Biochemical analysis of stool examines the intestinal microflora for the presence of dysbacteriosis. Dysbacteriosis is not an independent disease, but it affects the body and requires treatment.
Biochemical analysis of stool for dysbacteriosis can inform about the general condition of the intestines with the predominance of certain types of microbacteria. In fact, the intestinal cavity is inhabited by several thousand species of bacteria that form the normal conditions of the microflora necessary for a high-quality digestion process. Failures in the quantitative indicator of microbacteria cause dysbacteriosis.
Dysbacteriosis does not carry the title of an independent disease, but based on the results of biochemical analysis, it is permissible to diagnose a specific disease in the human body.
Intestinal dysbiosis: what is it?
The human gastrointestinal tract (GIT) is inhabited by a group of bacteria that are of paramount importance for the healthy functioning of the entire body. It is intestinal microorganisms that work to synthesize vitamins and break down food. Gastrointestinal bacteria, in addition to the active distribution of nutrients, protect the cavity from the effects of pathogenic strains.
The coordinated activity of the body and intestines depends on the symbiosis of bacteria. Thus, disturbances in the quantitative and qualitative composition of the intestinal microflora cause a number of disorders that manifest themselves in the form of:
- flatulence;
- prolonged diarrhea;
- attacks of nausea;
- lack of nutrient supply to the tissues of the whole body.
The above manifestations represent a malfunction of the intestines - dysbiosis. Biochemical analysis of feces helps determine the quantitative and qualitative composition of the bacterial content of the gastrointestinal tract for the normal functioning of the body. In medical practice, to determine dysbiosis, three main diagnostic methods are used:
This research method is prescribed to a patient when visiting due to stool disorder (in acute or chronic manifestations), if there is unreasonable abdominal pain. If there is a sharp loss of weight, a coprogram is also prescribed.
The computer program method gives physical characteristics to the contents of the gastrointestinal tract, and is exclusively an auxiliary method for diagnosing a specific disease.
Don't want to get sick? Save the article on VKontakte
- Bacteriological examination of stool.
In laboratory conditions, a tank is inoculated with biomaterial on a nutrient medium, identifying and examining colonies of bacteria under a microscope.
- Biochemical analysis of feces.
The biochemical technique for examining stool gives quick and accurate results of the state of the gastrointestinal microflora, without delaying treatment for a long period.
Do you still think that healing your stomach and intestines is difficult?
Judging by the fact that you are now reading these lines, victory in the fight against diseases of the gastrointestinal tract is not yet on your side...
Have you already thought about surgery? This is understandable, because the stomach is a very important organ, and its proper functioning is the key to health and well-being. Frequent abdominal pain, heartburn, bloating, belching, nausea, bowel dysfunction... All these symptoms are familiar to you firsthand.
But perhaps it would be more correct to treat not the effect, but the cause? Here is the story of Galina Savina, about how she got rid of all these unpleasant symptoms... Read the article >>>
Dysbacteriosis is the result of pathological processes occurring in the body of a sick person. The disease not only does not have pronounced symptoms, but also does not have a special clinical picture. That is why identifying dysbiosis is not as simple as it might seem at first glance. A patient who has developed this disease to a greater or lesser extent experiences slight discomfort in the gastrointestinal tract, barely noticeable nausea and (in rare cases) an increase in temperature. Such symptoms can be associated with a disease of any organ. In some cases, dysbacteriosis proceeds completely unnoticed, and the only way to determine the presence or absence of the disease is to conduct competent and professional laboratory diagnostics.
Analysis of stool for dysbacteriosis can reveal the state of imbalance of the patient’s microflora even in the early stages of its occurrence. Today, in laboratory conditions, depending on the clinical picture and condition of the patient, medical staff can conduct two methods of stool analysis: bacteriological and biochemical. The most modern and popular, of course, is the biochemical method. Bacteriological analysis is perfect for primary or basic diagnosis. Having a number of significant drawbacks, this method of identifying dysbacteriosis is not only quite complex, but also inaccurate.
The essence of biochemical analysis of stool
Stool biochemistry for dysbacteriosis provides results a few hours after collecting the biomaterial. The essence of the process is to identify intestinal microorganisms in the full picture. When diagnosing, special attention is paid to the spectrum of fatty acids, since they are responsible for the synthesis of bacteria. In the medical industry, biochemical examination of stool for dysbacteriosis is also known as express diagnostics of microflora.
Not only specialists, but also patients prefer the biochemical method of examining dysbacteriosis for the following reasons:
- Tight research deadlines.
It is possible to obtain results of the state of intestinal microflora within a couple of hours after submitting the biomaterial to the laboratory.
- High sensitivity of the technique.
Diagnostics using the biochemical method reveals accurate results with specific determination of the concentration of compounds.
- Undemanding to samples of biological material.
Even yesterday’s collection of biomaterial is suitable for the method under consideration.
The human intestine is inhabited by
3 kg of bacteria. They represent the microflora necessary for normal digestion, but in the event of various malfunctions, the number of some microorganisms can noticeably decrease - dysbacteriosis will occur - an imbalance of bacteria.
Although doctors do not classify it as an independent disease, this does not reduce the harm. If intestinal dysbiosis is suspected, special stool tests are prescribed to establish an accurate diagnosis.
Indications for analysis
Human feces contain a large number of bacteria, and when examined in a laboratory, the activity of the entire digestive tract can be assessed. Microorganisms that form the intestinal flora perform many functions, participate in the digestion of food, ensure the absorption of nutrients and protection from the influence of pathogenic bacteria that enter the body along with water and food.
When there are disruptions in the hormonal system, antibiotic therapy, poor diet, or frequent stress, a person develops dysbiosis, which is characterized by an imbalance of microorganisms in the intestines.
This disease can be independent, but much more often it occurs against the background of other pathologies (inflammation in the digestive organs, disruptions in metabolic processes, immune disorders, etc.). Indications for examining stool for dysbacteriosis in adult patients and children:
- Diarrhea
- Constipation
- Pathologies of the digestive organs
- Painful sensations in the abdominal area
- Flatulence
- Rash on the skin
- Long-term therapy with antimicrobial drugs
- Long-term therapy with hormonal drugs
- Intestinal infections
- Foreign matter in excrement
- Allergies in a child
- Uncharacteristic foul or sour odor of feces
Stool analysis for dysbacteriosis, what is it?
Microorganisms living in the gastrointestinal tract are of paramount importance for human life. They synthesize vitamins, break down food and protect against attacks by pathogenic strains.
In other words, humans and bacteria are in symbiosis. But if the composition of the microflora is disturbed, flatulence, diarrhea, nausea may occur, not to mention the consequences of insufficient supply of nutritional compounds to the tissues.
The purpose of stool analysis is to determine the qualitative and quantitative composition of bacteria in the intestines.
For this purpose, 3 methods are usually used in medicine:
- Coprogram.
- Bacteriological analysis.
- Biochemical analysis.
Coprogram
A coprogram is prescribed when a person complains of chronic or acute stool disorder, abdominal pain of unknown origin, or sudden weight loss for no apparent reason.
Doctors also resort to such research when treating diseases not related to the gastrointestinal tract. This is especially true when treating pathologies in different parts of the body with antibiotics (throat, joints, etc.).
A coprogram is a primary examination, which is only an auxiliary method and gives a physical characteristic of the intestinal contents.
The analysis is carried out in 2 stages:
1. Macroscopic:
- stool color;
- form;
- quantity;
- smell;
- presence of parasites;
- the presence of pus, blood and mucus;
- leftover undigested food.
2. Microscopic:
- cells and tissue fragments;
- digested food (fiber, fat, salts, starch, etc.).
Bacteriological analysis of stool
If the coprogram shows deviations from the norm, the doctor has a reason to conduct a more thorough analysis. In the laboratory, stool is cultured on a nutrient medium.
After 4-5 days, the bacteria will multiply, which will allow their colonies to be examined under a microscope. After this, the specialist makes a conclusion about the number of microbes in 1 g of feces (CFU/g).
Based on the data obtained, the doctor makes a diagnosis. Test results for adults and children often differ, so the patient’s age must be taken into account.
But waiting 5 days for colonies to grow is not always permissible, because during this time a person’s condition can deteriorate significantly.
Biochemical analysis of stool
Biochemical analysis of stool for dysbacteriosis gives results on the day the samples are submitted. The essence of such research is to identify compounds present in the intestines.
Particular attention is paid to the spectrum of fatty acids, because they are synthesized by bacteria in the process of life. Biochemical analysis is also called rapid diagnostics.
The method is very informative and simple; it not only demonstrates the imbalance of microflora, but also establishes the section of the intestine in which the malfunction occurred.
Doctors much more often prefer this study due to its significant advantages:
- Speed. Results will be available in 1-2 hours.
- Sensitivity. The method very accurately determines the concentration of compounds.
- Undemanding to the freshness of samples. Even yesterday's poop will do.
Stool research methods
The scientific name for such medical manipulation is coprogram. It provides various ways to examine excrement. Fecal coprogram includes the following procedures:
- general analysis;
- biochemical research;
- bacteriological analysis;
- microbiological research.
General stool analysis
During such a survey, the main indicators of excrement are assessed. Stool examination includes the following aspects:
- Color of biological material
- in a healthy person, feces are colored brown. A change in shade can be caused by foods present in the diet. For example, blueberries give a brown color, and beets give a brownish-reddish color. In addition, there is a relationship between the color of feces and human pathologies. With cholelithiasis, the stool becomes whitish, and with cirrhosis of the liver, it becomes black. - Consistency of waste products
- normally the structure should be dense. If the stool is too dry, this indicates frequent constipation, accompanied by excessive absorption of water. An ointment-like consistency is a sign of an acute form of pancreatitis. The waste product has a liquid structure when intestinal motility is highly activated. A foamy mass is observed when there is excessive release of carbon dioxide. - Stool acidity
– normally this indicator should be neutral. Fluctuations in this value upward may indicate that foods rich in carbohydrates predominate in the diet. The value of the indicator is lower than normal more often when a person is on a protein diet. In addition, decreased acidity is a sign of pancreatic dysfunction, colitis and constipation. - The presence of mucus in biological material
- if a stool analysis shows the presence of this component, most likely the patient has polyps in the intestines. Also, the presence of this component indicates lactose intolerance, hemorrhoids or an intestinal infection.
In addition, a general stool analysis reveals parasites. More often, such a study identifies the following pests:
Bacteriological examination of stool
This analysis helps to identify all microorganisms living in the intestines. It contains a huge number of bacteria that take an active part in the digestion of food and the absorption of valuable substances. The following groups of microorganisms can live in the intestines:
- “Normal”
- these include lacto- and bifidobacteria, Escherichia. These microorganisms take part in the functioning of the digestive tract. - Conditionally pathogenic
are candida, enterococci, staphylococci. Under certain circumstances, for example, due to decreased immunity, these bacteria degenerate into pathogenic ones. They provoke the development of various diseases. - Pathogenic
– this group of microorganisms includes salmonella and shigella. Once ingested, they provoke the occurrence of serious infectious diseases.
For example, a stool test for Helicobacter provides complete information about the presence of this insidious microorganism. This parasite produces toxins that affect the mucous membrane of the duodenum and stomach. All this leads to the development of a serious inflammatory process and provokes ulcers, gastritis and other pathologies of the digestive system.
Microbiological examination of stool
This test determines the degree of digestion of food. In addition, stool can be examined for the intestinal group and for the presence of protozoa. During the procedure, the following elements are analyzed:
- Detritus is small particles.
They are a product of cell breakdown and food debris. The better the food is digested, the greater the specific gravity of detritus in the feces. - Muscle fibers - their quantity depends on the food consumed.
The presence of plenty of meat in the diet increases their content. - Connective fibers - these include the remains of cartilage tissue, ligaments and blood vessels.
Outwardly, they are similar to mucus. To distinguish the first from the second, a drop of acetic acid is added to the biological material during the study. Under its influence, the connective tissue swells and loses its structure.
At the same time, such a stool analysis is aimed at identifying the following indicators:
- starch;
- bilirubin;
- stercobilin;
- neutral fats;
- leukocytes;
- vegetable fiber
- fatty acids;
- ammonia.
Biochemical study of stool
This analysis is carried out to identify hidden bleeding in the digestive tract. In the future, these disorders can provoke the development of inflammatory, ulcerative and tumor processes. Such stool testing allows us to evaluate the following indicators:
- acidity of biological material;
- the presence of digestive enzymes, fats and proteins;
- mineral content and so on.
Preparing for a stool test
The reliability of the research results directly depends on proper preparation. The fact is that many food products contain substances that will give a positive reaction.
First of all, it's meat. It is in it that hemoglobin is present.
Secondly, it's iron. All red products contain this element. It is worth refraining from eating such foods for 3 days before the test, so that the laboratory does not accidentally get a false positive result.
Restrictions also apply to raw vegetables and fruits: during the preparation period you need to eat only thermally processed plant products.
In addition, the patient must stop taking medications that directly affect the intestinal microflora:
- antibiotics;
- probiotics;
- laxatives (official and popular);
- rectal suppositories.
Adults prepare for a stool test for dysbiosis on their own. Examining the contents of a child’s intestines is no different, but parents will have to monitor the child’s compliance with all recommendations.
Treatment of diseases caused by enterococci
After carrying out diagnostic procedures to study disturbances in the intestinal microflora, namely in the case of the presence of enterococci exceeding the norm, treatment with antibiotics will be relevant.
In order to determine which antibiotics the enterococcus strain is sensitive to, culture should be performed. With the help of aminoglycosides, mild infections are combated.
The intestinal microflora is restored by taking special therapeutic tablets and suppositories. Taking immunomodulators helps restore and strengthen the body's defenses.
Treatment of adults and older children
Some treatment options may include:
- use of the Parkes anti-parasitic device;
- treatment with ampicillin and vancomycin;
- the use of bacteriophage occurs due to the complete destruction of pathogenic bacteria by this drug. The course of treatment generally lasts 5-6 days, after which in most cases an improvement in the general condition is diagnosed;
- antibiotic therapy (for example, ampicillin) generally lasts for five days; if there is a positive trend, the course of treatment can last up to several weeks.
Treatment of infants
The treatment is due to the peculiarity of a small organism, in the treatment of which antibiotic therapy is absolutely not acceptable. An infant's immune system is not sufficiently developed, and in such a situation, taking antibiotics will significantly worsen the patient's condition. Read what baby feces look like, its norms and deviations here.
In such a situation, gentle treatment is used:
- using bacteriophages;
- the drug Creon 1000, which stabilizes the baby’s microflora;
- restoration of breastfeeding;
- long and regular walks in the fresh air.
In addition to therapy that reduces the number of pathogenic bacteria, you should remember the need to take vitamin complexes that are important for the body.
How to properly take a stool test for dysbacteriosis?
Diet and medication withdrawal are the primary conditions for the reliability of analysis results. In addition, the patient will need to collect stool in accordance with the rules.
Handing over feces - 6 rules:
- Before the control bowel movement, wash the perineum (the possibility of getting old samples is eliminated).
- The use of any auxiliary means to speed up the process of defecation (enema, laxative) is prohibited.
- Prepare a special container with a tight lid in advance (must be purchased at a pharmacy).
- Do not allow liquid to get into the stool (urine, water, etc.).
- Take 3 stool fragments (1 teaspoon each from different areas).
- If blood or mucus is present, such samples must be taken.
Gut bacteria are primarily anaerobic. 1 hour after defecation, they will still maintain their population in their natural form, but gradually the microorganisms will begin to die.
In order to correctly test stool for dysbacteriosis, it is necessary to deliver excrement samples to the laboratory at least within 2 hours after bowel movement.
Urgency is not so important for biochemical research, which studies not bacterial colonies, but the result of their vital activity - fatty acids. These compounds almost do not disintegrate spontaneously, and therefore remain unchanged for quite a long time.
Doctors even allow you to freeze stool and bring it in the next day. In the case of newborn children, this option is sometimes the most preferable for parents.
Interpretation of the results of stool analysis for dysbacteriosis
The intestines are home to 100 trillion bacteria, which is 10 times the number of all cells in the body. If there are no microbes at all, then the person will simply die.
On the other hand, a shift in balance in any direction leads to diseases. The interpretation of stool analysis for dysbiosis is to determine the number and types of microbes.
Table of interpretation of results and norms of analysis
Biochemical analysis of stool for dysbacteriosis is a method of studying intestinal microflora, intended to establish the level of biochemical indicators.
Biochemical analysis informs about the predominance of certain types of bacteria in the intestines (Escherichia coli, bifidobacteria, lactobacilli, fungi, etc.).
It is carried out by establishing the spectrum of fatty acids, which are a product of the vital activity of intestinal bacteria.
As is known, the human intestine is practically sterile only at the moment of birth. Already in the first hours of a baby’s life, this organ is populated by entire colonies of various bacteria. Most intestinal bacteria perform useful work: they help digest food and neutralize harmful toxins. But there are also representatives of bacterial microflora that can cause health problems - from bloating to appendicitis.
As a rule, the normal number of beneficial bacteria in the intestines of an adult is about 85% of their total number, and pathogenic microorganisms - 15%. If this balance is disturbed, a condition such as dysbiosis may occur.
Symptoms of intestinal dysbiosis are quite varied: they include flatulence, diarrhea, and many other disorders of the digestive tract. Dysbacteriosis, in turn, can itself be a symptom of a number of quite serious diseases, so doctors often prescribe a stool test for dysbiosis.
Is it necessary to treat dysbiosis in infants?
The condition in question is not a disease, and therefore does not require therapy. Progressive pediatricians do not even prescribe a stool test for dysbiosis in a child, considering it uninformative. While the baby is growing, the intestinal microflora is constantly changing, adapting to new food. It will finally be established in adulthood. Analysis of feces for dysbiosis in an infant makes sense only if there is a suspicion of an acute intestinal infection, but in such cases specific symptoms are present.
Deciphering the test for dysbacteriosis in infants allows the doctor to understand the state of the baby’s gastrointestinal tract. In children, this analysis is especially relevant in the sense that a baby, unlike an adult, is not able to say what is bothering him, and expresses it in his own way - by crying loudly. Therefore, when it becomes obvious that the baby is experiencing some kind of inconvenience associated with digestion, the doctor prescribes a test for dysbacteriosis for the baby.
Indications for use
A biochemical analysis of stool for dysbacteriosis can be prescribed in the following cases:
- unstable stool (constipation, diarrhea) for a long time;
- pain in the abdomen;
- constant flatulence;
- intolerance to a number of food products;
- skin rashes;
- food allergies;
- after prolonged (more than seven days) therapy with antibiotics, anti-inflammatory drugs or hormones;
- the presence of other gastroenterological diseases (cholecystitis, pancreatitis, intestinal diseases).
Causes of enterococci
The reasons for the appearance of enterococci in feces are often revealed through disruption of the intestinal microflora.
This may be caused by:
- Sufficiently long-term use of antibacterial drugs.
- Infection through skin and mucous lesions. This can most often be observed during manipulations in hospitals, when using insufficiently processed instruments.
- Hormonal imbalance in women.
- In pregnant women, as a result of constant quantitative changes in estrogens and androgens.
- Changes occurring through endocrine processes in the body.
How to prepare?
To ensure that the analysis results are as objective as possible, you should pay attention to the following requirements:
- three to four days before the test, stop taking any laxatives;
- the analysis is prescribed no earlier than 10-14 days after discontinuation of antibiotics (if they were previously prescribed);
- bowel movements should occur naturally, and not with the help of an enema;
- to collect stool, you should first purchase a special container with a tight lid from a pharmacy or medical facility;
- Drops of urine or discharge should not get into the stool (in women);
- the volume of material required for analysis is at least 10 ml;
- It is advisable to take material for research from different parts of the stool using special spoons supplied with the container. If mucus or blood that has entered it from the intestines is visible in the stool, they are also collected along with the bulk of the material;
- the sample must be delivered to the laboratory no later than three hours after its collection. If the material cannot be delivered within the specified time frame, then the sample can be frozen in a freezer and then delivered the next day.
Methods
There are three ways to test for dysbacteriosis:
- Coprogram;
- Bacteriological;
- Biochemical.
Will the coprogram show dysbiosis?
A coprogram is a microbiological analysis of intestinal microflora, used after long-term use of antibiotics not associated with diseases of the gastrointestinal tract. And it identifies pathology by the appearance of feces and determines the presence of:
- Fragments of undigested food;
- Starch;
- Helminths and their eggs;
- Fat;
- Blood and mucus.
Bacterioscopic examination is the first stage of microbiological analysis. The thick part of stool consists of 30% microorganisms. In this case, the intestinal flora is not microscopically distinguished using colored preparations. Bacterioscopically it is possible to isolate iodophilic flora and tuberculosis bacillus.
Bacteriological research - how much and how it is done
If the coprogram shows an imbalance, then the doctor prescribes a more accurate study. A bacteriological culture of feces is performed in a nutrient medium. In some cases, an analysis is performed for bacteriosis of the oral cavity. A scraping is taken from the oral mucosa, then a tank is performed. sowing. After 5-7 days, when the bacteria multiply, they are recounted. Based on the results of bacteriological examination of feces, the specialist gives an opinion. If organs other than the intestines are involved in the pathological process, a detailed analysis of blood and urine is performed.
Biochemical method
Stool biochemistry - this type of analysis gives results in 1 hour. The advantage of this method:
- Relative speed;
- Increasing the time for delivery of samples to the laboratory to 24 hours;
- You can freeze the sample in the refrigerator;
- Accuracy of the data obtained.
To obtain the correct result from a biochemical analysis, you must:
- Stop taking antibiotics 2 weeks before collection;
- For women, do not take tests until your period ends;
- Take samples from different parts of the stool.
Standard analysis values
When processing the results of biochemical analysis, the absolute content of acids (unit of measurement - mg/g) and their relative content (unit of measurement - unit) are determined.
Acceptable values of the studied indicators are:
Biochemical analysis of feces is a laboratory study based on determining the level of biochemical indicators, namely metabolites of volatile fatty acids (acetic, propionic, butyric) produced by microorganisms living in the gastrointestinal tract. With various pathologies of the stomach, small and large intestines, and liver, the microflora changes, and, accordingly, the biochemical parameters. By determining the spectrum of volatile fatty acids, one can judge the location and disease of the digestive tract. The method allows us to identify the cause of dysbiosis.
- Avoid taking laxatives, administering rectal suppositories, oils, limit (in consultation with your doctor) taking medications that affect intestinal motility (belladonna, pilocarpine, etc.) and drugs that affect the color of stool (iron, bismuth, barium sulfate), within 72 hours before stool collection.
At home
: it is possible for a mobile service employee to take biomaterial.
At the Diagnostic Center
: collection or independent collection of biomaterial is carried out at the Diagnostic Center.
On one's own
: collection of biomaterial is carried out by the patient himself (urine, feces, sputum, etc.). Another option is for the doctor to provide samples of biomaterial to the patient (for example, surgical material, cerebrospinal fluid, biopsies, etc.). After receiving the samples, the patient can either independently deliver them to the Diagnostic Center or call a mobile service at home to transfer them to the laboratory.
* The price does not include the cost of taking biomaterial. Services for collecting biomaterial are added to the pre-order automatically. When ordering several services at a time, the biomaterial collection service is paid only once.
The human intestine contains “beneficial” bacteria – bifidobacteria and lactobacilli, which are responsible for normal digestion and neutralization of harmful substances. In addition to beneficial microorganisms, “harmful” bacteria can settle in the intestines - they cause digestive problems and other unpleasant pathologies.
Pathogenic microorganisms are always present in the intestines - in small quantities, but if their number increases several times, then dysbiosis develops.
What is it and what is it for?
In order to identify it, a laboratory test is used, which shows what type of bacteria predominates in the human intestines.
In total, there are 2 types of stool examination - bacteriological and biochemical . They are prescribed for the same unpleasant symptoms from the gastrointestinal tract.
Bacteriological analysis of stool is carried out to determine the types of pathogenic bacteria that affect the intestines - these can be staphylococci, streptococci, clostridia, fungi, etc.
Bacteriological examination is carried out using microscopy and the amount of pathogenic microorganisms per 1 gram of collected sample is examined. Results are recorded in CFU.
Biochemical analysis of feces is a type of laboratory diagnostics, the purpose of which is to determine biochemical parameters .
Using this procedure, the following pathologies can be identified:
- Irritable bowel syndrome.
- Colitis.
- Intestinal tumors.
- Liver dysfunction.
- Disorders of the pancreas.
Diagnosis of diseases caused by bacteria
It is possible to identify the cause of a disease caused by an increased number of enterococci only using laboratory research methods.
In addition to stool analysis, urine tests and a smear may be required. The latter is used in most cases in women, since bacteria often cause vaginitis and other inflammations of the genital tract.
If enterococci appear in large numbers, then blood tests may be required to determine the inflammatory response. Other diagnostic methods are selected taking into account the specific course of the pathology.
Indications for use
This study may be prescribed for the following indications:
- Alternating diarrhea and constipation for a long time.
- Stomach ache.
- Bloating, flatulence.
- Skin rashes, body rash.
- For gastroenterological diseases.
- After therapy with antibiotics, non-steroidal anti-inflammatory drugs or hormones.
Enterococci in stool are increased
The bacteria can cause serious health problems. These include:
- Meningitis. Infectious disease of the lining of the spinal cord or brain.
- Diverticulitis. A painful process associated with the formation of various formations on the walls. Disturbs the processes of normal intestinal motility.
- Pathologies of the genitourinary system. If left untreated, chronic forms may appear that are difficult to treat and cause relapses.
- Endocarditis. Heart disease, which can be acute or chronic. Pathogenic microflora affects the inner lining of the atria, ventricle, and valve apparatus.
- Septic arthritis. It causes infection of the joints.
- Gastritis. Characterized by superficial inflammation of the stomach lining.
- Enteritis. A pathology that mainly affects healthy cells of the small intestine.
In infancy, an excessive increase in the number of bacteria can be assumed based on various symptoms. These include the release of foul-smelling feces, diarrhea, and bloating. The child may become whiny and refuse to eat.
In adults, signs of an increase in pathogenic microflora are not only symptoms characteristic of a particular disease, but also depression, weakness, and increased fatigue. In men, potency may suffer.
How to take it correctly
In order for the results of the study to be as accurate as possible, the following conditions must be met before submitting:
- Specimens should be placed in a sterile container with a tight-fitting lid. You can buy such a container at the pharmacy, but if for some reason there is no special container, you can use an ordinary small glass jar, pre-washed and scalded with boiling water.
- For an objective study, you need to collect material from different parts of the feces using a spoon attached to the container.
- One spoonful of material from each area is enough for research.
- Urine, menstrual fluid and other substances should not get into the stool.
- If there is mucus, blood and other secretions in the stool, then the stool from these areas must be collected.
- The intestines should be emptied naturally; the use of enemas and laxatives is unacceptable.
- 3-4 days before the test, you must stop taking antibiotics, antidiarrheal and anthelmintic drugs, probiotics, drugs containing barium and bismuth (they tend to discolor stool), and non-steroidal anti-inflammatory drugs. You should also not use any rectal suppositories, Vaseline or any type of oils.
- The analysis should be prescribed no earlier than 2 weeks after stopping antibiotics.
- 3-4 days before the test, it is recommended to follow a diet: exclude all types of legumes, fermented milk products, sweets and flour. It is necessary to add foods rich in fiber to your diet - vegetables, fruits, cereals.
You need to attach a piece of paper with written data to the container with feces: full name and date of birth. This piece of paper can be obtained from your local doctor.
Features of therapy
Treatment largely depends on which microorganisms have deviated from the norm, whether there is mucus, blood and other particles in the stool that should not be there. The doctor, studying the results, makes a diagnosis no earlier than he analyzes all the indicators.
If the transcript shows a decrease in the amount of E. coli, this may indicate the presence of worms in the intestines. Sometimes the cause may be a decrease in enzymatic activity, which is why this bacterium does not bring any benefit (although it does not harm). Despite all the benefits of E. coli, its number should not exceed the norm. If this happens, it means that dysbiosis is developing in the body.
As for hemolytic E. coli, in young children they should be completely absent. These pathogens produce toxins that negatively affect the nervous system and intestines, and can also cause various intestinal diseases and allergies.
Deficiency of bifidobacteria and bacteroides leads to long-term intestinal disorders in both children and adults. These bacteria appear in the baby on the tenth day of life. At the same time, children born through cesarean section have significantly fewer of them than babies born naturally.
Lactose-negative enterobacteria in children and adults should not exceed the norm. If the analysis shows their increased proliferation, this can explain the baby’s heartburn, regurgitation, belching, and increased gas formation. Enterococci normally do not harm the body and are even beneficial. But if their number is higher than normal, they will cause the development of infectious diseases of the pelvic organs and urinary tract.
While non-pathogenic staphylococci do not particularly harm the body (within normal limits), the presence of Staphylococcus aureus is dangerous for children. It causes diarrhea, vomiting, abdominal pain, high fever in the baby, mucus and blood are present in the stool. Therefore, Staphylococcus aureus should be absent in the feces of infants . If Staphylococcus aureus is present in the body, then its effect depends on beneficial bacteria . If their number is normal, the body is not afraid of Staphylococcus aureus and the baby does not need treatment. In severe cases, hospitalization is required.
When the doctor prescribes treatment, his instructions must be followed. To destroy fungus, clostridia, Klebsiella, lactose-negative enterobacteria, Staphylococcus aureus, normalize the digestive system, and get rid of mucus in the feces, special medications designed for small children are needed.
During treatment, special attention should be paid to the nutrition of children, since in many cases it is an incorrectly selected diet that causes the growth of clostridia, enterobacteria, Klebsiella and other pathogens. The diet must be agreed with your doctor. If the baby is breastfed, the mother must follow the diet.
Problems with the functioning of the stomach and intestines bother many people. You can get rid of them after prescribing the right treatment. An analysis for dysbacteriosis will help determine the type of therapy. Thanks to the results, the attending physician will learn about the composition of the intestinal microflora of an adult or child, determine the cause of the imbalance, and prescribe appropriate methods of intervention.
Decoding the results
A normal stool test is negative for the following:
- Hidden blood - occurs with cancer of various parts of the intestine, hidden bleeding, helminths, inflammation.
- Bilirubin - manifests itself in liver disorders, gastroenteritis, acute food poisoning.
- Iodophilic flora - occurs as a result of the predominance of pathogenic microorganisms in the intestines (dysbacteriosis), pathologies of the stomach and pancreas.
- Starch – possible pathologies of the small intestine.
- Protein – appears in gastritis and pancreatitis.
- Ammonia – ammonia content increases during putrefactive processes in the intestines and during inflammation.
The normal acetic acid content should be 5.88 mg/g . An acceptable value is from 5.35 to 6.41 mg/g .
Propionic acid should normally be 1.79 mg/g , the permissible value can range from 1.63 to 1.95 mg/g .
Butyric acid should normally be 1.75 mg/g . Acceptable values can range from 1.6 to 1.90 mg/g .
The total content of monocarboxylic fatty acids should not exceed 10.51 mg/g .
Biochemical analysis of stool for dysbacteriosis is a method of studying intestinal microflora, intended to establish the level of biochemical indicators.
Biochemical analysis informs about the predominance of certain types of bacteria in the intestines (Escherichia coli, bifidobacteria, lactobacilli, fungi, etc.).
It is carried out by establishing the spectrum of fatty acids, which are a product of the vital activity of intestinal bacteria.
As is known, the human intestine is practically sterile only at the moment of birth. Already in the first hours of a baby’s life, this organ is populated by entire colonies of various bacteria. Most intestinal bacteria perform useful work: they help digest food and neutralize harmful toxins. But there are also representatives of bacterial microflora that can cause health problems - from bloating to appendicitis.
As a rule, the normal number of beneficial bacteria in the intestines of an adult is about 85% of their total number, and pathogenic microorganisms - 15%. If this balance is disturbed, a condition such as dysbiosis may occur.
Symptoms of intestinal dysbiosis are quite varied: they include flatulence, diarrhea, and many other disorders of the digestive tract. Dysbacteriosis, in turn, can itself be a symptom of a number of quite serious diseases, so doctors often prescribe a stool test for dysbiosis.
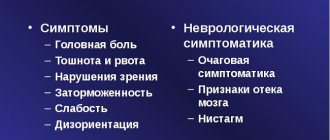
Symptoms and norms
When clostridia, lactose-negative enterobacteria, Klebsiella, Candida fungus, Staphylococcus aureus and other pathogens begin to predominate in the intestine over beneficial microorganisms, dysbiosis develops. Increased proliferation of microbes in a baby is accompanied by the following symptoms:
- regurgitation;
- diarrhea;
- blood, mucus in stool;
- constipation;
- diseases of the digestive system;
- increased accumulation of gases in the stomach (bloating);
- allergic reactions;
- abdominal pain;
- poor appetite;
- there are traces of white coating on the tongue;
- bad breath;
- the baby is often sick.
They will prescribe a dysbiosis test for the baby during or after antibiotic treatment. These medications can cope not only with pathogenic bacteria that have affected the body (clostridium, klebsiella, Staphylococcus aureus, etc.), but also kill beneficial microflora.
Dysbacteriosis can only be detected through stool analysis. Thanks to it, it is possible to determine which pathogenic bacteria have exceeded the norm, which will make it possible to prescribe the correct therapy. This is explained by the fact that to destroy the Candida fungus, different methods are needed than when activating clostridia, Staphylococcus aureus, Klebsiella or other pathogen.
Normally, the number of beneficial and harmful bacteria in the intestines of a baby should fluctuate within the following limits:
| Bacteria | Normal for infants | Children 1 year | After a year | ||
| Form of feeding | |||||
| Chest | Mixed | Artificial | |||
| Bifidobacteria | 10 7 -10 11 | 10 6 -10 9 | 10 6 -10 8 | 10 10 -10 11 | 10 9 -10 10 |
| Lactobacilli | 10 5 | 10 4 -10 6 | 10 4 -10 6 | 10 6 -10 7 | 10 7 -10 8 |
| E. coli | 10 5 -10 8 | 10 6 -10 9 | 10 7 -10 9 | 10 7 -10 8 | 10 7 -10 8 |
| Lactose-negative enterobacteriaceae | 10 3 -10 6 | 10 5 -10 7 | 10 5 -10 7 | up to 10 4 | until 10 7 |
| Enterococci | — | 10 5 -10 9 | 10 6 -10 9 | 10 6 -10 7 | 10 7 -10 8 |
| Staphylococcus | 10 2 -10 4 | 10 3 -105 | 10 3 -10 6 | up to 10 5 | up to 10 4 |
| Clostridia | 10 1 -10 3 | 10 2 -10 4 | 10 3 -10 6 | up to 10 5 | up to 10 5 |
| Candida | 10 2 -10 4 | 10 1 -10 3 | 10 2 -10 4 | up to 10 3 | up to 10 4 |
How to prepare?
To ensure that the analysis results are as objective as possible, you should pay attention to the following requirements:
- three to four days before the test, stop taking any laxatives;
- the analysis is prescribed no earlier than 10-14 days after discontinuation of antibiotics (if they were previously prescribed);
- bowel movements should occur naturally, and not with the help of an enema;
- to collect stool, you should first purchase a special container with a tight lid from a pharmacy or medical facility;
- Drops of urine or discharge should not get into the stool (in women);
- the volume of material required for analysis is at least 10 ml;
- It is advisable to take material for research from different parts of the stool using special spoons supplied with the container. If mucus or blood that has entered it from the intestines is visible in the stool, they are also collected along with the bulk of the material;
- the sample must be delivered to the laboratory no later than three hours after its collection. If the material cannot be delivered within the specified time frame, then the sample can be frozen in a freezer and then delivered the next day.
Preparation and subtleties of the study
To get the most reliable results, the child needs to be properly prepared. Three to four days before the stool collection, there is no need to give the baby new food that he has not yet eaten. A negative reaction of the body to such food can distort the results of the analysis.
Also, a few days before collecting the material, you need to stop giving the medications that the doctor prescribed to your baby. Since each medicine has its own characteristics, the doctor must tell you how long before the test you should not take it. The same applies to medications that relieve colic, as well as laxatives. You cannot give enemas or use rectal suppositories before the procedure.
Before you begin collecting feces, the baby must be washed well so that mucus and other foreign compounds do not get into the material. Feces should be collected after the baby has urinated, clearing the urine from the potty or having a spare one on hand. Otherwise, remnants of urine, mucus and other particles may enter the stool and distort the material. It is better to check with your doctor about how to properly collect material from a baby who does not go potty.
It is best to collect stool from children in the morning. If there is mucus or blood in the stool, they must be captured. The container must be clean, preferably sterilized. The material for examination must be submitted to the laboratory within two hours after it was collected: if the feces are left at room temperature for a long time, it will begin to decompose, and it will be impossible to evaluate the intestinal microflora.
If we talk about how long it will take for the analysis to be ready, then stool culture for dysbacteriosis is done in about a week.
The procedure looks like this: the material is placed in a special container with a nutrient medium. After seven days, all microorganisms (Klebsiella, staphylococci, etc.) living in the feces germinate, after which they are calculated how many are in one gram of feces (COG/g). If mucus and blood were found in the stool, they are also examined.
Most often, a biochemical analysis of stool for dysbacteriosis is used. It is considered more accurate and faster to do. The gastroenterologist makes a diagnosis no sooner than he analyzes the number of all bacteria (clostridium, enterobacteria, klebsiella and other microorganisms).
Standard analysis values
When processing the results of biochemical analysis, the absolute content of acids (unit of measurement - mg/g) and their relative content (unit of measurement - unit) are determined.
Acceptable values of the studied indicators are:
Absolute content, mg/g
Relative content, units.
Total content (C2+…C6)
Anaerobic index (C2-C4)
-0.686 to -0.466
The conclusion form usually contains a description of the intestinal microbiocenosis, detected pathologies of the digestive system, and a list of recommended therapeutic measures to eliminate the detected disorders.
Occult blood test
This examination is practically indispensable for identifying hidden bleeding localized in the organs of the digestive system. Such bleeding often becomes an early sign of a number of severe gastrointestinal pathologies, including oncology. With unnoticed bleeding, even if it has existed for quite a long time, it is quite difficult to detect the presence of blood in the stool, both visually and microscopically. Sometimes this is impossible.
This diagnosis is made by changing the amount of modified hemoglobin. A positive reaction of the studied biomaterial means that the patient has diseases of the gastrointestinal tract, accompanied by a violation of the integrity of the mucosal surface. This is typical for gastric and duodenal ulcers, Crohn's disease, polyps, ulcerative colitis, and helminthic infestations.
Diagnostics is also used to determine the presence of tumors, both primary and metastatic, since even in the initial stages they lead to damage to the intestinal mucosa. The reliability of the analysis increases significantly when it is carried out twice. At the same time, a negative result is not one hundred percent confirmation of the absence of an erosive-ulcerative lesion or neoplasm in the gastrointestinal tract in the person being examined.
What can you find?
Using biochemical analysis of stool, the following diseases and disorders can be diagnosed:
- irritable bowel syndrome;
- nonspecific ulcerative colitis;
- intestinal tumors;
- disorders of the liver (hepatitis, cirrhosis);
- pancreatic insufficiency;
- other pathologies of the stomach and intestines.
You should be aware that conducting a biochemical analysis is not advisable if infectious diseases of the digestive tract are suspected. In these cases, other types of research are carried out aimed at identifying the source of infection.
But in a situation where it is necessary to find the cause of dysbiosis, it is better to give preference to biochemical analysis, because this method is the most accurate and fastest. It should also be taken into account that only a doctor should decipher the results of the study, since a non-specialist is unlikely to be able to understand the reasons for deviations from the norm of certain parameters. Therefore, if the doctor recommends the above method, you should not refuse the offer, because with its help you can obtain important results for diagnosing the disease.
The presence of symptoms such as:
- smell from the mouth
- stomach ache
- heartburn
- diarrhea
- constipation
- nausea, vomiting
- belching
- increased gas formation (flatulence)
If you have at least 2 of these symptoms, then this indicates a developing
gastritis or ulcer.
These diseases are dangerous due to the development of serious complications (penetration, gastric bleeding, etc.), many of which can lead to
outcome. Treatment needs to start now.
Read the article about how a woman got rid of these symptoms by defeating their main cause. Read the material...
- home
- Analyzes and prices
- Biochemical analysis of stool
Biochemical analysis of stool
- Conversion of units of change
- Description of the study
- Preparing for the study
- Transcript of the study
Differential diagnosis of functional and organic diseases of the gastrointestinal tract in children and adults with individual recommendation therapy.
Biochemical analysis of stool for dysbacteriosis
is a laboratory study based on determining the level of biochemical indicators, namely metabolites of volatile fatty acids (acetic, propionic, butyric acid), which are produced by microorganisms, living in the gastrointestinal tract. With various pathologies of the stomach, small and large intestines, and liver, the microflora changes, and, accordingly, the biochemical parameters. By determining the spectrum of volatile fatty acids, one can judge the location and disease of the digestive tract.
To study microflora metabolites, a new method, gas-liquid chromatographic analysis, is used, which makes it possible to adequately assess the state of microbiocenosis not only of the intestines, but also of the oral cavity. Dysbacteriosis is a change in both the qualitative and quantitative composition of the intestinal bacterial flora, which occurs under the influence of various factors: the nature of nutrition, inflammatory processes in the body and treatment with antibiotics, physical and mental stress, surgical interventions, a state of immunodeficiency, a person’s residence in an uncharacteristic area (high mountains, Arctic).
Microorganisms participate in digestion processes with the formation of metabolites - volatile fatty acids (acetic, propionic, butyric). The results of studying volatile fatty acids in feces showed that a decrease or increase in acid concentrations correlates with a certain pathology of the gastrointestinal tract.
The capabilities of this analysis are extensive; it allows you to assess the state of the intestinal microflora and conduct screening diagnostics of intestinal diseases (irritable bowel syndrome, ulcerative colitis, colon cancer). Assess the detoxification function of the liver in liver diseases (chronic hepatitis, cirrhosis of the liver), diagnosis of the circulation of bile acids, cholesterol, and pancreatic insufficiency.
Based on the data obtained, an individual selection of treatment for the above diseases is made; in the case of effective treatment, the quantitative and qualitative composition of fatty acids in the feces is normalized.
The value of this study is that it allows us to understand the nature of changes in the intestinal microbiocenosis and identify the main pathology that led to its development. Also in the Hemotest Laboratory you can get tested for intestinal dysbiosis (with the usual spec. a/b) (code according to form 22.2.).
Biological material:
Stool (sterile container)
Research method: “Gas-liquid chromatography”
Laboratory equipment: "Chromos GC-1000". Modern gas chromatograph with digital control of mode parameters and data processing.
The sensitivity of the technique is 96+2%. Reproducibility of results 98+2%. The error does not exceed 2-4%.
How to properly prepare for taking a biochemical stool test:
- Feces should be obtained without the use of enemas or laxatives. The biomaterial is collected under the condition of spontaneous bowel movement.
- Avoid contamination of urine, genital secretions, personal hygiene items and water.
- Biomaterial is collected from a clean and non-moisture-absorbing surface. This could be a clean plastic bag or oilcloth. It is not recommended to collect from a diaper, diaper (diaper).
- A vessel or potty may be used. The container is washed well with soap, rinsed repeatedly with water, and then doused with boiling water and cooled.
- Take 2-4 g (1 teaspoon) of feces into a special container and deliver it to the laboratory within 3 hours.
- Be sure to indicate the type of stool (diarrhea, constipation, normal, stool with laxatives).
- The number of containers with feces is determined by the number of positions required (at the rate of 1 study - 1 container)
Dysbacteriosis is the result of pathological processes occurring in the body of a sick person. The disease not only does not have pronounced symptoms, but also does not have a special clinical picture. That is why identifying dysbiosis is not as simple as it might seem at first glance. A patient who has developed this disease to a greater or lesser extent experiences slight discomfort in the gastrointestinal tract, barely noticeable nausea and (in rare cases) an increase in temperature. Such symptoms can be associated with a disease of any organ. In some cases, dysbacteriosis proceeds completely unnoticed, and the only way to determine the presence or absence of the disease is to conduct competent and professional laboratory diagnostics.
Analysis of stool for dysbacteriosis can reveal the state of imbalance of the patient’s microflora even in the early stages of its occurrence. Today, in laboratory conditions, depending on the clinical picture and condition of the patient, medical staff can conduct two methods of stool analysis: bacteriological and biochemical. The most modern and popular, of course, is the biochemical method. Bacteriological analysis is perfect for primary or basic diagnosis. Having a number of significant drawbacks, this method of identifying dysbacteriosis is not only quite complex, but also inaccurate.
What does proliferation mean in hydrogen analysis?
Proliferation is a term that characterizes the process of cell division and growth. A natural procedure occurring in the body. Does not cause harm to humans, promotes recovery from illnesses and injuries.
Another thing is excessive proliferation in the analysis of dysbacteriosis. A hydrogen-based rapid test helps analyze the development of microflora in the human small intestine. Excessive growth of certain types of bacteria indicates an imbalance. Deviations lead to the development of dysbiosis, causing serious health problems and a significant deterioration in well-being.
Any analysis requires careful attention to compliance with the rules for collecting materials and evaluating the results obtained. With the right approach, research will help identify the cause of many diseases and eliminate their symptoms as quickly as possible in the early stages.
Rules for collecting stool for dysbacteriosis
In order for the outcome of the study to be effective and as accurate as possible, it is necessary to strictly adhere to the established rules for collecting stool for dysbacteriosis. First of all, you need to know what tests you need to take, what they are for, what the duration and cost of this procedure are. The timing of obtaining the finished result also plays an important role.
It is also worth considering that specialists need freshly excreted feces to collect tests. If all this time the patient is using any laxatives or any other medications, they must be discontinued two to four days before the procedure. The same applies to Vaseline oil, as well as the regular administration of any rectal suppositories. In addition, stool obtained after an enema or taking any medications is unsuitable for further research.
When collecting stool, it is necessary to use the natural defecation method. Before this, the patient should urinate to avoid urine feces getting into a special vessel, which must be pre-treated with an antibacterial agent, rinsed with water, and then rinsed with boiling water. Next, the material is placed in a closed container. The space occupied by feces should not exceed one third of its total volume. Please note that within two to three hours the material must be delivered to the analysis collection point. During this time, it is advisable to store it in a cool room, using either a special refrigerated container or a box of ice. Freezing of the product, as well as its long-term (more than three hours) storage is not allowed. Close the stool container tightly and securely and do not store it in any other environment. On the top of the container you must write the patient’s name, date of birth, and the time of collection of stool.
Treatment
Over the past 30 years, enterococci have become resistant to almost all known classes of antibiotics. Despite this, such drugs are among the main ones for the treatment of pathology.
To reduce the risk of developing resistance, combinations of different antimicrobial drugs are used. Additionally, culture is carried out to determine the degree of sensitivity of the enterococcus strain to a particular drug.
Beneficial enterococci allow you to cope with pathogenic microflora. Therefore, they are sold in the form of special products. Probiotics are intended to treat dysbiosis and restore normal gastrointestinal microflora.
Popular and well-known means are Bifiform, Linex. To create such drugs, strains that were selected for the food industry are often used. Such strains are not designed to remain in the body for too long.
If the growth of enterococci is too large, liquid bacteriophage is used. It can be given to children in the first months of life. The bacteriophage can be drunk or used for an enema.
In conclusion, we note that maintaining the normal growth of microflora in the intestines is easy if you follow the correct diet and take walks in the fresh air.
Doctors remind that bad habits reduce the body's defenses. Therefore, it is recommended to abandon them and focus on regular sports and hardening. Particular attention is paid to infants. Their immunity is not yet fully formed, so you need to monitor their proper nutrition.