Chronic atrophic gastritis
Chronic atrophic gastritis is an independent disease, and not a transformation of acute gastritis. This condition is sometimes called inactive gastritis or gastritis in remission. It is characterized by long-term, progressive atrophy of glandular tissue cells, the predominance of dystrophic processes over inflammatory ones.
Chronic atrophic gastritis is sometimes called inactive gastritis or gastritis in remission
Pathogenesis leads to changes in secretory, motor and absorption functions. In the chronic form of atrophic gastritis, the pathogenesis involves organs anatomically associated with the stomach: duodenum, esophagus, as well as organs functionally associated with the stomach: liver, pancreas, endocrine glands. Due to general intoxication of the body, the process of hematopoiesis and the nervous system are involved in pathogenesis.
Pathogenesis, as a rule, develops against the background of low acidity of gastric juice. Clinical symptoms correspond to gastritis with low acidity. The diagnosis of acute and chronic gastritis is made on the basis of differential diagnostic data. The examination is carried out using instrumental, functional and laboratory methods. Of particular value are endoscopy and its varieties, pH-metry, histological methods for examining biopsy specimens, and laboratory blood testing - gastropanel.
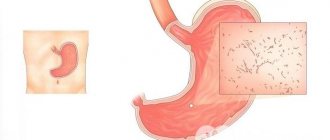
Signs of chronic atrophic gastritis:
- normal or thinned organ wall;
- smoothed mucous membrane;
- wide gastric dimples;
- flattening of the epithelium;
- low secretory activity of the glands;
- moderate infiltration of leukocytes outside the vessels;
- degeneration (vacuolization) of gland cells.
Diagnostics
The examination is comprehensive and includes a number of activities:
- examination of the digestive tract using an endoscope;
- cytological examination for the presence of Helicobacter pylori;
- analysis of stool, vomit, blood;
- breath test.
Diagnosis is carried out to identify the cause of the disease and the degree of damage to the mucous membrane. If the symptoms are mild, instrumental methods are used: sounding, gastroscopy.
During an exacerbation, devices are not inserted into the esophagus. The diagnosis is made on the basis of ultrasound, x-ray or computed tomography.
Using probing, the secretory function of the stomach and the level of acidity are assessed.
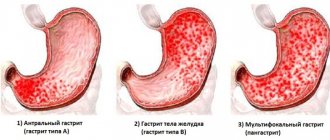
What is antral chronic gastritis
Antral gastritis is a chronic inflammatory lesion of the gastric mucosa, localized in the antrum (in the outlet section of the stomach). Approximately 95% of all cases of chronic antral gastritis are caused by the detection of the bacterium Helicobacter pylori in the gastric mucosa. This bacterium feels comfortable in gastric mucus with a pH of 4 to 6, however, even with increased acidity, the microorganism remains active.
A decrease in the acidity of gastric secretions is considered detrimental to bacteria. In an unfavorable environment, Helicobacter passes into the cyst stage, and when it gets into comfortable conditions, it becomes active again. Helicobacter bacteria produce certain enzymes that cause changes in the composition of mucus.
At the initial stage, inflammatory damage to the antrum of the stomach occurs as a non-atrophic process, not accompanied by insufficient secretion of gastric juice. The clinical course of antral gastritis is very similar to the course of ulcerative lesions of the gastric mucosa.
Such patients experience the appearance of hunger pain in the epigastric region or pain that occurs some time after eating; they may also experience heartburn, belching of sour or air, and constipation. With this disease, there is no loss of appetite.
Approximately 95% of all cases of chronic antral gastritis are caused by the detection of the bacterium Helicobacter pylori in the gastric mucosa
If antral gastritis is suspected, the patient is prescribed gastrography with contrast, during which thickening of the relief folds in the pyloric region, pyloric spasm, segmented peristalsis, and disordered evacuation of gastric contents are revealed.
Therapy for antral chronic gastritis begins with the appointment of a special therapeutic diet, characterized by the exclusion of fatty, spicy, fried, salty and rough foods from the patient’s menu. To eliminate the pathogen, the patient is prescribed anti-Helicobacter drugs. Etiotropic therapy for this bacterium is quite complex, this is due to the fact that the microorganism quickly adapts to antibiotics.
In most cases, a combined antibacterial treatment regimen is used, consisting of two or three antibacterial drugs. Also, such patients receive proton pump inhibitors, which suppress the activity of Helicobacter. An important component of the treatment regimen is the administration of reparative agents to patients that stimulate protein synthesis.
Features of the clinical picture
Clinically, superficial antral gastritis is a disease that is very similar to peptic ulcer disease. When the doctor palpates the abdomen in the epigastrium (just below the solar plexus), some pain is noted. Patients do not notice a decrease in appetite, as with other diseases of the gastrointestinal tract.
Symptoms of the disease:
- a few hours after eating, pain occurs in the epigastrium;
- heartburn;
- belching air with a sour smell;
- there is a tendency to constipation.
Chronic antral gastritis symptoms treatment
According to the modern classification, chronic antral gastritis is called “non-atrophic”. Also in the literature you can find other names for this stomach disease - gastritis with increased secretory activity, superficial, type B gastritis.
Antral gastritis is inflammation of the gastric mucosa in its lower section near the transition to the duodenum.
Antral gastritis is an inflammation of the gastric mucosa in its lower section, near the transition to the duodenum. In this case, the damage is superficial. Therefore, endoscopic examination of the stomach (FGDS) usually reveals catarrhal forms without erosions, hemorrhages and ulcers. There is a special type of this pathology associated with the reflux of the contents of the duodenum into the stomach (duodeno-gastric reflux).
Among all forms of inflammatory diseases of the stomach, chronic antral gastritis accounts for more than 75% of cases and occurs in almost half of the adult population. According to ICD-10, the disease has code K29.3. Gastritis of the antrum is characterized by a long course, while atrophic forms of the disease do not develop, but concomitant duodenitis is possible. The lesion is widespread; focal changes in the antrum are uncharacteristic.
Antral gastritis is accompanied by minor complaints or manifests itself in various variants of dyspepsia - digestive disorders:
- ulcer-like dyspepsia: dull pain in the upper abdomen, heartburn;
- dyskinetic variant of gastric dyspepsia: nausea, rapid satiety, bloating after eating.
As the pathology progresses, the pain syndrome intensifies. The pain becomes cramping, aching, sucking, and can bother you on an empty stomach and at night.
In order for the treatment of antral gastritis to be effective, it is necessary to undergo a course of therapy under the supervision of a therapist or gastroenterologist
It is accompanied by belching, a burning sensation in the chest, often reminiscent of an angina attack. When you feel (palpate) the abdomen, you can determine moderate pain in the upper abdominal cavity and its swelling. With a chronic course of the process, weight loss, sleep disturbances, and irritability are possible.
For treatment of antral gastritis to be effective, it is necessary to undergo a course of therapy under the supervision of a therapist or gastroenterologist. It begins after an examination, which usually includes an FGDS, a biopsy and a rapid urease test to detect Helicobacter pylori. Treatment includes a diet enriched with proteins.
Along with proper nutrition, patients with antral gastritis are prescribed:
- antibacterial agents in various combinations for a course of 10 or 14 days;
- drugs that reduce the intensity of gastric secretion;
- medications to reduce gastric acidity.
Chronic gastritis of the antrum
https://youtu.be/JI65t2BoWB4
The main, and in many cases the only, distinguishing feature of this form of gastritis is the atrophy of specialized cells in the deep layers of the gastric mucosa. In the lamina propria of the mucous membrane, a polymorphocellular infiltrate is determined, the qualitative and quantitative composition of which depends on the activity of the process and the severity of atrophy.
Depending on the activity of the process, almost all foreign authors propose to distinguish three variants of gastritis: active gastritis (exacerbation), inactive (remission) and gastric atrophy. According to the degree of severity, atrophy is classified into weak, moderate and severe. With mild atrophy of the stomach, the glands are only slightly shortened, framed by thin fibrous layers.
In the fundic glands there is moderate hyperplasia of accessory glandulocytes, the main parietal glandulocytes are mostly preserved, only some of them are replaced by mucoid ones. With severe atrophy, massive fields of sclerosis and a polymorphic cell infiltrate are visible in the place of the former glands.
The surviving glands are short, parietal and chief cells are completely replaced by mucus-forming cells. Moderate atrophy occupies an intermediate position, i.e., along with preserved fundic glands, there are glands represented only by accessory cells.
The nature of the damage to the fundic glands in atrophic gastritis (displacement of specialized main and parietal cells by accessory cells) implies that for atrophic gastritis, pyloric metaplasia of the body and fundus of the stomach is a prerequisite. This circumstance should be taken into account, since a biopsy of the true mucous membrane of the body of the stomach can be interpreted as originating from the antrum. The glands of the pyloric type identified in this case are usually called pseudopyloric.
Stages of the malignant process
Stomach cancer can have the following stages of development:
- 1A: T1, N0, M0.
- 1B: T1, N1, M0; T2, N0, M0.
- 2: T1, N2, M0; T2, N1, M0; T3, N0, M0.
- 3A: T2, N2, M0; T3, N1, M0; T4, N0, M0.
- 3B: T3, N2, M0.
- 4: T4, N1-3, M0; T 1-3, N3, M0; any T, any N, M1.
Read here: Liver cholangiocarcinoma: developmental features
T (tumor size):
- T1 – the tumor infiltrates the gastric wall to the submucosal layer;
- T2 – there is infiltration of cancer cells to the subserous layer. Possible involvement of the gastrointestinal, gastrohepatic ligament, greater or lesser omentum, but without penetration into the visceral layer;
- T3 – neoplasm that has spread to the serosa or visceral peritoneum;
- T4 – tumor growth into organs adjacent to the stomach.
N (metastases in regional lymph nodes):
- N0 – no metastases.
- N1 – metastases in 1-6 regional lymph nodes.
- N2 – regional nodes 7 to 15 are damaged.
- N3 – metastases in more than 15 lymph nodes.
M (distant metastases):
- M0 – no distant metastases.
- M1 – metastases in distant organs.
Atrophic gastritis of the antrum of the stomach
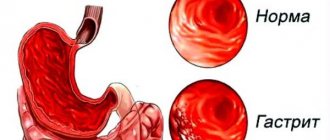
Atrophic gastritis is inflammation, thinning of the gastric mucosa, in which there is a disruption in the functioning of cells and atrophy of the excretory glands. As the disease progresses, these glands are replaced by connective tissue and cannot produce gastric juice, the main element of normal digestion.
One of the most dangerous consequences of the disease is stomach cancer, which develops when the symptoms of dying glands are ignored. The general clinical picture of the disease, atrophic gastritis, is almost no different from ordinary gastritis.
Gastric atrophy can occur without pronounced pain or external manifestations, and is practically unnoticeable for a long time, especially if the patient has other gastrointestinal diseases. Atrophic changes can be diagnosed using endoscopic examinations, analysis of antibodies in the blood, and x-rays.
Symptoms of atrophic gastritis are:
- aching pain in the abdomen, which intensifies after eating;
- sudden weight loss, dystrophy and anemia;
- thick white coating on the tongue;
- bloating, diarrhea, constipation, belching, nausea, upset stomach;
- bad breath;
- decreased appetite, weakness, dizziness.
Atrophic gastritis is an inflammation of the thinning of the gastric mucosa, in which there is a disruption in the functioning of cells and atrophy of the excretory glands. The
chronic form of the disease is a separate disease that is not associated with remission of the acute form. The disease has a negative impact on neighboring organs: liver, duodenum, pancreas, and affects the nervous and endocrine systems. Chronic atrophic gastritis is characterized by prolonged internal destruction of cells without severe inflammation, and develops due to a decrease in the acidity of gastric juice.
A sign of atrophic gastritis of the antral type is high levels of secretory function and partial oxidation of the body’s environment. Antral atrophic gastritis affects the antrum of the stomach (lower, adjacent to the duodenum), scarring and inflammation form.
Instrumental studies show deformation of the mucous membranes and decreased peristalsis activity. The walls of the esophagus narrow, and there is no healthy metabolism. In addition, focal atrophy of the mucous membrane of the antrum of the stomach provokes the appearance of ulcers and significant thickening of the walls as it progresses.
It is almost impossible to achieve regeneration, that is, complete restoration of damaged glands in the treatment of atrophic gastritis, but stopping the processes of death and regulating their development and spread in the stomach is quite possible. For complex therapy, medications are used: enzymes, vitamins, anti-inflammatory drugs, and sometimes hormonal and immunomodulatory drugs.
Physiotherapeutic methods and physical therapy have a good effect on the condition of a patient diagnosed with atrophic gastritis. Many herbs and foods can have a beneficial effect on the inner lining of the stomach, causing it to produce more of the necessary enzyme, reducing inflammation and pain. When treating atrophic gastritis with folk remedies, it is important to strictly follow the diet, monitor the course of the disease and adjust the list of medications together with your doctor.
Causes of the disease
Scientists have established the reasons that cause or predispose to the development of pathology:
- Exposure to the pathogenic bacterium Helicobacter pylori. Its role in the formation of any form of gastritis has been scientifically proven. This bacterium is a gram-negative rod that lives happily in the acidic environment of the organ. In the place where the bacillus has settled, the environment becomes alkalized, and the mucosal area becomes vulnerable to aggressive factors. At this point, the process of inflammation occurs.
- Poor diet. Here they celebrate the intake of junk food: fried, salted, smoked, spicy, sour, mechanically poorly processed. Harm is caused by quick, dry snacks, rare but plentiful meals, and overeating.
- Drinking large amounts of alcohol. Alcohols negatively affect the stomach's defenses.
- Smoking.
- Excessive intake of coffee drinks.
- Stable stressful and neurotic conditions.
- Poisoning with poisons, burns of the mucous membranes with acidic and alkaline chemicals.
- Poor environment, harmful working conditions.
- Systematic intake of medications: non-steroidal anti-inflammatory drugs, hormonal pharmacological substances, antibiotic therapy, chemotherapy, cytostatic drugs. Paracetamol has a negative effect on the stomach.
- Chronic concomitant diseases, diabetes mellitus, thyrotoxicosis, liver-renal failure, HIV infection.
- Autoimmune and immunodeficiency conditions.
- Hereditary predisposition.
Process stages:
- There are active or acute stages of the disease. It is characterized by a rapid course, development of the main clinic and symptoms. In this case, the patient will actively complain. All pathological changes with it are reversible.
- Chronic stage of the process. It is characterized by less pronounced symptoms and complaints, an increase in the area of pathology, and is not reversible. In this case, there are episodes of exacerbation.
Gastritis of the antrum treatment
A specialized physician will tell you how to properly treat inflammation of the antrum, and you should contact him as soon as the main symptoms of antral gastritis are noticed. Therapy for antral gastritis requires an integrated approach and includes taking medications, following a therapeutic diet and physiotherapy.
To treat antral gastritis, the patient is prescribed pharmaceutical drugs of the following groups:
- antibacterial medications;
- PPI;
- NSAIDs;
- antispasmodics;
- reparative medicines that restore the mucous membrane.
Therapy for antral gastritis requires an integrated approach and includes taking medications, following a therapeutic diet and physiotherapy.
In addition to medications, the patient may be prescribed physiotherapeutic procedures, namely: UHF, electrophoresis, ultrasound. At the end of the course, paraffin therapy and mud therapy procedures will be useful to normalize the condition.
If the mucous membrane of the antrum of the stomach is inflamed, the patient will need to adjust the menu. You need to give up sour, salty, fatty and hot foods, and include low-fat broths, cereals and dietary types of fish and meat in your diet.
To prevent the development of antral gastritis, it is necessary to try in every possible way to avoid infection with Helicobacter. To do this, you need to maintain personal hygiene, adhere to a diet, avoiding foods that irritate the gastric mucosa, as well as drinking alcoholic beverages and smoking. It is important to maintain your immunity at the highest level and avoid emotional shocks and physical stress.
Disease prevention
The development of hyperplastic, erythematous or other antral gastritis can only be prevented by maintaining a healthy lifestyle. Prevention closely borders on protection from provoking factors:
- you need to give up smoking and alcohol abuse;
- it is important to lead a measured lifestyle without unnecessary stress and worries;
- diet is a necessary condition for a healthy body;
- Medicines must be taken under the strict supervision of doctors.
There are no “safe” types of disease that do not need to be treated. Moreover, even the primary catarrhal stage already indicates serious changes in the body. But timely detection of antral gastritis in any form will help the patient quickly get rid of provoking factors. If a person makes every effort to recover (diet, daily routine, giving up bad habits, systematically taking medications and folk remedies), then the pathology will go into stable remission.
Where is the antrum (stomach) treated?
The Gastroenterology Department performs diagnostic, treatment, advisory, organizational and methodological work on the provision of specialized inpatient care to gastroenterological patients. Provides emergency care to patients with gastroenterological diseases.
The Gastroenterology Department carries out diagnostic, treatment, advisory, organizational and methodological work on the provision of specialized inpatient care to patients with gastritis
Conducts a complex of rehabilitation measures aimed at social and labor adaptation of gastroenterological patients. Introduces new advances in the provision of medical care for diseases of the digestive system into clinical practice and analyzes the effectiveness of their implementation. Prepares and conducts scientific and practical conferences and seminars aimed at introducing the results of scientific research into the practice of gastroenterological services.
The organization of the department's work is determined by the regulations on the gastroenterology department. Planned hospitalization in the department is carried out in the direction of gastroenterological offices, local therapists, and general practitioners of family medicine in the city. Patients with chronic diseases of the digestive system are referred to the department. Hospitalization for emergency indications is carried out at the direction of emergency medical teams and the doctor on duty. —
Sources:
- https://www.ayzdorov.ru/lechenie_gastrita_atroficheskii.php
- https://www.eurolab.ua/diseases/1641/
- https://sovets.net/10857-atroficheskij-gastrit.html
- https://www.obozrevatel.com/health/bolezni/antralnyij-gastrit.htm
- https://kratko-news.com/2017/12/07/simptomy-i-lechenie-antralnogo-gastrita/
- https://micrazim.by/ru/interesting/antralnyj-gastrit/
- https://fb.ru/article/178791/antralnyiy-otdel-jeludok-i-ego-zabolevaniya-gastrit-yazva-polip-i-erozii-antralnogo-otdela-simptomyi-i-lechenie
Post Views: 703