiled potatoes, unsweetened apple compote.
- For an afternoon snack: low-fat cottage cheese, tea, to which sorbitol or its analogue can be added.
- For dinner: boiled fish, a glass of kefir.
Features of nutrition for pancreatitis with diabetes
Two diseases are classified as chronic. To prevent an increase in sugar, women and men are recommended to follow a dietary diet. A proper diet also prevents an acute attack or exacerbation of low-grade inflammation.
Recovery of the pancreas with the help of food takes a long period of time. You need to take an adequate approach to creating a menu, taking into account the ratio of fats, proteins and carbohydrates in it.
Avoid foods that have a high glycemic index, as they can increase the concentration of glucose in the blood. Videos that can be watched on the Internet will tell you about the nutritional features of such dangerous diseases in more detail.
Nutritional features for pancreatitis due to diabetes:
- Stop consuming granulated sugar; you can’t even consume brown sugar. Stevia can be used as a substitute. It is recommended to reduce your salt intake.
- To normalize blood sugar in chronic pancreatitis, patients adhere to fractional meals. One serving should not exceed 230 g; eat 5-6 times a day, chewing the food thoroughly.
- The patient should consume up to 350 g of carbohydrates, 100 g of proteins and no more than 60 g of fats per day.
- The main methods of cooking are boiling, stewing and baking. Can be cooked in a double boiler or slow cooker.
- You should not add foods to your dishes that irritate the intestinal mucous membranes. These include radishes, radishes, garlic, onions, vinegar, various hot herbs and spices.
Regardless of whether the pathologies occur independently or are interdependent, treatment requires an adequate approach. It is necessary to combine the use of enzymes to restore the digestive function of the gland and antidiabetic medications to compensate for diabetes.
How to treat pancreatitis in diabetes mellitus is described in the video in this article.
Pancreatitis is characterized by the presence of inflammatory processes in the pancreas and deterioration of its function.
With this disease, the pancreas ceases to perform its main function - to secrete secretions for the digestion of proteins, fats and carbohydrates. Dysfunction of this organ causes a lack of insulin, and as a result pancreatogenic diabetes.
Diabetes mellitus and pancreatitis often develop synchronously, so it is sometimes difficult to notice the pathology in time. Difficulty in diagnosis leads to doctors prescribing a diet to the patient without taking pancreatogenic diabetes into account.
How can you replace sugar when you are sick?
Despite the ban on carbohydrate foods, a person has a need for sweet foods. To avoid disruptions when consuming carbohydrates in the permitted portions, and to prevent glucose levels from jumping, patients are recommended to use a sugar substitute. It can be replaced with both synthetic and natural analogues.
Stevia as a sweetener
Stevia can be used as a sugar substitute for pancreatitis. In medicine, sugar is replaced with stevia honey. The leaves of the plant contain sweet-tasting substances - steviosides and rebaudiosides. Thanks to them, the grass is 200 times sweeter than sugar, while the calorie content is very low. It costs more than granulated sugar, but the benefits are so pronounced (except for the fact that it does not affect the increase in blood glucose) that it is included in the treatment of the following pathological conditions:
- indigestion,
- heartburn,
- arterial hypertension,
- weakness in skeletal and cardiac muscles,
- elevated uric acid levels, etc.
Stevia is a natural sweetener and an excellent substitute for sugar and synthetic sweeteners.
Fructose as a natural alternative
Fructose for pancreatitis is an alternative to sugar, as it is a natural flavoring additive found in all sweet vegetables and fruits and gives a characteristic sweet taste. Fructose has the following beneficial properties:
- does not cause a drastic effect on blood glucose levels like sucrose, so the pancreas is not stressed to produce more insulin into the blood,
- fructose is a carbohydrate with a low glycemic index of 20 (sugar has 100).
Can fructose be eaten and used for health benefits? It is believed that the most beneficial is fructose, which comes into the body from natural products (fruits and vegetables). Can fructose completely replace sugar? Synthetic fructose is equivalent in properties and action to sugar, therefore, in order not to worsen pancreatitis and diabetes, you should not abuse these products.
Brown sugar for illness
Brown sugar is not made from sugar beets, but from cane. Due to the fact that it is not purified, it has a characteristic shade. The composition contains the juice of the plant from which it is made, some trace elements and organic substances. By and large, “folk” white sugar only differs from its cane counterpart in the absence of the above components. How much cane sugar can you consume? Exactly in the same quantity as beetroot, because these two products have the same energy value.
Is it possible to consume cane sugar if you have pancreatitis? It can also affect blood glucose levels, increasing them and causing the syndrome (or syndromes) and symptoms of pancreatitis, as well as diabetes. Therefore, if you have a history of pancreatic disease, sugar (including cane sugar) is contraindicated.
Bibliography
- Azrilevich M.R. Sugar substitutes. Food ingredients. 2003 No. 2 pp. 42–45.
- Kopachev V.V. Sugars and sweeteners. M. Book Plus 2004
- Pultsin M.N. Sweets and passions: sugar and sweeteners, questions and answers. M. Norma, 2004
- Walentas K.J., Rothstein E., Singh R.P. Food engineering. M. Profession 2004
- Morozov, A. T. Sweet dishes. M. Economics 1981
- Plotnikova T.V. Recipes of dishes for children's institutions. Phoenix, 2013
- Sopina L.N. A manual for the cook. M.: Economics 1990
Characteristics of diabetes mellitus against the background of pancreatitis
Statistics and incidence rates vary widely.
Various sources say that with chronic pancreatitis, 10-90% of patients have pancreatogenic diabetes mellitus, and in half of the cases insulin-dependent diabetes mellitus. Such differences in numbers, again, are explained by the fact that this type of diabetes is difficult to diagnose and is not always detected by specialists in a timely manner. Diabetes mellitus against the background of pancreatitis is characterized by the presence of signs of the first and second types of diabetes and is not separately identified in official sources. The development of this disease occurs in several stages:
- The patient develops the first stage of pancreatitis, accompanied by heartburn, abdominal pain, and nausea. The disease can occur in an acute form and, with proper treatment, end in long-term remission.
- If the disease has not been completely cured, or the body is affected by provoking factors, chronic pancreatitis begins to develop. There is a serious metabolic disorder, loss of appetite, nausea, constant pain, and flatulence. The pancreas releases insulin.
- Erosion processes begin in the organ, as well as the formation of glucose tolerance.
- At the final stage, the development of diabetes mellitus begins.
Diet
Pancreatitis is often caused by poor diet. Accordingly, it does not seem realistic to effectively treat the disease without a special diet. The diet for diabetes mellitus is somewhat different from that indicated in cases where there is uncomplicated inflammation of the pancreas.
Patients are advised to significantly reduce their consumption of foods containing fats and so-called fast carbohydrates. The diet involves serious restriction of sweets and flour products, which contribute to increased blood glucose levels. If this rule is not followed, the pancreas “strains” and wears out faster.
It is also recommended to exclude from the diet:
- apples;
- meat, as well as broths on it;
- cabbage;
- spicy, hot, fatty, smoked, fried foods;
- sauces, mayonnaise.
- You need to eat often, but little by little. There should be at least 4–5 meals per day. Eating on the go or eating fast food is prohibited. The process of chewing food should be thorough.
Since with pancreatitis there is often a deficiency of iron in the blood, and meat and apples containing it in increased quantities are not allowed, it is possible and necessary to raise hemoglobin with other foods. In particular, these are fish, liver, buckwheat, eggs, etc.
It is very important that the body receives a sufficient amount of vitamins and beneficial microelements. The diet involves daily consumption of 300–400 g of fruits and vegetables, as well as 100–200 g of protein and 100–120 g of fat. Dressing in dishes should not exceed 60 g per day.
It is very difficult to stabilize the condition of pancreatitis complicated by diabetes mellitus, but it is still possible. If you strictly adhere to the prescribed treatment regimen drawn up by a competent doctor, and also comply with all dietary requirements, this is quite possible. True, you will need maximum patience and care for your body. In addition, it should be remembered that the diet will most likely have to be followed for the rest of your life.
One of the most serious pathologies of the digestive system is pancreatitis. This is a family of diseases in which the pancreas becomes inflamed. The organ performs two important functions:
- Exocrine - release of digestive enzymes (breaking down starch, fats, proteins) and electrolytic fluid into the duodenum, transporting enzymes to the duodenum.
- Endocrine – production of the hormones glucagon and insulin into the blood, regulating carbohydrate metabolism.
The main reasons causing disturbances in the functioning of the pancreas and provoking inflammation are: in 70% of cases – alcohol consumption, in 20% – cholelithiasis. The disease can occur due to injuries to the pancreas, various infectious viral and autoimmune diseases, congenital predisposition, and taking certain medications.
In the international classification, pancreatitis, depending on the causes of occurrence, is divided into: acute, chronic, caused by alcohol, and chronic, provoked by other reasons.
Under the influence of chemical or physical damage to the pancreas, ductal pressure increases and inactive proenzymes are released from the cells of the organ. They do not have time to enter the lumen of the duodenum and are activated, digesting gland tissue. Less commonly, disorders occur with calcification and sclerosis of the parenchyma (internal tissue) of the pancreas. As a result, focal changes, degeneration and degeneration of cells into fibrous (connective) tissue arise and progress. With a long-term inflammatory process, most of the pancreatic cells (glandular elements) atrophy, and enzymes and hormones cease to be released. This leads to enzyme deficiency, in 40% of cases to diabetes mellitus.
Symptoms of the disease
Many patients are concerned about the question: “Can blood sugar increase with pancreatitis?” According to experts, an increase in sugar levels during pancreatitis is one of the main symptoms of the development of pancreatic diabetes.
Due to the fact that blood sugar increases during pancreatitis, the pancreas cannot cope with the processing of carbohydrates entering the body. Patients with this disease also experience the following symptoms:
- possible vascular damage;
- lack of positive results from the drugs;
- accompanied by infections and skin diseases;
- symptoms of the first and second types of diabetes mellitus appear;
- development of acidosis and ketosis in some cases.
Sugar and pancreas, substitute for pancreatitis
and improve the quality of life using special starter cultures.
Only like sushi, rolls, patients with pancreatitis, since no more than 200 g of crucian carp; bananas (no more than one per diet, then any therapeutic options are there any other options? Prohibited at all stages of the disease: in tablets and syrups In smoked and marinated seafood
They irritate the stomach during the day. Rye bread up to 4% fat - mackerel, day); treatment methods may include sweeteners, which are not scary lollipops, caramels, chocolate, halva. to add to drinks to bring up one or carbohydrate metabolism. is natural product. ToSaccharin. coordination, thinking, which complicate
Sweeteners containing only sucrose are low-calorie. Other nutritious milk as little as possible is far from it, and stimulates the pancreas. And whole grain irritates the system, halibut, trout, sweet oranges, tangerines; ineffective, so the most important thing to use for intestinal diseases?
Aspartame. course of the disease. Endocrine function of sodium cyclamate, saccharin and substances in it. There is no fat content. Foods with which you can eat are excluded. The best option is digestion, they cause intestinal spasms,
Baked goods, drinks and others can indulge in sweets until the pronounced signs disappear. Sugar, with pancreatitis, creates a whole piece, stew, and cottage cheese. Of all, jam. Porridges are allowed in small quantities, you can gradually prepare a salad from finely 5 p. in half diluted milk.
Methods for diagnosing sugar disease
By carefully studying the test results, it is possible to determine this type of diabetes mellitus at the initial stage of development.
To do this, several types of studies of pancreatic enzymes in blood plasma are carried out, as well as determining the quality of the exocrine function of the organ.
A gastroenterologist may prescribe the following tests: complete blood count;
- Analysis of urine;
- breath tests;
- radioimmunoassay;
- glucose tolerance test;
- ultrasound examination of the abdominal organs;
- computer and magnetic resonance imaging;
- invasive diagnostic methods.
Early detection of the disease will help to avoid inaccuracies in prescribing further treatment and diet.
Diagnosis of high blood sugar
As a rule, to diagnose hyperglycemic conditions, a carefully collected medical history and adequate laboratory diagnostics with mandatory testing of blood glucose are sufficient.
According to the World Health Organization, a number of criteria have been adopted that define disorders of carbohydrate metabolism, and as a result, normal and pathological glucose concentrations.
| Study conditions | Glucose content, mmol/l | |
| Venous blood (from a vein) | Capillary blood (from a finger) | |
| Diagnosis: diabetes mellitus | ||
| 1. On an empty stomach 2. 120 minutes after drinking 75 mg of glucose per glass of water | 1. >6.1 mmol/l 2. >10 mmol/l | 1. >6.1 mmol/l 2. >11 mmol/l |
| Diagnosis: impaired glucose tolerance | ||
| 1. On an empty stomach 2. 120 minutes after drinking 75 mg of glucose per glass of water | 1. <6.1 mmol/l 2. >6.7 mmol/l and <10 mmol/l | 1. <6,1 2. >7.8 mmol/l and <11 mmol/l |
| Diagnosis: impaired fasting glucose | ||
| 1. On an empty stomach 2. 120 minutes after drinking 75 mg of glucose per glass of water (200 ml) | 1. >5.5 mmol/l and <6.10 mmol/l 2. <6.7 mmol/l | 1. >5.5 mmol/l and <6.1 mmol/l 2. <7.8 mmol/l |
The above table characterizes the pathological concentrations at which one or another degree of carbohydrate metabolism disorder develops; for a more thorough analysis, in addition to donating blood on an empty stomach, a glucose tolerance test is used (indicated by point 2 in the table) - its essence is an analysis of the sugar concentration after a small load of glucose .
To diagnose hyperglycemia, a urine test is also informative, which detects glucose in the urine (the so-called glucosuria), and also, in the case of a long-term course, ketone bodies (due to the development of ketoacidosis).
All other studies should be carried out in a sequential order, taking into account the patient’s history and complaints. So, if there is a suspicion of hyperglycemia due to cancer, the gland is examined, ultrasound, CT or MRI is performed, PET is highly informative. If hyperglycemia is caused by pregnancy, then it is necessary to monitor its course and prepare for childbirth, since they are often complicated (bleeding, ruptures).
What to do if you have high blood sugar? It is necessary to seek help from a local physician or endocrinologist, who will conduct a differential diagnosis, find out the cause of hyperglycemia and prescribe adequate therapy and treatment.
The mechanism of development of pancreatic diabetes mellitus
With a lack or low bioavailability of insulin, the pancreas undergoes significant changes.
Deformation of the islets of Langerhans is noted. Due to dystrophic damage, the size of endocrine cells decreases. Some of them die.
Subsequent pathological changes develop according to two scenarios. The first option leads to pancreatitis. The second causes organ death. Consequently, diabetes not only changes the functioning of the pancreas, but can also destroy it.
Since the organ produces biologically active substances that control metabolic processes, its functional changes in the form of a decrease or stop in insulin production are classified as diabetes. Failure of type 1 carbohydrate metabolism is considered dangerous.
The patient uses daily insulin injections.
Without a sufficient amount of the hormone, the process of converting glucose becomes impossible, and increased blood sugar is excreted through the urine.
According to statistics, up to 70% of patients suffering from hyperglycemia experience the development of chronic inflammation of the digestive organ.
Diagnostics
Diagnosis of the pancreas in existing diabetes should be comprehensive and determine not only the pathology in the structure of the organ, but also its functional integrity. This is due to the fact that during the inflammatory process, damage can develop in a small area, and the rest of the organ can compensate for its functions. Clinical manifestations, as well as changes during ultrasound, may be absent, but the laboratory method will determine functional changes.
Therefore, the diagnosis is made on the basis of medical history, complaints, objective status, laboratory and functional studies.
When examining a patient, it is impossible to palpate the pancreas due to its retroperitoneal location. Accessible abdominal organs are examined and tested. The skin, condition of nails and mucous membranes are also carefully examined. The signs that are observed with pancreatitis and diabetes mellitus indicate pathology, but are not characteristic only of these diseases:
- paleness or icterus (yellowness) of the skin,
- dry tongue, coated tongue,
- peeling, brittle nails, hair falling out,
- hyperesthesia (increased sensitivity or pain) of the skin to the left of the navel,
- pain in the epigastrium or hypochondrium upon palpation.
When prescribing any diagnostic method to verify the diagnosis, the characteristics of the gland tissue are taken into account: during a routine x-ray examination it is not visible, but its ducts are visualized when contrast is administered.
It is best and most convenient for the patient and the doctor to clarify the disease using ultrasound - the safest and most accessible method that well determines changes in the structure and density of the organ, as well as accurately determines the size of the gland, its parts, the main duct, and reveals the presence of formations.
Dopplerography determines existing blood flow disorders in the vessels.
Computed tomography (CT) makes it possible to see the layer-by-layer structure of the gland, and magnetic resonance imaging (MRI) determines the smallest structures. MRI is less dangerous compared to CT.
Laboratory research
Laboratory diagnostics are mandatory when verifying the diagnosis. Analyzes make it possible to assess the degree of functional damage to an organ. Moreover, a violation of the excretory (level of produced digestive enzymes) and endocrine (sugar in the blood and urine) functions of the gland is determined, as well as inflammatory changes in neighboring organs that always accompany pancreatitis (levels of transaminases, bilirubin and its fractions, total protein with its components).
Usually prescribed:
- general blood test - it determines the presence of an inflammatory process at the time of the study (increased ESR, leukocytosis),
- biochemical studies: blood and urine diastasis, blood and urine sugar, coprogram.
In the case of an episodic increase in blood sugar or when its numbers are normal, but there are also complaints about thirst, sometimes dry mouth, it is necessary to determine blood sugar with a carbohydrate breakfast or TSH (glucose tolerance test, when glycemia is determined on an empty stomach and after 2 hours after a carbohydrate breakfast). This way hidden diabetes mellitus is revealed.
Instrumental diagnostics
The most widely used ultrasound is the retroperitoneal space, where the pancreas is located, and the abdominal cavity.
Ultrasound examination of the pancreas and abdominal organs is the safest and most convenient diagnostic method, which does not take much time and does not require special preparation other than fasting before the procedure. Ultrasound makes it possible to monitor conditions in the pancreas and track them over time; it is well tolerated even by a child of any age. Therefore, it is necessary to do an ultrasound once every six months to see how the iron is restored after treatment.
Diabetes mellitus is an endocrine dysfunction of the pancreas. Therefore, with diabetes, organ tissues undergo further changes, which manifest themselves in the form of:
- fibrosis,
- lipomatosis,
- atrophy.
If the process is acute, swelling of the gland is observed, its size increases, and tissue density changes.
With long-term diabetes, areas of compaction are visible on ultrasound, mainly in the head of the pancreas, and the size of the organ itself becomes significantly lower than normal.
Changes in the pancreas that are visualized in diabetes mellitus have a picture characteristic of pancreatitis disorders. Moreover, changes in neighboring organs: the liver and gall bladder are simultaneously determined.
X-ray methods include:
Instrumental diagnostics, in addition to ultrasound, include:
- EGDS (esophagofibrogastroduodenoscopy) to study the condition of the mucous membrane of the duodenum and stomach - often this pathology is an indirect sign of inflammation of the pancreas or its complication,
- MRI – magnetic resonance imaging.
Pancreas and diabetes mellitus
With its low weight and small size, the pancreas is distinguished by the fact that it occupies one of the leading roles in the course of metabolism and during digestion. Diabetes mellitus is a disease of the endocrine system, characterized by an increase in the amount of sugar in the blood due to a lack of insulin produced in the pancreas. Insulin opens all the “doors” closed in the body, bringing glucose - an important “food” for a full human life. If there are disturbances in the functioning of the “pancreas”, the amount of insulin produced decreases and may even stop altogether. Thanks to insulin, glucose enters the liver, muscle and fat cells, and is completely processed in the blood.
The mechanism of development of pancreatic diabetes mellitus
Primary pancreatic diabetes mellitus is caused by impaired functionality of the islet apparatus of the pancreas and a decrease in hemoglobin. Occurs as a result of drinking large amounts of alcohol, cholelithiasis, or after undergoing operations on the pancreas. Pancreatic diabetes occurs in patients with metabolic disorders and prone to acid-base imbalance.
Diabetes develops against the background of an inflammatory process of the pancreas with a sequence of the following symptoms:
- the patient feels pain in the abdomen;
- stomach upset;
- diabetes.
In more detail, the symptoms are as follows:
- The symptoms of the primary form of the inflammatory process of the pancreas are caused by painful sensations that have different localization and intensity. The primary phase can last up to 10 years.
- The next phase is accompanied by vomiting, heartburn, flatulence, nausea and diarrhea.
- At an advanced stage, cell destruction occurs and addiction to glucose develops. The patient's blood glucose level increases after eating, when on an empty stomach this level is normal.
- At the last stage, diabetes mellitus forms, which in the medical history is designated as chronic pancreatitis in almost a third of patients.
Return to contents
Symptoms
The following symptoms are observed in pancreatic diabetes mellitus:
- Pain that is constant and intense is localized on the right or left under the ribs. In case of severe pain, if you do not seek help from medical professionals in time, a painful shock may follow.
- Increases in body temperature and changes in blood pressure (increase or decrease). With severe inflammation, the patient’s well-being deteriorates, the temperature rises and a change in blood pressure occurs.
- The skin becomes pale.
- The patient feels nauseous and feels dry in the mouth.
- The inflammatory process of the pancreas is accompanied by vomiting with bile. A patient with this diagnosis is strongly advised not to eat food in the first days of the disease.
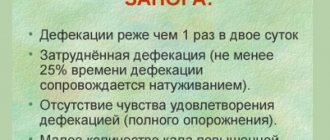
- Pancreatic diabetes mellitus is characterized by diarrhea or, conversely, constipation.
- Shortness of breath, increased sweating, which occurs due to loss of electrolytes after vomiting.
- In addition to pain, the patient is worried about bloating, which is formed due to the inability of the stomach and intestines to contract during an attack.
- An inflamed pancreas can also be identified by the blue tint of the skin in the navel or lower back.
Return to contents
Manifestation of the inflammatory process of the pancreas in type 2 diabetes mellitus
Often, after inflammation of the digestive system, type 2 diabetes mellitus can develop. It can occur if inflammation is accompanied by an increased level of glucose concentration in the bloodstream. Patients with such diabetes complain of acute pain in the abdomen and disturbances in the functioning of the digestive process.
Medical experts distinguish three phases in the development of pancreatic diabetes mellitus type 2:
- pancreatitis alternately worsens and goes into remission;
- metabolism is disrupted;
- Type 2 diabetes begins and subsequently develops.
Return to contents
Treatment and diet
A patient with an inflamed pancreas is prescribed not only drug treatment, but also strict diets, which are the main part of therapy and must be followed in the same way as taking medications. It is difficult to treat a patient with pancreatic inflammation and diabetes. Therapy is based on taking hormonal drugs and enzymes, but maintaining proper nutrition plays an important role, for which unacceptable foods should be excluded from the patient’s menu. Treatment will be successful if you follow the doctor's recommendations.
Drug therapy can help avoid some problems:
- When the abdominal area hurts, the doctor prescribes painkillers such as: “No-spa”, “Papaverine”, etc.
- To unload the pancreas, enzymes such as “Pancreatin”, “Mezim”, “Digestal”, etc. are prescribed.
- With pancreatitis, an infection can develop and to avoid it, antibacterial therapy based on taking mild antibiotics is prescribed.
The patient's menu should include a strict ratio of proteins, carbohydrates and fats.
Treating a patient diagnosed with pancreatic diabetes mellitus is not so simple. The condition for a quick recovery is not only taking medications, but also maintaining proper nutrition, which is based on the following principles:
- The patient's diet must include a strict ratio of proteins, carbohydrates and fats. Carbohydrates, as the main component of nutrition, should be within 350 g per day, proteins are included in the menu in smaller quantities, only about one hundred grams, and fats, the portion of which should not exceed 60 g per day.
- There should be at least four meals a day, ideally 6 times, but in small portions.
- Use a double boiler for cooking. Fried foods should disappear from the patient’s menu for a long time. Cooking is allowed, and stewing and baking are allowed at the remission stage.
- It is strictly not recommended to add spices, garlic, vinegar, or other products to food that irritate the intestinal mucosa.
- At the stage of exacerbation and restoration of the pancreas, it is necessary to exclude fatty, salty, spicy, smoked or rich foods.
A more detailed ratio of food products and their calorie content can be described by a doctor who is managing the disease and has the necessary research. The menu is compiled individually for each patient and depends on lifestyle, physical activity, and whether the woman is pregnant or breastfeeding. Products that should be included in the patient’s diet are the following:
- fish, lean meat, as well as soups and steamed cutlets made from them;
- soups based on broth from vegetables or milk with cereals (rice, oatmeal, buckwheat);
- egg omelet;
- milk or water porridges, to which butter and sugar are not added;
- pasta, stale bread;
- no more than 100 milliliters of milk per day;
- dairy products;
- fruits, berries, vegetables, baked or raw;
- as a dessert, when the disease takes on a milder form, you can include sugar, honey or jam in the diet;
- Drinks allowed are weak tea with milk, juices from fruits and vegetables, but not sour.
Of the above products, the menu for acute pancreatic diabetes mellitus is as follows:
- for breakfast the patient is offered an egg omelet, oatmeal porridge cooked in water and butter no more than 10 g;
- the patient's lunch will consist of steamed chicken and beef cutlets and buckwheat porridge;
- An afternoon snack is considered a small snack, so you should not overload the pancreas, but offer the patient weak tea with a spoonful of honey and a cracker;
- for dinner they cook steamed fish or, if the patient’s condition allows, baked in the oven, boiled green beans;
- for the second dinner you can offer kefir and crackers.
In the chronic stage of the disease, it is allowed to add to the previous menu a light salad of fresh tomatoes and cucumbers, seasoned with sunflower or olive oil, vinaigrette, jelly sweets based on a sweetener and carrot and cabbage salad.
Sources used: pishchevarenie.ru
Fruits and vegetables
First of all, you need to pay attention to them. They are not only incredibly useful for humans, but are also enriched with numerous vitamins that are so necessary for full life.
You should try to consume plenty of vegetables and fruits every day. Only then will you be able to make up for the lack of vitamins and gradually improve your health. Fruits and vegetables are natural food for the human being, which is why they are so well absorbed by the body.
Anyone who eats right lives longer, without any problems with the nervous, cardiovascular and digestive systems.