For various severe diseases of the stomach, conservative treatment does not always give the expected effect. If the pathology is in an advanced stage, the patient is offered more radical therapy, in particular, surgery to remove tissue from the affected organ - resection. This method of treatment is complex, invasive and traumatic, but in many cases it is the patient’s only hope for successful healing. After the operation, various serious consequences may occur, however, if the patient follows all the doctor’s recommendations, the recovery period will go well.
What is this procedure?
Gastric resection is a surgical method for treating many diseases of the stomach, in which part of this organ is removed and the subsequent restoration of the integrity of the gastrointestinal tract with the formation of an anastomosis. If the stomach is completely removed without leaving a gastric stump, the operation is called a total gastrectomy.
Nowadays, gastric resection is a common and quite effective operation, which provides a wide range of possibilities for its implementation, and, therefore, for an individual approach to the patient and his disease. It’s hard to believe, but the first such operation took place in 1881 under the leadership of Theodor Billroth, whose name is given to one of the subtypes of resections used to this day.
Resection with preservation of the pylorus
Gastric resection usually takes place under endotracheal inhalation anesthesia. During the operation, the surgeon removes a strictly specific area of the stomach, which he had previously identified, and according to indications, both a more gentle resection (removal of a small area, most often the middle third) and a subtotal resection (in which almost the entire stomach and duodenum are removed) connects to the esophagus).
The variety of resection methods can create a false impression of prosperity in this branch of surgery, but only the imperfection of methods can stimulate the creation of new modifications of the operation. In the human body, everything is arranged harmoniously, and the removal of any part of an organ is not physiological and leads to corresponding consequences. Only vital necessity can be a serious reason for gastric resection.
Preparing for surgery
Before the operation, the doctor prescribes urine blood tests, x-rays, CT, MRI and other diagnostic methods.
They are needed in order to assess the patient’s health, the extent of cancer spread, and determine the extent of surgical intervention. Some patients have disorders in the body that require correction before surgery. In such cases, the doctor may prescribe IVs with water-salt solutions, blood transfusions and blood substitutes, red blood cells, drugs to improve the functioning of the cardiovascular system, antibiotics to prevent infections.
Indications for the procedure
Overweight and obesity are modern pandemics that are difficult to treat and sometimes require surgical intervention. The generally accepted basis for resection for the purpose of weight loss is a body mass index of 40 kg/m2 or higher (in the absence of concomitant diseases) and 35 kg/m2 or higher (for example, with diabetes mellitus or other severe pathology). Increased body weight contributes to rapid fatigue and high blood pressure, which is especially dangerous in later life. As weight loss occurs, concomitant symptoms (arterial hypertension, type 2 diabetes, etc.) decrease, which significantly prolongs the life of such patients.
This branch of medicine is called bariatric (metabolic) and has existed since 1966. The effectiveness of resection aimed at weight loss directly depends on the size of the removed area of the stomach. By reducing the volume of the organ, the surgeon achieves a smaller capacity and a quicker feeling of saturation. By consuming less food, the patient loses weight.
Before and after the procedure
Despite many plastic surgeries performed to eliminate stenosis of any part (for example, the pylorus), additional resection of the area is still resorted to. Resection is also used for organic lesions, for example, peptic ulcers (peptic ulcers directly caused by the digestive process in the stomach). In addition, an absolute indication for surgical intervention will be penetration (transition of the ulcerative process) to other nearby organs and perforation with bleeding. The operation is also performed in cases of long-term non-healing ulcers in elderly people.
Since the ulcer does not have the correct geometric shape, it is necessary to remove an area significantly larger than the size of the lesion. Despite many techniques aimed at maintaining normal digestion of food, resections are sometimes complicated by scarring and stenosis of the lumen. In this case, the surgeon must completely remove the ulcerative defect and stitch it in the most physiological position. In addition to surgical treatment, peptic ulcer requires long-term follow-up therapy due to the tendency to relapse.
Resection is the only truly effective treatment for stomach cancer in the early stages. Cancer (or carcinoma) can be found in any part of the stomach, which is a fundamental factor in choosing resection. If the lesion is located in the antrum, distal resection is preferred. If in the cardiac (or subcardial), then they make a choice in favor of the proximal one.
The stomach has an extensive network of lymphatic vessels, which ensures the rapid spread of cancer metastases inside the wall, into the peritoneum and lymph nodes. That is why in case of cancer, subtotal resection is most often performed, always giving preference to a more radical method.
Subtotal resection for oncology
Gastrectomy
A total (complete) gastrectomy is performed as a treatment for cancer localized in the middle part of the stomach. Surgical intervention is performed in the form of removal of the entire organ followed by the use of a Y-shaped anastomosis according to Roux. As a result of such an intervention, the esophagus becomes directly connected to the small intestine.
Extended gastrectomy is performed for patients whose cancer is located in the upper part of the stomach, or at the junction of the stomach with the esophagus. During this operation, surgeons remove not only the stomach. The following is removed along with it:
- A small part of the omentum (a small part of the peritoneum responsible for holding the stomach in its proper place);
- Spleen (an important organ of the immune system);
- Total or partial removal of the pancreas;
- Regional lymph nodes.
Classification of intervention methods
Depending on the location of the operated part of the stomach, proximal (cardial or subcardial) and distal (antrum) resections can be distinguished. With the development of endoscopy, more and more people are trying to resort to laparoscopic surgery, bypassing wide incisions.
The volume of intervention performed also matters; there are:
- economical resection of a third or half of the stomach;
- extensive resection of 2/3 of the stomach;
- subtotal resection of the stomach with preservation of 1/5 of the organ.
Theodor Billroth is the founder of gastric surgery; the invented method of resection is known and is still used in two versions. Billroth-1 is a less radical operation in which the anastomosis is formed “end to end”. Billroth-2 provides convenient suturing of the gastric stump without tension on the sutures and narrowing of the opening with greater possibilities for removal. Statistics confirm the fact that Billroth-1 is more dangerous than Billroth-2. Since there is no difference in the postoperative period, and in case of cancer early metastasis must be taken into account, Billroth-2 is preferred.
Billroth-2 underwent numerous modifications. For example, when modifying according to Balfour, an anastomosis is applied between the stomach and intestines on the jejunum, additionally forming an interintestinal anastomosis (using the Brown method). The Hoffmeister-Finsterer method is used more often, since a kind of artificial valve is formed, replacing the previously removed antral valve. In this case, food is not thrown into the intestines too quickly, and dumping syndrome does not occur.
Other operation modifications
Longitudinal gastrectomy has a short history; the first such operation was performed in 2000. The purpose of resection, unlike other types, is not organic damage to the stomach, but to improve the quality of life. As part of bariatric medicine, gastrectomy is effective for weight loss.
The operation is performed under general anesthesia and lasts several hours (usually 2-3 hours). The surgeon removes most of the stomach along its side, ensuring the safety of the valves and areas of production of hydrochloric acid, pepsin, and the area of absorption of vitamin B12. By removing the side wall of the stomach, the surgeon also affects the feeling of hunger and satiety, since the side wall contains the production zone of the hormone ghrelin, which is responsible for the feeling of hunger.
Laparoscopic gastrectomy
This operation is performed using a special laparoscope apparatus, which minimizes the surgeon’s intervention inside the body. It does not require wide incisions. When using a laparoscope, the doctor operates an instrument that is similar to an elastic tube. It has a special eyepiece, through which the doctor examines the abdominal cavity. The laparoscope allows the use of small instruments that the surgeon uses through an eyepiece. In most laparoscope operations, it is enough to create several small incisions (no more than 1 centimeter in length) through which a tube is inserted. But in some cases, they may be a little wider. In the hands of an experienced specialist, this device will help remove part or all of the organ.
Statistics show that treating patients with laparoscopic surgery significantly reduces the development of a number of complications when compared with traditional surgical methods. Doctors also give more positive prognoses for a speedy recovery.
But there are also disadvantages to this method of treatment, which do not occur very often, but still bring some inconvenience to the surgeon’s work. In rare cases, during a laparoscope operation, the doctor is forced to switch to the standard operating method. This may be caused by the inconvenient location of the tumor or its large size. Sometimes the reasons lie behind complex bleeding that cannot be controlled with a laparoscope.
Consequences of gastric resection
As mentioned earlier, removal of part of the stomach is not a physiological situation, which, although therapeutic in nature, has associated complications. The strength and severity depend on the volume of the intervention performed and the volume of tissue removed: the larger the area that was resected, the sooner the patient will encounter a disorder in the gastrointestinal tract. Not everyone experiences such complications, but the frequency of such cases has made it possible to identify a whole separate group of post-gastroresection syndromes.
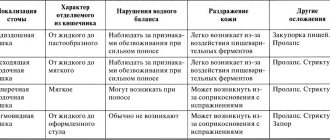
Dumping syndrome
The most specific complication of gastric resection is dumping syndrome (failure syndrome). Patients report characteristic symptoms after eating:
- palpitations, dizziness;
- dyspeptic disorders (nausea, vomiting);
- weakness and neurotic signs (tic, etc.).
Due to the fact that the stomach is reduced, its shape changes slightly, and this leads to the rapid passage of food through the stomach into the intestines. The osmotic characteristics of such food, which has not actually gone through the stage of digestion in the stomach, differ from those usual in the intestines, which leads to inadequate absorption of fluid and resulting hypovolemia.
There are three stages of dumping syndrome severity, determined by the condition's impact on organ systems.
- In mild cases, only rare attacks accompanied by dyspepsia are observed.
- With a moderate degree, blood pressure, tachycardia, and dyspeptic symptoms increase.
- The third degree is characterized by regular attacks with loss of consciousness, severe metabolic disorders, and cachexia.
Treatment in mild cases can be carried out conservatively, by normalizing the diet (eating in small portions and often, diet therapy), the third degree is subject to surgical treatment.
Anastomasis
Anastomositis is inflammation at the site of anastomosis, the formed junction of cut sections of the gastrointestinal tube. Often, such inflammation is accompanied by a pathological narrowing of the stomach and difficulty in passing the bolus of food further through the intestines, which causes stretching of the gastric wall, pain, nausea and vomiting. If left untreated, anastomositis leads to deformation of the stomach and the need for repeated surgery.
When forming gastroenteroanastomoses on a long loop, the food bolus passes mainly through the pyloric part of the stomach, and the food bolus, squeezing the efferent intestine, ensures difficult passage in it. A kind of vicious circle is formed, giving symptoms of nausea, vomiting, and exhaustion. The condition is diagnosed by X-ray examination and subsequently requires surgical intervention (removal of the anastomosis and part of the stomach, application of an additional anastomosis).
Possible complications
Complications often arise after gastrectomy has been performed. After surgery, the state of anastomotic obstruction is one of them. Often occurs from improper application or swelling. Bleeding into the peritoneal area is dangerous because anemia quickly develops. Intestinal obstruction also occurs. An extremely dangerous condition is postoperative peritonitis. Subsequently, a fistula may form due to incorrectly applied sutures. All these complications arise when the surgical technique is violated. They are extremely rare among experienced specialists. Doctors say that only about 5% of all surgeries require revision surgery. The rehabilitation period includes the following points: for the first six months it is necessary to limit physical activity and wear a special bandage; specialists also prescribe a special diet.
Diet and nutrition after surgery
During the first time after surgery, the patient is given intravenous parenteral nutrition solutions containing amino acids, carbohydrates and small amounts of fats. Two days after resection, the patient can drink liquids (decoctions, tea, compote) in small portions and often. Baby formulas begin to be administered through a tube. Gradually, the diet expands, and after two weeks the patient can independently adhere to a gentle diet, the purpose of which is to prevent inflammatory processes and complications (for example, dumping syndrome).
In the late postoperative period, it is better to give preference to purees and soups based on vegetables or cereals (but without cabbage or millet). The method of preparing other dishes can be steamed, oven-baked or boiled; fried foods should be avoided. You need to refrain from eating baked goods during the first month, and after that, control your consumption within reasonable limits. It is also better to limit plant foods containing a coarse fibrous structure. You can only eat lean meat; give preference to poultry (turkey, chicken). The fish consumed should also not contain large quantities of fat (bream, hake, cod, pike perch). Dairy products, milk and eggs can be eaten in limited quantities and not earlier than 2 months after surgery.
After removing part of the stomach, the patient will have to eat small portions and quite often (up to 5 times a day). Small portions will not cause discomfort, since the feeling of hunger does not form if the stomach is full. You should not try to increase single servings; this can lead to stretching of the gastric wall and the formation of an overly large stomach, which is undesirable for patients with existing obesity, which was the reason for seeing a doctor.
That is why, when forming a diet, they pay attention to the primary reason for visiting a doctor.
If the patient has suffered from a peptic ulcer for a long time, then the diet after gastrectomy in the postoperative period should limit the consumption of acidic foods, include the intake of mineral water and antacid and antibacterial (targeted Helicobacter Pylori) drugs.
Food
For a patient in the postoperative period, there are very strict dietary restrictions. Many foods that a healthy person eats are considered prohibited.
| Allowed | Forbidden |
|
|
A case of locally advanced gastric cancer
Statistics show that approximately 75% of patients suffer from stage III-IV gastric cancer at the time of hospitalization. This leads to the fact that quite often there is a need for combined operations - they are performed in 30-50% of cases.
Despite the fairly high degree of risk, today combined operations occupy a very important place in the treatment of gastric cancer - this is due to the peculiarities of local spread of the tumor and regional metastasis of the tumor. Even if we are talking about palliative surgery, the intervention in any case reduces the symptomatic manifestations of the disease and increases the life of patients.
The most common combination is surgery accompanied by splenectomy. Resection of the colon and its mesentery, diaphragm, adrenal gland, distal resection of the pancreas, left upper evisceration of the abdominal cavity, and gastropancreatoduodenal resection are performed somewhat less frequently.
Surgery is aimed at relieving symptoms
If surgery cannot be used for treatment, it can be performed for symptomatic therapy that will improve the patient's life. It is often required when there is complete or partial obstruction of food in the stomach. If the cancer has reached an impressive size, it can become an obstacle to the passage of food; this complication occurs quite often. In order to alleviate this condition, the patient undergoes surgery to remove part or all of the organ.
Some patients undergo surgery - bypass surgery. During such an intervention, the surgeon sutures a part of the stomach above the blockage, to the small intestine. This allows food masses to move freely through the gastrointestinal tract.
Even if the tumor has grown so large that it cannot be removed surgically, operations are carried out to alleviate the condition in any case. This method of treatment is called (palliative surgical treatment). Reviews from many doctors can say that patients feel better and, thanks to this treatment, live a little longer.
Removal of the stomach and part of the esophagus
When the tumor has managed to affect the esophagus, at the junction of it with the stomach, surgeons decide to perform an esophagogastrectomy. After such an operation, the upper esophagus remains permanently connected to the small intestine.
Some surgeons may save the patient's lower stomach from which a tube is formed. During this operation, the esophagus is connected not to the small intestine, but to the preserved part of the stomach.
The operation can be performed by making an incision on the abdominal wall or chest. Taking this into account, a scar on the body of a patient who was undergoing treatment for stomach cancer and underwent surgery to remove part of the esophagus with the stomach can be placed along one of the ribs, or in the middle part of the abdominal wall.