Dysbacteriosis in a breastfed baby is not an independent disease: it is a consequence of an imbalance between beneficial and pathogenic microorganisms inhabiting the intestines. This diagnosis is made to approximately half of children under the age of one year, and most often infants who were born prematurely suffer from dysbiosis. Naturally, any diagnosis given to a baby frightens parents and forces them to look for information about the disease discovered by the pediatrician. There is no need to panic, but information about how dysbiosis manifests itself and how it should be treated will not be superfluous.
What is dysbiosis?
By definition, dysbiosis is an imbalance of normal and harmful microorganisms inhabiting the intestines. Due to dysbacteriosis, the work of the gastrointestinal tract becomes significantly more difficult.
There is normally no microflora in the stomach and duodenum. However, the further the gastrointestinal tract is from the stomach, the more bacteria of all kinds live in it. The intestines are populated by lactobacilli, fungi, staphylococci and streptococci. Bacteria take an active part in digestion: a sterile intestine would not be able to digest food. Sometimes the intestinal microflora is called an accessory organ. And this is not surprising: the weight of bacteria that live in the intestines of an adult reaches 1.5 kg!
In some cases, the balance of microflora is disturbed, and the pathological condition resulting from this disturbance is called dysbiosis.
Prevention measures
In order not to fight dysbiosis, it is better to prevent it, so prevention occupies a special place. The main ways to prevent the disease include:
- correct use of antibiotics only as prescribed by the attending physician;
- parallel use of prebiotics with antimicrobial drugs;
- balanced nutrition and diet, it is better to eat smaller meals and in small portions;
- restorative therapy in the presence of chronic gastrointestinal diseases, normal functioning of all organs should be restored;
- daily consumption of fermented milk products;
- maintaining a healthy lifestyle.
It is worth understanding that all these measures may be useless if dysbiosis occurs due to any disease, so you should constantly strengthen your immune system and take care of the general condition of the body, trying to cure all chronic diseases. It is also important to pay attention to the psychological state of the child.
The somatic causes of dysbiosis in children have not yet been studied very well, but the connection between the state of the nervous system and the gastrointestinal tract is definitely evident. If a child does not communicate with peers, is embarrassed about his photo because of acne, or leads a secluded lifestyle, he is at risk for dysbacteriosis.
Loading…
Share with friends!
https://youtu.be/YLZxlD6NNE4
Formation of intestinal microflora
The baby is born with a sterile intestine: there are no bacteria in it. The first “meeting” with the maternal microflora occurs at the moment the child is born. Passing through the birth canal, the child “receives” microorganisms that will later populate his intestines and become faithful helpers, contributing to the normal course of digestive processes.
After the baby is born, the mother puts him to the breast. At this moment, he receives liquid colostrum, which contains substances that positively affect the development of bacteria necessary for the normal functioning of the gastrointestinal tract.
Within a week after birth, bacteria, including pathogenic ones, colonize the baby’s intestines. However, due to the fact that the child receives immunoglobulin with mother’s milk, he feels excellent: the body copes with pathogenic microbes, and the microflora comes into a balanced state. Sometimes, due to the presence of pathogenic bacteria in the body in the first days of life, a child may experience a so-called transit form of dysbacteriosis, manifested in the form of colic, regurgitation and watery feces with mucus inclusions. Such a disorder does not require medical intervention: just wait a little, and the baby will return to normal.
By the end of the first week of life, beneficial microorganisms completely replace pathogenic ones. As a result, the baby’s well-being returns to normal.
The final balance between beneficial and harmful bacteria is established when the child reaches one month of age.
The intestine and its “inhabitants”
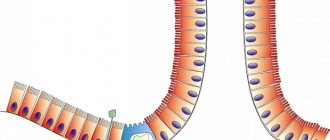
Having been born, a child comes from the absolutely sterile environment of the mother’s body into a world populated by a huge number of different microbes. It cannot remain sterile for long. Almost immediately after birth, his body begins to be populated by representatives of the microbial world. The baby’s intestines are partially colonized by microbes during the birth process, when the baby moves through the mother’s birth canal. After the first portion of food enters the stomach, the intestines become the habitat of many microorganisms. Their number gradually increases and eventually becomes so significant that for every 3 grams of a child’s stool there is 1 gram of microbes! The presence of so many microbes in the intestines is very useful not only for microbes, but also for humans. Such mutually beneficial coexistence of the human body and the microbes existing in its intestines is called symbiosis .
All intestinal microorganisms are divided into two groups. The first group is called obligate flora . These microbes must be present in the intestines. It consists of microbes, without which there can be neither normal digestion, nor stable immunity, nor good health. These are bifidobacteria, lactobacilli and E. coli. This group also includes saprophytic bacteria that do not have any effect on human health - neither positive nor negative. These are bacteroides and enterococci. The group of obligate microorganisms is the largest, accounting for about 97% of the total number of intestinal microbes.
The second group is called facultative flora . Its presence in the intestines is not necessary. Moreover, under unfavorable conditions, which include decreased immunity, infections, stress, trauma, dietary errors, microbes from this group can become pathogenic (disease-causing) and, multiplying in large numbers, cause clinical manifestations of intestinal infection. Among them there are microorganisms called opportunistic pathogens (clostridia, Klebsiella) and microorganisms that should not normally be present in a child’s intestines. These are staphylococci, proteus, yeast fungi of the genus Candida. Being conditionally pathogenic for an adult, they certainly become pathogenic for an infant, that is, if in an adult these microorganisms will cause disease I only in certain cases, then in a child they always do.
Speaking about the microbes that live in the intestines, we cannot help but dwell especially on the group of beneficial microbes. These are lactobacilli and bifidobacteria , which are the number one protective factor. Existing in the intestines, they, firstly, create conditions there that are completely unsuitable for the life of pathogenic microbes. Thus, through their vital activity they provide protection to the intestines from excessive growth of opportunistic and pathogenic microorganisms. Secondly, these microbes stimulate the child’s immune system to produce its own immunoglobulins - a reliable shield against infection from the outside. Thirdly, bifidobacteria and lactobacilli promote the production of natural vitamins in the intestines, such as B6, B12 and folic acid. Fourthly, these microorganisms promote the absorption in the intestines of such important food components as iron, calcium and vitamin D. And finally, they stimulate intestinal peristalsis (motor function).
The correct ratio of the number of bacteria in the intestines is very important; if it is disturbed, immunity decreases, which means the risk of intestinal infections increases, hypovitaminosis occurs, anemia may develop due to insufficient iron intake and rickets due to a deficiency of calcium and vitamin D. Here in what is the meaning of this symbiosis, this is the price microorganisms pay us for the honor of existing with us!
Advertising
Causes of disease development in an infant
Children born prematurely, as well as weak babies, may develop a condition that doctors call the primary form of dysbiosis. Dysbacteriosis in breastfed infants is provoked by the following factors:
- refusal to breastfeed the baby and early transition to breast milk substitutes;
- taking by a breastfeeding mother antibiotics or drugs that contain hormones;
- infection of a nursing mother with a nosocomial infection, for example, Staphylococcus aureus. Staphylococcus passes into breast milk and infects the baby's intestines;
- abuse of any complementary feeding product, for example, mashed potatoes;
- in children who have reached the age of 10-12 months, the cause of dysbiosis can be infection with helminths;
- severe stress experienced by the child, or his stay in unfavorable socio-psychological conditions.
Diagnostic methods
Changes in the behavior of a child and a schoolchild should alert parents. There are more and more cases when a teacher brings a child to the pediatrician. Any complaints of abdominal pain should not leave close adults indifferent.
To accurately confirm dysbiosis, an examination is necessary:
How to properly test stool for dysbacteriosis?
- Bacterial analysis of stool and examination of intestinal flora. Feces are collected in a sterile jar and delivered within two hours to the laboratory for culture. If this condition is not met, then it is impossible to judge the reliability of the results, since some of the bacteria will die.
- Examination of stool for coprogram allows you to check the progress of food digestion in the intestines.
- Ultrasound of the abdominal organs is necessary to exclude primary pathology and congenital structural abnormalities.
- General blood tests indicate the absence of anemia. Biochemical tests are carried out to detect damage to the liver and pancreas.
If necessary, the doctor prescribes a more “targeted” examination of the organs. If the symptoms are unclear, in order to find out how to treat dysbiosis in a baby, sometimes it is necessary to examine the nursing mother.
How to recognize the disease?
Usually, observant mothers and fathers quickly notice that the baby is suffering from unpleasant manifestations of dysbiosis and go with the child to the doctor. However, it is important to remember that only a specialist can make a diagnosis: self-medication can lead to symptoms getting worse.
Pediatricians call these characteristic symptoms of dysbiosis in a newborn baby:
- severe lethargy and lethargy;
- paleness of the skin;
- the appearance of an unpleasant putrid odor from the mouth;
- every feeding provokes colic;
- drying of the skin and the appearance of a rash;
- poor appetite: after taking a few sips of milk, the child immediately abandons the breast and begins to cry. This is due to the peculiarities of the anatomical structure of the baby’s intestines: if there are any pathogenic processes, even a small amount of food causes severe discomfort;
- stomatitis or the appearance of rashes on the mucous membranes of the oral cavity;
- frequent regurgitation, nausea and vomiting;
- the presence of foam or mucus in the stool is a serious sign of indigestion.
Sometimes similar symptoms are observed when complementary foods are introduced. However, after the baby’s intestines adapt to the new food, the manifestations of dysbiosis disappear on their own, without requiring special intervention.
The manifestation of dysbiosis in an infant can be in the form of a whole range of symptoms, for example, diarrhea, constipation, skin rash, etc.
Cause-and-effect relationships of dysbiosis
Thus, the main reason for the development of this disease is the lack of beneficial bacteria in the intestinal microflora of a growing organism.
Thus, primary intestinal dysbiosis in an infant can develop as a result of a refusal to:
- From breastfeeding;
- Early transfer to artificial nutrition: infant formula;
- During lactation, the mother takes antibiotics, hormonal medications, as well as food containing them.
Secondary dysbiosis has an identical origin, but is formed against the background of slightly different factors. Thus, secondary dysbiosis is a consequence of:
- Stomach diseases in an infant;
- Use of antibiotics in the treatment of a child;
- Enzymes for digestion are produced in insufficient quantities;
- Intestinal motility disorders;
- Incorrect feeding;
- Infectious infections;
- Injuries during childbirth;
- Mastitis and infectious diseases in mother.
The most common cause of dysbiosis in newborns is infection with Staphylococcus aureus. It is essentially a hospital-acquired infection that most infants contract. The risk of dysbiosis occurs with hormonal therapy and antibiotics, even if a nursing mother is undergoing treatment.
Why is dysbiosis dangerous in infants?
Interestingly, large-scale studies of dysbiosis in infants began only ten years ago. And not all doctors agree with the existence of such a diagnosis: many believe that dysbiosis just needs to be waited out, and gradually digestion will return to normal. Nevertheless, under no circumstances should dysbacteriosis be caused, if only because this condition can force the baby to refuse food for a long time. As a result, the child has to be hospitalized and even fed with a tube or intravenous fluids. If treatment of dysbiosis is started at an early stage, it can be dealt with in a few weeks.
Advanced dysbiosis during breastfeeding can cause quite serious problems:
- due to the fact that food is not digested properly, the baby becomes weaker and develops worse;
- the intestines are constantly irritated, which in the future provokes the development of dangerous diseases, for example, ulcers or gastritis;
- pathogenic microflora can spread to the entire intestine, as a result of which proteins, fats and carbohydrates necessary for the development of the baby will not be absorbed from food;
- Due to dysbacteriosis, immunity decreases, resulting in the creation of a favorable environment for the development of infectious diseases.
Symptoms of dysbiosis at varying degrees of severity
Conventionally, dysbiosis can be divided into 4 degrees of severity. The first two are not considered clinical and are usually asymptomatic, but stages 3 and 4 are characterized by the presence of certain symptoms. Signs of dysbiosis in children:
- Abnormal stool. Most often, children experience diarrhea, but in some cases, the child, on the contrary, begins to suffer from constipation. The main cause of diarrhea is that water absorption deteriorates due to increased peristalsis and disruption in the synthesis of bile acids. If you miss this sign at the very beginning, diarrhea will acquire an unpleasant putrefactive odor, mucus impurities will appear, and then blood (we recommend reading: what does putrid odor from a child’s mouth mean?). If the child’s intestinal flora is too weak, constipation may develop, which at first is not always identified as dysbiosis. In some cases, alternating constipation and diarrhea can be observed.
- Stomach ache. It is usually cramp-like due to a sudden increase in pressure. When the gases in the abdomen are released, the pressure decreases and the pain disappears. If dysbiosis has affected the small intestine, the discomfort will be localized near the navel; if there is pathology of the large intestine, the right lower abdomen will begin to hurt.
- Bloating, which occurs due to the formation of gases in the large intestine as a result of impaired absorption and excretion of substances by the altered intestinal wall. Externally, this symptom is expressed in the rumbling of the stomach.
- Dyspeptic disorders. These include nausea, vomiting, belching and even loss of appetite.
- Often the temperature with dysbacteriosis in children reaches 38 or even 39 degrees. This is due to increased intoxication of the body and accumulation of metabolic products. Often, as the temperature rises, the child’s head and stomach begin to hurt. The baby often gets tired, sleeps poorly and refuses to eat. Low-grade fever should also confuse parents.
- Allergy to toxins and rotting products. It is expressed in the form of itching, redness of the skin, acne, and even swelling of some areas of the face and eyes. Any rash indicates problems with the gastrointestinal tract.
- Vitamin deficiency in dysbiosis. Depending on which vitamins are lacking in the body, it can be expressed in stomatitis, thrush, increased dryness of the skin, decreased elasticity of the epithelium, brittle nails and hair, as well as pale skin after sleep.
- Loss of body weight. As a rule, a sick child sharply loses weight or simply stops “getting heavy” and does not meet his age standards.
- Bad breath (we recommend reading: causes of bad breath in a 7-year-old child). If a child brushes his teeth twice a day, but his breath smells bad and even putrid, and also complains of a metallic taste, this indicates the development of the disease.
- Dysfunction of the rectal sphincter. Upon palpation, you can detect compliance of the anus. Often the child complains of pain, itching and burning in the anus.
How is dysbacteriosis diagnosed?
A stool test performed in a laboratory helps determine that a baby has developed dysbiosis. The following studies are being carried out:
- coprogram. With its help, the doctor can determine whether food is being absorbed well in the baby’s intestines. At the same time, thanks to the coprogram, it is possible to determine whether there is an inflammatory process in the child’s intestines;
- bacterial culture of stool. The analysis makes it possible to determine the ratio of pathogenic and beneficial microflora in the intestine;
- culture for dysbacteriosis. Reveals the degree of formation of the microflora of the gastrointestinal tract.
Any error in collecting material can lead to an incorrect diagnosis. You need to collect feces according to the following rules:
- Wash your baby and put a clean diaper on him. It is advisable to abandon the diaper;
- Feces should be taken for analysis immediately after it is collected;
- you need to collect feces in a special sterile container, which can be purchased at any pharmacy;
- If the child’s diet includes milk formulas containing preboitics, they should be discontinued two to three days before submitting stool for analysis.
In order for the analysis to give accurate results, parents must take care to collect it correctly
Dysbacteriosis: the essence of the disease
In medical science, there is a lot of controversy surrounding the term and, in general, such a disease as dysbiosis. Some argue that the disease is far-fetched, others attribute it to serious ailments of the intestinal microflora. The opinion of the former began to find less and less support, and the disease began to be classified as a complex disease of the digestive system.
In essence, dysbiosis is an imbalance between pathogenic and healthy microflora in the intestines, which leads to significant disruptions in the child’s digestive system. An increase in pathogenic bacteria, primarily staphylococci, fungi, streptococci, which kill beneficial or healthy microorganisms, causes disturbances in the functioning of the food digestion system.
Eating disorders and dysbiosis
It was said above that dysbiosis in infants can develop due to the wrong approach of parents to feeding the baby. Indeed, very often the reasons lie in the following:
- overfeeding A similar nuisance often occurs when the mother feeds the baby on demand. It should be remembered that the baby should eat every 2.5-3 hours. If you put your baby to the breast too often, you may experience serious digestive problems. The food simply does not have time to break down completely, as a result, stagnation begins in the intestines, which provokes an imbalance in the microflora;
- undercover Many babies are “lazy” and don’t make any effort while at the breast. As a result, they drink only the so-called “fore” milk, without getting to the “hind” milk, which is rich not only in fats and carbohydrates, but also in enzymes;
- sudden change in diet. If you abruptly wean a child from the breast and transfer him to formula milk, the body simply will not have time to adapt to the change in diet.
If dysbiosis occurs due to an intestinal infection, then treatment will require much more effort. Moreover, the younger the child, the slower the microflora will recover.
If the cause of the development of dysbiosis is the infant’s poor nutrition, then the symptoms will disappear on their own after the cause of the pathology is eliminated
Dr. Komarovsky’s opinion: this is a commercial diagnosis
Komarovsky talks a lot about dysbiosis. The pediatrician devoted several programs to explaining the causes of intestinal microflora disorders, methods for identifying the problem and methods of treatment.
Komarovsky says: “Every person has a huge number of bacteria in their intestines, which are found there in very specific concentrations, and these concentrations are specific to each person. They can change under the influence of a huge number of factors: emotional state, nutrition, environmental conditions. There are plenty of reasons for the components of the intestinal flora to change among themselves. A change in the composition of the intestinal microflora is not a cause, but a consequence.
Dysbacteriosis is not a disease. It is not treated in civilized countries. Nowhere and no one in civilized countries has any idea what an analysis for dysbacteriosis is. A huge number of drugs supposedly intended to treat dysbiosis are sold and used only where dysbiosis is treated. It’s better for parents to leave the child alone and stop treating the tests.”
The doctor says that dysbiosis in a child is not the root cause. The imbalance of microorganisms in the intestines can be disrupted due to some circumstances. Therefore, it makes no sense to drink mountains of tablets with beneficial bacteria in order to get rid of abdominal pain and improve bowel movements.
If the problem persists for a long time, then you need to look for the causes of dysbiosis. Komarovsky believes that the diagnosis of “dysbacteriosis” is made only for parents. The mother is worried that her baby is pooping somehow differently from his peers. Doctors, in turn, prescribe medications for the baby for 5-7 days. It takes approximately this amount of time for the child’s intestinal microflora to independently restore itself after the mother stops feeding him something other than breast milk.
https://youtu.be/nTBBWbRAxvg
Stages of dysbiosis
In the literature you can find a description of the four main stages of dysbiosis:
We recommend reading: Why does a newborn have diarrhea?
- first stage. Beneficial bacteria predominate in the intestines, and two types of pathogenic microorganisms are isolated in the feces. We can say that this condition is not a pathology: there are no symptoms that bother the baby, and the state of the microflora normalizes on its own. The first stage can be caused by the mother eating any new product;
- second stage. An equal amount of beneficial and pathogenic microflora is released in the feces. The child suffers from diarrhea, bloating and flatulence. In addition, the rate of weight gain decreases. Usually, for treatment it is enough to reconsider the mother’s diet or refuse to introduce complementary foods too early;
- third stage. Pathogenic microflora dominates in the intestines. Proteus, staphylococci, streptococci, etc. are found in large quantities. The baby experiences abdominal pain, diarrhea, in which particles of incompletely digested food are noticeable, and the child often suffers from nausea and vomiting. Sometimes babies develop a fever;
- fourth stage. This stage of dysbacteriosis is considered the most dangerous; it causes a lot of suffering to the child. Pathogenic microflora almost completely displaces the beneficial one and begins to dominate in the child’s intestines. The symptoms of the disease intensify, the child begins to lose weight, and he experiences symptoms of intoxication of the body caused by waste products of pathogenic bacteria entering the blood. Often at the fourth stage, shortness of breath, insomnia, asthma, etc. are added to the symptoms of dysbiosis.
Dysbacteriosis: what worries the baby?
A baby in whose intestines the quantitative and qualitative composition of the microflora is disturbed often behaves restlessly, his sleep is disturbed due to painful intestinal spasms, which are paroxysmal in nature and appear 1.5-2 hours after feeding. This is almost always accompanied by bloating due to increased gas formation and rumbling along the intestines. Due to bloating and impaired movement of food through the intestines, regurgitation and vomiting are observed. In especially severe cases, intestinal dysbiosis is accompanied by malabsorption syndrome (impaired absorption of nutrients in the small intestine), which is manifested by diarrhea (foamy stool with a sour or putrid odor) and a decrease in the rate of weight gain. And since intestinal dysbiosis is always a secondary process, developing against the background of some underlying problem in the child’s body (intestinal infections, taking antibiotics, prematurity, improper feeding), the addition of malabsorption syndrome further aggravates the severity of this disease.
Many children develop persistent constipation against the background of dysbacteriosis, since in the absence of a normal number of bifidobacteria, the substance that stimulates intestinal contractility is not produced in sufficient quantities.
According to its course, dysbacteriosis can be compensated and uncompensated.
With compensated intestinal dysbiosis there are no clinical manifestations. The child feels quite well, and a disturbance in the microbial landscape becomes an accidental discovery when a stool test (by the way, this study serves as the main laboratory criterion for dysbiosis) is taken for a completely different reason.
Uncompensated dysbacteriosis is accompanied by all the clinical signs mentioned above. In such cases there are a lot of complaints and the question of whether the child needs treatment or not is not raised. The baby’s parents strive to carry out the most effective course of treatment as soon as possible in order to save the child from suffering.
As for the first case, when there are practically no complaints, the baby is gaining weight well, sleeps well or quite satisfactorily, and there are no obvious manifestations of allergies, then parents ask the traditional question: “Why treat the child if nothing bothers him?” In older children, this is the case - if compensated intestinal dysbiosis is detected, then, as a rule, it does not require treatment. This issue is resolved in a completely different way in infants - in them, dysbiosis requires treatment in any case, because in such young children, compensation for impaired intestinal microflora is a temporary and very unstable condition due to imperfect immunity. At the slightest disturbance of this balance (and it can be caused by teething, vaccination, hypothermia, transfer to artificial feeding, a simple cold, and even stress), dysbiosis becomes uncompensated. That is why any dysbiosis in infants requires treatment, which must be strictly individual, balanced, based on laboratory data, and comprehensive.
Advertising
Treatment of dysbiosis
In the early stages of development, dysbiosis does not require special treatment: doctors recommend waiting a little until the body returns to normal. If the disease causes severe discomfort to the child or has reached the third or fourth stage of development, it may be necessary to take special medications: probiotics and prebiotics.
Probiotics are medicines that contain live bacteria that are beneficial to humans. The main task of probiotics is to normalize the intestinal microflora and displace pathogenic organisms. There are dry and liquid probiotics, which contain either one strain of bacteria or several at once. The most popular probiotics include Bifimbacterin, Lactobacterin, Hilak Forte, Acipol, etc.
Only a doctor can prescribe probiotics. He also selects the most suitable drug, based on the results of laboratory tests of the child’s stool
Simultaneously with probiotics, prebiotics are prescribed, that is, drugs that contain substances that stimulate the reproduction of beneficial microflora. Prebiotics include proteins, fats, vitamins and other components that have a positive effect on the condition of the gastrointestinal tract.
Probiotics perform the following functions:
- suppress the growth of pathogenic bacteria;
- eliminate flatulence;
- contribute to the restoration of the mucous membranes of the gastrointestinal tract damaged due to the inflammatory process;
- help maintain optimal levels of gastric acidity;
- stimulate the immune system.
In pharmacies you can buy drugs that contain both probiotics and prebiotics. Such medications have an excellent effect on the baby’s body and help quickly get rid of the unpleasant symptoms of dysbiosis.
If the child has severely impaired digestion, enzymes can be used, for example, Creon, Pancreatin, etc.
Finally, in order to strengthen the body's resistance, vitamin preparations are recommended.
Treatment
To cure dysbiosis, you will need the patience of parents, the organization of nutrition control, and the elimination of the main cause of the problems. Gastroenterologists advise an integrated approach in such cases. In the treatment of intestinal dysbiosis in a child, it is necessary to provide proper nutrition, medication, and symptomatic remedies.
Diet Requirements
Children under one year of age should receive breast milk. It is recommended to at least supplement feeding when lactation decreases. This natural method will help “populate” the baby’s intestines with the necessary flora. Breastfeeders need the safest milk formulas. Changing them frequently is prohibited.
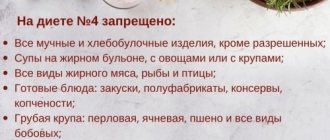
If the child is over a year old, the diet must include fermented milk products: kefir, yogurt, medium-fat cottage cheese (no more than 5%), fermented baked milk, yogurt, sour cream. Sugar is limited, so you need to get used to drinking unsweetened kefir.
Your pediatrician can help you choose the best formula
You will have to exclude baked goods, confectionery, everything fried and fatty, chocolate, sausage, sausages, sauces, seasonings, ketchup, carbonated drinks, and fast food products from your diet. These products are harmful even to a healthy child. Vegetables can be prepared in the form of stewed puree, vinaigrette without salty ingredients, or grated salad.
Temporarily avoid sour fruits. Bananas and baked apple are shown. The use of diet is sometimes sufficient to correct digestion. If after 10 days of rational nutrition there are no results, then medications are prescribed.
Features of drug therapy
The transition to drug therapy aims to:
- suppress or destroy pathogenic microflora found in the intestines - a short course of antibiotics and bacteriophages are prescribed (for dysentery, salmonellosis);
- introduce beneficial bacteria into the intestines and promote their reproduction - prebiotics, probiotics and symbiotics are used for this;
- remove accumulated waste and toxins from the intestines using drugs from the sorbent group;
- replenish the loss of vitamins, stimulate the development of immunity.
Probiotics are basic preparations containing live beneficial bacteria. For children, forms in soluble powder, syrup, and drops are more suitable. Pediatricians prescribe: Bifiform, Linex, Acipol, Bifidumbacterin, Enterol. They contain different concentrations of bifidobacteria and lactobacteria. Suitable for children in the first month of life.
Antibacterial drugs to normalize intestinal microflora
At the fourth stage of dysbiosis, the use of antibiotics that suppress the development of pathogenic microflora may be required. Unfortunately, antibiotics also kill beneficial microflora, so after the course the child must take probiotics and prebiotics.
Typically, antimicrobial drugs are taken over a course of 7-10 days. After treatment, it is necessary to re-take the stool for analysis to make sure that the imbalance between the microflora necessary for the body and pathogenic bacteria has been eliminated.
Under no circumstances should you buy antibiotics yourself: only the attending physician can choose the optimal treatment regimen for dysbiosis!
Dysbacteriosis in children is a rather serious disorder that requires immediate medical intervention. Of course, the doctor may conclude that there is no need for treatment and the condition will stabilize on its own. Carefully monitor your baby's condition: this will help you avoid serious digestive disorders, which cause a lot of anxiety for both the baby and his parents!
Diagnosis of dysbiosis in children under one year of age
Diagnosis of intestinal dysbiosis will allow you to correctly assess the quality of the intestinal microflora, the ratio of pathogenic and normal microorganisms in the digestive tract.
Diagnosis of this condition is carried out using microbiological analysis of stool. By analyzing stool, you can determine the sensitivity of bacteria to various medications. This will help you choose a treatment regimen and choose the right medications.
For this test, parents need to collect about 5-10 grams of stool. The material should not be stored for a long time at room temperature, since it will no longer be possible to determine the intestinal microflora.
To determine dysbiosis in children under one year old and assess the activity of the digestive tract, a coprogram is often prescribed. Using this method, you can assess the ability of a child’s intestines to digest food, identify violations of its absorption and breakdown.
Evening stool is also suitable for this analysis, but it must be stored in a closed glass container (in the refrigerator).
Drug treatment
Violation of the natural microflora requires proper, comprehensive treatment. The main thing is to eliminate pathogenic organisms and disturbing symptoms. Medications help get rid of constipation, diarrhea, vomiting, and improve the baby’s sleep and appetite.
- Mothers of complementary feeding children are advised to focus on breastfeeding. Babies who do not receive breast milk will need a special balanced diet.
- To treat a simple form of dysbiosis, antiseptics such as prebiotics, bacteriophages, and probiotics are prescribed.
- In the third and fourth degrees, antibiotic therapy is prescribed in the form of systemic antimicrobial drugs in combination with probiotics (Eubicor, Inulin, Effidigest, Colibacterin). Combination drugs are effective in treatment.
- Bacteriophages can be effectively used for the fourth degree of dysbacteriosis. When they enter the intestines, they begin to immediately displace pathogenic pathogens of the facultative flora.
- You cannot give antibiotics to infants on your own! This type of drug treatment is prescribed by specialists, taking into account the benefits and risks for the infant.
- For diarrhea and constipation, treatment is aimed at improving intestinal motility. A pediatric gastroenterologist individually prescribes hepatoprotectors, prokinetics, and laxatives.
Note : the treatment is long-term, the course lasts from 10-12 days. The duration is determined by the doctor, taking into account the condition of the small patient and the presence of concomitant pathologies. Often, intestinal upset is a symptom of diseases of the pancreas, gastritis, diabetes, viral infection, asthma, colitis. Such children require constant monitoring by a pediatrician.
Main symptoms in children
It is problematic to independently determine the disease due to the immaturity of the digestive system. Signs by which the disease can be recognized include: dyspepsia, anorectal syndrome, impaired intestinal absorption.
Dyspepsia
The concept of “dyspepsia” includes symptoms of a disorder of the digestive system, which appears as a result of low secretion of necessary enzymes. There are nutritional (unbalanced diet) dyspepsia.
Nutritional dyspepsia is divided into subtypes: fermentative (consumption of carbohydrate products), fatty (poor absorption of fats), putrefactive (slow breakdown of proteins).
Due to improper gastric motility, intestinal receptors are irritated, causing increased peristalsis.
Fermentative dyspepsia is expressed by rumbling sounds, bloating, increased gas formation, light foamy feces with a sour aroma. Putrefactive dyspepsia is manifested by diarrhea with dark stool, loss of appetite, general weakness and low performance. With fatty dyspepsia, stools are profuse and light in color interspersed with fat.
Diagnosis of dyspepsia is made on the basis of questioning patients, clinical signs, and laboratory tests.
Anorectal syndrome
Anorectal syndrome is expressed by fecal retention, persistent pain in the anus, small intestine; a feeling of spasms, burning, itching in the anus with an inflammatory process on the skin. Often, anorectal symptoms appear as side effects after drug treatment.
The disease is determined by digital examination, rectoscopy, radiographic examination of the coccyx and sacrum, sphincterometry. Based on the results of diagnostic procedures, proctological diseases are excluded.
Anorectal spasms are treated with massage and physiotherapy.
Intestinal malabsorption
Malabsorption syndrome (malabsorption) occurs due to improper absorption, digestion, and transport of nutrients. Symptoms of this phenomenon include: foul-smelling feces with fatty patches, chronic stool disorder, increased formation of gases, flatulence, weight loss, anemia, bleeding, pain in the musculoskeletal system.
Observing your child will help you understand at home whether there is an intestinal illness. In case of sudden weight loss, chronic diarrhea, anemia, you should consult a doctor for help. The doctor will order the necessary laboratory tests: tests for the presence of fat in the stool within 72 hours. The patient undergoes an endoscopic procedure to take a biopsy from the intestinal walls; X-ray of the small intestine, breath test using Xylose.
A folk method available at home and following a therapeutic diet will help you get rid of malabsorption. The diet is compiled strictly individually by the attending physician, taking into account the characteristics of the disease, medical history, and age category. As soon as the provoking factor disappears, the disease recedes. The process usually takes from 4 to 6 days. The recovery period lasts from one to several months.