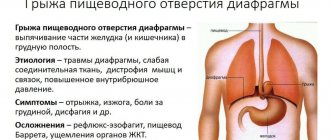
A pathological condition in which vasodilation appears in the lower part of the esophageal tube or the area of the stomach adjacent to it is called esophageal varicose veins, the symptoms of which will be discussed in detail in this article.
Another name for this disease is phlebectasia of the esophagus. The disease develops due to increased pressure in the portal vein and decreased blood flow. This condition is caused by chronic hepatitis B and liver cirrhosis. There is a change in the structure of blood vessels. Bag-like protrusions form on their walls, and the capillary shell itself becomes thinner.
The vessels have a tortuous shape, the mucous membrane is hyperemic and has ulcerations. This leads to massive bleeding that has no preliminary symptoms.
The pathology has an ICD code of 185, which is defined as varicose veins of the esophagus, 185 (9) without bleeding, 185 (0) with bleeding.
What it is
Sustained hypertension (high pressure) in the portal vein 2-4 times higher than normal leads to phlebectasia. A further increase in pressure (24 - 27 water column) leads to rupture of the vessel and the development of bleeding.
Hypertension in the portal vein leads to a decrease in blood outflow, deformation of blood vessels, their elongation and thinning of the walls. Protrusions form on the walls of blood vessels, where blood collects. With increased pressure, the load on the capillary wall increases and it can rupture.
In pathologies of the cardiac system, varicose veins are small in size and localized over the entire surface of the esophageal tube. If the expansion is caused by pathological processes occurring in the liver, then the vessels are more dilated, and they are affected in the lower region of the esophagus.
Complications in the form of bleeding depend not on the size of the varicose node or on the condition of the vascular wall, but on the pressure surge in the portal vein.
It is provoked by:
- binge eating;
- increased physical activity;
- increase in intra-abdominal pressure.
Sometimes bleeding occurs during sleep. There are factors that aggravate the condition: cardia failure, as well as decreased blood clotting. This is why varicose veins of the esophagus are dangerous.
If you have esophageal varicose veins, the ICD 10 code should be known to your doctor.
Varieties
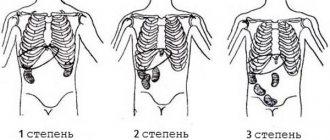
There is a classification of the disease depending on the degree of the disease. Thus, esophageal varicose veins are divided into 3 degrees:
- Grade 1 - characterized by the fact that the veins reach five millimeters in diameter, and upon examination you can notice that they are significantly elongated. They are located in the lower part of the esophagus;
- 2nd degree – characterized by an increase in the diameter of the veins to one centimeter. They are noticeably convoluted and localized in the middle part. At the second stage, the appearance of internal bleeding is not typical;
- Grade 3 – the vessels dilate by more than one centimeter. The walls of the esophagus are significantly tense, thinned and covered with red spots.
The fourth degree of the disease is known, which cannot be classified, because it leads to the formation of many vein nodules and can cause internal bleeding. In such cases, only half of the patients survive. Most survivors experience recurrence of the disease within 3 years.
Varicose veins of the esophagus: causes
The reasons for its development are pathological processes leading to hypertension in the portal vein. This:
- parenchymal liver diseases caused by cirrhosis, tumors, amyloidosis;
- stenosis of the portal vein (thrombosis, external compression, sclerosis);
- chronic failure of the cardiovascular system.
People at risk for developing esophageal varices include:
- persons over 50 years of age (usually men);
- patients with chronic pathologies of the cardiovascular system and gastrointestinal tract;
- patients with liver cirrhosis.
Most often, dilation of the esophageal veins develops with cirrhosis of the liver and chronic hepatitis. Alcohol abuse causes changes in the structure of the parenchyma. Scarring forms there, which disrupts normal blood flow and slows it down, resulting in blood stagnation and the formation of varicose veins.
Classification
According to clinicians, according to the classification of the disease, it is divided into congenital and acquired forms. In the second type of disease, early diseases play a significant role, which led to the formation of varicose veins.
Congenital pathology manifests itself due to a hereditary factor in people aged 50 years. Sometimes doctors diagnose this disease in patients in childhood or adolescence.
Doctors also developed a classification according to the degree of development of the disease. Based on these data, the patient is diagnosed and treatment is prescribed. Thus, varicose veins of the esophagus are formed in 4 stages:
- 1st degree – veins stretch by 3 mm;
- 2nd degree – expansion remains within 3 mm, tortuosity and unevenness of the structure appear;
- 3rd degree – the opening of the vein decreases and it becomes serpentine-shaped;
- Grade 4 – noticeably severe thinning of the vessel wall.
Stages of the disease
There is a congenital form, which is observed in newborns. But such a pathology occurs rarely and is accompanied by other serious disorders. The development of the disorder is caused by a hereditary factor and the course of pregnancy. The acquired form is observed in men who have crossed the 50-year mark and have bad habits.
Based on the degree of vascular damage, four types of disease are distinguished:
1st phase . This is the initial degree, in which varicose nodes do not exceed 3 mm in size and are determined only by endoscopic examination. When taking an x-ray with contrast, slow blood circulation is visible, but there is no bleeding. In this case, the esophageal opening contracts “intermittently.” Read more about the first stage of the disease here.
2nd phase .
At this stage, the lumen of the vessels is not disturbed and varicose veins are not enlarged, but the veins acquire a tortuous structure. The diagnosis is confirmed using contrast radiography, which shows unclear contours of blood vessels and rounded protrusions. There is no bleeding. 3 phase .
There is a persistent dilation of some parts of the vessels, the lumen of the vein is narrowed. Varicose nodes are clearly visible, the mucous membrane is changed (thinning). This phase is characterized by a high risk of bleeding. The X-ray image shows formations on the mucous membrane of the esophagus in the form of polyps, as well as precise perforation of the mucous membrane. The condition is assessed as serious and requires urgent hospitalization.
Phase 4 . There is a strong thinning of the mucous membrane of the blood vessels and the formation of polyps on it. Esophageal varices at this stage have the appearance of clusters and significantly block the lumen of the esophagus. As the disease progresses, it may close completely. During this period, the patient experiences hyperemia of the mucous membrane and the formation of erosive defects on it. This condition is regarded as critical because it causes frequent and massive bleeding.
How does varicose veins of the esophagus manifest?
Symptoms of esophageal varicose veins can be vague and blurred for a long time, without clear signs. The veins of the esophagus lengthen, twist, dilate and gradually lose tone. The protrusions of the walls form nodes in which blood accumulates and stagnates. The patient feels pain and burning behind the sternum, belching, difficulty swallowing, heaviness after eating. There is shortness of breath and fatigue. Spider veins appear on the skin of the chest.
For ease of diagnosis and treatment, varicose veins of the esophagus are classified into several stages:
- Grade 1 esophageal varicose veins are noted when the cross-section of the vessels increases by 2-3 mm. Small single nodes are detected. The lumen of the esophagus has areas of expansion and narrowing that are not related to the anatomical and physiological features of the structure. Stage 1 varicose veins are determined only by instrumental examination. There is no bleeding. The mucous membrane of the esophagus is normal.
- With stage 2 disease, the venous vessels acquire a tortuous structure, and nodes up to 3 mm in size appear. The walls of the vessels are thin, the impetus for bleeding from dilated veins will be increased physical activity, falling, overeating, or injury to the esophagus with a large piece of food. Symptoms of internal hemorrhage may include belching blood, coffee-colored stools, and general weakness. After bleeding, the tension in the vessel subsides for some time.
- At stage 3 of the disease, visible vascular plexuses appear on the mucous membrane. The walls of the veins stretch even more, the vessel is greatly tortuous. Veins overflowing with blood bulge into the lumen of the esophagus. The third stage imposes changes on the mucous membrane of the organ - it becomes folded, like the gastric mucosa. Externally it manifests itself as painful heartburn after every meal. The risk of bleeding from varicose veins increases many times over. Constant blood loss is accompanied by anemia, loss of strength, and drowsiness.
- For grade 4, the presence of a whole cluster of dilated nodes on the inner walls of the esophagus is specific. They can partially or completely block the esophageal canal. Erosion of the esophageal mucosa occurs. The vessels are greatly thinned and stretched. The likelihood of esophageal bleeding is very high.
A deadly complication of the disease is esophageal and gastrointestinal bleeding. Rupture of the affected vessel results in heavy blood loss. Scarlet or coffee-colored bloody vomit appears. The pressure drops sharply, the heart is pounding, sticky and cold sweat, impaired consciousness. A special case is a fountain of blood from the mouth. Loss of more than 2 liters of blood is considered fatal. After the first episode of bleeding, 25% of patients die. Repeated blood loss gives only 50% of the unfortunate people a chance to survive.
Esophageal varicose veins: symptoms
The onset of the disease does not manifest itself in any way. Therefore, patients seek medical help when the disease has already “gained momentum.” It is impossible to recognize the disease on your own, because the initial manifestations of the disease are similar to the symptoms of a digestive system disorder. So, if there is dilatation of the veins of the esophagus, the symptoms will be as follows:
- the appearance of shortness of breath ;
- the presence of heartburn (does not depend on food intake);
- pain in the area of the xiphoid process;
- swallowing disorder.
If there are varicose veins of the esophagus and stomach, its main sign is a vascular pattern on the skin of the anterior abdominal wall in the form of a “jellyfish head”. It is formed by pathologically altered veins. This symptom appears later in the course of the disease. Later, when bleeding occurs, the patient has:
- bloody vomiting;
- blood in stool;
- tachycardia;
- hypotension (sharp decrease in blood pressure);
- shock.
This is an extremely serious condition of the patient, requiring urgent hospitalization, since delay leads to death.
Diagnosis and treatment
The patient's varicose veins of the stomach and esophagus are determined by such methods as:
- Ultrasound examination of the esophagus, abdominal organs;
- general blood analysis ;
- radiography using contrast;
- esophagoscopic examination of the esophagus.
When making a diagnosis, take into account that bleeding can be caused by an ulcerative lesion of the esophagus, a disintegrating tumor, or Mallory-Weiss syndrome. This is a longitudinal tear in the lining of the upper stomach or distal esophagus caused by frequent vomiting.
When the diagnosis of varicose veins of the esophagus is confirmed, treatment is prescribed according to the degree of damage to the vessels of the esophageal tube. If the disease is detected when bleeding occurs, then treatment is aimed at stopping it:
- blood transfusion;
- vasoconstrictor drugs;
- hemostatic drugs;
- electrocoagulation of the affected vessel;
- squeezing the affected vessels with a special probe.
After this, therapeutic measures are carried out aimed at preventing a relapse (repetition) of the attack. If varicose veins of the esophagus are observed with cirrhosis of the liver, then treatment of the underlying disease is carried out. It is aimed at restoring the function of liver tissue. The patient is also advised to give up bad habits and avoid strenuous physical activity.
- Antacids are prescribed to prevent unnecessary irritation of the esophageal mucosa.
- Astringents that relieve inflammation.
- Vitamin therapy.
If esophageal varicose veins are diagnosed, medication treatment can be supplemented with surgical intervention to prevent relapses.
Bandage – small rubber discs are installed over varicose veins. Sclerotation is the introduction of a hemostatic solution into the affected vein. The procedure must be carried out at least four times a year. Devascularization - all damaged veins that cannot be restored are completely removed.
With cirrhosis of the liver, the patient cannot undergo classical surgery. In this case, endoscopic alloying of the esophageal vessels is performed. The procedure involves tying the vessel with nylon loops or elastic rings.
Portosystemic shunt, in which the portal and hepatic veins are connected. This makes it possible to normalize the pressure in the vessels.
Diet food
Once diagnosed with esophageal varicose veins, treatment includes many measures, including adherence to certain dietary rules.
A diet for varicose veins of the esophagus involves consuming foods that can increase the elasticity of blood vessels, strengthen them, and also prevent the formation of blood clots.
Recommended food products should contain vitamin B, C, and fiber:
- legumes;
- lettuce leaves;
- corn and olive oil;
- citrus;
- seafood;
- nuts;
- vegetables and fruits.
It is better to replace meat with seafood or beef liver. It is not advisable to eat salty, spicy and hot dishes, after which the patient drinks a large amount of water. This leads to tissue swelling. The recommended volume of fluid per day is 2 liters. You should also not drink whole milk, as it reduces the elasticity of blood vessels.
Cannot be consumed:
- alcohol;
- black tea and coffee;
- confectionery;
- canned and smoked foods;
- sugar.
There are nuances in preparing and eating dishes. You need to cook food by steaming or boiling, as well as baking. You need to eat food in small portions so as not to convey it, and the dishes should not be too hot or cold.
You should not eat rough and hard food, so as not to injure the esophageal mucosa. During the meal, you need to chew your food well. You need to eat 5-6 times a day, and the last meal should be taken 2-3 hours before bedtime.
Preventive actions
To prevent phlebetasia, you need to consult a doctor in a timely manner. Treat liver pathologies if there is a history of them. It is necessary to maintain proper nutrition, get rid of bad habits, and monitor your weight. There is also no need to subject the body to excessive physical stress.
This applies not only to the type of activity, but also to training in the gym with strength exercises. Physical exercise should not be excluded, but you need to perform exercises developed by a physical therapy doctor specifically for patients with varicose veins of the esophagus. A set of such exercises is aimed at improving blood circulation, reducing the risk of blood clots, and reducing cholesterol deposits.
Also, in the prevention of such a disease as varicose veins of the esophagus, the coordinated work of the gastrointestinal tract plays an important role. Therefore, such patients are recommended to use infusions of medicinal herbs that have a choleretic effect and improve digestion. To prevent reflux (reflux) of stomach contents into the esophagus, thereby irritating the mucous membrane, you need to sleep with the head of the bed raised by 10 cm.
Following these recommendations will help avoid the development of a serious disease or its relapse. And you need to remember that you need to see a doctor when the first symptoms appear, in order to prevent serious complications in the form of heavy bleeding. It is undesirable to deal with the disease venous dilatation of the esophageal veins.
Prognosis for recovery
Regarding non-traditional treatment methods, it is stupid to use them in this case. They can only improve the state of the immune system and normalize the composition of the blood in the body, but traditional medicine will not help eliminate the dilation of the veins itself.
The prognosis for full recovery is not always favorable, since esophageal varicose veins end in death in 71% of cases. If the pathology is diagnosed at stage 3, then doctors can no longer cure it; the only thing in their power is to normalize the patient’s general condition and prevent the development of complications. If there was bleeding from the esophagus, then this has already reduced the patient’s life expectancy by about 3 years, since the risk of repeated hemorrhage is quite high. Chronic endoscopic and medical treatment reduces this risk, but overall the hope for long-term survival remains extremely low. Only constant care for your body can protect you from diseases of the circulatory system and other equally dangerous pathologies.