Hemorrhagic pancreatic necrosis is a severe pathology in which rapid death of groups of cells in the tissues of the pancreas is observed. This process is irreversible and inevitably leads to disruption of enzyme and humoral functions, which dramatically affects the general condition of the body.
The disease is dangerous because it has a fairly high risk of developing severe consequences for the body of varying degrees, including death.
Factors contributing to the destruction of pancreas
Alcohol is one of the causes of pancreatic disease.
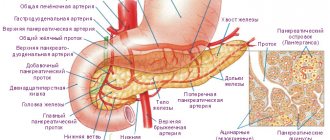
Pancreatic necrosis is a rather dangerous condition that directly threatens human life. There are a great many factors that can cause destruction of the pancreas. First of all, it is cholelithiasis. As you know, the cystic duct (gallbladder duct), like the pancreatic duct, directly opens into the duodenum. If there are stones in the gall bladder or ducts, a situation may arise when one of the stones blocks the outflow of pancreatic juice from the pancreas, as a result of which the pressure in the ducts of the gland increases, the secretion begins to be absorbed into the organ, which leads to “self-digestion” of tissues and their destruction .
Another dangerous factor that can cause destruction of the pancreas is certainly the abuse of alcohol and fatty foods. The influence of these two factors is often observed. This combination is deadly! If the diet is violated, a spasm of the sphincter of Oddi occurs (the hole through which the ducts of the gland open into the intestine), which again contributes to the disruption of the release of pancreatic juice and self-lysis of the organ.
Reasons for the development of pancreatic necrosis
Acute pancreatitis, a complication of which is pancreatic necrosis, is in third place in terms of frequency of occurrence, ahead only of acute appendicitis and cholecystitis. As a rule, it develops as a result of damage to the secretory cells of the pancreas, excessive production of pancreatic juice and disruption of its outflow. These processes can provoke:
- abdominal injuries;
- operations on the abdominal organs;
- intoxication of the body (including alcohol);
- allergic reactions;
- cholelithiasis;
- infectious or parasitic diseases;
- excessive consumption of fried meat, extractives, and animal fats.
The causes of pancreatic necrosis of the pancreas are numerous, but most often it develops after consuming large amounts of alcohol combined with fatty protein foods. It happens that the disease occurs almost instantly and an attack can develop against the background of complete well-being. Cases have been recorded in which pancreatic necrosis of the pancreas, a fatal outcome in which occurred within a matter of hours after the appearance of the first signs of the disease, developed several days after a heavy feast.
Symptoms characterizing pancreatic necrosis
All symptoms that occur with this disease can be divided into three main groups
Severe pain in the upper abdomen
- Clinical symptoms. These include acute, sharp pain in the upper or middle abdomen, which can spread to the left hypochondrium and radiate to the shoulder blade, back, often being encircling in nature. Along with pain, the patient develops symptoms such as nausea, and then repeated vomiting, which, for obvious reasons, does not bring relief. There may be an increase in body temperature and the appearance of loose stools, bloating, and flatulence. When examining such a patient, the doctor pays attention to the forced position - the patient is writhing in pain, trying to bend over, and does not allow him to touch his stomach. The skin acquires a bluish tint with purple spots.
- Laboratory symptoms. In a general blood test of a patient with pancreatic necrosis, significant leukocytosis, an increase in the erythrocyte sedimentation rate, and signs of blood thickening appear. Blood biochemistry is marked by an increase in liver tests, as well as a significant increase in the level of amylase and lipase in the blood, combined with a decrease in protein levels. An increase in diastase is detected in the urine.
- Instrumental symptoms. Instrumental diagnostic methods. Ultrasound examination of the organs of the hepatopancreatoduodenal zone, computed tomography, and diagnostic laparoscopy can confirm this diagnosis. During these examinations, symptoms such as an increase in the size of the gland, heterogeneity of its structure, and areas of necrosis and pus leakage can be detected.
How is diagnosis done?
The signs characteristic of hemorrhagic pancreatic necrosis are in many ways similar to the manifestations of other inflammatory diseases of the digestive system, so just examining the patient is not enough for diagnosis.
First, the doctor collects data for anamnesis, which includes answers to the following questions:
- whether the patient abuses alcohol;
- whether the person was intoxicated at the time of the development of clinical signs;
- whether the patient has liver or biliary tract diseases.
To clarify the primary diagnosis, the doctor issues an appointment for the following diagnostic examinations:
- a blood test that determines the level of presence of enzymes in pancreatic secretions. With hemorrhagic pancreatic necrosis, enzyme activity can be exceeded 6-9 times;
- urine analysis with determination of uroamylase and trypsinogen;
- determination of the acidity of stomach contents;
- Ultrasound of the abdominal organs to detect effusion;
- examination of pancreatic secretions by probing to identify bicarbonates and active enzymes;
- coproscopy, which helps to determine the percentage of unprocessed fat in feces;
- radiography of the pancreas;
- determination of amylase and triglycerides in exhaled air;
- endoscopic cholangiopancreatography;
- puncture to take a sample of necrotic tissue;
- magnetic resonance imaging and CT to identify foci of necrotic formations.
Conservative treatment of pancreatic necrosis
Pancreatic necrosis is very difficult to treat and this must be done in an intensive care unit under the strict guidance of specialists.
Treatment of pancreatic necrosis in a hospital
With this pathological process, the entire body suffers, since the products of tissue breakdown are absorbed into the blood, and accordingly, symptoms of intoxication appear. First of all, it is necessary to carry out detoxification therapy using intravenous administration of glucose-salt solutions.
In addition, an essential stage of treatment is antisecretory therapy - the introduction of drugs that help reduce the production of pancreatic enzymes.
An important role is played by the prescription of broad-spectrum antibacterial drugs, preferably two different groups, to prevent infection and to reduce existing symptoms. Complex therapy for such a serious disease as pancreatic necrosis gives good results in the initial stages of the disease.
Stages of development of necrotizing pancreatitis
Pancreatic necrosis has three stages of development, in which untimely detection of pathology can significantly harm the human body and lead to death:
- The first stage of pancreatic necrosis. Toxins and harmful bacteria accumulate in the victim’s blood. There is a problem of identifying microbes in the blood, so the disease at this stage is difficult to determine.
- The second stage of pancreatic necrosis. Since the reason for the first stage has not yet been identified, this becomes the reason for delayed treatment and the occurrence of an abscess, which affects the pancreas and neighboring organs of the gastrointestinal tract.
- The third stage of pancreatic necrosis. Purulent inflammatory processes develop in the pancreas and peritoneum, and this leads to death.
In case of pancreatic necrosis, only timely and correct diagnosis of the pancreas will create conditions for urgent surgery and give a chance to avoid death.
Surgical methods of treatment
Unfortunately, it often happens that medications alone are not enough and you have to resort to surgical treatment. Indications for it are extensive necrosis of the gland with the appearance of many purulent streaks in the abdominal cavity. Surgery for destruction of the pancreas is quite traumatic. A wide dissection of the tissues of the anterior abdominal wall is performed, after which the surgeon removes the sloughing necrosis and sequestra of the pancreas, and all pockets and leaks are opened. After this manipulation, external drainage of the abdominal cavity is performed using polymer tubes and gauze swabs. The surgical area remains accessible for inspection, dressings and rinsing.
Acute pancreatitis - diet
Since it is the food factor that very often becomes the cause of acute pancreatitis, it is of great importance in the treatment process. As mentioned above, in the first days after acute pancreatitis was diagnosed, the diet is very strict - complete fasting is observed. In severe cases, parenteral administration of nutrients may continue for several weeks.
In the future, nutrition for pancreatic necrosis of the pancreas implies a gentle regimen, which is ensured by the maximum exclusion from the diet of fats and carbohydrates, as well as foods that cause increased gas formation. The food is steamed and thoroughly chopped. Taken in small portions five to six times a day. The use of extractives and salt is completely excluded. Such a diet, depending on the severity of the disease, should last from several months to a year.
Of course, with such a serious disease as pancreatic necrosis of the pancreas, death is possible, and, of course, it is better not to bring your body to an attack, eliminating risk factors as much as possible. But if the disease does develop, then careful adherence to the diet will help to avoid relapses in the future.
Forecast
In conclusion I would like to say. That pancreatic necrosis is a very serious disease. If the patient remains alive, it is already a miracle. Accordingly, the quality of life is significantly reduced. It is necessary to maintain a constant diet, the slightest deviation from which causes pain and dyspeptic disorders.
After surgery, non-healing fistulas may remain, requiring constant care and dressings. The patient’s life becomes inextricably linked with the constant use of drugs that replace pancreatic function. And of course, we should not forget about the possibility of developing such a serious complication as diabetes, the symptoms of which are well known to all people.
Symptoms of pathology
The first and main warning sign of pancreatic necrosis is acute pain in the left hypochondrium. Therefore, it is necessary to understand what pain symptoms the human pancreas gives:
- pain radiates to the back;
- creates deceptive pain in the heart muscle;
- shoulder pain.
All these symptoms indicate a problem in the gland, and the pain effects are dulled when lying in a ball, tucking the knees to the chest, which only confirms the diagnosis. In addition to the listed symptoms, frequent vomiting may also occur, after which there is no relief, which leads to dehydration.
In the bloodstream of the affected person, or rather in his plasma, there is a high concentration of vasoactive components, which leads to redness of areas of the skin and face. With serious consequences, the opposite will occur: severe pallor of the skin.
purple spots on belly button
At the moment of pancreatic necrosis of the gland, the concentration of elastase increases greatly in the affected organism. With its strong increase, human blood vessels are destroyed, which leads to bleeding in the gastrointestinal tract. During this period, blood clots are observed during vomiting. You can also see physical changes - purple spots on the navel and buttocks of the person affected by the disease.
Pancreatic necrosis carries symptoms and complications, as well as consequences that require urgent surgery, which will give the sick person a chance to survive.
Mechanism of disease development
If an alcoholic overeating provokes an increase in the exocrine function of the gland, the following occurs:
- increased pressure inside the pancreatic duct,
- violation of the outflow of bile,
- overdistension of the bile ducts,
- stimulation of enzyme synthesis.
As a result of these interrelated processes, the enzyme outflow from the gland is disrupted - self-digestion of its tissues with its own enzymes (trypsin, chymotrypsin, lipase, elastase) begins. They are activated not in the duodenal bulb, as this should happen normally, but in the pancreas itself, disrupt the walls of blood vessels, and enter the blood. An initial vascular spasm occurs, which is replaced by a sharp expansion of their lumen and a slowdown in blood flow. Formed elements of blood, fluid, as well as biologically active substances (serotonin) are released into the tissue, causing severe swelling of the pancreas. This is the pathogenesis of acute pancreatitis.
Due to microscopic ruptures of the vascular membranes, hemorrhage occurs in the gland tissue and fatty tissue - areas of hemorrhagic necrosis appear.
Due to impaired microcirculation, increased thrombus formation occurs, cell death in these areas, and the release of intracellular lipase, which destroys adipose tissue. Foci of fat necrosis form.
Stages of development of pancreatic necrosis
The first 4–7 days the disease proceeds as aseptic necrosis. This phase takes place without the participation of pathogenic microorganisms.
If a pathological microflora joins, the process goes beyond the pancreas: the omentum, fiber, nearby organs and structures are involved. Various complications (abscess) occur.
As the infection spreads throughout the body, due to the large number of breakdown products, the following occurs:
- systemic inflammation,
- disruption or cessation of the functioning of organs and systems.
Shock develops (septic or pancreatogenic enzymatic) and death.
Mortality in sterile pancreatic necrosis is 10% of all cases of the disease; in case of infection of areas of necrosis, it increases to 30% or more.