- Vascular lesions: eyes, kidneys, stroke
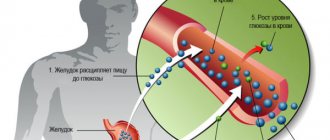
Diabetes mellitus is a systemic metabolic disorder associated with a complete or partial deficiency of the hormone insulin secreted by the pancreas. As a result of this deficiency, a steady increase in the concentration of glucose in the blood occurs, and all types of metabolism are disrupted.
The most common types of acute complications of diabetes
Ketoacidosis
It is a variant of metabolic acidosis that develops against the background of impaired carbohydrate metabolism due to insulin deficiency. This deficiency can be absolute in type I diabetes mellitus or relative in type II diabetes mellitus. The cause of the pathological condition is an increase in the concentration of glucose and ketone bodies in the blood, formed as a result of lipolysis - a disorder of fatty acid metabolism. In this case, the indicators significantly exceed the physiological norm. The risk of ketoacidosis increases with poor diet, trauma, surgery, inflammation, infections, the use of insulin antagonist drugs (including glucocorticosteroids, sex hormones, diuretics), and taking medications that reduce the sensitivity of tissues to the action of insulin (for example, atypical antipsychotics) ), depletion of insulin production during prolonged course of type II diabetes mellitus, surgery on the pancreas (pancreatectomy), pregnancy (gestational diabetes).
Symptoms of this complication of diabetes usually appear within one or several days. First, signs of elevated blood sugar levels appear due to a lack of insulin: excruciating thirst, frequent urination, weakness, dry skin and mucous membranes, unmotivated weight loss.
Later, signs of ketosis (increased production of ketone bodies) and acidosis begin to appear. These include increased irritability or lethargy, drowsiness, headaches, Kussmaul breathing (noisy and deep breathing), nausea, vomiting, and the smell of acetone from the mouth. Since ketone bodies irritate the gastrointestinal tract, dehydration of its cells occurs and potassium levels decrease due to increased urination; the described symptoms are accompanied by signs reminiscent of surgical problems with the gastrointestinal tract: pain in the abdomen, tension and soreness of the abdominal wall, decreased intestinal peristalsis.
Mechanism of development of complications
In diabetes mellitus, glucose, which should penetrate into cells (especially muscle and fat cells, which together make up almost 2/3 of all cells) and provide them with energy, remains in the blood. If it is constantly increased, without sudden “jumps”, then, being a substance that creates hyperosmolarity (because of this, fluid leaves the tissues and overflows the vessels), it leads to damage to both the walls of blood vessels and the blood supplying organs. This is how “gradual”, late consequences develop. When there is a sharp shortage of insulin, acute complications develop that require emergency medical care, without which they can be fatal.
In type 1 diabetes there is little insulin. If this deficiency is not compensated for by an analogue of one’s own hormone, administered in injections, complications develop quite quickly and shorten a person’s life.
In the case of type 2 diabetes, the body has its own insulin, but it is poorly “sensed” by the cells that are supposed to work with it. Here, treatment is carried out using tablet medications, which should “indicate” the necessary tissues to insulin, as a result of which the metabolism will be normalized for the duration of the action of these drugs. Acute complications are less likely to develop here. It often happens that a person learns that he has diabetes not by the known symptoms, when he is thirsty or has to go to the toilet at night due to the amount of water consumed, but when late complications develop.
In type 2 diabetes, human tissue is insensitive only to its own insulin. Injecting the hormone normalizes metabolism. Therefore, if a special diet and glucose-lowering drugs cannot maintain blood sugar below 7 mmol/l, remember: it is better to select the dosage of exogenous (supplied from the outside) insulin and constantly administer the drug than to shorten life expectancy and reduce its quality out of unnecessary stubbornness. Of course, such treatment should be prescribed by a competent endocrinologist, who must first make sure that the diet really does not help, and is not simply not followed.
See New type of diabetes not recognized in time.
Hypoglycemia
The complication is associated with an extreme decrease in blood sugar levels due to an overdose of medications for diabetes, increased physical activity, unhealthy diet (excessive consumption of foods with refined carbohydrates, deficiency of vitamins in the diet), drinking alcoholic beverages, dehydration, late or insufficient meals, menstruation in women, various diseases (renal or liver failure, exhaustion, sepsis).
Symptoms of hypoglycemia: increased aggressiveness, agitation, fear, anxiety, restlessness, tremor, muscle hypertonicity, arrhythmia, increased sweating, pale skin, general weakness, nausea, vomiting, increased blood pressure, disorientation, impaired coordination of movements, headaches, dizziness , visual disturbances, decreased concentration, amnesia, drowsiness, circulatory and respiratory problems.
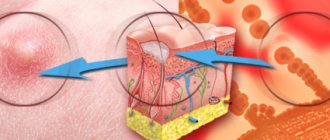
Foot care for nerve damage:
- Don't go barefoot.
- Always wear clean and dry socks. Wear them inside out (less risk of chafing from seams).
- Check your feet once or twice a day to look for redness or calluses. Use a mirror to see your soles.
- Wear shoes that fit well and are not too tight. Clean it frequently to remove sand.
- Wash your feet thoroughly and apply moisturizer to prevent skin cracks.
- Call your doctor immediately if you notice redness, calluses, blisters, ingrown toenails, or signs of infection.
- Regular monitoring of the condition of the feet at a diabetic center is necessary. Learn how to properly treat your toenails without damaging the skin.
- If you smoke, then give it up!
1
2
3
4
Hyperglycemic coma
This complication of diabetes is a special type of diabetic coma, which is characterized by an extreme degree of metabolic disorder against the background of a sharp increase in blood sugar levels (severe hyperglycemia - up to 33 mmol/l or more) without ketoacidosis. Severe dehydration of the body, hypernatremia, hyperchloremia, cellular exicosis, and azotemia develop. A feature of hyperglycemic coma is the manifestation of frequent and varied symptoms of damage to the nervous system: convulsions, speech disorders, nystagmus (involuntary rhythmic movements of the eyeballs), paresis, paralysis of certain muscle groups. Signs of this type of complications of diabetes mellitus also include unquenchable thirst (polydipsia) and increased urination (polyuria).
Other complications in diabetic patients
In addition to the main complications of diabetes described above, diabetes mellitus causes a weakened immune system. A person with diabetes is more susceptible to various infections, including tuberculosis. Diabetic arthropathy is a disease of the joints that causes pain and reduces their mobility. Diabetic encephalopathy covers a number of mental disorders, such as emotional instability and a tendency to depression. Damage to the reproductive system is manifested by a decrease or disappearance of potency in men and infertility, miscarriages, premature birth, and menstrual irregularities in women. The latter may also have vulvitis and vaginitis.
Lactic acid coma
This pathological condition is associated with the accumulation of lactic acid in the blood. It can develop against the background of renal, cardiovascular, and liver failure.
Lactic acid coma develops with severe hypoxemia, which can be associated with pathologies of the cardiovascular, respiratory systems, liver, collapse, and shock. Due to oxygen starvation, the body spends a large amount of glycogen, the level of lactic acid in the blood increases, while ketonuria and hyperketonuria are absent.
Symptoms of this complication of diabetes are: severe weakness, abdominal pain, nausea, vomiting, moderate dehydration, respiratory failure, impaired consciousness, stupor with delirium and coma, acidotic breathing, hypotension, oliguria, shock.
Most of the listed complications of diabetes develop extremely quickly, almost within a few hours. However, signs of hyperglycemic coma can begin to appear several days, and in some cases, several weeks before the onset of the crisis. It is almost impossible to determine in advance that such an acute condition may occur. Specific signs of diabetes complications in most cases go unnoticed against the background of symptoms of the underlying disease.
Any of the listed pathological conditions requires immediate hospitalization. The lack of qualified medical care within two hours after the onset of symptoms of complications of diabetes mellitus significantly worsens the prognosis for the patient’s life.
Diabetic retinopathy
Diabetic retinopathy is a leading cause of blindness. However, not all people with diabetes go blind. Diabetic retinopathy can be simple (non-proliferative) or proliferative.
Diabetic retinopathy
| Simple | Proliferative |
| Increased capillary permeability. | Vessel proliferation. |
| Occlusion and dilatation of capillaries. | Fibrosis. |
| Microaneurysms. | Hemophthalmos. |
| Arteriovenous fistulas. | Retinal disinsertion |
| Dilatation of veins. | |
| Hemorrhages (dotted and in the form of spots). | |
| Cotton-like exudates. | |
| Hard exudates |
The first sign of retinal damage is increased capillary permeability, which is judged by the appearance of fluorescein in the vitreous after intravenous injection (fluorimetry). Then occlusion of the retinal capillaries develops, followed by the formation of saccular and fusiform aneurysms.
Arteriovenous fistulas also occur. Vascular damage is accompanied by proliferation of endothelial cells and loss of pericytes, which serve as supporting elements. Hemorrhages in the inner layers of the retina are usually punctate, whereas hemorrhages in the more superficial neuroepithelial layer are shaped like flames, spots, or streaks. Preretinal hemorrhages are usually cup-shaped.
Exudates are of two types. Cotton-like exudates on angiography often turn out to be microinfarcts—nonperfused areas of the retina surrounded by dilated capillaries. A sudden increase in the number of cotton wool-like exudates is a poor prognostic sign and usually marks the onset of rapidly progressing retinopathy.
Hard exudates are more common than cotton wool and are apparently formed by proteins and lipids released from damaged capillaries. Retinal edema is also caused by increased capillary permeability; it most often develops near the posterior pole of the eyeball and is often combined with hard exudates.
If the swelling affects the macula, visual acuity decreases, sometimes irreversibly. Macular edema should be suspected when vision deterioration is not corrected by glasses, especially when there is exudation near the posterior pole of the eyeball. To identify it, a slit lamp examination or binocular stereoscopic ophthalmoscopy is necessary. Since laser coagulation can save vision, consultation with a specialist is indicated.
Proliferative retinopathy is characterized by vascular proliferation and fibrosis. The stimulus for vascular proliferation appears to be retinal hypoxia due to occlusion of arterioles or capillaries.
The most important role is played by endothelial growth factor, which stimulates angiogenesis. Among the complications of proliferative retinopathy, the most severe are hemophthalmos (vitreous hemorrhage) and retinal detachment. Each of them can lead to sudden loss of vision in one eye.
The incidence of diabetic retinopathy depends on the age at which diabetes began and how long the disease has been present. Sooner or later it occurs in approximately 85% of patients; but in some it is absent even 30 years after the onset of diabetes.
In elderly patients, diabetic retinopathy develops faster, but is less likely to be proliferative. In 10-18% of cases, simple retinopathy transforms into proliferative retinopathy after 10 years. Half of patients with proliferative retinopathy become blind within 5 years. Proliferative retinopathy occurs somewhat more often among patients receiving insulin therapy.
Treatment is laser coagulation. It reduces the incidence of hemorrhage and fibrosis. When retinal vessels grow, treatment is indicated for all patients. Laser coagulation is also used for simple retinopathy; it successfully eliminates microaneurysms, hemorrhages and macular edema. To reduce the retinal oxygen demand, panretinal laser coagulation is often used, in which several thousand cauterizations are performed over 2 weeks.
It is believed that this suppresses angiogenesis. Laser coagulation is not accompanied by severe complications. With extensive burns, some deterioration in peripheral vision is inevitable. Another surgical method for the treatment of diabetic retinopathy, vitreoecgomy with access through the pars plana of the ciliary body, is used for persistent hemophthalmos and retinal detachment. Complications are more common than with laser photocoagulation and include retinal tears and detachments, cataracts, recurrent hemophthalmos, glaucoma, infections and blindness.
Hypophysectomy is no longer used to treat diabetic retinopathy. There is hope that angiogenesis inhibitors, in particular the heparin analogue tetradecasulfate β-cyclodextrin, will help prevent proliferative retinopathy. All patients should be observed by an ophthalmologist.
Late complications of diabetes
This type of complication develops over several years. Their main danger is the gradual deterioration of the patient's condition. In some cases, even with proper treatment, it is impossible to completely protect against such complications.
Late complications of diabetes mellitus are:
Diabetic retinopathy
The essence of this complication is damage to the vessels of the retina. Retinopathy is the leading cause of vision loss in diabetic patients. The disease develops during a long course of diabetes with frequent periods of decompensation. The walls thicken over time, and the lumen of the vessels narrows. As a result, the blood supply to the retina is disrupted, which leads to deterioration and then loss of vision. The consequences of these pathological changes begin to appear ten years after the onset of diabetes. After 20 years of the disease, the probability of developing diabetic retinopathy is almost 100%.
The initial symptoms of retinopathy are periodic discomfort in the eyes and blurred vision. Many people attribute these phenomena to age, working on a computer, and do not consult a doctor. Gradually, hemorrhages begin in the retina of the eyes, dark spots or indistinct blurry fragments appear in the field of vision. This phenomenon goes away as the blood clots dissolve, and many patients believe that their condition has improved. Meanwhile, the pathological process progresses. Massive bleeding, rupture of several vessels can lead to retinal detachment, irreversible changes in it and complete loss of vision.
Diabetic angiopathy
This is a late complication of diabetes mellitus , in which all the blood vessels of the body are affected. There are two types of this pathology:
- Microangiopathy – small vessels (capillaries) are affected.
- Macroangiopathy – large vessels (veins, arteries) are affected.
As a rule, it manifests itself during a long course of diabetes (approximately from 10 to 15 years) with frequent decompensations.
The causes of angiopathy are the same as the causes of retinopathy: when passing through the vessels, sugar-saturated blood leads to thinning and deformation of the vascular walls, which in turn provokes disruption of blood flow and metabolic processes in tissues.
The result is oxygen starvation (hypoxia) of nearby tissues and damage to the internal organs of patients.
In 70% of cases, the vessels of the legs and heart are affected. They are the ones who are subjected to the greatest load, which leads to accelerated vascular damage.
Symptoms of angiopathy are determined by the size of the affected vessels and the degree of the lesion.
There are six stages of diabetic microangiopathy:
Zero: the patient has no complaints, but preventive diagnostics reveals initial changes in the vessels.
First: the skin of the lower extremities is pale, the legs are cold to the touch. Small, superficial, painless ulcers may appear. There is no inflammatory process.
Second: ulcers progress, can spread to muscle fibers, bones, and pain appears.
Third: areas of necrosis appear at the bottom and along the edges of the ulcer. Swelling and redness of the affected area are observed. Osteomyelitis, purulent diseases of the skin and underlying layers (abscess, phlegmon) may develop.
Fourth: the necrotic process extends beyond the ulcer (it can go to the beginning of the foot or toe).
Fifth: necrosis covers the entire foot. The only treatment in such cases is amputation.
During macroangiopathy, the following stages are distinguished:
First: the patient experiences increased fatigue, stiffness (especially in the morning), and numbness in the toes. Nails thicken. Patients complain of increased sweating and chilliness of the lower extremities. Intermittent claudication may occur, occurring at intervals of 500 meters to 1 km.
Second: the main symptoms of this stage of diabetic macroangiopathy are chilliness of the legs (occurs even in hot weather), numbness of the feet, increased sweating, pallor of the skin of the legs, a reduction in the time interval between manifestations of intermittent claudication (from 200 to 500 m).
Stage 2B: the same symptoms persist, but intermittent claudication occurs every 50-200 meters.
Stage 3A: the listed clinical manifestations are accompanied by pain in the lower extremities, which intensifies at night. Leg cramps occur. Patients experience tingling and burning sensations on the skin of their legs. In a horizontal position, the skin turns pale, and if you stay in a position with your legs down (standing or sitting) for a long time, your fingers become bluish. The skin is extremely dry and flaky. Intermittent claudication occurs when walking less than 50 meters.
Stage 3B: pain in the legs becomes constant, swelling of the legs is observed, single or multiple ulcers with necrotic areas may appear.
Stage 4. The fingers or the entire foot undergo necrosis, severe weakness appears, a secondary infection occurs, and body temperature rises.
Diabetic neuropathy
The essence of this complication is damage to the nervous system. As a rule, it develops 15-25 years after the onset of diabetes. In rare cases, neuropathy may appear up to 5 years after the onset of diabetes symptoms.
The causes of the complication are disruption of the nutrition of nerve fibers due to damage to the blood vessels through which nutrients and oxygen enter the nerves. Symptoms of diabetic polyneuropathy depend on the stage of the disease.
1 (subclinical) stage . It is quite difficult to recognize. Nothing bothers the patients, however, there are already initial changes in the nervous tissues: sensitivity to the effects of temperature, pain, and vibration decreases.
2 (clinical) stage . At this stage, there are several different forms of neuropathy.
Acute painful form . It is characterized by the periodic occurrence of pain of varying intensity in different parts of the body, and sensory disturbances also occur.
Chronic pain form. The patient feels tingling, burning, decreased sensitivity, numbness, pain in almost any area of the body, mainly in the legs. Symptoms become especially severe at night.
Painless form. Patients complain only of numbness and decreased sensitivity, mainly in the feet.
Amyotrophic form. In addition to pain and numbness in the lower extremities, muscle weakness and heaviness appear when walking.
Stage 3 (stage of complications). Ulcerative lesions appear on the skin (mainly of the lower extremities). As a rule, they are painless. This stage of complications is characterized by amputation of the affected areas in approximately 15% of patients.
Diabetic foot
The essence of this complication lies in the damage to the foot. In the vast majority of cases, it develops in patients with type II diabetes - usually 15-25 years after the onset of diabetes, at the stage of decompensation. Diabetic foot syndrome is a consequence of various pathological processes occurring in the body of patients with diabetes. Constant jumps in blood sugar levels lead to gradual damage and destruction of blood vessels throughout the body. Similar processes occur with nerve fibers. As a result, metabolic processes in tissues, including the skin, are disrupted.
Symptoms of diabetic foot depend on the form of the complication.
Neuropathic form with predominant symptoms of nerve damage . The pain threshold increases, the sensitivity of the foot decreases, the foot gradually becomes deformed, the skin thickens, and calluses appear.
Ischemic form with predominance of vascular damage. Symptoms include pale and cold skin on the feet and swelling. Ulcers may occur. Sensitivity does not decrease, the foot does not change shape, but the pulse in the arteries is either not audible at all or is very weak.
The mixed form occurs in most cases and includes the characteristics of the forms described above.
The symptoms of diabetic foot vary depending on the stage of the pathological process.
Zero stage . The foot becomes deformed, calluses form, the skin is cold and pale. No ulcers
Stage 1: Ulcers form on the surface of the skin. Other tissues are not affected.
Stage 2 . Ulcers spread deeper, damaging not only the skin, but also fiber, muscle tissue and tendons.
Stage 3 . Ulcers reach the bone.
Stage 4. Gangrene begins - for now in a limited area.
Stage 5. The gangrenous lesion spreads upward, moving to the lower leg and above.
Late effects of diabetes
As a rule, late complications of diabetes mellitus appear several years after they are first detected. They are dangerous because they slowly but constantly worsen the well-being of a diabetic. Even correctly prescribed treatment does not guarantee positive results for a person. Late complications include:
- Microangiopathy.
- Brain infarction.
- Hemorrhages.
- Diabetic retinopathy.
- Arterial hypertension.
- Myocardial infarction.
- Atherosclerosis.
- Loss of body weight.
- Nephrosclerosis.
- Atherosclerosis, gangrene.
- Infections.
- Neuropathy (vegetative and peripheral).
Diabetic retinopathy
This is damage to the eye vessels, which leads to circulatory problems. Due to poor blood circulation in a diabetic, atrophy and dystrophy of the optic nerve occurs, the retina detaches, which can lead to blindness. The danger of this complication is that it passes without symptoms. Patients in rare cases notice a sharp deterioration in vision and the appearance of floating spots in the eyes. It is extremely difficult to diagnose this, since it is necessary to be examined by several specialists and undergo many laboratory examination methods.
Retinal damage in diabetes is dangerous because timely diagnosis of this complication is almost impossible
Diabetic angiopathy
Angiopathy occurs due to damage to blood vessels and the nervous system. This disease is dangerous because it leads to complete blindness. Angiopathy occurs in both adults and children. Due to the high concentration of glucose in the blood, the walls of blood vessels are destroyed, which disrupts the conductivity of the capillaries. This leads to blockage of blood vessels and metabolic disorders.
Diabetes mellitus: chronic complications
With a long course of diabetes, for about 10-15 years, high blood sugar levels gradually lead to disruption of the functioning of organs and systems, destruction of the body, and the development of dangerous diseases. In patients with diabetes, the composition of the blood changes significantly, which is fraught with chronic damage to almost all internal organs.
Blood vessels
Under the influence of sugar, blood vessels are primarily affected. Their lumen narrows, and the permeability of the walls for nutrients decreases. As a result, the supply of tissues with oxygen and vital substances is disrupted. Vascular damage leads to an increased risk of cardiovascular diseases, heart attacks, and strokes.
Kidneys
In diabetes, blood with a high glucose content passes through the kidneys. It attracts a large amount of fluid, which provokes an increase in pressure inside the glomeruli. For this reason, at the initial stage of diabetes, the glomerular filtration rate, which is one of the most important indicators of the quality of kidney function, increases sharply. The glomeruli are surrounded by a glomerular basement membrane. In diabetes, it, like other adjacent tissues, thickens. This leads to the gradual displacement of capillaries inside the glomeruli. With a decrease in the number of active glomeruli, the quality of blood filtration by the kidneys decreases. Due to the presence of a sufficient glomerular reserve, blood purification continues. However, gradually the reserves are depleted, and as a result, symptoms of renal failure begin to appear.
Nervous system
Chronic damage to the nervous system, like other systems and organs, is associated with increased concentrations of glucose in the blood. Under its influence, nerve fibers undergo pathological changes. The sensitivity of the limbs decreases until it is completely lost. Many patients experience intense pain.
Skin covering
Due to damage to the blood vessels in patients with diabetes, the supply of nutrients to the skin is significantly reduced, which gradually leads to the development of trophic ulcers. Damaged areas easily become a source of infection or contamination.
Diabetes and cardiovascular diseases
Statistics show that diabetes is often accompanied by diseases of the cardiovascular system, such as atherosclerosis, coronary heart disease (CHD)
, hypertension, etc. This is especially true for type 2 diabetes mellitus, in combination with excess weight.
The risk of early development of coronary heart disease in diabetes mellitus is very high:
it is two to three times higher than in the general population. Unfortunately, women, who are usually more resistant to the development of coronary artery disease than men, lose this “protection” if they have diabetes. The most common forms of coronary heart disease are angina and myocardial infarction. The basis of IHD is atherosclerotic damage to the heart vessels, an important shaping factor of which is a violation of fat (lipid) metabolism - dyslipidemia. The most well-known and easy-to-determine manifestation of it is an increase in cholesterol levels in the blood; Less known, but also important, are triglycerides and cholesterol fractions.
Other manifestations of atherosclerosis
- damage to the blood vessels of the brain, leading to impairment of memory and mental activity; as well as the above-mentioned disruption of the blood supply to the legs.
Arterial hypertension (high blood pressure)
- also a frequent companion to diabetes. It is against the background of high blood pressure, which is not reduced, that such a formidable complication as a stroke can develop - an acute disorder of cerebral circulation, which is often fatal or leads to paralysis. Arterial hypertension has a bad effect on the condition of the blood vessels of the kidneys and fundus, and we already know how important it is to protect them with all our might.
Prevention and treatment of cardiovascular disease
Arterial hypertension and dyslipidemia are subject to mandatory monitoring and treatment.
Every diabetic patient needs to check their lipid metabolism and blood pressure levels at least once a year. Such frequency of monitoring is sufficient only at normal levels of these indicators, i.e. If:
- The total cholesterol level is below 5.2 mmol/l (and according to the latest data below 4.8 mmol/l!);
- The level of upper (systolic) blood pressure is below 140 mm Hg. Art.;
- The lower (diastolic) blood pressure level is below 85 mm Hg. Art.
If the levels of these parameters exceed the norm, more frequent monitoring and, of course, treatment are required.
Typically, medications are prescribed to treat both hypertension and dyslipidemia. However, diet is also a powerful tool for influencing these disorders. It can be used as the only method of treatment if deviations from the norm are not very pronounced, and is an indispensable background for the use of medications. It is important to reiterate that weight loss has a significant positive effect on blood pressure and cholesterol levels. If your blood pressure cannot be controlled without the use of medications and your doctor prescribes medication, do not be alarmed. There are now a lot of modern drugs for the treatment of hypertension, they have minimal adverse effects and, as a rule, can be taken for a long time (years).
Each patient can always choose effective treatment, that is, achieve normalization of blood pressure. The process of individual selection of a drug or, as is often and quite reasonably undertaken, a combination of several drugs, can take some time. This process necessarily requires monitoring: repeated measurement of blood pressure by both the doctor and the patient (home self-monitoring), sometimes some laboratory tests, an electrocardiogram (ECG)
etc.
In the process of treating hypertension, the participation and understanding of the patient himself is important. Sometimes patients make a big mistake by interrupting medications when their blood pressure has returned to normal, believing that the “course of treatment” is over, or taking medications occasionally when they feel unwell.
By the way, the idea that high blood pressure must cause a headache, or that something else must bother the patient, is incorrect. Clinical observations show that most patients do not experience any discomfort with high blood pressure. That is, the body can also get used to it, as well as to an increased level of blood sugar, and a deceptive feeling of well-being arises.
It is necessary to understand that it is necessary to take medications for the treatment of arterial hypertension constantly, i.e. not only when the blood pressure is high, but also when the blood pressure drops to normal so that it does not increase!
Since self-monitoring of blood pressure at home is very useful, it is advisable for all patients with arterial hypertension to have a blood pressure measuring device at home and be able to use it.
Best natural remedy for diabetics
Dragee NRM from APL is a unique product for quickly lowering blood sugar levels based on healing extracts of medicinal plants, which have long been used in folk medicine in the treatment of diabetes. Thanks to their complex effect on the body, it is possible to reduce blood sugar levels. Plant extracts also help speed up metabolic processes, strengthen blood vessels, significantly improve the health of the body, strengthen the immune defense, thereby preventing the development of dangerous complications of diabetes . The product inhibits the progression of the disease and greatly reduces the risk of severe consequences.
Cells that do not depend on insulin (for example, retinal cells, kidney cells, or nerve cells):
It may seem counterintuitive that some cells can take up glucose without insulin, but in a situation where a healthy body becomes glucose deficient (for example, during fasting), insulin production stops. This will save the remaining glucose for your body's most vital organs. However, when a person has diabetes, this phenomenon causes these cells to absorb huge amounts of glucose whenever your blood glucose is high. Glucose binds inside cells, forming so-called AGEs (end-products of glycation), which can potentially damage cells.
Long-term high blood glucose levels cause glucose to bind to cells in the walls of blood vessels, causing the vessels to become more brittle. It is those cells that do not need insulin to transport glucose, i.e. The cells of the retina, kidneys, nervous system and blood vessels are mainly affected by glucose toxicity. Since glucose can freely pass into these cells, when blood glucose is high, they are always exposed to high concentrations of glucose. Because intestinal lining cells are not dependent on insulin, they will transport glucose from the intestines (for example, after a meal) into the bloodstream even when blood glucose is high.
If a person has diabetes, glucose binds to a protein in the membrane of red blood cells. This reduces the elasticity of red blood cells. It becomes difficult for such tough cells to pass through the thinnest vessels (capillaries), which they must do to supply oxygen to all tissues of the body. Therefore, from the point of view of red blood cells, it is important that blood glucose is under control. Normal blood glucose levels within 24 hours restore the normal structure of the blood cell wall, resolving this problem.
The risk of eye damage has decreased significantly with modern treatments for diabetes and eye diseases. Today, half of people with 15 to 20 years of diabetes may have varying degrees of retinal damage, half of which will require laser treatment. Of 1,000 people with diabetes, one will develop severe vision impairment (visual acuity of 0.1 or less) each year ), but blindness due to diabetes is very rare today in countries where modern treatments are available.
Small bulges called microaneurysms can form in fragile capillaries. They are considered “background” disorders that do not affect vision. It is important to recognize that this type of early change may be reversed as blood glucose control improves. On the other hand, if you continue to have high blood glucose and high HbAlc, the process of changes in the fundus will continue, retinal damage will worsen and new vessels will begin to form. These new vessels are very fragile and can rupture easily, causing hemorrhage and vision damage. Usually the hemorrhages resolve and vision is restored. Large or repeated hemorrhages that remain untreated can lead to permanent vision damage and, in worst cases, blindness. Impaired color or night vision is a result of damage to the nervous system caused by diabetes. Smoking also increases the risk of vision damage.
Characteristics of complications
The occurrence of complications is due to both the lack of treatment and the duration of the disease itself. Unfortunately, the fact that the body has not produced insulin on its own for 10-15 years cannot but have an impact on the condition of individual organs.
Thus, often with diabetes, the risk of high blood pressure increases and cholesterol levels increase. In men, due to impaired vascular circulation, impotence may develop. And for women, this disease causes difficulties in planning pregnancy. If it does occur, then monitoring the condition of both the woman and the fetus is especially difficult.
In general, all complications are divided into the following types: acute, late and chronic.
Diabetic neuropathy
If a patient with type 1 or type 2 diabetes is poorly treated and has high blood sugar, this damages the nerves and disrupts the conduction of nerve impulses. This complication is called diabetic neuropathy. Nerves carry signals from throughout the body to the brain and spinal cord, as well as control signals from there back. To reach a center, for example, from a toe, a nerve impulse must travel a long way. Along this entire path, the nerves receive nutrition and oxygen from the smallest blood vessels called capillaries. High blood sugar in diabetes can damage the capillaries and prevent blood flow through them. As a result of this, part of the nerve will die, the chain will be disrupted and the signal will not be able to travel in both directions.
Diabetic neuropathy does not occur immediately because the number of nerves in the body is excessive. This is a kind of insurance that is inherent in us by nature. However, when a certain percentage of nerves are damaged, symptoms of neuropathy appear. The longer the nerve, the more likely it is that problems will arise due to high blood sugar. It is therefore not surprising that diabetic neuropathy most often causes problems with sensation in the feet, fingers, and impotence in men.
Loss of nerve sensation in the legs is the most dangerous thing. If a diabetic ceases to feel heat and cold, pressure and pain on the skin of his feet, then the risk of a foot injury increases hundreds of times, and the patient does not pay attention to it in time. This is why people with diabetes often have to have their lower limbs amputated. To avoid this, learn and follow diabetic foot care guidelines. In some patients, diabetic neuropathy does not cause loss of nerve sensitivity, but rather phantom pain, tingling and burning in the legs. Read “Legs hurt with diabetes - what to do.” In a sense, this is even good, because it encourages the diabetic to undergo intensive treatment.
Less common symptoms of diabetic neuropathy are dizziness, fainting, difficulty swallowing and digestion (diabetic gastroparesis), speech problems, incomplete emptying of the bladder, and others. Read the article “Diabetic neuropathy” for more information. The good news is that this complication of diabetes is completely reversible. Follow a type 1 diabetes treatment program or a type 2 diabetes treatment program, and in a few months or years, nerve conduction will be completely restored.
Classification of complications in DM-1
Conventionally, all complications that arise with type 1 diabetes are classified into:
- Acute (for example, they develop against the background of a glycemic coma, when the patient’s condition deteriorates very quickly);
- Chronic (diseases of the cardiovascular system due to the accumulation of cholesterol in the vessels);
- Late (develops in patients mainly after 50 years, it is almost impossible to prevent this).
Acute
These include:
- ketoacidosis;
- hypoglycemia;
- lactic acid coma (excess lactic acid in the blood);
- hyperglycemia.
Ketoacidosis is the accumulation of excess indigestible metabolic products.
First of all, it negatively affects the functioning of the liver, kidneys, and cardiovascular system. It also leads to large amounts of “bad” cholesterol entering the blood.
Treatment means normalizing the balance of nutrients in the body and adjusting the diet.
Hypoglycemia is an excessive decrease in blood sugar levels, which can cause coma. This is a kind of protective reaction of the body to low glucose levels, which will not be enough for normal muscle function (including the heart).
This complication occurs either due to prolonged exclusion of foods containing carbohydrates from the diet, or due to too large a dose of insulin administered through injection (in type 1 diabetes, it is not produced by the body or is so small that it is not enough for the synthesis of glucose ).
Treatment is a glucose injection. You can get by with eating a product with a high GI (glycemic index). That is why doctors recommend that patients with type 1 diabetes always have several sweets with them.
Hyperglycemia is a complication that occurs when there is too much glucose in the blood.
Occurs due to eating a large number of foods or dishes with a high glycemic index. Coma or cardiac arrest may also occur.
If your glucose level rises to 14 mmol/l or higher, you need to give an insulin injection. In the future, reconsider your diet.
Lactic acid coma in most cases develops only after 40–45 years and later. This is preceded by lactic acidosis (lactic acidosis).
The most dangerous thing in this case is a disruption in the process of tissue oxygenation, when cells begin to oxidize at a very fast pace. Moreover, this condition primarily affects smooth muscles.
The optimal treatment option is constant physical activity (moderate, according to the calendar drawn up by the doctor).
Chronic
Chronic complications of type 1 diabetes include:
retinopathy;
- angiopathy;
- polyneuropathy;
- so-called “diabetic foot”;
- heart failure;
- renal failure;
- pancreatic atrophy;
- vascular lesions.
Such complications develop over years, but their first signs can be noticeable even at the age of 20 (according to statistics, type 1 diabetes is most often diagnosed in teenage children).
Retinopathy and angiopathy are visual impairments. Doctors say that it occurs in almost 90% of patients with diabetes mellitus (both type 1 and type 2).
Develops against the background of impaired blood microcirculation in the eyeball. In essence, the sensitivity of the optic nerve is damaged, causing visual acuity to gradually decrease. You should consult an ophthalmologist about retinopathy.
IMPORTANT! Diabetic retinopathy is virtually untreatable. But vision correction is possible, although it gives only a temporary effect.
Polyneuropathy is a disease also associated with the functioning of the nervous system. It develops due to a disruption in the conduction of nerve endings, due to which the patient’s arm or leg muscles become less sensitive to brain signals.
The exact cause of this phenomenon has not yet been established. But physical therapy gives a good result in eliminating it. You should consult a neurologist about polyneuropathy.
“Diabetic foot” is associated with changes in blood composition and disruption of its clotting process. In this case, patients develop trophic non-healing ulcers, which can even turn into the form of gangrene. You should seek help from an endocrinologist and surgeon (or traumatologist).
REFERENCE! This disease can affect not only the lower extremities, but it appears most often on the feet.
Kidney failure is a consequence of persistent potassium deficiency and overactive kidneys. This is a normal reaction of the body to increased sodium levels.
Substances with this element in most cases are waste products of water-salt metabolism. Monitoring salt balance and taking specialized diuretics will help improve the patient’s condition and prevent renal failure. You can contact a nephrologist for help.
But complications of the cardiovascular system are a consequence of excess cholesterol. In principle, all patients with diabetes have a blood chemical composition that is far from normal. It is impossible to prevent these complications, but they can be minimized by consistently following a balanced or low-carbohydrate diet. You should contact a cardiologist for help.
Psychological complications
Psychologically, type 1 diabetes is the most difficult for children to cope with. It is simply difficult for them to understand that their life should be fundamentally different from the one their peers can afford. This is why doctors recommend that children, especially those under 14-16 years old, constantly consult a psychologist on this matter.
If you allow prolonged depression, this can lead to complete disregard of medical recommendations, which will definitely aggravate the complications of diabetes.
And older patients often develop dementia. This is a consequence of the constant depletion of neurons, which disrupts the normal functionality of the brain.
Diet for type 1 diabetes
Proper nutrition for type 1 insulin dependence is one of the ways to maintain the patient’s body.
The following principles must be adhered to:
- no more than 200g of bakery products per day,
- Dairy products are allowed only those whose fat content does not exceed 1%,
- the presence of first courses in lean and vegetable broths is important,
- limit your intake of cereals,
- lean meat and fish - only stewed and boiled,
- boiled eggs no more than once a week,
- vegetables are allowed in any form,
- Sweets and refined sugar are prohibited.
It is not recommended to season dishes with seasonings. It is also necessary to limit salt intake.
Why is high sugar bad?
Patients with type 1 diabetes are forced to calculate their carbohydrate intake daily, measure their sugar levels, and take insulin. However, it is difficult to replace the fine regulation of the body with your own calculations. There is a high probability of an insufficient dose of insulin if there is an excess of carbohydrates in food. Thus, in diabetes, sugar accumulates in a person's blood.
High sugar levels cause thirst. A person feels thirsty all the time, the urge to urinate becomes more frequent, and weakness appears. These are only external manifestations of the disease. Internal complications are much larger and more dangerous. They are formed with constant elevated sugar levels. Even if the amount of glucose is slightly higher than normal (more than 5.5 mmol/l on an empty stomach), slow destruction of blood vessels and other organs occurs.
Prevention
To avoid serious complications of diabetes, follow preventive measures:
- watch your diet, control the amount of carbohydrates consumed;
- lead a physically active lifestyle;
- drink enough water to prevent dehydration;
- follow all doctor’s recommendations, take prescribed medications;
- listen to your body and if you feel worse, contact a medical facility, do not self-medicate.
Complications of diabetes can develop rapidly or gradually, affecting a specific organ or the body as a whole. Regardless of the type, they are equally dangerous to the health and life of a diabetic.
Rate this article 5 5 (1 ratings)
Diabetic nephropathy
Diabetic nephropathy is a complication of diabetes on the kidneys. As you know, the kidneys filter waste from the blood and then excrete it in urine. Each kidney contains about a million special cells that act as blood filters. Blood flows through them under pressure. The filtering elements of the kidneys are called glomeruli. In diabetics, the glomeruli of the kidneys become damaged due to increased levels of glucose in the blood that flows through them. The electrical balance in the kidney filters is disrupted, causing proteins to enter the urine from the blood that normally should not get there.
The smallest diameter protein molecules leak out first. The more diabetes damages the kidneys, the larger the diameter of the protein molecules that can be found in the urine. At the next stage, not only blood sugar increases, but also blood pressure, because the kidneys cannot cope with removing enough fluid from the body. If you do not take pills that lower your blood pressure, hypertension accelerates the destruction of your kidneys. A vicious circle arises: the more severe the hypertension, the faster the kidneys are destroyed, and the more damaged the kidneys, the higher the blood pressure rises, and it becomes resistant to the effects of drugs.
As diabetic nephropathy progresses, more and more of the protein the body needs is excreted in the urine. There is a deficiency of protein in the body, and patients experience swelling. Eventually, the kidneys completely stop functioning. This is called kidney failure. In such a situation, in order for the patient to survive, he needs to undergo regular dialysis procedures or undergo a kidney transplant operation.
Every year, several tens of thousands of people around the world seek help in specialized institutions because their kidneys have failed due to diabetic nephropathy. The vast majority of “clients” of kidney transplant surgeons and dialysis centers are diabetics. Treating kidney failure is expensive, painful and not accessible to everyone. Complications of diabetes on the kidneys greatly reduce the patient’s life expectancy and worsen its quality. Dialysis treatments are so unpleasant that 20% of people who undergo them eventually give up voluntarily, thereby committing suicide.
Heredity plays an important role in the development of diabetes complications on the kidneys. If parents suffered from diabetic nephropathy, then their offspring have an increased risk. However, if you take care of your health in time, it is possible to avoid kidney failure in type 1 and type 2 diabetes, even if you have inherited bad genes. To do this you need:
- Strictly control your blood sugar by following a type 1 diabetes treatment program or a type 2 diabetes treatment program;
- take blood and urine tests every 3 months to check kidney function;
- have a good blood pressure monitor at home and measure your blood pressure regularly, preferably once a week.
If hypertension has developed and it cannot be brought under control without “chemical” tablets, then you need to consult a doctor so that he can prescribe a medicine - an ACE inhibitor or an angiotensin-II receptor blocker. Read more about treatment of hypertension in diabetes. Drugs from these classes not only lower blood pressure, but also have a proven protective effect on the kidneys. They allow you to delay the end stage of renal failure for several years.
Lifestyle changes for people with type 1 and type 2 diabetes are much more effective than medications because they address the causes of kidney damage rather than just “dulling” the symptoms. If you follow a disciplined type 1 diabetes treatment program or a type 2 diabetes treatment program and maintain consistently normal blood sugar, then diabetic nephropathy will not threaten you, like other complications. The activities we recommend normalize blood sugar and at the same time blood pressure.
Diagnostics
There are three standard blood tests that are commonly used to diagnose type 1 and type 2 diabetes. A person may be diagnosed with type 1 diabetes if they meet one of the following criteria:
- Your fasting blood glucose level is greater than 126 milligrams per deciliter (mg/dL) in two separate tests.
- Random glucose test greater than 200 milligrams per deciliter (mg/dL) with symptoms of diabetes.
- Hemoglobin a1C test exceeds 6.5 percent in two separate tests.
When diagnosing T1DM, two other factors are taken into account: the presence of specific antibodies, such as antibody to glutamic acid decarboxylase 65 (Anti-GAD65) and/or others; and low levels of C-peptide, a substance produced by the pancreas along with insulin that can indicate how much insulin the body is making.