Diseases of the digestive tract are not uncommon. Gastric transplantation is performed extremely rarely and is used for complex incurable pathologies. Before a digestive organ transplant operation, the doctor is obliged to inform the patient about the possible difficulties and benefits of surgical intervention. The process of organ transplantation itself is very dangerous and requires ideal training of doctors and good physical condition of the patient.
Gastric transplant: main indications
Digestive organ transplantation is performed after complete removal of the affected organ. Gastrectomy is performed for the following pathologies:
- stomach cancer;
- diffuse polyposis;
- ulcer with bleeding;
- perforation of the stomach lining;
- the latest form of obesity.
The appearance of a tumor on the medial part of the organ is the very first indication for gastrectomy. The condition of a damaged stomach due to cancer is severe and may be accompanied by secondary gastrointestinal diseases. With diffuse polyposis, when most of the organ is covered with polyps and which cannot be removed separately, the entire affected organ is removed. In case of an ulcer, the damaged organ is rarely removed, only in life-threatening conditions. In patients who are overweight, doctors may cut out the fundus of the stomach to limit the amount of food they eat.
Return to contents
Treatment Options
The main goal of treating the syndrome is to restore the patency of the sphincter of Oddi or eliminate other disorders accompanying the pain syndrome. Drug therapy is prescribed. The patient takes antispasmodic medications that relax the sphincter of Oddi and help remove obstructions in the path of bile. Such drugs cannot be used for a long time, as they have a number of side effects.
In rare cases, if there are other abnormalities in addition to the valve malfunction, surgery is prescribed. It is carried out to stop the inflammation that appears after removal of the gallbladder or removal of stones.
Preparing for surgery
Gastrectomy and transplantation require a lot of preliminary preparation, a detailed examination of the patient, and treatment of secondary diseases. A few weeks before the operation, the patient’s diet is reviewed, spicy, fried, salty, and alcohol are excluded from the diet. Smoking and taking medications are strictly prohibited.
Before undergoing a gastric transplant, you should consult with doctors. When diagnosed with heart disease, diabetes or pneumonia, they must be treated first so that the patient can safely undergo anesthesia and surgery.
Fluorography is a necessary study before surgery.
Before the procedure, tests such as:
- chemical analysis of blood and urine;
- fluorography;
- studies for hepatitis and HIV infections;
- Ultrasound of the abdominal organs;
- electrocardiography.
After all studies, the patient is observed in the hospital. The day before surgery, the patient's diet should be light, and 6 hours before surgery, food and water are prohibited for consumption. Otherwise, this may adversely affect the patient’s condition during the operation itself. The patient's health condition must be completely stable.
Return to contents
"I'm a culinary maniac"
I have stomach cancer, but I'm a culinary maniac. I believe that cooking is a construction set and any dish needs to be remade to suit you: you can add something, remove something. The other day I cooked chicken with grapes - I just put it in a roasting pan, added water, grapes and simmered it in the oven. No complicated steps. Maybe it’s not dietary, because I’m not a nutritionist, but it was delicious and I felt good after.
I knew my diet would have to change after surgery. Immediately after the diagnosis, I went online and started looking at what I could eat. Many things had to be changed radically, because I loved fatty, salty, and smoked foods - I did not deny myself any gastronomic pleasures.
After the removal of the stomach, I did not have enough information on nutrition - at the Herzen Moscow Research Institute of Oral Medicine, doctors gave detailed recommendations only for the first time after the operation. In general, it was clear that fried, highly salted and peppered foods were not allowed. But what foods can you still eat? In my extract it was written like this: “Regime: frequent split meals 6-7 times a day, every 2-2.5 hours. Single volume no more than 250 milliliters. After eating, do not lie down or bend over for 20 minutes. Last meal 2-3 hours before bedtime.” Dietary recommendations - list of products, half an A4 sheet.
Steam omelet with broccoliPhoto: Nikita Poludo
It turned out that there is practically no information on nutrition on the Internet, or rather, it is presented in such a way that a person gets lost. Those who have never cooked and cannot come up with a dish need an example, step-by-step recipes with photos. And the recommendations - for the same diet No. 0b - simply give a set of products. Everything is written as for doctors - there are practically no specifics, at most the menu is written for one day. At the same time, not everyone understands what it means to steam, that it is not necessary to buy a steamer and for vegetables you can use the same colander. People sometimes ask me what pureed soup is, what it means to “poach” or “blanch.” I believe that all this needs to be discussed together with doctors. And it’s good when the doctor explains what the diet should be, how much protein, carbohydrates, and kilocalories there should be per day. But we don’t have that.
Now there are more than 400 members in my “Life after Gastric Removal” group on Facebook. These people actively communicate and share advice with each other. Thanks to the group, I learned that doctors in Moscow say one thing, but in the outback they forget to say about some things, for example, about vitamin B12 or iron. After removal of the stomach, the vitamin must be administered artificially, and iron must also be taken separately. Local oncologists don’t say this - but it’s easier to prevent anemia than to treat the consequences later. Or they don’t tell you that you need to periodically take a general blood test and monitor your sugar levels: since there is no stomach, it is absorbed faster.
I have published two articles with nutritional recommendations, and it says who wrote them. I don’t understand how you can just post a faceless reprint on the Internet. Any information must have a source. I have come across many recommendations that are not supported by anything - then how can you trust them?
How to find a donor?
The main problem with gastric transplantation is the shortage of donor organs. In Western Europe, anyone who has reached the age of majority and has the same blood type as the recipient can donate an organ. But in the CIS countries there is one more rule - the donor must be a blood relative of the patient. Before transplantation, he needs to donate blood to determine compatibility with the patient’s blood. And after a consultation of a whole group of doctors, weighing all the pros and cons, you can get a conclusion about the possibility of being a donor.
Return to contents
Diet
An important stage is the rapid transition to oral nutrition. In this case, all food should be served only in a crushed and ground state. We need to rethink our approach to nutrition.
The nutritionist prepares a special diet for the patient, which must be balanced so that there is a sufficient amount of nutrients, vitamins and important microelements. The following food groups are excluded from the diet:
- alcoholic and carbonated drinks;
- canned foods;
- legumes;
- fatty meats and fish;
- ice cream;
- chocolate products;
- fresh bread;
- spices;
- sour berries;
- citrus.
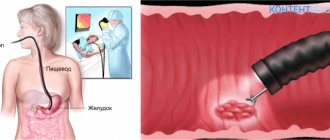
How it is carried out: stages of implementation
Opening the abdominal cavity is the first stage of the intervention.
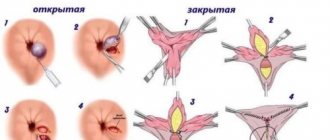
Gastric transplantation takes place in stages:
- Opening the abdominal cavity.
- Inspection of internal organs.
- Mobilization of the damaged organ.
- Installation of a donor stomach.
- The process of stitching blood vessels and tissues.
Mobilization of the stomach is the main part of the operation, which involves cutting the ligaments, omentum and suturing the small intestine. The pancreatic ligaments and vessels are intersected, and as they are dissected, the surgeon ligates the vessels. At the end of the operation, the surgeon connects the donor stomach to the small intestine and esophagus.
Return to contents
Side effects of anesthetics
Today, many different anesthetics have been developed, and which of them will be used in a particular case is determined by the anesthesiologist. His choice depends on the type and complexity of the surgical intervention, and whether the patient has contraindications to certain types of drugs. The experience and qualifications of the anesthesiologist matter.
Drugs for surgical anesthesia that provide general anesthesia are potent and have a number of side effects.
About a third of patients feel vomiting and dizziness after general anesthesia. These effects are due to a decrease in blood pressure. The patient must recover from anesthesia lying down without eating.
Confusion of thoughts, biased assessments of reality, and behavior deviating from the norm during recovery from anesthesia are more often observed in elderly patients. As the effect of the anesthetic wears off, this condition disappears.
Tremor of the limbs and head, general tremors of the body can be provoked by certain types of anesthetics. It is safe and lasts no more than half an hour.
Consequences after anesthesia may manifest as itchy sensations on the skin. This effect should be reported to the doctor, since it may equally indicate an allergy to medications and a side effect of morphine-type anesthetics.
What complications may arise?
The likelihood of difficulties after transplantation of a damaged organ is very high. The most possible complications are:
Bleeding after transplantation can occur due to incorrect surgical intervention when the suture is not tight. Dumping syndrome occurs if the patient consumes a large amount of food. It manifests itself in symptoms such as headaches, tachycardia, increased sweating and vomiting. Many patients in the postoperative stage suffer from vitamin deficiency, nutritional deficiency, resulting in drowsiness, weight loss, and weakness in the body.
Return to contents
Spectrum of symptoms
Symptoms of PCES may vary. In addition to the fact that the patient has a stomach ache, other abnormalities often develop after removal of the bladder:
- Pain in the right hypochondrium. The sensation may be mild or acute, depending on the severity of the problem. Acute pain occurs spontaneously, 2-3 times a month, causing discomfort in paroxysms. A few hours after the onset, the patient feels relief.
- Stomach dyspepsia (dysfunction). Mainly accompanied by bitterness in the mouth. In more advanced conditions, bloating, nausea, and occasionally vomiting are observed.
- Intestinal and stomach disorders. Constipation or diarrhea.
- Pain in right shoulder. This should not be considered a sign of another disease. Just unpleasant sensations from the right hypochondrium radiate to the shoulder or collarbone.
- Weakened state of the body. Due to impaired bile secretion, food is poorly digested and important vitamins do not enter the blood. Against this background, pale skin, increased fatigue, weakness, and drowsiness develop. Problems are observed when performing both mental and physical work, and the person does not understand why this is happening.
- Jaundice. This is a rare symptom; it occurs against the background of liver dysfunction. Bile stagnates in the organ, causing the color of the skin and whites of the eyes to change.
Deviations associated with cholangitis should be included in a separate category of symptoms. This is inflammation of the bile ducts. The disease develops against the background of an infection introduced into the ducts or bladder. It can get there through parasites transmitted by pets or through surgical instruments. In more than 50% of cases, cholangitis is directly related to removal of the gallbladder.
After removal of the organ, inflammation worsens, causing an increase in body temperature. Low-grade fever persists for a long time, from 37.1 to 38 degrees Celsius. This is not enough to cause a fever, but the person still feels weak.
Recovery
During the first stage of recovery, the patient receives nutrition through a vein.
After surgery, the patient is prescribed only intravenous nutrition. 2 days after the stomach transplant, the patient can drink water and eat light, completely ground food. If there were no complications, then the convalescent patient is gradually transferred to a dietary diet. But such nutrition should be done in small portions 6-8 times a day.
If the organ transplant was done correctly, the prognosis for the patient is optimistic. But the patient will have to make considerable efforts to restore the functioning of the digestive system so that the body receives the nutrients it needs. Physical activity is required to stimulate stomach function. The sooner the patient gets up after surgery (within reason), the greater the likelihood of a speedy recovery. A stomach transplant is a very rare operation, so doctors do not guarantee a complete recovery.
Source: EtoZheludok.ru
Recovery period
How to live without a stomach? Anyone who has had their stomach removed knows that rehabilitation is a long and difficult process.
The patient remains in the hospital for at least another 5-7 days, after which he is transferred to outpatient treatment. Antibiotics (to prevent secondary bacterial infection) and proton pump inhibitors (to suppress gland secretion) are necessarily prescribed.
Early activation of the body is also of great importance. It is advisable that on the second day he sits, and on the third he walks within his room. Subsequently, he is prescribed physical therapy exercises, which contribute to a faster recovery of the patient.
They also provide daily care for the postoperative scar. It is necessary to change the bandages, treat the wound with antiseptic solutions and monitor its condition.