The pancreas has an alveolar-acinous structure, consists of many lobules, which are located at a short distance from each other, separated by layers of connective tissue. Each lobule is a cluster of secretory epithelial cells of different shapes; pancreatic juice is formed in them.
Among the parenchyma cells there are specific cells that are grouped into clusters. They are called the islets of Langerhans. The size varies from 50 to 40 microns in diameter. The total mass is no more than 3% of the entire pancreas of an adult.
The pancreatic islets are richly supplied with tiny blood vessels and capillaries; they are not equipped with excretory canals, but have internal secretion, as a result of which they produce hormones directly into the blood. They also regulate carbohydrate processes in the human body.
Let's consider the physiology of the pancreas, what is the intrasecretory and exocrine functionality of the internal organ.
Exocrine activity
The exocrine and intrasecretory functions of the pancreas are responsible for many processes in the human body. Exocrine activity is observed during the digestion of food. As already noted, the gland can produce up to 2000 ml of pancreatic juice per day.
It is this secret that facilitates the digestion of food, since it contains digestive enzymes that break down organic components that enter the body along with food.
The breakdown of carbohydrate, protein and fatty substances to the smallest molecules is revealed, which are also broken down by enzymes to an acceptable state, and are subsequently absorbed in the intestines.
Pancreatic juice enters the duodenum - characterized by the same osmotic pressure as blood plasma. Most of it is water and electrolyte, the smaller part contains enzymes. Electrolyte concentrations always fluctuate.
The pancreas produces up to 20 g of fermented proteins per day. This means that the organ occupies a dominant position in the body in terms of its ability to produce enzyme substances. The release of enzymes is due to stimulation of the organ. The process of removing enzyme components from cells does not depend on enzyme production. Basically, secretogens directly control the release of protein from the atic cell.
Enzymes responsible for the hydrolysis of proteins found in pancreatic juice are determined in an inactive form. This appears to be a kind of protection of the pancreas from self-digestion. Enzymes are activated exclusively in the duodenum. The activator is enterokinase, synthesized by the intestinal mucosa.
This is what causes the cascade phenomenon of enzymes.
Symptoms and diagnosis of exocrine insufficiency
The deficiency condition is quite difficult to diagnose. This is due to the fact that all the symptoms of this pathological condition are similar to the symptoms of other diseases, among which there are such ailments as irritable bowel syndrome, peptic ulcers, cholelithiasis, inflammatory processes in the intestines and many others.
Intrasecretory function
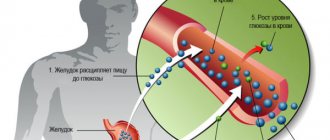
The intrasecretory part of the pancreas is responsible for the normal concentration of sugar in the human body. Glucose levels are regulated by certain hormones. Their functionality is described by the endocrine mechanism of the processes occurring. In other words, a cluster of cells (pancreatic islets) secrete the hormone glucagon and insulin.
Insulin is aimed at reducing the concentration of sugar, glucagon, on the contrary, increases the content. If there is a deficiency of insulin, then a chronic disease occurs – diabetes mellitus. There is little of it, or it is not synthesized at all.
This pathology is considered one of the most complex diseases of the endocrine pancreas. During the course of diabetes, the functionality of the internal organ is significantly impaired, which leads to the development of complications. In the absence of glycemic correction, there is a threat not only to the health, but also to the life of the patient.
Diabetes mellitus is of the following types:
- The first type is characterized by insulin deficiency, while glucagon is within normal limits or slightly above acceptable limits.
- The second type of disease occurs against the background of a normal amount of insulin, but insulin resistance syndrome occurs.
The intrasecretory function of the pancreas is disrupted due to various reasons - age-related changes in the body, unhealthy diet, physical inactivity, pathologies of the digestive tract, gastrointestinal tract, etc.
The role of the pancreas in the development of diabetes mellitus
Diabetes mellitus is a group of diseases characterized by an increase in glucose (sugar) in the blood due to absolute and/or relative deficiency of insulin.
By the way, insulin was first used on January 1, 1922 to treat a 14-year-old boy, Leonardo Thompson, suffering from diabetes; unfortunately, there was no result then.
The classification distinguishes four types of diabetes, let's talk about the main ones - the first and second.
Type 1 diabetes mellitus is a disease that occurs as a result of an absolute deficiency of insulin, i.e. as a result of some reason, the B cells in the pancreas or all of the islets of Largehans are destroyed and, accordingly, there is no insulin. This disease is typical for children and adults under 30 years of age.
There are many reasons for the destruction of pancreatic islets, the main one is destruction due to autoimmune processes, i.e. As a result of an immune failure, the body releases active cells that attack the islets and, over time, completely destroy them. Accordingly, there is only one treatment here - the administration of insulin by injection, since the body no longer has its own.
Type 2 diabetes mellitus is a disease of people after 40 years of age, a different mechanism works here, the pancreas produces enough insulin, often even more than needed! But due to various reasons, cells “do not see” insulin and it cannot perform its function. The main reason is overweight or obesity; it is the excess of fatty acids (fats) that leads to “blind” cells. Over time, the resources of the pancreas are depleted and insulin becomes less and less, and if other diseases, such as acute or chronic pancreatitis, are added, then this process goes much faster. Treatment of diabetes mellitus can be different, depending on the condition of the individual patient. The main thing is not to delay going to the doctor, since diabetes mellitus that persists for a long time without treatment can lead to very serious consequences, such as heart attack and stroke.
Diabetes mellitus type 1 and 2 - basic principles
In conclusion, I would like to note the importance of prevention, early diagnosis and treatment of diseases of the pancreas, since without its coordinated work both as a digestive and as an endocrine “factory”, it is impossible to be completely healthy, and, therefore, a completely happy person.
Where is the pancreas located and its structure
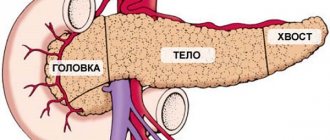
The name of the gland directly indicates its location in the abdominal cavity. The gland is located behind the stomach in the abdominal cavity, although it may move slightly with different body positions. For example, when a person stands, the stomach and gland are approximately at the same level, but in a lying position the stomach hangs over it.
If we consider the position of the organ according to symmetry, then the body of the glandular tissue is located in the center, moving slightly to the left side of the hypochondrium.
The entire gland is anatomically divided into three parts: head, body, tail. It is closely surrounded by the duodenum - this is due to its functional characteristics. The duodenum wraps around the head of the pancreas like a crescent. The glandular tissue is connected to the duodenum by the duct of Wirsung, through which enzymes are supplied to the digestive tract.
The tissue of the gland is a bit like an inverted pyramid, where the head is the thickest, then gradually decreases and goes into the body, and the top of the pyramid is the tail. It is the tail that is responsible for the production of insulin. If pathologies affect this area, the patient may develop a terrible disease called diabetes mellitus.
All parts of the organ are held together by connective tissue called the pancreas capsule.
Types of functions
The work of the organ to produce various enzymes and hormones is divided into 2 types:
- Exocrine (exocrine) activity.
- Intrasecretory (endocrine or endocrine).
Thus, the work of the pancreas is characterized by mixed functions. The pancreatic juice it produces contains various enzymes in concentrated form. Thanks to these secretions, it breaks down food. In addition, the exocrine function of the organ ensures the timely entry of pancreatic enzymes into the lumen of the duodenum, which neutralize the acidity of gastric juice. In this case, a mechanism is activated that protects the pancreas itself from damage by enzymes.
It performs an exocrine function during the digestion of food. The production of pancreatic secretion is activated by incoming food along with gastric juice. The exocrine function of the pancreas is to ensure that this secretion is produced in the required quantities.
The intrasecretory activity of the organ consists of the production of the most important hormones - insulin and glucagon, which regulate the concentration of glucose, which are so necessary for the optimal functioning of the body. Secretions are produced by the islets of Langerhans - endocrine cells, most of which are concentrated in the tail of the organ. The endocrine function of the pancreas is also to regulate the amount of hormones produced. If necessary, it helps reduce the volume of insulin and somatostatin, so the levels of these secretions do not go beyond normal limits.
Excretory ducts and lymphatic vessels
The pancreas has many lymphatic vessels and excretory ducts. Its anatomy suggests familiarity with them. The main excretory ducts, of which there are usually two in humans, run from the tail to the head of the pancreas, passing along its entire axis. The main ducts along their path receive many branches that carry secretions from the lobules. They stand out clearly in white against the background of the pancreatic parenchyma, which has a gray-pink color. At the confluence of the main excretory duct into the duodenum, its diameter reaches 2-3 mm. The tail and body are supplied by a number of branches of the splenic artery.
The anatomy of the pancreas is marked by the presence of a dense network of lymphatic vessels, which is closely connected with the network of the duodenum, gallbladder and bile ducts. Lymph from it flows to many regional lymph nodes, which are located in the stomach, hilum of the liver, mesentery, spleen and left adrenal gland.
We hope you understand the topographic anatomy of the pancreas.
Types of cells
Different groups of cells produce their own type of hormone, regulating digestion, lipid and carbohydrate metabolism.
- Alpha cells . This group of OBs is located along the edge of the islets; their volume makes up 15-20% of the total size. They synthesize glucagon, a hormone that regulates the amount of glucose in the blood.
- Beta cells . They are grouped in the center of the islets and make up most of their volume, 60-80%. They synthesize insulin, about 2 mg per day.
- Delta cells . They are responsible for the production of somatostatin, they range from 3 to 10%.
- Epsilon cells . The amount of the total mass is not more than 1%. Their product is ghrelin.
- PP cells . The hormone pancreatic polypeptide is produced by this part of the OB. They make up up to 5% of the islands.
Over the course of life, the proportion of the endocrine component of the pancreas decreases - from 6% in the first months of life to 1-2% by the age of 50.
What are the signs of pancreatitis in men?
Among the adult population, problems with the pancreas often arise due to systematic alcohol consumption, but the symptoms of acute pancreatitis are the same in men and women. In childhood, organ dysfunction is less common. With a mild degree of the disease, the symptoms are weakly expressed, and the acute form is painful and difficult. There is a high probability of complications, such as hemorrhagic pancreatitis or pancreatosis (total damage to the pancreas due to self-destruction).
Symptoms of pancreatic inflammation
The main clinical sign of the onset of the disease is severe abdominal pain. It must be borne in mind that pain can radiate to the heart area, which resembles a myocardial infarction. The sick person:
- continuous vomiting occurs;
- blood pressure drops;
- general weakness appears;
- the skin turns pale.
General symptoms of pancreatic disease are similar to other abdominal diseases:
- inflammation of the gallbladder;
- hepatic colic;
- acute intestinal obstruction;
- food poisoning.
What are the pains with pancreatitis?
Prolonged cutting pain in the upper abdomen is the first symptom of pancreatitis in men and women. It becomes so intense, bursting, that a person experiences a painful shock. When the entire organ is affected, the pain is girdling in nature. A sitting position with your legs pulled up to your chest can bring some relief, but lying on your back only intensifies the pain. Attacks can last up to several days, appear suddenly or after eating or drinking.
Temperature
When the disease worsens, inflammatory processes cause a slight increase in body temperature. Thermometer readings above 38°C and chills indicate the onset of a purulent complication, peritonitis. If the temperature during pancreatitis is reduced to 35.5°C, this is a symptom of collapse (painful shock) or excessive fluid loss. The body can react with heat to unbearable pain, but in the chronic course of the disease the temperature does not decrease for a long time, which indicates the hidden progression of the disease.
Chair
Useful article? Share the link on VKontakte
Problems with intestinal function and diarrhea always accompany the disease. At the beginning of the attack, constipation and bloating are possible. Then the stool becomes mushy, foamy, heterogeneous, and acquires a gray tint. Upon examination, you can notice particles of undigested food and a large amount of unprocessed fats due to enzyme deficiency. Loose stools with pancreatitis are a common occurrence, although they may return to normal during the remission stage.
Where does it hurt
The localization of pain in pancreatitis is determined by the affected area:
- the focus of inflammation is on the head of the pancreas - pain will occur in the epigastric region, closer to the right side;
- if the process has formed in the middle part of the gland, the pain will be recognized at the top, in the middle, or radiate to the left side of the abdomen;
- if the tail of the pancreas is affected, then the pain shifts deep to the left hypochondrium;
- when the entire surface of the organ is affected, painful spasms are centered in the upper abdomen, become encircling in nature and can spread to the heart area.
6.7. Drugs that affect the excretory function of the pancreas.
In diseases that are accompanied by insufficiency of the excretory function of the pancreas, digestion and metabolism are disrupted. Since pancreatic enzymes take part in the breakdown of proteins, fats and carbohydrates, there is a need for drugs that contain pancreatic juice enzymes.
Classification. This group includes drugs of various origins that stimulate or replace the excretory function of the pancreas or inhibit it, suppress the activity of proteolytic enzymes. Accordingly, these funds can be divided into the following groups.
I. Medicines that stimulate or replace excretory activity under
1) animal origin (organic preparations) (secretin, cholecystokinin, pancreatin, panzinorm forte, festal, creon, etc.);
2) microbial origin (solizim);
3) which are obtained from mushrooms (oraza);
4) of plant origin (herbal preparations): medicinal mixtures from dill seeds, peppermint leaves, hawthorn fruits, immortelle flowers, chamomile, medicinal teas from mint, St. John's wort, tricolor violet, linden blossom, chamomile.
II. Medicines that inhibit the excretory activity of the pancreas (proteolytic enzyme inhibitors):
1) pancreatic preparations (Gordox);
2) which are obtained from lung tissue (contrical, ingitril);
3) synthetic origin (aminocaproic acid);
4) of plant origin (herbal preparations): medicinal mixtures from anise fruits, celandine herbs, columns with corn silks, dandelion roots, St. John's wort herbs, etc.
In case of insufficiency of pancreatic function, pancreatin (powder from dried cattle pancreas) is prescribed for replacement therapy.
Amylase in pancreatin, like pancreatic juice, is in an active state. It ensures the breakdown of starch and glycogen into disaccharides. Trypsin in pancreatin is presented in the form of trypsinogen, that is, in an inactive form. Under the influence of enterokinase in intestinal juice, it is converted into active trypsin, which breaks down proteins and polypeptides into amino acids. The action of this enzyme is complemented by the enzyme chymotrypsin, which is also part of the pancreatic juice. Trypsin destroys peptide bonds formed by the carboxyl groups of arginine and lysine, and chemo-trypsin destroys the bonds of cyclic amino acids.
The mechanism of the organ's operation
Regulation of the exocrine function of the organ is carried out by neurohumoral reactions, that is, under the influence of the nervous system and biologically active substances of blood, lymph, and tissue fluids. The hormones gastrin, secretin, and cholecystokinin stimulate the exocrine activity of the gland.
It has been scientifically proven: not only the taste, smell, type of food, but even the verbal mention of it instantly excites the pancreas through the reflexes of the parasympathetic nervous system. This also leads to stretching of the stomach by the food consumed and the production of hydrochloric acid. And according to command signals from the sympathetic nervous system, the hormones glucagon and somatostatin are produced, which reduce the activity of the organ.
The flexibility of the functions of the pancreas is amazing: it can rearrange its work every day depending on a person’s different food preferences. If carbohydrates predominate in the menu, amylase is mainly synthesized. If proteins dominate, trypsin is produced, and when eating fatty foods, lipase is secreted predominantly.
Thanks to the endocrine function, the hormones insulin and glucagon produced by the organ are released directly into the bloodstream and distributed throughout the body. Moreover, different cells specialize in the synthesis of different hormones. Beta cells produce insulin, and alpha cells produce glucagon. Foods rich in carbohydrates and proteins stimulate insulin synthesis. The compensatory function of the pancreas is amazing: even if 70-80% of it is removed, insulin deficiency still does not occur - the cause of diabetes mellitus.
Acute pancreatitis
He appears suddenly. Its main symptoms are pain, often vomiting, diarrhea, dyspepsia, weakness, and emaciation. In acute pancreatitis, pain is usually felt in the left side. Unpleasant sensations can take on the character of “girdling” pain. In other words, they can spread to the entire left side and also extend to the back.
If symptoms of acute pancreatitis appear, you should consult a doctor, as this disease does not go away on its own. In addition, severe complications cannot be ruled out. Acute pancreatitis involves monitoring the patient and injecting him with drugs that reduce pain and inflammation.
Symptoms of exocrine insufficiency
Determining exocrine insufficiency is not particularly difficult. Its first sign of manifestation is a peculiar reaction of the digestive system to highly fatty foods, which is accompanied by a significant amount of various hot spices. Patients exhibit symptoms such as changes in stool, heartburn, attacks of nausea and vomiting, and most importantly, a feeling of heaviness in the stomach. This indicates a decrease in the performance of the pancreas, in particular in the small intestine of the digestive tract.
Due to the fact that the digestive system cannot cope with its direct functions, all food passes into the large intestine. Since digestion is impossible in full, the synthesis of colonocytes occurs. Therefore, disturbances in bowel movements appear, that is, the stool takes on a different shape, and the urge to visit the toilet increases. Feces can take different forms, but an unpleasant odor, a grayish tint, and a fatty or oily film always predominate. There will definitely be small pieces of food in the stool that have not been processed by the body. The number of urges to go to the toilet increases 5-6 times per day, which causes a person some discomfort in everyday life. The same state of health manifests itself in intrasecretory insufficiency.
Patients with deficiency disease also experience symptoms such as bloating and colic. This is accompanied by pain in the abdominal area. A decrease in protein breakdown affects the protein balance, and a deficiency of this element appears. A person rapidly loses body weight as dehydration occurs, accompanied by anemia. As a result, there is a lack of microelements, nutrients, and vitamins in the internal system. This condition poses a threat to the patient's life.
We also recommend viewing: Pancreatic pulsation: causes, diagnosis and treatment
The main symptoms include:
- feeling of constant weakness;
- rapid fatigue;
- decreased performance;
- tachycardia;
- difficulty breathing due to shortness of breath;
- the skin takes on an unnaturally pale hue.
Histological structure
Each island is an independently functioning element. Together they form a complex archipelago, which is made up of individual cells and larger formations. Their sizes vary significantly - from one endocrine cell to a mature, large islet (>100 µm).
In pancreatic groups, a hierarchy of cell arrangement is built, there are 5 types of them, all perform their role. Each island is surrounded by connective tissue and has lobules where capillaries are located.
In the center there are groups of beta cells, along the edges of the formations there are alpha and delta cells. The larger the islet, the more peripheral cells it contains.
The islets do not have ducts; the hormones produced are excreted through the capillary system.
Pancreatic oncology
Pancreatic cancer
occurs as a result of long-term infection of the canal, which spreads into the body of the organ. Blood vessels that are very close to the gland can take part in the proliferation of cancer cells.
The main risk categories include:
- aged people.
- people leading an unhealthy lifestyle and abusing bad habits.
Cancer treatment requires special attention from a person, since ignoring it can lead to death.
Endocrine part of the pancreas
⇐ PreviousPage 7 of 15Next ⇒The pancreas consists of exocrine and endocrine parts. Endocrine part
represented by groups of epithelial cells
(islets of Langerhans),
separated from the exocrine part of the gland by thin connective tissue layers. Most of the islets are concentrated in the tail of the pancreas. The sizes of pancreatic islets range from 0.1 to 0.3 mm, and their total mass does not exceed 1/100 of the mass of the pancreas.
Pancreatic islets have two main types of glandular cells. Cells that synthesize insulin are called beta (or b) cells; cells that produce glucagon are alpha (or a) cells.
Insulin
is a protein hormone with a molecular weight of about 6000 Da. It is formed from proinsulin under the influence of proteases. The conversion of proinsulin to the active hormone insulin occurs in beta cells. Regulation of insulin secretion is carried out by the sympathetic and parasympathetic nervous system, as well as under the influence of a number of polypeptides that are produced in the gastrointestinal tract.
Glucagon -
a polypeptide consisting of a single chain with a molecular weight of about 3500 Da. It can also be produced in the intestines in the form of enteroglucagon.
Regulation of glucagon secretion is carried out using glucose receptors in the hypothalamus, which detect a decrease in blood glucose levels. This chain of interactions includes growth hormone, somatostatin, enteroglucagon, and the sympathetic nervous system.
Islet cell hormones have a significant impact on metabolic processes. Insulin is an anabolic hormone with a broad spectrum of action. Its role is to increase the synthesis of carbohydrates, fats and proteins. It stimulates glucose metabolism, increases the penetration of glucose into myocardial cells and skeletal muscles, which promotes a greater flow of glucose into the cell. Insulin lowers blood glucose levels, stimulates glycogen synthesis in the liver, and affects fat metabolism.
The main effect of glucagon is associated with increased metabolic processes in the liver, the breakdown of glycogen into glucose and its release into the bloodstream. Glucagon is a synergist of adrenaline. When blood glucose levels deviate from normal, hypo-
or
hyperglycemia.
With a lack of insulin or a change in its activity, the glucose content in the blood increases sharply, which can lead to the appearance
of diabetes mellitus
with corresponding clinical symptoms. High levels of glucagon in the blood cause the development of hypoglycemic conditions.
Endocrine part of the gonads
The testicle (testis) in men and the ovaries in women, in addition to germ cells, produce and release sex hormones into the blood, under the influence of which the formation of secondary sexual characteristics occurs.
The interstitium, which is represented by glandular cells - interstitial endocrinocytes,
testicles, or
Leydig cells,
which are located in the loose connective tissue between the convoluted seminiferous tubules, next to the blood and lymphatic vessels.
Interstitial endocrinocytes of the testicle secrete the male sex hormone - testosterone.
The ovary produces sex hormones such as estrogen, gonadotropin and progesterone. The place of formation of estrogen (folliculin) and gonadotropin is the granular layer of maturing follicles, as well as the interstitial cells of the ovary. Estrogen stimulates, and gonadotropin inhibits the growth and development of germ cells. Under the influence of follicle-stimulating and luteinizing hormones of the pituitary gland, follicles grow and interstitial cells are activated. Luteinizing hormone causes ovulation and the formation of the corpus luteum, the cells of which produce the ovarian hormone progesterone.
This hormone prepares the lining of the uterus for implantation of a fertilized egg, and also inhibits the growth of new follicles.
Regulation of endocrine glands
Endocrine glands and the hormones they secrete are closely related to the nervous system and form a common integration mechanism of regulation. The regulatory influence of the central nervous system on the physiological activity of the endocrine glands is carried out through the hypothalamus. In turn, the hypothalamus is connected through afferent pathways with other parts of the central nervous system (with the spinal cord, medulla oblongata and midbrain, thalamus, basal ganglia, cerebral cortex fields, etc.). Thanks to these connections, the hypothalamus receives information from all parts of the body: signals from extero- and interoreceptors go to the central nervous system through the hypothalamus and are transmitted to the endocrine organs.
Thus, the neurosecretory cells of the hypothalamus convert afferent stimuli into humoral factors with physiological activity (releasing hormones,
or
liberins),
which stimulate the synthesis and release of pituitary hormones.
And hormones that inhibit these processes are called inhibitory hormones
(or factors) or
statins.
Hypothalamic releasing hormones influence the function of pituitary cells, which produce a number of hormones. The latter, in turn, influence the synthesis and secretion of hormones from the peripheral endocrine glands, and these affect the target organs or tissues. All levels of this system of interactions are closely interconnected by a feedback system.
In addition, it is known that various hormones also affect the functions of parts of the central nervous system.
Mediators of sympathetic and parasympathetic nerve fibers play an important role in regulating the function of the endocrine glands.
However, there are endocrine glands (parathyroid, pancreas, etc.), which are regulated in a different way due to the influence of the level of antagonist hormones, as well as as a result of changes in the concentration of those metabolites (substances), the level of which is regulated by these hormones. There are some hormones produced in the hypothalamus (antidiuretic hormone, oxytacin), pituitary hormones that directly affect target organs and tissues.
Thus, the regulation of endocrine glands in the human body is a complex system with many unknown processes.
Questions for self-control
1. Tell us about the role of the endocrine glands in the human body.
2. Explain the structure of the pituitary gland and its connection with other endocrine glands.
3. What do you know about the hormones of the anterior pituitary gland?
4. Name the functional features of the posterior lobe of the pituitary gland.
5. Structure and functional features of the thyroid gland.
6. The structure and role of the parathyroid glands in the body and their position.
7. Tell us about the role of the thymus gland for the human body.
8. Features of the structure and function of the adrenal glands.
9. What role do adrenal hormones play in the body?
10. Tell us about the endocrine function of the pancreas.
11. What endocrine functions do the gonads perform?
12. Explain how the regulation of the endocrine glands occurs.
Practical lessons
The purpose of the classes is
study the anatomical and histological structure of the endocrine glands.
Equipment -
a set of histological preparations, electron micrographs, diagrams, tables, slides, microscope, overhead projector.
The content of the work.
The student must know: 1) the general structure of the endocrine system; 2) study using histological preparations and microphotographs: a) pituitary gland; b) thyroid gland; c) adrenal gland; d) pancreas; 3) functions of the endocrine glands; 4) principles of regulation of endocrine glands.
Drawing up the protocol.
Draw a diagram of the structure of pancreatic insulocytes; diagram of a glandulocyte and give designations. Write down the main hormones produced by the glands of the endocrine system.
THE CARDIOVASCULAR SYSTEM
Performing one of the main functions - transport - the cardiovascular system ensures the rhythmic flow of physiological and biochemical processes in the human body. All necessary substances (proteins, carbohydrates, oxygen, vitamins, mineral salts) are delivered to tissues and organs through blood vessels and metabolic products and carbon dioxide are removed. In addition, hormonal substances produced by the endocrine glands, which are specific regulators of metabolic processes, and antibodies necessary for the body’s protective reactions against infectious diseases are carried through the blood vessels into organs and tissues. Thus, the vascular system also performs regulatory and protective functions. In collaboration with the nervous and humoral systems, the vascular system plays an important role in ensuring the integrity of the body.
The vascular system is divided into circulatory and lymphatic. These systems are anatomically and functionally closely related and complement each other, but there are certain differences between them. Blood in the body moves through the circulatory system. The circulatory system consists of the central circulatory organ - the heart, the rhythmic contractions of which allow blood to move through the vessels.
The structure of arteries, veins and capillaries. The vessels that carry blood from the heart to organs and tissues are called arteries,
and the vessels carrying blood from the periphery to the heart are called
veins.
The arterial and venous parts of the vascular system are connected to each other by capillaries,
through the walls of which the exchange of substances between blood and tissues occurs.
The arteries that supply the walls of the body are called parietal (parietal),
arteries of internal organs -
visceral (visceral).
According to the topographic principle, arteries are divided into extra-organ and intra-organ. The structure of intraorgan arteries depends on the development, structure and function of the organ. In organs that form a common mass during development (lungs, liver, kidneys, spleen, lymph nodes), the arteries enter the central part of the organ and then branch out into lobes, segments and lobules. In organs that are formed in the form of a tube (esophageal tract, excretory ducts of the genitourinary system, brain and spinal cord), the branches of the arteries have a ring-shaped and longitudinal direction in its wall.
There are main and scattered types of branching of arteries. With the main type of branching
there is a main trunk and lateral branches extending from the artery with a gradually decreasing diameter.
The loose type of branching
of the artery is characterized by the fact that the main trunk is divided into a large number of terminal branches.
Arteries that provide a roundabout flow of blood, bypassing the main path, are called collateral.
There are intersystem and intrasystem anastomoses. The former form connections between branches of different arteries, the latter - between branches of the same artery.
Intraorgan vessels are sequentially divided into arteries of the 1st-5th order, forming a microscopic system of vessels - the microvasculature.
It is formed from an arteriole, precapillary arteriole, or precapillaries, capillaries, postcapillary venules or postcapillaries and venules.
From the intraorgan vessels, blood enters the arterioles, which form rich blood networks in the tissues of the organs. Then the arterioles pass into thinner vessels - precapillaries,
the diameter of which is 40-50 microns, and the latter - into smaller ones -
capillaries
with a diameter of 6 to 30-40 microns and a wall thickness of 1 micron. The narrowest capillaries are located in the lungs, brain, and smooth muscles, while the widest ones are located in the glands. The widest capillaries (sinuses) are observed in the liver, spleen, bone marrow and lacunae of the cavernous bodies of the lobar organs.
In the capillaries, blood flows at a low speed (0.5-1.0 mm/s) and has low pressure (up to 10-15 mm Hg). This is due to the fact that the most intense exchange of substances between blood and tissues occurs in the walls of capillaries. Capillaries are found in all organs, except for the epithelium of the skin and serous membranes, tooth enamel and dentin, cornea, heart valves, etc. Connecting with each other, the capillaries form capillary networks, the features of which depend on the structure and function of the organ.
After passing through the capillaries, the blood enters the postcapillary venules, and then into the venules, the diameter of which is 30-40 microns. From the venules, the formation of intraorgan veins of the 1st–5th order begins, which then flow into extraorgan veins. In the circulatory system, there is also a direct transition of blood from arterioles to venules - arteriole-venular anastomoses.
The total capacity of venous vessels is 3-4 times greater than that of arteries. This is due to pressure and low blood velocity in the veins, compensated by the volume of the venous bed.
Vienna
are depots for venous blood. The venous system contains about 2/3 of the body's total blood. Extraorgan venous vessels, connecting with each other, form the largest venous vessels of the human body - the superior and inferior vena cava, which enter the right atrium.
Arteries differ in structure and functional purpose from veins. Thus, the walls of the arteries resist blood pressure and are more elastic and stretchable. Thanks to these qualities, the rhythmic flow of blood becomes continuous. Depending on the diameter, arteries are divided into large, medium and small.
The wall of the arteries consists of the inner, middle and outer membranes. The inner membrane is formed by the endothelium, basement membrane and subendothelial layer. The middle shell consists mainly of smooth muscle cells in a circular (spiral) direction, as well as collagen and elastic fibers. The outer shell is built of loose connective tissue, which contains collagen and elastic fibers and performs protective, insulating and fixing functions, has blood vessels and nerves. The inner lining does not have its own vessels; it receives nutrients directly from the blood.
Depending on the ratio of tissue elements in the wall, arteries are divided into elastic, muscular and mixed types. To elastic type
include the aorta and pulmonary trunk.
These vessels can become very stretched when the heart contracts. Arteries of the muscular type
are found in organs that change their volume (intestines, bladder, uterus, arteries of the extremities).
The mixed type (muscular-elastic)
includes the carotid, subclavian, femoral and other arteries. As you move away from the heart, the number of elastic elements in the arteries decreases and the number of muscle elements increases, and the ability to change the lumen increases. Therefore, small arteries and arterioles are the main regulators of blood flow in organs.
The capillary wall is thin, consists of a single layer of endothelial cells located on the basement membrane, determining its metabolic functions.
The wall of veins, like arteries, has three membranes: internal, middle and external.
The lumen of the veins is slightly larger than that of the arteries. The inner layer is lined with a layer of endothelial cells, the middle layer is relatively thin and contains few muscle and elastic elements, so the veins collapse when cut. The outer layer is represented by a well-developed connective tissue membrane. Along the entire length of the veins there are valves located in pairs that prevent the reverse flow of blood. There are more valves in the superficial veins than in the deep veins, and in the veins of the lower extremities than in the veins of the upper extremities. Blood pressure in the veins is low, there is no pulsation.
Depending on the topography and position in the body and organs, veins are divided into superficial and deep. On the extremities, deep veins accompany arteries of the same name in pairs. The name of the deep veins is similar to the name of the arteries to which they are adjacent (brachial artery - brachial vein, etc.). Superficial veins connect to deep veins using penetrating veins, which act as anastomoses. Often neighboring veins, connected to each other by numerous anastomoses, form venous plexuses on the surface or in the walls of a number of internal organs (bladder, rectum). Between the large veins (superior and inferior vena cava, portal vein) there are intersystem venous anastomoses - cavo-caval, portacaval and cavo-portacaval, which are collateral pathways for the flow of venous blood bypassing the main veins.
The location of the vessels of the human body corresponds to certain patterns: the general type of structure of the human body, the presence of an axial skeleton, symmetry of the body, the presence of paired limbs, asymmetry of most internal organs. Usually the arteries are directed to the organs by the shortest route and approach them from their inner side (through the gate). On the extremities, the arteries run along the flexor surface and form arterial networks around the joints. On the bony base of the skeleton, arteries run parallel to the bones, for example, the intercostal arteries run next to the ribs, and the aorta runs next to the spine.
In the walls of blood vessels there are nerve fibers associated with receptors that perceive changes in the composition of the blood and the vessel wall. There are especially many receptors in the aorta, carotid sinus, and pulmonary trunk.
The regulation of blood circulation both in the body as a whole and in individual organs, depending on their functional state, is carried out by the nervous and endocrine systems.
Heart
Heart
(cor) is a hollow, muscular organ of a cone shape, weighing 250-350 g, ejects blood into the arteries and receives venous blood (Fig. 87, 88).
Rice. 87.
Heart (front view):
1 —
aorta;
2 -
brachiocephalic trunk;
3 -
left common carotid artery;
4—
left subclavian artery;
5—ligament arteriosus (fibrous cord at the site of the overgrown ductus arteriosus); 6—
pulmonary trunk;
7 - left ear; 8, 15 -
coronal groove;
9 -
left ventricle;
10—
apex of the heart;
11—
cutting of the apex of the heart;
12—
sternocostal (anterior) surface of the heart;
13 -
right ventricle;
14 -
anterior interventricular groove;
16—
right ear;
17—
superior vena cava
Rice. 88.
Heart (opened):
1 - semilunar valves of the aortic valve; 2 - pulmonary veins; 3 —
left atrium;
4, 9—
coronary arteries;
5 -
left atrioventricular (mitral) valve (bicuspid valve);
6—
papillary muscles;
7— right ventricle; 8 -
right atrioventricular (tricuspid) valve;
10 -
pulmonary trunk;
11—
superior vena cava;
12—
aorta
It is located in the chest cavity between the lungs in the lower mediastinum. Approximately 2/3 of the heart is in the left side of the chest and 1/3 is in the right. The apex of the heart is directed down, left and forward, the base is directed up, right and back. The anterior surface of the heart is adjacent to the sternum and costal cartilages, the posterior surface is adjacent to the esophagus and thoracic aorta, and below is to the diaphragm. The upper border of the heart is located at the level of the upper edges of the third right and left costal cartilages, the right border runs from the upper edge of the third right costal cartilage and 1-2 cm along the right edge of the sternum, descends vertically down to the fifth costal cartilage; the left border of the heart continues from the upper edge of the third rib to the apex of the heart, running at the level of the middle of the distance between the left edge of the sternum and the left midclavicular line. The apex of the heart is determined in the intercostal space 1.0-1.5 cm inward from the midline. The lower border of the heart runs from the cartilage of the fifth right rib to the apex of the heart. Normally, the length of the heart is 10.0–15.0 cm, the largest transverse dimension of the heart is 9–11 cm, and the anteroposterior dimension is 6–8 cm.
The boundaries of the heart vary depending on age, gender, constitution and body position. A shift in the border of the heart is observed with an increase (dilatation) of its cavities, as well as in connection with thickening (hypertrophy) of the myocardium.
The right border of the heart increases as a result of splitting of the right ventricle and atrium with tricuspid valve insufficiency, narrowing of the mouth of the pulmonary artery, and chronic lung diseases. A shift in the left border of the heart is often caused by increased blood pressure in the systemic circulation, aortic heart defects, and mitral valve insufficiency.
On the surface of the heart, the anterior and posterior interventricular grooves are visible, which run in front and behind, and the transverse coronary groove, located in a ring. The heart's own arteries and veins pass through these grooves.
The human heart consists of two atria and two ventricles.
Right atrium
It is a cavity with a capacity of 100-180 ml, shaped like a cube, located at the base of the heart on the right and behind the aorta and pulmonary trunk. The right atrium includes the superior and inferior vena cava, coronary sinus and the smallest veins of the heart. The anterior part of the right atrium is the right auricle. The pectineus muscles protrude on the inner surface of the right atrial appendage. The dilated posterior part of the wall of the right atrium is the entry point of large venous vessels - the superior and inferior vena cava. The right atrium is separated from the left by the interatrial septum, on which the fossa ovale is located.
The right atrium is connected to the right ventricle via the right atrioventricular foramen. Between the latter and the entry point of the inferior vena cava there is the opening of the coronary sinus and the mouth of the smallest veins of the heart.
Right ventricle
It has the shape of a pyramid with the apex directed downward, and is located to the right and in front of the left ventricle, occupying most of the anterior surface of the heart. The right ventricle is separated from the left by the interventricular septum, which consists of muscular and membranous parts. At the top of the wall of the left ventricle there are two openings: behind is the right atrium - the ventricular opening, and in front is the opening of the pulmonary trunk. The right atrioventricular orifice is closed by the right atrioventricular valve, which has anterior, posterior and septal leaflets resembling triangular tendon plates. On the inner surface of the right ventricle there are fleshy trabeculae and cone-shaped papillary muscles with chordae tendineae, which are attached to the valve leaflets. When the muscles of the ventricle contract, the valves close and are held in this state by the chordae tendineae; contraction of the papillary muscles prevents blood from flowing back into the atrium.
Directly at the beginning of the pulmonary trunk is the pulmonary valve.
It consists of the anterior, left and right posterior semilunar valves, which are located in a circle, with the convex surface towards the ventricular cavity, and the concave surface into the lumen of the pulmonary trunk. When the muscles of the ventricle contract, the semilunar valves are pressed against the wall of the pulmonary trunk by the blood flow and do not interfere with the flow of blood from the ventricle; and when the ventricle relaxes, when the pressure in its cavity drops, the reverse flow of blood fills the pockets between the walls of the pulmonary trunk and each of the semilunar valves and opens the valves, their edges close and do not let blood into the ventricle of the heart.
Left atrium
has the shape of an irregular cube, separated from the right atrium by the interatrial septum; has a left ear in front. In the posterior section of the upper wall of the atrium, four pulmonary veins open, through which blood enriched in O2 flows in the lungs. It is connected to the left ventricle via the left atrioventricular orifice.
Left ventricle
has the shape of a cone, with the base directed upward. In its anterosuperior section there is the opening of the aorta, through which the ventricle is connected to the aorta. Where the aorta exits the ventricle is the aortic valve, which has right, left (anterior) and posterior semilunar valves. Between each valve and the wall of the aorta there is a sinus. The aortic valves are thicker and larger than those in the pulmonary trunk. The atrioventricular orifice contains the left atrioventricular valve with anterior and posterior triangular leaflets. On the inner surface of the left ventricle there are fleshy trabeculae and anterior and posterior papillary muscles, from which thick chordae tendineae extend to the cusps of the mitral valve.
The heart wall consists of three layers: the inner - endocardium, the middle - myocardium and the outer - epicardium.
Endocardium
is a layer of endothelium lining all the cavities of the heart and tightly fused with the underlying muscle layer. It forms the heart valves, semilunar valves of the aorta and pulmonary trunk.
Myocardium
is the thickest and functionally most powerful part of the heart wall; formed by cardiac striated muscle tissue and consists of cardiac cardiomyocytes connected to each other by intercalary discs. Uniting into muscle fibers or complexes, myocytes form a narrow-loop network that ensures rhythmic contraction of the atria and ventricles. The thickness of the myocardium is uneven: the greatest is in the left ventricle, the smallest in the atria. The ventricular myocardium consists of three muscle layers - outer, middle and inner. The outer layer has an oblique direction of muscle fibers running from the fibrous rings to the apex of the heart. The fibers of the inner layer are arranged longitudinally and give rise to papillary muscles and fleshy trabeculae. The middle layer is formed by circular bundles of muscle fibers, separate for each ventricle.
The atrial myocardium consists of two layers of muscles - superficial and deep. The surface layer has a circular or transverse direction of fibers, and the deep layer has a longitudinal direction. The superficial layer of muscles covers both atria simultaneously, and the deep layer covers each atrium separately. The muscle bundles of the atria and ventricles are not connected to each other.
The muscle fibers of the atria and ventricles originate from the fibrous rings that separate the atria from the ventricles. Fibrous rings are located around the right and left atrioventricular openings and form a kind of skeleton of the heart, which includes thin rings of connective tissue around the openings of the aorta, pulmonary trunk and the adjacent right and left fibrous triangles.
Epicardium -
the outer layer of the heart, which covers the outside of the myocardium and is the inner layer of the serous pericardium. The epicardium consists of thin connective tissue covered with mesothelium and covers the heart, the ascending aorta and pulmonary trunk, and the terminal sections of the vena cava and pulmonary veins. Then from these vessels the epicardium passes into the parietal plate of the serous pericardium.
Conduction system of the heart. The regulation and coordination of the contractile function of the heart is carried out by its conduction system, which is formed by atypical muscle fibers (cardiac conduction muscle fibers), which have the ability to conduct stimuli from the nerves of the heart to the myocardium and automaticity.
The centers of the conduction system are two nodes: 1) the sinus-atrial node, located in the wall of the right atrium between the opening of the superior vena cava and the right ear and giving off branches to the atrial myocardium;
2) atrioventricular, located in the thickness of the lower part of the interatrial septum. The atrioventricular bundle (bundle of His) departs from this node, which continues into the interventricular septum, where it is divided into right and left legs, which then pass into the final branching fibers (Purkine fibers) and end in the ventricular myocardium.
Blood supply and innervation of the heart. The heart receives arterial blood, usually from two coronary (coronary) arteries, the left and right. The right coronary artery begins at the level of the right aortic sinus, and the left coronary artery begins at the level of its left sinus. Both arteries begin from the aorta, slightly above the semilunar valves, and lie in the coronary sulcus. The right coronary artery passes under the right atrial appendage, along the coronary groove around the right surface of the heart, then along the posterior surface to the left, where it anastomoses with a branch of the left coronary artery. The largest branch of the right coronary artery is the posterior interventricular branch, which along the same groove of the heart is directed towards its apex. The branches of the right coronary artery supply blood to the wall of the right ventricle and atrium, the posterior part of the interventricular septum, the papillary muscles of the right ventricle, the sinoatrial and atrioventricular nodes of the conduction system of the heart.
The left coronary artery is located between the beginning of the pulmonary trunk and the appendage of the left atrium, and is divided into two branches: the anterior interventricular and flexor. The anterior interventricular branch runs along the heart groove of the same name towards its apex and anastomoses with the posterior interventricular branch of the right coronary artery. The left coronary artery supplies the wall of the left ventricle, the papillary muscles, most of the interventricular septum, the anterior wall of the right ventricle, and the wall of the left atrium. The branches of the coronary arteries make it possible to supply blood to all the walls of the heart. Due to the high level of metabolic processes in the myocardium, microvessels anastomosing among themselves in the layers of the heart muscle repeat the course of muscle fiber bundles. In addition, there are other types of blood supply to the heart: right coronary, left coronary and middle, when the myocardium receives more blood from the corresponding branch of the coronary artery.
There are more veins of the heart than arteries. Most of the large veins of the heart gather into one venous sinus.
The following flow into the venous sinus: 1) the great vein of the heart -
departs from the apex of the heart, the anterior surface of the right and left ventricles, collects blood from the veins of the anterior surface of both ventricles and the interventricular septum;
2) middle vein of the heart -
collects blood from the posterior surface of the heart;
3) small vein of the heart -
lies on the posterior surface of the right ventricle and collects blood from the right half of the heart;
4) posterior vein of the left ventricle -
is formed on the posterior surface of the left ventricle and drains blood from this area;
5) oblique vein of the left atrium -
originates on the posterior wall of the left atrium and collects blood from it.
There are veins in the heart that directly open into the right atrium: the anterior veins of the heart,
into which blood enters from the anterior wall of the right ventricle, and
the smallest veins of the heart,
flowing into the right atrium and partially into the ventricles and left atrium.
The heart receives sensitive, sympathetic and parasympathetic innervation.
Sympathetic fibers from the right and left sympathetic trunks, passing as part of the cardiac nerves, transmit impulses that accelerate the heart rate, expand the lumen of the coronary arteries, and parasympathetic fibers conduct impulses that slow the heart rate and narrow the lumen of the coronary arteries. Sensitive fibers from the receptors of the walls of the heart and its vessels go as part of the nerves to the corresponding centers of the spinal cord and brain.
The innervation diagram of the heart (according to V.P. Vorobyov) is as follows. The sources of innervation of the heart are the cardiac nerves and branches that go to the heart; extraorgan cardiac plexuses (superficial and deep), located near the aortic arch and pulmonary trunk; intraorgan cardiac plexus, which is located in the walls of the heart and is distributed throughout all its layers.
The upper, middle and lower cervical, as well as thoracic cardiac nerves begin from the cervical and upper II-V nodes of the right and left sympathetic trunks. The heart is also innervated by cardiac branches from the right and left vagus nerves.
The superficial extraorgan cardiac plexus lies on the anterior surface of the pulmonary trunk and on the concave semicircle of the aortic arch; the deep extraorgan plexus is located behind the aortic arch (in front of the tracheal bifurcation). The superficial extraorgan plexus includes the superior left cervical cardiac nerve from the left cervical sympathetic ganglion and the superior left cardiac branch from the left vagus nerve. The branches of extraorgan cardiac plexuses form a single intraorgan cardiac plexus, which, depending on its location in the layers of the heart muscle, is conventionally divided into subepicardial, intramuscular and subendocardial plexuses.
Innervation has a regulatory effect on the activity of the heart, changing it in accordance with the needs of the body.
⇐ Previous7Next ⇒
Chronic pancreatitis
Its exacerbation is characterized by less intense pain. In addition, they tend to recur from time to time (after alcohol abuse or dietary errors). This disease does not require emergency surgery. However, this does not mean that it does not need to be treated. With chronic pancreatitis, as with any other dysfunction of the organ of interest to us, there is a failure of the digestive process. This negatively affects the health of the body.