What is intestinal anastomosis, and in what cases is it prescribed?
Fistulas are a cause of colon cancer.
Anastomosis is the joining of two hollow organs and their suturing. In this case, we are talking about stitching together two parts of the intestine.
There are two types of intestinal operations that require subsequent anastomosis - enteroctomy and resection.
In the first case, the intestine is cut to remove the foreign body from it.
During resection, you cannot do without an anastomosis; in this case, the intestine is not just cut, but part of it is also removed, after which only two parts of the intestine are stitched together in one way or another (varieties of anastomosis).
Bowel anastomosis is a major surgical procedure. It is performed under general anesthesia, and after it the patient requires long-term rehabilitation, and complications are possible. Bowel resection with anastomosis may be prescribed in the following cases:
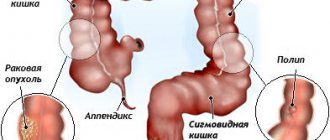
Colon cancer. Colon cancer occupies a leading place among cancer diseases found in developed countries. The cause of its occurrence may be fistulas, polyps, ulcerative colitis, and heredity. Resection of the affected area followed by anastomosis is prescribed in the initial stages of the disease, but can also be carried out in the presence of metastases, since leaving the tumor in the intestine is dangerous due to possible bleeding and intestinal obstruction due to tumor growth. Intestinal obstruction. Obstruction may occur due to a foreign body, tumor, or severe constipation. In the latter case, you can rinse the intestines, but for the rest, you will most likely have to undergo surgery. If the intestinal tissue has already begun to die due to compressed vessels, part of the intestine is removed and an anastomosis is performed. Intestinal infarction. With this disease, the flow of blood to the intestines is disrupted or completely stops. This is a dangerous condition that leads to tissue necrosis. It is more common in older people with heart disease. Crohn's disease. This is a whole complex of different conditions and symptoms that lead to intestinal dysfunction. This disease cannot be treated surgically, but patients have to undergo surgery, since life-threatening complications can arise during the course of the disease.
This video will tell you about colon cancer:
Postoperative diet
Diet and postoperative nutrition directly depend on which part of the intestine the operation was performed on. Nutrition after intestinal resection includes quickly digestible foods. Eat meals in small portions so as not to overload the intestines.
Nutrition is conventionally divided into a diet for the small and large intestines. This is due to the fact that different parts of the intestine perform different functions. Thus, each site has its own diet strategy and its own set of food products.
For the small intestine, which usually absorbs proteins, vitamins, and minerals from chyme (food moving along the entire length of the small intestine), the postoperative diet prescribes:
- Lean meat, vegetable protein (it is extremely important for the body that has undergone surgery, this substance accelerates wound healing).
- Butter and vegetable oil.
The following products are prohibited:
- The patient's diet should not contain plant fiber, which is found in radishes or cabbage.
- It is prohibited to drink drinks containing carbon dioxide and caffeine.
- The diet completely excludes beet and carrot juice.
- The patient's diet should not include foods that provoke intestinal motility (in particular, plums have this feature).
After resection of the large intestine, its ability to absorb minerals, water, and produce necessary enzymes and vitamins is impaired. Thus, the diet in the postoperative period should include foods that will compensate for these losses.
In order for the intestines to recover faster after surgery, bed rest should be strictly observed. A light massage of the anterior wall of the peritoneum will also help the intestines.
Sometimes a person develops a phobia of eating after surgery. In this case, a detailed conversation is held with the patient on the topic of postoperative nutrition. During this conversation, he is told about the need to change his diet and about the foods that need to be consumed.
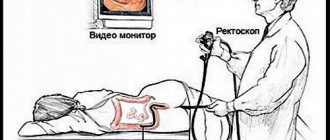
Preparation and procedure
Espumisan eliminates gases.
Such a serious procedure as intestinal anastomosis requires careful preparation. Previously, preparation was carried out using enemas and diet.
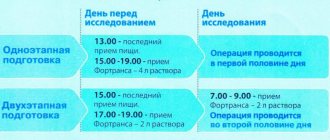
Now the need to follow a slag-free diet remains (for at least 3 days before the operation), but the day before the operation the patient is prescribed the drug Fortrans, which quickly and efficiently cleanses the entire intestine.
Before surgery, you should completely avoid fried foods, sweets, hot sauces, some cereals, beans, seeds and nuts.
You can eat boiled rice, boiled beef or chicken, and simple crackers. You should not break your diet, as this can lead to problems during surgery. Sometimes before surgery it is recommended to drink Espumisan to eliminate gases.
The day before the procedure, the patient only has breakfast and starts taking Fortrans from lunch. It is available in powder form. You need to drink at least 3-4 liters of the diluted drug (1 sachet per liter, 1 liter per hour). After taking the drug, painless watery stools begin within a couple of hours.
Fortrans is considered the most effective drug for preparing for various manipulations on the intestines. It allows you to completely clean it in a short time. The procedure itself is performed under general anesthesia. Anastomosis has 3 types:
"End to end." The most effective and frequently used method. It is only possible if the parts of the intestine being connected do not have a big difference in diameter. If it consists of slightly smaller parts, the surgeon slightly incises it and increases the lumen, and then sews the parts together edge to edge. "Side to side." This type of anastomosis is performed when a significant part of the intestine has been removed. After the resection, the doctor sutures both parts of the intestine, makes incisions and stitches them side to side. This surgical technique is considered the simplest. "End to side." This type of anastomosis is suitable for more complex operations. One of the parts of the intestine is stitched tightly, making a stump and first squeezing out all the contents. The second part of the intestine is sewn to the side of the stump. Then a neat incision is made on the side of the deaf intestine so that its diameter coincides with the second part of the intestine and the edges are sutured.
Bowel resection technique
Bowel resection surgery can be performed through laparotomy or laparoscopy. In the first case, the surgeon makes a longitudinal incision in the abdominal wall; the operation is performed in an open manner. The advantages of laparotomy are a good overview during all manipulations, as well as the absence of the need for expensive equipment and trained personnel.
With laparoscopy, only a few puncture holes are needed to insert laparoscopic instruments. Laparoscopy has many advantages, but is not always technically feasible, and for some diseases it is safer to resort to laparotomic access. The undoubted advantage of laparoscopy is not only the absence of a wide incision, but also a shorter rehabilitation period and faster recovery of the patient after the intervention.
After processing the surgical field, the surgeon makes a longitudinal incision in the anterior abdominal wall, examines the abdominal cavity from the inside and looks for the altered section of the intestine. Clamps are applied to isolate the portion of intestine that will be removed, and then the affected area is cut off. Immediately after dissection of the intestinal wall, it is necessary to remove part of its mesentery. Vessels feeding the intestine pass through the mesentery, so the surgeon carefully ties them up, and excises the mesentery itself in the shape of a wedge, with its apex facing the root of the mesentery.
Removal of the intestine is carried out within the healthy tissue, as carefully as possible, in order to prevent damage to the ends of the organ by instruments and not provoke their necrosis. This is important for the further healing of the postoperative suture on the intestine. When the entire small or large intestine is removed, it is called a total resection; subtotal resection involves excision of part of one of the sections.
subtotal resection of the large intestine
To reduce the risk of infection with intestinal contents during surgery, tissues are isolated with napkins and tampons, and surgeons practice changing instruments when moving from a more “dirty” stage to subsequent ones.
After removing the affected area, the doctor faces the difficult task of creating an anastomosis (connection) between the ends of the intestine. Although the intestine is long, it cannot always be stretched to the required length; the diameter of the opposite ends may differ, so technical difficulties in restoring the integrity of the intestine are inevitable. In some cases, this cannot be done; then the patient has an outlet hole placed on the abdominal wall.
Types of intestinal connections after resection:
- End to end is the most physiological and involves connecting the lumens in the same way as they were located before the operation. Disadvantage: possible scarring;
- Side to side - the opposite ends of the intestine are connected by their lateral surfaces;
- Side to end - used when connecting parts of the intestine with different anatomical characteristics.
If it is technically impossible to restore the movement of intestinal contents as physiologically as possible, or the distal end needs to be given time to recover, surgeons resort to placing an outlet on the anterior wall of the abdomen. It can be permanent, when large sections of the intestine are removed, or temporary, to speed up and facilitate the regeneration of the remaining intestine.
A colostomy is a proximal (near) segment of the intestine, removed and fixed to the abdominal wall, through which feces are evacuated. The distal fragment is sutured tightly. With a temporary colostomy, a second operation is performed after a few months, in which the integrity of the organ is restored using one of the methods described above.
Resection of the small intestine is most often performed due to necrosis. The main type of blood supply, when blood flows to the organ through one large vessel, then branches into smaller branches, explains the significant extent of gangrene. This happens with atherosclerosis of the superior mesenteric artery, and the surgeon in this case is forced to excise a large fragment of the intestine.
If it is impossible to connect the ends of the small intestine immediately after resection, an ileostomy is fixed to the surface of the abdomen to remove feces, which either remains permanently or is removed after several months with the restoration of a continuous flow of the intestine.
Resection of the small intestine can also be performed laparoscopically, when instruments are inserted into the abdomen through punctures, carbon dioxide is injected for better visibility, then the intestine is clamped above and below the site of injury, the mesenteric vessels are sutured and the intestine is excised.
Resection of the colon has some peculiarities, and it is most often indicated for neoplasms. In such patients, all, part of the colon, or half of it is removed (hemicolectomy). The operation lasts several hours and requires general anesthesia.
With an open approach, the surgeon makes an incision of about 25 cm, examines the colon, finds the affected area and removes it after ligating the mesenteric vessels. After excision of the large intestine, one of the types of end joining is performed or a colostomy is performed. Removal of the cecum is called a cecectomy, the ascending colon and half transverse or the descending colon and half transverse is hemicolectomy. Resection of the sigmoid colon - sigmoidectomy.
The operation for resection of the colon is completed by washing the abdominal cavity, layer-by-layer suturing of the abdominal tissue and installing drainage tubes into its cavity for the outflow of discharge.
Laparoscopic resection for lesions of the colon is possible and has a number of advantages, but is not always feasible due to severe damage to the organ. Often there is a need to switch from laparoscopy to open access right during surgery.
Operations on the rectum differ from those on other parts, which is associated not only with the structural features and location of the organ (strong fixation in the pelvis, proximity of the genitourinary system), but also with the nature of the function performed (accumulation of feces), which is unlikely to be possible. take over another part of the colon.
Resections of the rectum are technically complex and result in much more complications and unfavorable outcomes than those performed on the thin or thick sections. The main reason for interventions is cancer.
Resection of the rectum when the disease is located in the upper two-thirds of the organ makes it possible to preserve the anal sphincter. During the operation, the surgeon excises part of the intestine, ties the vessels of the mesentery and cuts it off, and then forms a connection that is as close as possible to the anatomical course of the terminal intestine - anterior resection of the rectum.
Postoperative period and complications
Eating cereals will reduce the load on the intestines.
After intestinal surgery, the patient must undergo a mandatory rehabilitation course. Unfortunately, complications after intestinal resection are very common even with highly professional surgeons.
In the first days after surgery, the patient is observed in the hospital. Minor bleeding is possible, but it is not always dangerous. Seams are regularly inspected and processed.
For the first time after surgery, you can only drink still water; after a few days, liquid food is acceptable. This is due to the fact that after such a serious operation you need to reduce the load on the intestines and avoid bowel movements for at least the first 3-4 days.
Proper nutrition is especially important during the postoperative period. It should provide loose stools and replenish the body's strength after abdominal surgery. Only those products are allowed that do not cause increased gas formation, constipation and do not irritate the intestines.
Liquid cereals, dairy products, after a while fiber (fruits and vegetables), boiled meat, and puree soups are allowed.
Complications after surgery can occur both due to the fault of the patient himself (non-compliance with the regime, poor diet, increased physical activity), and due to the fault of circumstances. Complications after anastomosis:
Infection. Doctors in the operating room follow all safety rules. All surfaces are disinfected, but even in this case it is not always possible to avoid infection of the wound. With infection, redness and suppuration of the suture, fever, and weakness are observed. Obstruction. The intestines may stick together after surgery due to scarring. In some cases, the intestine becomes bent, which also leads to obstruction. This complication may not appear immediately, but some time after the operation. It requires repeated surgery. Bleeding. Abdominal surgery is most often accompanied by blood loss. Internal bleeding is considered the most dangerous after surgery, since the patient may not notice it immediately.
It is impossible to completely protect yourself from complications after surgery, but you can significantly reduce the likelihood of their occurrence if you follow all the doctor’s recommendations, regularly undergo preventive examinations after surgery, and follow nutritional rules.
Tell your friends!
Share this article with your friends on your favorite social network using social buttons. Thank you!
Surgeries on the intestines are considered one of the most difficult. The surgeon must not only eliminate the pathology, but also maintain maximum functionality of the organ. To connect hollow organs during surgical interventions, a special technique is used - anastomosis.
Preventing complications
Complications of anastomoses may include:
- seam divergence;
- inflammation in the anastomosis area (anastomositis);
- bleeding from damaged vessels;
- formation of fistula tracts;
- formation of narrowing with intestinal obstruction.
To avoid adhesions and intestinal contents entering the abdominal cavity:
- the surgical site is covered with napkins;
- the incision for suturing the ends is carried out after clamping the intestinal loop with special intestinal sponges and squeezing out the contents;
- the incision of the mesenteric edge (“window”) is sutured;
- the patency of the created anastomosis is determined by palpation before completion of the operation;
- in the postoperative period, broad-spectrum antibiotics are prescribed;
- The rehabilitation course necessarily includes diet, physical therapy and breathing exercises.
Types of intestinal surgeries
Most often, operations performed on the intestine include enterotomy and resection. The first type is chosen if a foreign body is detected in the organ. Its essence lies in the surgical opening of the intestine with a scalpel or electric knife. The suture is selected depending on the section of the intestine, the presence or absence of an inflammatory process in the area of intervention. The wound is sutured with the so-called interrupted Gumby suture, making a puncture through the muscular, submucosal layer without capturing the mucous membrane, as well as with a Lambert suture, connecting the serous (covers the small intestine from the outside) and muscular membranes.
Resection means surgical removal of an organ or part of it. Before performing it, the doctor assesses the viability of the intestinal wall (color, ability to contract, presence of an inflammatory process). After the doctor marks the boundaries of the resected area, he selects the type of anastomosis.
Methods of anastomosis
There are several ways to perform an anastomosis. Let's look at them in detail.
End to end
End to end
This type is considered the most effective and is most often used if the difference in the diameter of the compared ends of the intestine is not very large. On the one that has a smaller diameter, the surgeon makes a linear incision to increase the lumen of the organ. Upon completion of resection of the sigmoid colon (this is the final region of the colon before transition to the rectum), this particular technique is used.
After intestinal surgery, the patient must undergo a course of rehabilitation: breathing exercises, therapeutic exercises, physical and dietary therapy. Together, these components will greatly increase the chances of effective recovery of the body.
Side to side
Side to side
It is used when resection of a large area is necessary or when there is a risk of severe tension at the anastomotic site. Both ends are closed with a double-row suture, and then the stumps are sutured with a continuous Lambert suture. Moreover, its length is 2 times the diameter of the lumen. The surgeon makes an incision and opens both stumps along the longitudinal axis, squeezes out the contents of the intestine, and then closes the edges of the wound with a continuous suture.
End to side
This type of anastomosis consists in the fact that the stump of the efferent intestine is closed using the “side to side” technique, the contents of the organ are squeezed out and compressed with intestinal sphincter. The open end is then applied to the side of the intestine, sewn using a continuous Lambert suture.
End to side
The next stage is when the surgeon makes a longitudinal incision and opens the efferent part of the intestine. Its length should correspond to the width of the open end of the organ. The anterior part of the anastomosis is also sutured with a continuous suture. This type of anamostosis is optimal for many interventions, even such complex ones as extirpation of the esophagus (meaning its complete removal, including the nearest lymph nodes and fatty tissue).
Intestinal anastomoses with any type of connection are used on the small and large intestines. But in the first case, a one-story suture is necessarily chosen (that is, all layers of tissue are captured), in the second - only two-story interrupted sutures (the first row consists of simple sutures through the thickness of the walls being stitched, and the second without puncture of the mucous membrane).
The main purpose of the anastomosis is to restore the continuity of the intestine after resection and to form a passage in case of intestinal obstruction. This technique allows you to save life and at least partially compensate for the role of removed organs. Even with hemicolectomy (removal of half of the colon with the formation of a bone fracture - an unnatural anus brought to the anterior abdominal wall), it allows you to preserve most of the functionality of the intestine.
Surgery on the rectum for oncology almost always involves its removal, especially if the tumor is “low”, that is, located close to the anus (less than 6 cm). The formation of an anastomosis is the only way to restore its patency, most often if an anterior resection of the organ is performed.
In 4-20% of cases (depending on the condition of the tissues and the professionalism of the doctor), complications arise: obstruction, insufficient sutures, peritonitis. To minimize the risk, the surgeon must carry out thorough sanitation of the suture and nearby areas on the lumen side.
Advice: to reduce the likelihood of complications, the patient should follow all the doctor’s recommendations and remember to independently monitor the connection. For example, in order to minimize the threat of developing narrowing and obstruction after removal of the stomach, it is worth regularly undergoing X-ray examinations.
Intestinal anastomosis is a unique surgical technique that allows you to connect hollow organs and at least partially restore the functionality of the intestine. Different application methods are used depending on the type of operation. To maximize the effectiveness of the anastomosis, the doctor needs to follow the technology and carefully treat the seam with antiseptics.
We recommend reading: how to cleanse the intestines before surgery
Attention! The information on the site is presented by specialists, but is for informational purposes only and cannot be used for independent treatment. Be sure to consult your doctor!
In almost all intestinal diseases requiring surgical intervention, an intestinal anastomosis is performed at the end of the operation. This allows you to restore the functionality of the organ, bringing the patient’s standard of living as close as possible to the period when there was no disease. Even if half of the large intestine is removed, this method gives a chance for the organ to resume functioning. However, this procedure does not always go smoothly, in some cases carrying with it the consequences of anastomotic leakage.
Intestinal anastomosis is a necessary surgical measure performed after certain types of surgery.
Recommendations for preparing for anastomosis
Colon anastomosis is a serious type of surgery. It requires a long and thorough restoration of the body and the functionality of the intestinal canal. Therefore, the patient after anastomositis should undergo a special rehabilitation course. This includes breathing training, physical therapy, and a strict diet. All these recommendations must be followed in their entirety.
One of the main rules is to follow a diet. It should be gentle so as not to injure the stomach and intestinal tract. Therefore, the diet should consist of soups and liquids for one to two months.
To avoid the development of peritonitis or other serious complications, the doctor must carry out thorough sanitation in the area of the surgical intervention and the suture. External cuts must be treated very well several times a day.
To avoid adhesions, the patient must control the patency of the intestinal canal. To be sure that everything is going well, you need to regularly perform x-ray examinations.
Types of intestinal surgeries
The type of intestinal surgery depends on the disease of the organ, as well as on the circumstances requiring surgical intervention. If the intestine ruptures, it must be stitched up. This operation is called enterorraphy. When a foreign body enters the intestine, enterotomy is used, when the intestine is opened, cleared of the foreign object and sutured. If it is necessary to create a stoma, a colostomy, jejunostomy, or ileostomy are performed, when a hole is made in the desired part of the intestine and brought to the surface of the peritoneum. If a tumor develops and it is impossible to remove it, an artificial canal is placed between the intestines past the neoplasm by applying an interintestinal anastomosis.
The anastomosis technique is used for intestinal resection, removal of the affected area of the intestine in order to restore the viability and functionality of the organ. The need for intestinal resection may be prompted by:
growing tumors; gangrene; caused by strangulation; volvulus; vascular thrombosis; tuberculosis; ulcerative colitis; actinomycosis.
What is anastomosis?
This is a procedure for fusion (natural way) or stitching (artificial process) of two hollow organs, creating a fistula between them. Natural processes occur mainly between capillaries and vessels, and have a beneficial effect on blood circulation throughout the body and internal organs of a person. Artificial anastomoses are applied between hollow organs, if necessary, using surgical thread, special instruments and the skillful hands of an experienced surgeon. An intestinal anastomosis can be laid between the intestines to connect them in the event of removal of part of the intestine, or to create a bypass channel in the event of intestinal obstruction. If the operation is performed at the junction of the stomach and small intestine, in this situation a gastroenteroanastomosis is performed.
Depending on the location, the interintestinal anastomosis is divided into small-intestinal, small-colic, and large-colic. Single-layer sutures are made on the small intestine - all balls of tissue are stitched. The large intestine is sewn with two-story interrupted sutures. The first row consists of sutures through all layers of tissue, the second row of sutures is made without touching the mucous membrane.
Consequences of surgery, complications, rehabilitation
The consequences of the operation may not always have a positive result, and complications after it are not uncommon:
- Special sterile operating room conditions , disinfected surfaces and instruments minimize the risk of infection. But if sterilization measures are not followed, the wound may become infected. In this case, redness, suppuration of the suture, fever, and weakness are observed.
- Internal bleeding is dangerous because, unlike external bleeding, it does not appear immediately.
Overlay methods
End to end
This method of anastomosis is used when the diameter of the connected parts of the intestine is almost the same. In this case, the smaller end is slightly cut and thus enlarged to the size of the second end, then these parts are sewn together. This type of anastomosis is considered the most effective and is ideal for similar operations on the sigmoid colon.
https://youtu.be/WVfSct2ImwE
Side to side method
This method is used in case of large-scale intestinal resection or when there is a threat of strong tension in the anastomotic area. In this case, both ends of the intestine are sutured with a double suture, but incisions are made on their lateral parts, which are then sutured side to side with a continuous suture. The lateral fistula between the intestines should be twice as long as the diameter of the lumen of the ends.
End to side
This type of anastomosis is used for more complex operations when significant intestinal resection is required. It looks like this. One end of the intestine is tightly sutured, creating a stump. The two ends of the intestine are then sutured side by side. An incision is made in the side of the stump, equal to the diameter of the hole in the second sewn end of the intestine. The end hole is sutured to the side incision on the stump.
Leakage of intestinal anastomosis
Despite all the positive aspects of this procedure, there are cases when the imposed intestinal anastomosis shows its failure. This manifests itself in different ways and at the beginning the consequences can be completely unnoticeable, without revealing any symptoms. However, bloating, increased heart rate, and fever may then appear. Then the patient develops peritonitis or the release of feces through the resulting fistula. These consequences of anastomotic failure may be accompanied by septicemic shock (the patient's blood pressure drops, the skin turns pale, urine does not enter the bladder, acute heart failure occurs, and fainting occurs).
The diversity of causes that are the causative agents of the symptoms that appear indicates that anastomotic failure can occur in all operated patients. Therefore, after surgery, every patient needs active health monitoring. If the patient does not show positive dynamics, and his condition worsens, you should sound the alarm and figure out what’s wrong. In such a situation, an x-ray of the chest and peritoneum, an extensive analysis of the cellular composition of the blood, computed tomography, irrigoscopy with a contrast agent are immediately prescribed. If the anastomosis fails, the level of leukocytes in the blood often rises, and x-rays show dilation of the intestinal loops.
Unsuccessful intestinal anastomosis is eliminated by repeated surgery followed by drug therapy.
Treatment of anastomotic leak
Elimination of insolvency depends on the cause of its occurrence. Patients with extensive peritonitis are prescribed laparotomy. In this case, the anastomosis is removed, the stitched ends of the intestines are renewed, and the anastomosis is reconstructed. After this, the intestines are thoroughly washed with saline solution with the addition of antibiotics. Next, the patient receives antibacterial therapy intravenously for 5 days.
In patients with local peritonitis the situation is simpler. It is enough for them to undergo a course of antibacterial therapy administered intravenously. However, if no improvement is observed, then laparotomy should not be delayed. If a fecal fistula has formed in the wound, then you can also do without a scalpel. If the fistula does not go away for a long time, the patient may need artificial nutrition. In this case, special attention should be paid to the surrounding areas of the skin so that feces do not cause irritation.