Causes of gastritis in children
Gastric juice contains a colossal concentration of hydrochloric acid. Many people know how easily acid destroys various materials, especially living tissue. In a normal body without signs of stomach diseases, there are a number of blockers that do not allow acid to act, these are mucus in the stomach and immunity. The pathological factors of the body's defense are reduced significantly, thus, the acid begins to actively destroy the gastric mucosa, thereby developing gastritis; if you do not intervene in the process and do not begin treatment, then an ulcer is subsequently diagnosed.
Experts say that gastritis can be a hereditary disease if one of the child’s relatives suffers or has suffered from this disease. But usually this happens due to parents’ inattention to their child’s nutrition. This is a violation of the baby’s diet, frequent consumption of dry foods, rare but dense meals and a large amount of unhealthy food that irritates the stomach. These include all types of mayonnaise, chips, various ketchups and quick lunches.
Diagnostics
Diagnosis of the disease is carried out as follows:
- general and detailed blood test;
- stool test (to determine the presence of blood);
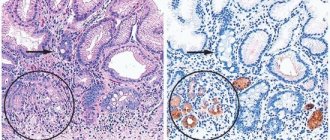
- fibrogastroduodenoscopy;
- histological analysis (determines the degree of damage to injured tissues).
Fibrogastroduodenoscopy is performed with a special flexible tube device with a microscopic video camera installed at its end. The probe helps to examine the condition of organ tissue and allows you to take samples for further microbiological research.
This procedure provides an accurate diagnosis of the type of pathological process and allows one to identify characteristic lesions: an increase in the amount of mucus in the folds, multiple small erosions, the presence of granular, papillary-like accumulations.
Gastritis: symptoms in children
The first warning sign is the child's complaints of abdominal pain. The intensity of the pain can vary, ranging from acute unbearable (to the point of tears) to mild constant pain. Sharp pain in the ribs. The onset of pain usually occurs early in the morning before the baby has had breakfast, or an hour after breakfast.
The doctors drew up a diagram of the onset of pain: hunger, pain, sharp pain - food - some relief, pain subsides and again hunger - pain. For gastritis, eating small amounts of food reduces pain levels. If we talk about what increases pain, it is fatty and spicy foods. Gastritis also expresses itself clearly during active sports. In addition to the symptoms described above, gastritis can manifest itself with vomiting and nausea, frequent belching, heartburn and, of course, indigestion. The active phase of gastritis is expressed in frequent increases in body temperature, sometimes up to critical numbers of 39-40 degrees.
Exacerbation of gastritis
An acute attack of gastritis manifests itself as severe pain on an empty stomach and vomiting after eating. Vomiting does not bring relief, the pain intensifies after it. The child’s condition worsens – dizziness and fatigue occur. The skin becomes pale, it is difficult for the baby to study, which is associated with an additional stress factor that worsens the condition.
Without treatment, complications of gastritis arise - the formation of ulcers, the spread of inflammation to neighboring organs - duodenitis , enteritis. For complications to form, several exacerbations or one severe inflammation must occur.
Acute gastritis in children
In children, acute gastritis develops for a variety of reasons, usually accompanied by an active inflammatory process and, importantly, degenerative rapid changes in the tissues of the stomach. Experts distinguish this type of disease as both primary and secondary (which develops as a pathology). Factors such as overeating, poor diet, hot food, large amounts of spicy foods, long-term use of various antibiotics, as well as damage to the walls of the stomach (quite often damage occurs from exposure to chemicals). Lead to the rapid development of acute gastritis.
Reasons for development
It is impossible to determine the exact causes of the disease. Today, most gastroenterologists believe that the disease develops against the background of individual intolerance to gluten, which is part of most bread and other baked goods, and cereal products.
In people suffering from lymphofollicular gastritis, the body's defenses attack this protein (gluten), considering it a health threat. Having dealt with gluten, immune cells are mistaken for the tissues of the digestive tract.
Doctors are convinced that Helicobacter pylori, which causes various pathological processes in the gastrointestinal tract, also makes its destructive contribution. Her favorite organs are the stomach and duodenum. With lymphocytic gastritis, lesions characteristic of this pathogenic bacterium are found in the tissues of these organs, and its presence is confirmed by the results of laboratory tests.
Doctors believe that people who abuse sweet soda, alcoholic beverages, and “junk” foods (chips, crackers, sandwiches) are at risk and can develop this type of gastritis. The list of potential victims also includes fans of fatty, spicy, fried and smoked foods.
In addition to lymphocytic, there is also plasmacytic gastritis, and also of unclear etiology. This form is characterized by the accumulation of a large number of leukocytes in the organs of the digestive tract. The symptoms of the disease are similar to typical manifestations of chronic inflammation of the inner lining of the stomach. Without a thorough medical examination and laboratory test results, pathology cannot be diagnosed.
Chronic gastritis in children - clinical recommendations
Chronic gastritis differs from acute gastritis in some ways. The first is the mechanism of occurrence of the disease, the second is the duration of the disease. Chronic gastritis, as its name suggests, is a rather long process, with mild symptoms of the disease. It is worth noting that the symptoms are weak until gastritis enters its full stage, then it begins to manifest itself sharply and cause pain. During an exacerbation of gastritis, gastric juice begins to devour the gastric mucosa, hence the pain.
The first signs of chronic gastritis in a baby are rare pain in the stomach; parents usually immediately give a pill, but this should not be done since any chemical component can only intensify the development of the disease. It is worth visiting a specialist and conducting a series of studies, and only after the tests have been carried out, take the recommended medications. Also, chronic gastritis often manifests itself in the form of belching and heartburn, sometimes belching and heartburn occur against the background of nausea. Well, the general condition of the baby: he becomes weak, inactive and spends a lot of time in a lying or sitting position.
Sydney classification
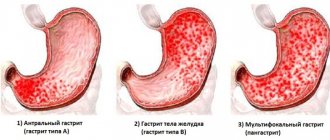
The second classification of gastritis was adopted in Sydney in 1990. Systematization was carried out according to the following criteria: volume of the lesion, rate of clinical development, morphological structure of the defect and origin:
| Criterion | Description |
| Speed of development of the clinic | Gastritis is divided into main forms depending on the severity of symptoms and clinical picture. Pathology is classified into acute, chronic and other (special) forms |
| Volume of lesion | Gastropathology is divided according to the anatomical part of the stomach in which the lesion develops: in the body of the organ, the antrum, or the entire inner surface of the stomach is affected (pangastritis) |
| Morphology of defects | Morphological changes in gastritis include atrophy and metaplasia. The degree of the inflammatory process is described. If the superficial form produces exudate, it is an exudative form. When there is no exudate, only hyperemia is noted - an erythematous type of pathology. Forms of erosion (flat or raised), tissue hyperplasia, hemorrhage or reflux are also described. All these manifestations can be visualized using endoscopic examination. |
| Etiology | Gastritis is systematized according to the reasons for its development:
|
The Sydney classification has the advantage of a visual analog scale expressing the degree of morphological and histological changes in mucous tissues. Features are assessed using points:
- 0 – no changes occurred;
- 1 – minimal changes;
- 2 – moderate changes;
- 3 – significantly pronounced changes.
Nutrition for gastritis in children
Treatment of gastritis is, first of all, dietary and proper nutrition:
- The general rule for patients with gastritis is to eat 5 times a day and in small portions.
- The last meal should be approximately 4 hours before bedtime.
- Before going to bed, it is recommended to drink a glass of low-fat kefir or fermented baked milk.
- It is strictly forbidden to eat dry foods, those that can injure an inflamed stomach, no crackers, chips or other harmful things.
- Each meal should last at least 25 minutes, this is necessary so that the baby chews the food as thoroughly as possible.
- Salt should be kept to a minimum. For a child under 3 years of age, no more than 5 grams per day, from 3 to 8 years, no more than 8 grams per day.
What foods should be excluded from your child’s menu:
- Meat broths of all types (except chicken broth).
- Smoked meats, fried potatoes and fried fish, salted foods including various pickles and marinades.
- White cabbage, including soup made from it.
- Carbonated drinks with the exception of still mineral water.
- Persimmon, lemon, orange.
- Fresh milk is also not recommended during a diet for gastritis, but porridge with milk is recommended.
Secondary prevention
The goal of secondary prevention of chronic hepatitis is to reduce the frequency of relapses and prevent the progression of the disease and the development of ulcerative lesions and gastric cancer. The secondary prevention program includes:
- I. Active identification of patients with clinically pronounced forms of chronic hepatitis, frequent exacerbations and their adequate non-drug and drug therapy. The regimen of drug therapy for hCG is presented in Table No. 36.
245 Treatment regimen for chronic gastritis
With low acidity
| With increased acidity | |
| 1. Replacement therapy (acedin-pepsin, pepsidil, hydrochloric acid, gastric juice) | 1 . Secretolytics - H2-histamine blockers: cimetidine, ranitidine, famotidine (quamatel), - Proton pump inhibitors (PPIs): omeprazole (gastrozol, Losek, Omez, Romesec), lansoprazole (Lanzap), pantoprazole, rabeprazole (Pariet ), esomeprazole (Nexium) - Anticholinergics: metacin, gastrocepin, buscopan |
| 2. Stimulation of secretion (aminophylline, nicotinic acid, limontar, calcium gluconate) | 2. Antacids - Non-absorbable: aluminum, magnesium hydroxide - Maalox, Almagel - Adsorbent: vikalin, vikair, ventrisol - Absorbable (soluble): soda, burnt magnesia - not currently used |
| 3. Improving microcirculation (chimes, prodectin) | 3. Gastroprotectors - Enveloping and astringent (film-forming): bismuth salts (de-nol), aluminum (sucral-fat), alginic acid, herbal medicines (chamomile, flax seed, plantain, mint, yarrow, St. John's wort) - Synthetic analogues of prostaglandin E1: misoprostol |
| 4. Symptomatic (antispasmodics, prokinetics (motilium, ganaton), herbs, multivitamins) | 4. Antibiotics in case of AR detection (tetracyclines, macrolides, nitrofurans, penicillins) |
When a Helicobacter pylori infection is detected, its eradication is necessary, which is the most important factor in preventing the development of stomach cancer.
According to international recommendations, there is first-line therapy, including PPI + 2 antibiotics for 7 or 14 days:
Omez 20 mg 2 times a day + Klacid 500 mg 2 times a day + amoxicillin 1000 mg 2 times a day.
If ineffective, second-line therapy (quadritherapy) is used, including PPI + bismuth salts + 2 antibiotics.
De-nol 240 mg 2 times a day + tetracycline 500 mg 4 times a day + metronidazole 500 mg 3 times a day.
When prescribing treatment, it is advisable to use drugs that normalize the species composition of the intestinal microflora, in particular probiotics (Linex, BionZ), prebiotics (Normase), and lactic acid products.
- I. Active identification of persons with latent forms of hCG and conducting dispensary observation of them with a set of differentiated treatment and preventive measures.
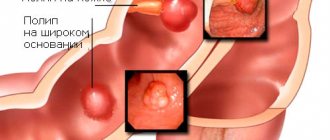
- II. Active dynamic monitoring of patents with precancerous forms of chronic gastritis is important: fundic gastritis type A with a pronounced decrease in secretory function; gastritis with intestinal epithelial metaplasia;
III. Atrophic-hyperplastic gastritis; gastritis with Addison-Birmer anemia; Ménétrier's disease; polypous gastritis. These patients are subject to annual endoscopy with biopsy and complete eradication of HP.
- IV. Clinical observation of patients with chronic hepatitis and systematic anti-relapse treatment. The dispensary observation scheme for patients with chronic hepatitis is presented in Table No. 37.
Scheme of clinical observation of patients with chronic hepatitis
| Frequency of therapist observations | Examination by other specialists | Name and frequency of diagnostic tests | Basic therapeutic and recreational activities |
| 2 times per year | Dentist, oncologist - according to indications | 1-2 times a year class. an. blood, vol. an. urine, coprogram, Gregersen's reaction, FGDS with biopsy, X-ray of the stomach, according to quantification - fractional duodenal intubation. | Diet. Mode. Drug treatment. Anti-relapse treatment - according to indications. Spa treatment. |
Prevention of exacerbation of chronic hepatitis involves anti-relapse treatment, including agents that normalize the functional and morphological state of the gastrointestinal tract.
- Of utmost importance in preventing the development of relapse of the disease is adherence to a diet that provides functional, mechanical, thermal and chemical sparing of the organ. Fractional 5-6 meals a day are indicated. Avoid foods and dishes that have a strong irritant effect on the mucous membrane (pickles, smoked meats, marinades, hot seasonings, fried meat, fish). It is recommended to limit the consumption of salt, strong tea and coffee, and exclude alcoholic and carbonated drinks.
- It is necessary to carry out measures aimed at eliminating risk factors that can cause exacerbation and progression of chronic hepatitis: giving up bad habits, rational employment (switching to work without night shifts, frequent business trips, excessive physical and mental stress), avoiding taking medications that damage the mucous membrane the lining of the stomach, harmful production factors, treatment of other diseases of the digestive system, endocrine system, kidneys, contributing to the development and aggravation of the course of chronic hepatitis.
- Drug treatment. For type A gastritis in the presence of secretory insufficiency, replacement therapy (acidin-pepsin, pepsidil) during or immediately after meals is indicated. To stimulate the secretory function of the stomach, aminophylline, calcium preparations, acids, limontar, which is a mixture of succinic and citric acids, and calcium are recommended. Take on an empty stomach, after dissolving the tablet in water, 2-3 times a day.
Multivitamin preparations are prescribed - in a course of 1-2 months, which improves the course of metabolic processes in the gastric mucosa and helps to increase the functional activity of its glands. Trophic processes in the gastroduodenal mucosa are improved by nicotinic acid preparations, trental, prodectin, and cinnarizine. In case of severe secretory deficiency, replacement therapy with multienzyme drugs (Creon, Mezim Forte, pancitrate) is carried out. In case of severe disorders of protein metabolism, anabolic steroids (retabolil, silabolin, nerobol) are prescribed.
In the presence of spastic phenomena, myotropic antispasmodics (debridet, dicetel) are used to relieve them. In the presence of duodenogastric reflux, prokinetics are prescribed (Motilium 10 mg 3 times a day 30 minutes before meals and 1 time at night), omez D.
If HP is detected, eradication therapy is carried out (see above).
- Treatment with mineral waters. For chronic hepatitis, it is recommended to drink mineral waters: with preserved and increased secretion, use non-carbonated mineral waters of low and medium mineralization, mainly alkaline: “Borjomi”, “Smirnovskaya”, “Slavyanovskaya”, which are used warm (37-38 degrees) at 3 / 4 glasses 3 times a day 1 hour before meals for 21-24 days.
For reduced secretion, use “Narzan”, “Arzni”, Essentuki” No. 4, No. 17. Water is taken 15-20 minutes before meals in a less warm form (30 degrees), in small sips of 1/4-1/2 cup 2 -3 times a day.
- Herbal medicine is widely used for all types of hCG. For low acidity, plantain leaves, mint, St. John's wort, wormwood, yarrow, calendula, thyme are recommended, which have an anti-inflammatory effect and have the ability to stimulate the secretory function of the stomach. For the treatment of Helicobacter pylori with normal or high acidity, herbs with anti-inflammatory, enveloping, astringent, and adsorbing effects are used: chamomile, St. John's wort, mint, flax seed, oat seed, yarrow, cinquefoil, knotweed, fresh pink potato juice 1/4-1 /2 glasses 3 times a day before meals for 3-4 weeks.
- Normalizes the motor and secretory function of the stomach, improves blood supply to the mucous membrane; physiotherapeutic treatment: hyperbaric oxygenation, inductothermy to the epigastric region, sinusoidal modulated currents, decimeter waves, diadynamic Bernard currents. For Helicobacter gastritis with preserved and increased acidity, thermal procedures on the epigastric region (therapeutic mud applications) are effective. Physiotherapy is carried out only after the exacerbation of the disease has stopped.
- Sanatorium-resort treatment is carried out in the remission phase. The main therapeutic factors in sanatoriums are nutritional therapy, herbal medicine, mineral water intake, physiotherapy, exercise therapy, psychotherapy and climatotherapy. The resorts of Druskininkai, Essentuki, Izhevsk Mineral Waters, Staraya Russa, and Jurmala are recommended.
alexmed.info
Treatment of gastritis in children
Only a doctor can prescribe the correct treatment. And it’s worth saying right away that self-treatment of a child can lead to a general deterioration in the baby’s well-being. Before starting treatment for gastritis, you should consult a specialist. As a rule, the first thing treatment begins with is complete lavage of the baby’s stomach; this is done by affecting the stomach, inducing vomiting. And only after that the treatment begins.
If we talk about the medicinal method of treatment, then a complex of tablets is prescribed, which are taken in pairs, such as regular activated carbon with sorbex. For acute pain, an anesthetic is prescribed, but if we are talking about a child, nothing other than no-shpa is prescribed. And as already mentioned, all this while the child is on a diet, since even taking the medicine but not following the diet, there will be no effect.
Symptoms of pathology
The clinical picture of the disease may include discomfort in the epigastric zone, a feeling of fullness and heaviness in the stomach. Dyspeptic symptoms are often observed: heartburn, sour belching, nausea, vomiting, stool instability: diarrhea alternates with constipation. The pathognomonic symptom of chronic gastroduodenitis is considered to be an unpleasant odor from the oral cavity, a yellowish-brown coating on the tongue, and teeth marks on the lateral surfaces of the tongue. Autonomic disorders are present: increased sweating, pallor, irritability, fatigue, sleep disturbances.
For chronic gastroduodenitis, alternation of an acute period and a period of remission is typical. During the period of exacerbation, the symptoms are pronounced; the period itself can last up to 2 months. In case of incomplete remission, there are no complaints in the presence of morphological and endoscopic pictures of the disease.
For the ulcerative form of the pathology, vomiting with blood is typical, this indicates the presence of internal bleeding. This condition requires immediate hospitalization, as the ulcer may perforate, which can lead to peritonitis. Dizziness may occur, and some patients may faint.
Prevention of gastritis in children
Prevention of gastritis is very important, since this disease has the property of transformation, which leads to major health problems in the future.
- Prevention of inflammation of the mucous membrane consists, first of all, in a properly balanced diet.
- The child's menu must be appropriate for his age and include recommended foods.
- Visit your doctor every year to have your baby's stomach checked, even if there is no apparent reason. A control examination can detect the disease at a very early stage, which will allow it to be dealt with quickly and effectively.
Do not neglect the advice, if your child periodically complains that his stomach or stomach hurts, visit a doctor immediately.
What symptoms indicate pathology?
A nonspecific form of dangerous pathology may not manifest itself in any way, and the sick person will not even know about the stomach problem.
Symptoms of the initial stage of lymphocytic gastritis can be manifested by the following sensations:
- Pain in the stomach area;
- The appearance of belching or heartburn;
- Nausea accompanied by vomiting;
- Bloating, flatulence;
- Constipation or diarrhea.
With a prolonged course of the disease, the pain syndrome manifests itself as cutting or cramping pain. A person loses appetite and weight, signs of iron deficiency anemia develop, and there is a risk of gastric bleeding.
If the symptoms of lymphocytic gastritis develop with increased secretion of gastric juice, the patient’s tongue becomes covered with a white coating.
In the case of gastritis that develops with low acidity, the tongue remains dry, but the patient complains of rumbling in the stomach with its distension. A likely sign is severe vomiting with blood fragments and a sour smell. With a reduced level of acid secretion, no weight loss or appetite occurs.
Treatment of chronic gastroduodenitis
Considering the high risk of detecting Helicobacter pylori infection, eradication of the pathogen is carried out according to a scheme that is prescribed based on the severity of the pathology:
- "Metronidazole", a bismuth preparation, a tetracycline antibiotic - for several weeks;
- "Omeprazole", "Clarithromycin", "Metronidazole" - within a week;
- “Amoxicillin”, “Ranitidine”, “Metronidazole” - for one and a half to two weeks.
For increased acidity, proton pump inhibitors are used - Lansoprazole, Omeprazole, Rabeprazole, Esomeprazole, H2-histamine receptor blockers - Ranitidine, Cimetidine, Famotidine, antacids - Maalox, Phosphalugel ", "Almagel", gastroprotectors - sucralfate. For vomiting and flatulence, prokinetics are used - Motilium, Cerucal.
In the treatment of the pathology of chronic gastroduodenitis, great importance is attached to balneological and sanatorium-resort treatment, moderate physical activity, physiotherapeutic procedures, and exercise therapy.