Inflammation of the pancreas is medically called pancreatitis. Where is it located? Below the stomach, under the duodenum. The pancreas plays an important role in the process of digesting food. It also regulates the level of glucose in a person’s blood; when the pancreas becomes inflamed, this entails a number of negative consequences for the entire body, because the processes in it are connected like links in a chain.
Statistics show that both children and adults are susceptible to this disease, but the latter suffer from this disease three times more often. The symptoms of pancreatitis are especially pronounced in women.
Many patients delay going to the doctor and are treated with traditional recipes. But are they always effective? Is it possible to treat pancreatitis only with traditional medicine or is this a disease that can only be treated with medication? As with any disease, pancreatitis needs to be diagnosed and treated as quickly as possible. Timely treatment helps improve the patient's quick recovery.
Reasons for the development of pancreatitis in women
The main reasons why an inflammatory process develops in the tissues of the pancreas are considered to be alcohol abuse and poor diet. Since these factors are mostly “male”, in women other reasons come to the fore in the list of etiological factors, although bad habits and unhealthy eating are also common among women.
Poor nutrition
The pancreas is the main organ of the digestive system, producing enzymes necessary for the complete digestion of food. Everything a person eats or drinks goes from the mouth to the stomach, then to the intestines. The process of breaking down complex compounds begins in the mouth, then further along the digestive tract. When saliva and gastric juice are secreted, the pancreas reflexively begins to produce enzymes that normally enter the duodenum. That is, food intake is the main irritant for the gland, provoking its activity.
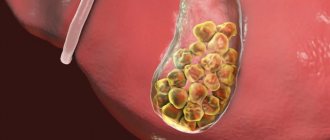
If food is too salty, sweet, fatty, spicy, bitter, coarse in consistency, cold or hot, the functional activity of the pancreas increases and more pancreatic juice is produced than required. When the outflow of secretions is disrupted due to impaired motility of the pancreatic ducts, the proteolytic enzymes of the gland begin to destroy its own tissues: this is how acute inflammation develops, which can be complicated by a dangerous condition - pancreatic necrosis.
Poor nutrition is called not only when you eat prohibited foods, but also when your diet is violated:
- rare meals
- frequent overeating
- unbalanced diets associated with a lack of vital nutrients in the diet (proteins, complex carbohydrates, vitamins, micro- and macroelements).
Alcohol
Abuse of drinks containing alcohol is one of the main causes of liver and pancreas diseases. “Female” alcoholism has become a fairly common problem in modern society.
The ethanol contained in alcohol and its metabolic products cause toxic damage to the parenchymal tissue of the pancreas: both the exocrine and endocrine parts of the gland are destroyed. This quickly leads to digestive disorders, diabetes, and dangerous complications of pancreatitis.
Other reasons
Among other causes of pancreatitis in women, the leading role is played by:
- pathologies of other organs of the digestive tract, especially cholelithiasis, cholecystitis, biliary dyskinesia, gastritis, hepatitis, duodenitis, tumors of the hepatobiliary system, peptic ulcer of the stomach or duodenum,
- frequent stress,
- smoking,
- metabolic pathologies, endocrinopathies (hypothyroidism, obesity),
- infectious or parasitic diseases of the gastrointestinal tract,
- pregnancy,
- circulatory disorders of the gastrointestinal tract due to atherosclerotic vascular lesions, hypertension,
- abdominal injuries,
- congenital anomalies of the structure of the digestive organs,
- taking medications (diuretics, antibiotics, anthelmintics, contraceptives),
- hereditary predisposition.
Pancreatic amylase: normal in the blood
One of the main indicators for diagnosing pancreatitis is the amylase content . Amylase is an enzyme produced by the pancreas and salivary glands to digest food.
The level of enzyme in the blood changes with age, but does not depend on gender.
Normal levels of amylase in the blood:
| age | Indicators, units/l |
| Up to a year | <8 |
| 1-10 | <30 |
| 10-20 | <40 |
| 20-70 | <125 |
| From 70 | <160 |
Exceeding the normal level of pancreatic amylase indicates inflammatory disease of the pancreas. Moreover, the amount of enzyme is not related to the severity of the disease. This enzyme is also excreted in the urine; analysis of its content is called urine diastasis. The normal level of pancreatic amylase in the blood of women 20-50 years old is 50-65 units/l.
Clinical picture of pancreatitis in women
The symptoms of pancreatitis in women and men are almost the same. The differences may be associated with the anatomical and physiological characteristics of the female body (with the development of inflammation of the pancreas during pregnancy), greater concern for their health, compared to men, and excessive emotionality.
The clinical picture of the disease depends on the type of pancreatitis (acute or chronic), the severity of inflammation, the pain threshold (in women it is usually lower than in men), and the general condition of the gastrointestinal tract.
The first manifestations of pancreatitis
Usually the very first and most striking symptom of pancreatitis is abdominal pain. It is usually localized in the stomach (the area between the sternum and the navel), left or right hypochondrium. When the body and tail of the pancreas are inflamed, the pain is girdling in nature, felt in the back, chest, radiating to the lower abdomen, heart area, right or left collarbone, shoulder, forearm. Unpleasant sensations in the stomach begin after eating, drinking alcohol, or due to “nerves.”
In addition to the pain syndrome, dyspepsia syndrome appears (the patient feels sick after eating, problems with stool appear, and gas formation in the intestines increases).
Acute phase symptoms
Acute pancreatitis develops less often in women than in men. This pathology has the most vivid clinical picture, which is associated with massive acute damage to the parenchymal tissue of the pancreas under the influence of a pathogenic factor (alcohol, “prohibited foods,” nervous or physical stress). The main signs of acute pancreatitis in women:
- severe pain in the abdomen (in the epigastrium, right or left hypochondrium, of a girdling nature, radiating to the lower back, chest),
- nausea,
- profuse vomiting that does not improve the patient’s condition,
- diarrhea,
- temperature rise to febrile levels,
- general weakness, fatigue,
- dizziness,
- decreased blood pressure, increased heart rate, breathing,
- pallor of the skin, mucous membranes or their yellowness with simultaneous blockage of the bile ducts,
- hemorrhagic spots on the skin in the projection of the pancreas.
Acute pancreatitis can be complicated by the occurrence of internal bleeding, pancreatic necrosis, the formation of an abscess on the gland, followed by peritonitis. Such conditions require immediate hospitalization of the patient in the surgical department: such diagnoses cannot be treated at home.
If severe chest pain suddenly appears, along with other symptoms of acute pancreatitis, then it is necessary to exclude acute cardiac pathology (myocardial infarction, angina attack).
Chronic inflammation often occurs due to inadequate treatment.
Signs of chronic form
Chronic pancreatitis is characterized by an undulating course with periodic exacerbations and periods of remission. Due to exacerbations of the inflammatory process, pancreatic tissue is gradually destroyed and replaced by connective tissue: inactive areas appear on the organ.
When the exocrine part of the gland is damaged, characteristic disturbances in the digestive processes develop, which are manifested by the following symptoms:
- constant pain in the abdomen,
- feeling of heaviness, distension, bloating,
- bad breath,
- bowel disorder (diarrhea or constipation),
- belching, nausea after eating,
- weight loss, anemia, signs of vitamin deficiencies, lack of microelements.
If, as a result of the inflammatory process, the islets of Langerhans (endocrine section of the pancreas) are damaged, then the patient develops diabetes mellitus. The main characteristics of this pathology:
- constant thirst, dry mouth,
- frequent urination,
- numbness in the limbs due to diabetic polyneuropathy (nerve damage due to long-term diabetes),
- visual impairment,
- headaches, dizziness due to diabetic damage to cerebral vessels,
- disturbances of consciousness (from fainting to coma).
Exacerbation of chronic pancreatitis
The chronic inflammatory process in the pancreas worsens due to errors in diet and other external or internal factors. According to the clinical picture, exacerbation of chronic pancreatitis is similar to acute pancreatitis. But, as a rule, the attack is not so pronounced, and with each new episode the pain and other symptoms are felt less strongly. But this only indicates that the patient is “getting used to” exacerbations, and the gland is increasingly damaged.
Why does the disease develop?
The mechanism for the formation of this disorder is expressed in the following: pancreatic enzymes begin to corrode and digest their own matter. Cell destruction occurs, a reaction is observed from the body - an inflammatory process occurs.
All this is accompanied by intoxication, which can also lead to the emergence of an infectious process. Damage to other organs and systems, for example, kidneys, brain, heart, lungs, is formed.
In most situations, they directly lead to the death of the patient.
However, this is a simple diagram. In fact, the picture of the disease is always more complex. For example, it is important to distinguish between chronic and acute processes, relapses of acute and exacerbation of chronic diseases.
Pancreatitis during pregnancy and early postpartum period
During pregnancy, a woman develops pancreatitis due to impaired blood supply to the gland due to compression of blood vessels by the growing uterus. In addition, the excretory pancreatic and bile ducts are compressed, which provokes stagnation of bile and pancreatic juice. During pregnancy, in the postpartum period, and while breastfeeding a child, a woman’s body undergoes serious hormonal changes, as a result of which changes occur in the functioning of the gastrointestinal tract. These factors contribute to the development of swelling and inflammation of the pancreas.
With the development of a severe hemorrhagic form of pancreatitis, the woman’s condition suffers greatly, and there is a threat to the course of pregnancy. Therefore, it is extremely important to be examined in advance and treated for all serious diseases, and to follow a therapeutic diet for pancreatitis.
It is impossible to rely only on folk remedies for the treatment of pancreatitis, despite positive reviews and the commitment of pregnant women to precisely this “safe” treatment. You should take all traditional medications prescribed by your doctor: enzyme preparations (Pancreatin, Mezim), antispasmodics (No-Shpa) and many others.
A woman may consider symptoms of dyspepsia (nausea, vomiting) to be manifestations of toxicosis, which makes it difficult to timely diagnose pancreatitis in the first trimester of pregnancy. A comprehensive examination, including laboratory and instrumental diagnostic methods, helps to establish a correct diagnosis.
Therapeutic diet
Diet is one of the most important stages in the treatment of diseases of the digestive system.
The list of permitted products for pancreatitis outside of exacerbation includes:
- fresh and boiled vegetables, soups with vegetable broth;
- boiled lean meat;
- low-fat dairy products;
- porridge;
- compotes;
- egg whites;
- slightly stale bread.
- alcoholic drinks;
- fatty meats, fish and broths based on them;
- canned food, pickles, marinades;
- fast food;
- mushrooms;
- beans;
- carbonated drinks;
- fresh bakery;
- sauces and seasonings;
- fruits high in sugar.
In case of pancreatitis, to ensure the pancreas rests, you need to eat in small portions, every 2.5-3 hours. Chew food slowly and thoroughly. The food should be warm and of a rough consistency; it is not recommended to wash it down with water or other drinks. This diet is followed for several months.
Acute pancreatitis in the first days requires fasting, and in the future - the appointment of a 5P table. When the exacerbation subsides and turns into chronic pancreatitis, 1 table is prescribed.
Therapy for any disease is always more difficult and longer than its prevention. To avoid problems with the digestive system, you should pay special attention to food and avoid bad habits. And if you detect the first signs of the disease, do not self-medicate and immediately seek help from specialists. Timely diagnosis will help to establish the causes of the disease and avoid serious complications.
Diseases of the gastrointestinal tract manifest themselves in almost every second person. The process of inflammation of the pancreas – pancreatitis – occurs in an uncomfortable manner. The organ produces insulin, substances necessary for processing food; if the pancreas does not function properly, all these processes go away from the norm. There are many causes of the disease, and it manifests itself depending on its form. Each person should independently be able to identify the signs of pancreatitis, the symptoms, where it hurts, in order to be able to seek medical help in a timely manner and solve the problem with minimal harm in a short time.
Exacerbation of chronic pancreatitis What is pancreatitis We treat pancreatitis quickly at home Is it possible to eat watermelon if you have pancreatitis? Learn about the symptoms and treatment of reactive pancreatitis
Features of the alcoholic form of pathology
With pancreatitis of alcoholic origin, the pain is usually localized in the right hypochondrium. In addition to pain, signs of alcoholic damage to the pancreas and concomitant pathology of the liver and biliary tract are jaundice, bitterness in the mouth, nausea, vomiting bile, dark urine, light-colored feces.
As a result of frequent exposure to alcohol, the pancreas is constantly inflamed, irreversibly damaged, and symptoms usually develop gradually.
Effect on pregnancy
Pancreatitis of the pancreas during pregnancy most often occurs in a chronic form. The acute form of the disease is much less common. The mortality rate in this case is less than 1%. If an attack of acute pancreatitis occurs in the first or second trimester of pregnancy, it is treated in the usual way, but without using many medications that can adversely affect the fetus and the course of pregnancy.
If the situation allows, the necessary surgical intervention is postponed until the postpartum period. In the first two months of pregnancy, an attack of pancreatitis can lead to miscarriage . An attack in the last stages of pregnancy can be an indication for premature birth.
Doctors agree that pancreatitis does not affect pregnancy. However, patients with pathology of the bile ducts and gallbladder are 20% more likely than others to give birth prematurely. In this regard, women diagnosed with pancreatitis of the pancreas are registered from the moment pregnancy is confirmed and monitored throughout the entire period.
Complications of pancreatitis
Inflammation of the pancreas is a serious disease; if it is not diagnosed and treated on time, dangerous consequences develop:
- pancreatic necrosis,
- gastrointestinal bleeding from minor, detected only by examining stool for occult blood, to hemorrhagic shock,
- erosive and ulcerative lesions of the stomach or duodenum,
- abscesses, phlegmon of the pancreas,
- peritonitis, infectious-toxic shock,
- pancreatic cancer,
- diabetes,
- pancreatogenic diarrhea, cachexia (exhaustion),
- pain shock.
Pancreatitis in women has some differences in the clinical picture compared to “male” pancreatitis. This is due to the anatomical, physiological and neuropsychic characteristics of the female body. Symptoms of the disease depend on the causes that caused it, concomitant pathological or physiological conditions. In order to avoid severe complications of pancreatitis, it is necessary to establish a correct diagnosis in time and begin effective treatment.
Bibliography
- Maksimov, V. A. Clinical symptoms of acute and chronic pancreatitis. Directory of General Practitioners. 2010 No. 3 pp. 26–28.
- Bozhenkov, Yu. G. Practical pancreatology. Guide for doctors M. Medical book, N. Novgorod Publishing house NGMA, 2003.
- Merzlikin N.V., Pancreatitis. – M.: GEOTAR-Media, 2014.
- Khazanov A.I., Vasiliev A.P., Spesivtsev V.N. et al. Clinical problems of chronic pancreatitis. Chronic pancreatitis: Mater, scientific. conferences. M.: GVKG im. N. N. Burdenko, 2000, pp. 3–14.