Reasons for appearance
Phlegmon can occur in both adults and children of any gender. Inflammation begins as an independent pathology or develops as a complication of purulent processes: boils, abscesses, arthritis, osteomyelitis, carbuncles and others. In addition to these provoking factors, the reasons may be:
- limb tissue injury;
- bite of an infected shellfish, fish or animal;
- introduction of chemicals under the skin (kerosene, turpentine, gasoline, narcotic drugs, etc.);
- violation of asepsis measures during surgical interventions.
Cellulitis can appear anywhere in the body. The disease is localized on the tissues of the jaw due to caries, chronic tonsillitis, lymphadenitis or pulpitis that has not been cured for a long period. Cellulitis of the thigh is sometimes a primary pathology, but there are often cases of disease development due to the ingress of pus from nearby areas (hip joint, abdominal tissue).
Diagnostics
At the appointment, the doctor clarifies the patient’s complaints, the fact of a previous foot injury, the patient’s state of health and the presence of concomitant diseases. The last point is very important, since some chronic pathologies, for example, diabetes, have a very negative effect on the course of the inflammatory process in the soft tissues of the foot, reduce the effectiveness of therapy, delay recovery or even make it impossible.
We also recommend reading: Swelling and pins and needles in an injured foot
Then the doctor examines and palpates (feels) the foot, specifying the extent of hyperemia and swelling, points of greatest pain, and the presence of fluctuations. The last symptom, namely fluctuation, is a feeling under the fingers of liquid transfusion under the skin or its vibration, and if you lightly tap on one edge of the phlegmon, then after a split second the shock will be felt at the other end of the lesion. However, this symptom is not specific to phlegmon; it also occurs with an abscess (a cavity in the soft tissues filled with pus, but with clear boundaries due to the presence of a dense capsule).
At the same time, the doctor checks the functionality of the foot joints, damage to regional lymph nodes, and measures the patient’s body temperature. If necessary, he prescribes a clinical and biochemical blood test. The results obtained in the laboratory and during a clinical examination are used for the differential diagnosis of phlegmon, that is, to exclude such pathologies and to make a final diagnosis.
A patient's blood test helps clarify the diagnosis.
As a rule, phlegmon of the foot is differentiated from the following diseases:
- abscess;
- tenosynovitis (inflammation of the tendon bed);
- purulent arthritis;
- osteomyelitis (inflammation of the periosteum of the foot bones).
Risk factors and pathogens
The chance of developing leg phlegmon increases with decreased immunity, which is a consequence of diabetes, oncology, HIV infection, hypovitaminosis, tuberculosis, various blood diseases and other reasons. In this condition, the disease develops quickly and is severe. Researchers have found that opportunistic bacteria can also cause the formation of phlegmon.
The pathology is often observed in people suffering from diabetes. Their immune responses are reduced, and because of this, even minor disorders of the skin can cause severe tissue damage. Pathogenic microflora, entering an open wound, causes the rapid spread of infection in the patient’s body.
The most dangerous bacteria are those that are resistant to medications, for example, Staphylococcus aureus. If it affects the skin and tissues, then therapy will be extremely difficult. The microorganism becomes a provocateur of purulent inflammation not only if it penetrates the wound surface, but also without damaging the skin and fatty tissue. This can occur when microbes enter the lymphogenous route or through the bloodstream.
Alcoholism and drug addiction disrupt the functioning of all human organs and systems, which makes it less resistant to the influence of pathogens. This is facilitated by regular severe intoxication. Therefore, such people often suffer from the disease in question.
Cellulitis is also caused by other microbes. Pseudomonas aeruginosa, which lives in water and soil, is introduced into tissues as a result of a deep cut or scratch. Pasturella multocida comes into contact with the skin of people who frequently interact with dogs and cats. Infection with Erysipelothrix rhusiopathiae can occur from crabs, fish and other river and sea life.
Cellulitis - causes
Putrefactive processes are provoked by pathogenic bacteria, mainly Staphylococcus aureus. Less commonly, inflammation is caused by other microorganisms (anaerobes, streptococcus, Proteus vulgaris, Haemophilus influenzae or Escherichia coli), and sometimes the causes of phlegmon remain unknown. The classification of the disease is carried out depending on the nature and characteristics of the causative agent of decay.
All the factors that provoke the pathology in question are easy to identify if you better understand the mechanisms by which phlegmon develops, what it is, and where it begins. To trigger the inflammatory process, it is necessary for pathogenic microorganisms to penetrate the adipose tissue. This happens in the following cases:
- abrasions;
- cuts;
- injuries;
- suppuration of the lymph nodes;
- caries;
- furunculosis;
- tonsillitis;
- breakthrough of a purulent focus (carbuncle, abscess);
- animal bites and other injuries.
There are conditions that help accelerate the progression of pathology:
- immunodeficiencies;
- diabetes;
- tuberculosis;
- HIV;
- hepatitis;
- chronic intoxication;
- exhaustion of the body.
Classification and forms
The disease can be primary (occurs as a result of direct infection), secondary (when inflammation spreads from nearby tissues), acute, sluggish, superficial or internal, progressive or limited.
According to the type of tissue destruction, phlegmon is divided into the following forms:
- serous;
- purulent;
- necrotic;
- putrid.
According to the method of localization, the disease is classified into types: subcutaneous, intermuscular, subfascial, retroperitoneal, interorgan, as well as phlegmon of the mediastinal tissue, phlegmon of the neck, left and right hand, leg, thigh and phlegmon of the foot. The possibility of infection, the characteristics of the pathology and susceptibility to drugs are also determined by the type of pathogenic microorganism.
If inflammation with the formation of pus appears next to some organ, then it is called from the Latin name of this organ with the addition of the prefix “para”, which means “near” or “around”. For example, around the kidneys there is paranephritis, near the uterus there is parametritis.
During the acute period, phlegmon moves from one organ to another. From the finger area it can reach the calf muscle, and then to the thigh.
Forms of phlegmon
The described disease is classified according to the nature and extent of tissue damage. The following types of inflammation of adipose tissue are distinguished:
- Serous phlegmon - what is it: a mild, initial form of the disease, which is characterized by the accumulation of exudate in damaged areas. The cells of the subcutaneous fat layer are infiltrated with leukocytes, it takes on a gelatinous appearance, as it is saturated with a turbid watery liquid. The border between affected and healthy areas is not visible.
- Purulent phlegmon or histolysis. The tissue melts, the exudate becomes yellowish, green, white, and becomes very cloudy. Erosion, ulcers, fistulas, and cavities may form. Sometimes the inflammatory process spreads to tendons, muscles and bones, causing their destruction.
- Putrid phlegmon.
Without treatment, the previous form of pathology deeply affects the tissues, leading to their dissolution, turning into a slippery, loose mass of a dark green or dirty brown hue. There is a stench and symptoms of acute intoxication are present. - Necrotic phlegmon - what is it: a severe type of disease accompanied by tissue death. Such zones can be limited from healthy cells by a granulation barrier, or rejected by the body, leaving deep wounds in their place.
- Anaerobic or gas phlegmon. The inflammatory process is very extensive, characterized by the appearance of large necrotic zones and the formation of blisters on them. Soft fabrics acquire a dark gray color and a strong, unpleasant odor. During palpation, crepitation (crunching) is heard, which is explained by the bursting of bubbles and the release of gas.
Symptoms and signs
The obvious symptoms of cellulitis will be inflammation, swelling and deterioration in well-being. In the affected area, there is obvious redness on the skin and swelling due to the accumulation of pus. There is swelling of the lymph nodes. Acute phlegmon is characterized by high temperature up to 38-40º and above, general intoxication, thirst, lethargy, chills and headaches.
The sore spot is hot to the touch and the skin is shiny. Pus can melt deeper layers of tissue, due to which the area of formation becomes much larger. With the development of extensive phlegmon, all signs become more obvious. The pain is regular, throbbing, and intensifies at night. In addition, the outer covers may be damaged, and the purulent contents come out. The patient develops shortness of breath and a strong increase in temperature. The pulse and blood pressure drop, little urine is produced, the head hurts severely and yellowness appears on the skin.
Symptoms of phlegmon, first signs
Phlegmous inflammation of the subcutaneous tissue has different forms, and the first signs of phlegmon are as follows:
- soreness of the affected area;
- swelling;
- the skin becomes warm to the touch;
- redness appears if inflammation reaches the superficial layers;
- enlargement of nearby lymph nodes;
- general weakness;
- the temperature can rise to 38-40 °C.
Phlegmon develops through two stages - infiltrative and purulent. In the first phase, a dense formation forms under the skin.
When it enters the purulent stage, it softens, and the symptoms are as follows:
- chills, fever (39-40 °C);
- confusion, depressed or excited mood;
- lack of appetite;
- weakness, feeling of weakness;
- tachycardia;
- headache.
In severe cases, the liver and spleen become enlarged, the sclera of the eyes and mucous membranes turn yellow. Red stripes appear on the body along the inflamed lymphatic vessels. If the infection penetrates into the deep and superficial veins, thrombophlebitis develops.
Oral phlegmon is also called Ludwig's angina and develops when pathogens penetrate the submandibular area. The symptoms in this case are as follows:
- swelling of the tongue, sometimes so severe that it blocks the throat, interfering with normal breathing;
- bad breath;
- pain in the area of inflammation;
- increased salivation, pain when swallowing, or inability to swallow;
- general loss of strength.
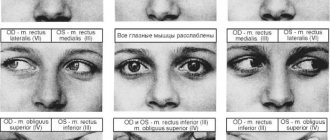
Phlegmon of the orbit develops rapidly and usually on one side. Symptoms:
- throbbing pain in the area of inflammation;
- swelling and redness of the eyelid;
- malaise, nausea;
- inability to open the eye;
- fever.
At the same time, the risk of developing blindness is high. If inflammation affects the optic nerve, a purulent corneal ulcer or neuritis is formed.
With late diagnosis due to eye atrophy, the chances of regaining vision are reduced to zero.
Cellulitis of the neck often accompanies purulent lymphadenitis. Provocateurs can be tonsillitis, sinusitis, otitis media and other inflammatory diseases of the oral cavity and respiratory tract.
The neck increases in diameter, and when you try to turn your head, a sharp pain occurs. Symptoms common to phlegmatic inflammation also appear - high fever, headache, weakness.
Abscesses and phlegmon of the maxillofacial area are dangerous because the infection can spread to the meninges and brain, causing meningitis and brain abscess. If inflammation develops in the deep tissues under the fascia, then the risk of blood poisoning is high.
Diagnostic measures
If there is a suspicion of the presence of phlegmon of the thigh, then the specialist examines this area of the lower limb, takes blood for analysis, as well as pus that is released from the wound. The first study will reveal inflammation in the patient’s tissues, and the second will determine the type of pathogen that caused the disease.
Despite the fact that phlegmon is an infectious disease, it is not contagious. It usually develops under the skin, and the epidermis layer prevents it from coming out and spreading. This distinguishes it from a similar disease - impetigo, which is localized on the surface of the skin and is highly contagious.
Symptoms
In the acute form, all pathological symptoms are most pronounced, and their intensity increases over 1-2 days or even several hours. First, the patient begins to feel pain in the foot, which intensifies when putting on familiar shoes. Walking becomes difficult, the flexion and extension of the fingers, the raising and lowering of the foot, and its movements in the ankle joint are somewhat limited.
Then there is an increase in the volume of the foot due to swelling and increasing accumulation of exudative and purulent masses in the subcutaneous space. At the same time, the patient begins to feel heat in the foot and visually notices hyperemia of the skin (redness), sometimes a local “bulging” of the reddened skin is visible. Hyperemia is combined with a characteristic shine that occurs due to stretching of the dermal structures by edema. It is noteworthy that the boundaries of hyperemia appear diffuse, blurry and do not have clearly defined boundaries. This sign is very important for differential diagnosis and helps to distinguish cellulitis from another disease caused by streptococcus, called erysipelas of the foot.
Fever with phlegmon is an integral part of the pathology
The further the disease progresses, the more the foot increases in volume, the more its contours smooth out, the toes swell, the more painful and intense the pain syndrome becomes.
Regional lymph nodes (popliteal, inguinal) begin to respond to the presence of infection in the structures of the foot and its spread throughout the lower limb. Most often this happens to the popliteal lymph nodes, which increase in size and become easily palpable and painful. In severe cases, the skin over them turns red, and pink or red stripes appear from the foot along the entire shin, which indicate the development of lymphangitis (inflammation of the lymphatic vessels).
Simultaneously with the development of local signs of phlegmon on the left or right foot, general symptoms appear, which are combined into the concept of intoxication syndrome. It manifests itself as follows:
- fever, or increased body temperature, which with phlegmon of the foot can reach 39-40 degrees;
- Strong headache;
- a sharp deterioration in health, severe weakness, malaise, lack of appetite;
- characteristic laboratory signs (in a clinical blood test there is an increase in the number of leukocytes, a shift towards young leukocyte forms, an increase in ESR).
In case of complications of phlegmon, the patient is urgently taken to the hospital
It is important that when the very first pathological symptoms appear, the patient goes to a clinic or hospital. The later this happens, the more complications that threaten the health and life of the patient may develop in the future.
Treatment methods
Without surgical intervention, phlegmon of the thigh and other parts of the lower limb can be treated only in the initial stage, if there is still no pus under the skin. The patient is strongly advised to remain in bed with immobilization of the knee and ankle joints. The patient is prescribed intramuscular antibiotics or a complex of antibiotics with corticosteroids, as well as physical therapy (UHF) and dry heat to the sore spot. It is also recommended to drink plenty of fluids in order to remove intoxication from the body as quickly as possible.
Treatment of leg phlegmon
Given the high probability of developing severe complications, treatment of phlegmon should be carried out under the strict supervision of a specialist. The disease is characterized by rapid spread, so inadequate therapy can lead to extensive tissue infection, disability and death. Treatment can be conservative (with the use of antibiotics) or surgical. It depends on the nature of the pathogen that caused the disease and the stage of the disease. If the inflammation is superficial and the disease is at an initial stage, treatment using the UHF physiotherapeutic procedure is allowed.
Possible complications
The sooner treatment for phlegmon is started, the lower the risk of adverse consequences. An infectious process that spreads through the blood and lymphatic system can cause purulent diseases such as:
- arthritis;
- meningitis;
- thrombophlebitis;
- osteomyelitis;
- sepsis;
- erysipelas;
- pleurisy.
Under no circumstances should you delay your visit to the doctor and try to be treated with traditional methods. If phlegmon is not diagnosed in time, then the above diseases can be acquired, and in advanced cases, blood poisoning.
The nature of phlegmon
Leg phlegmon is a disease of an infectious nature. With this disease, adipose tissue is damaged as a result of purulent inflammation. With pathology, the subcutaneous fatty tissue is completely destroyed. The intensity of the process directly depends on the severity of the disease, the presence of other diseases, and the state of the patient’s immunity.
Compared to other pathologies of similar etymology, phlegmon does not have clearly defined boundaries of localization; it penetrates much deeper than the skin. A characteristic feature of the disease is that the patient experiences and develops painful subcutaneous inflammation, manifested by swelling with purulent contents. In some cases, the inflammation process is accompanied by chills and high fever.
Prevention
Strengthening the immune system, correct and timely treatment of inflammatory and purulent processes in the body will help reduce the risk of developing phlegmon. It is very important to establish a good metabolism and get rid of all chronic bacterial foci.
To prevent phlegmon of the thigh and lower leg, it is necessary to avoid damage to the skin of the legs, especially in areas where there is a high risk of infection (forest, river, sea, animal habitats). If you suddenly injure your leg, immediately remove any foreign objects that could get into the wound. After this, treat the affected area with an antiseptic (alcohol, vodka, brilliant green, iodine), cover it with a band-aid or cover it with a sterile bandage (cloth).
Prevention can also include a quick visit to a surgeon or traumatologist. A diagnosis made on time will avoid serious inflammation of the tissue and cure phlegmon with therapeutic methods. Follow these simple preventive measures and reduce the risk of developing the disease to a minimum.
https://www.youtube.com/watch?v=6ylqjBugiDs
Forecast
Predicting the outcome of treatment for diabetic phlegmon is quite difficult. This outcome depends on many factors - general health, the state of the immune system, the ability to restore blood flow and close wounds.
Our practice shows that with timely surgery to open the phlegmon and restore blood flow, it is possible to save the supporting limb in 75% of patients. Mortality is about 5% and is associated with worsening concomitant diseases.
Causes
In most clinical cases, the cause of the development of phlegmon of the hand is the penetration of pathogenic microflora into the tissue of the hand through its damaged skin, less often - with a deep violation of the integrity of the nail plate of any finger.
But pathogens are also able to penetrate into the soft tissues of the hand from foci of infection already existing in the body. Such foci may be:
- acute - abscess (limited abscess), boil (purulent inflammation of the hair follicle), carbuncle (purulent inflammation of several hair follicles and sebaceous glands with involvement of surrounding tissues in the pathological process);
- chronic - tonsillitis (inflammatory damage to the tonsils), caries (destruction of hard tooth tissue, accompanied by the development of infection).
Contact spread of the pathological process is also possible - when an abscess, boil or carbuncle breaks through.
note
Cases have been described where phlegmon of the hand was caused by the ingress of a number of chemicals into its tissue - gasoline, turpentine, kerosene and others.
Of the infectious pathogens in the vast majority of cases with phlegmon of the hand, the following are detected:
- Staphylococcus aureus;
- streptococcus.
May also be found:
- coli;
- Proteus.
Other pathogens are detected less frequently; their type depends on the circumstances in connection with which phlegmon of the hand developed. It can be:
Haemophilus influenzae – provokes the development of phlegmon of the hand in young children;
- Pasteurella multicida - this pathogen penetrates the soft tissues of the hand when bitten by a cat or dog, causing the development of phlegmon 4-24 hours after infection;
- a pathogen called Erysipelothrix rhusiopathiae - it is involved in the development of cellulitis of the hand after contact with poultry, pigs, marine fish or shellfish.
This pathology can develop in the presence of an anaerobic infection in the tissues - pathogens that require an oxygen-free environment for reproduction and development. Such phlegmons occur less frequently than with infection with other pathogenic microflora, but they are more severe. These may be anaerobes:
- non-spore-forming (these include bacteroides, peptostreptococci, peptococci);
- spore-forming anaerobes (clostridia).
The chronic form of phlegmon of the hand (also called woody phlegmon) can be caused by:
- diphtheria bacillus;
- paratyphoid bacillus;
- Pneumococcus
and some other pathogens.
It has been revealed that in the presence of certain factors, phlegmon of the hand occurs more often and progresses faster. Such contributing factors include:
- violation of the body's defenses - congenital and acquired immunodeficiencies;
- endocrine diseases - most often diabetes mellitus (impaired carbohydrate metabolism due to lack of insulin), against which phlegmon of the hand is especially severe;
- blood pathologies;
- chronic diseases of the cardiovascular, respiratory, nutritional and other systems;
- exhaustion of the body - mainly after suffering severe injuries and conditions (comas), long-term operations;
- diseases accompanied by chronic intoxication (alcoholism, drug addiction).
Bed rest
During the treatment period, the patient is prescribed bed rest, and the injured limb should be kept at rest. The area of inflammation must be warmed up using a heating pad. Symptomatic therapy allows the use of drugs that relieve pain. This type of therapy must be agreed upon with a competent specialist, since only a doctor can accurately determine the degree of tissue inflammation. With self-treatment, extensive tissue damage cannot be ruled out as a result of the spread of the pathological disease to tissues located near the source of inflammation.
Symptoms
The course of the disease depends on the nature of its pathogenic agent. For example, when infected with putrefactive staphylococcus or Pseudomonas aeruginosa, a putrefactive type of phlegmon develops. When infected with obligate anaerobes, the pathology develops very aggressively, symptoms appear rapidly. Virulence is weakly expressed when affected by weakened strains of the pathogen, which contributes to the chronic course of phlegmon, in which symptoms practically do not appear. Nevertheless, all types of pathology have common clinical signs by which the disease can be diagnosed.
With phlegmon of the leg, inflammation can always be observed. This is the most obvious sign of the presence of the disease. The affected area becomes swollen and there is slight redness due to pus that has accumulated under the skin. Palpation of this area is painful, and its temperature is increased.
Another symptom of leg phlegmon is swelling. Against the background of intoxication of tissues located near the source of infection, extensive swelling of the limb is observed.
General deterioration
The patient also notes a general deterioration in health. The spread of pathology and tissue destruction is accompanied by infiltration of nearby areas. The general condition of the infected person worsens, and a strong fever occurs. In the absence of proper treatment, a severe degree of intoxication of the body occurs.
It is important to note that a disease such as hemostatic dermatitis, which is not infectious, can be disguised as phlegmon. It occurs when blood supply to the affected area deteriorates.
Phlegmon of subcutaneous tissue: microscopic specimen
One of the most dangerous diseases that can lead to death is phlegmon of the subcutaneous tissue. The disease leads to purulent inflammation of the soft tissues. Inflammation is caused by pathogenic bacteria, the activity of which leads to the formation of pus.
Cellulitis can be caused by diseases of the lower jaw, infectious diseases of the larynx, inflammation of the lymph nodes in the neck, the presence of boils, wounds and scratches, and purulent inflammation.
Phlegmon can be submental, submandibular, superficial, interfascial. Superficial phlegmon can affect the sternocleidomastoid muscle (its anterior edge). It can also affect the anterior and lateral surfaces of the neck and trachea. The disease can affect the back of the esophagus or the socket of the sternum.
Types of phlegmon:
- Primary. The development of the disease occurs directly in the neck.
- Secondary. They develop due to the fact that inflammation has spread from other areas.
Only a doctor can diagnose phlegmon. Most often, for this he requires the result of research conducted in laboratory conditions. Examination shows that the patient's neck has enlarged. The patient becomes pale, has difficulty breathing, blood pressure decreases, and the temperature rises. The most reliable method of diagnosis is puncture.
Surgery for phlegmon
A skin incision is made in certain places corresponding to the site of inflammation, pus and modest discharge are evacuated. The wound is washed generously with antiseptic solutions, drainage is installed so that the wound does not have time to heal until it is completely cleansed and the inflammation subsides.
It is also very important to perform fasciotomy incisions in certain places and very carefully, professionally, in order to avoid damage to the most important structures of the hand:
- nerves
- vessels,
- tendons.
After performing a fasciotomy, the patient immediately feels better, the pain noticeably decreases, and the symptoms of intoxication of the phlegmon of the hand gradually disappear.
Next, daily dressings are performed and the wounds are washed until they are completely healed.
Antibiotics, vascular drugs that improve tissue nutrition, and anti-inflammatory drugs are prescribed.
In the case of aseptic phlegmon, fasciotomy is performed to reduce intrafascial pressure, namely to allow lymph to drain.
In this case, not antibiotics are prescribed, but antihistamines and anti-inflammatory (usually hormonal) drugs.
Daily dressings are also performed until the copious separation of serous fluid stops and the swelling subsides. The wounds are sutured so that they heal faster and there are no large scars left.
Additional diagnostics
Not only clinical symptoms confirm an abscess - to clarify the nature of the pathology, it is important to conduct additional examination. Among the studies prescribed by the doctor will be the following:
- Complete blood count (leukocyte count, ESR).
- Blood biochemistry (acute phase indicators).
- Puncture of the abscess (with further analysis of the contents).
- Ultrasound of soft tissues.
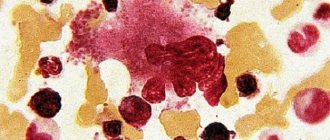
Laboratory signs of abscess and phlegmon include a shift in the leukocyte formula to the left, toxic granularity of neutrophils, and an increase in ESR. Indicators of the acute phase of inflammation (C-reactive protein, seromucoids, sialic acids) also increase. When analyzing pus, it is possible to establish the predominant flora and determine its sensitivity to antibiotics.
An abscess is a purulent inflammation limited to the capsule. Therefore, it is not as severe as phlegmon. However, there is always a danger of the abscess breaking not outward, but into cavities or organs. Therefore, it is important to diagnose it in time in order to immediately begin active therapy.
Immunomodulation
After the source of inflammation of the purulent phlegmon of the leg has been eliminated, the patient is indicated for immunomodulation aimed at strengthening the body's protective barrier. The patient must remember that after cured phlegmon there is still a possibility of re-infection. This is due to the body’s increased sensitivity to pathogens. Rehabilitation therapy involves giving up bad habits, switching to a special diet, taking immunomodulatory medications, and performing health procedures.
Development mechanisms
At the first stage of abscess formation, the tissues are infiltrated with leukocytes and leak with inflammatory exudate. Cellular elements secrete proteolytic enzymes that promote destruction and cavity formation. The walls of the latter are formed by purulent-necrotic masses and fibrous fibers, and later an inflammatory wall of granulations (pyogenic membrane) forms around it.
When pathological exudate has accumulated in the cavity, the second phase of abscess development begins. It can end spontaneously - when the abscess breaks out into the internal cavities or organs. Fresh abscesses that do not have a rough capsule collapse and heal. Less commonly, fistulas form, connecting the cavity of the abscess with the place of its drainage.
With phlegmon, the inflammatory exudate spreads in the subcutaneous tissue, moving from one interfascial space to another. Pus pushes tissue apart and destroys the neurovascular network, thereby causing necrosis. Based on localization, phlegmons are epi- and subfascial (intermuscular).
Measures to prevent phlegmon
The main measure to prevent cellulitis is to avoid breaking the skin, especially if conditions are present that increase the risk of infection. Care should be taken when cleaning and cutting fish - mucus from the scales, if it gets into the wound, causes inflammation in almost 100% of cases.
A cut or scratch, if any, must be properly treated. This in many cases allows one to avoid infection by pathogenic microorganisms. Injured skin should be immediately treated with an antiseptic - this can be a solution of brilliant green, iodine or alcohol. Then apply a sterile bandage or bactericidal patch.
If there are foreign objects in the form of splinters or fragments in a cut or scratch, they must be removed. After which the wound should also be treated with an antiseptic and a bandage applied. When the first signs of infection appear, it is recommended to immediately consult a doctor. This will allow timely treatment to begin and avoid widespread spread of the inflammatory process.
Thus, if you follow simple precautions, the risk of cellulitis is significantly reduced.
We looked at the causes, symptoms and treatment of leg phlegmon.
Source: FB.ru
Surgical drainage
For putrefactive phlegmon, surgical drainage of inflammation is indicated. To do this, incisions are made through which the pus is removed. After the source of inflammation has been removed, the patient is prescribed restorative therapy, including taking antibiotics and using bactericidal dressings.
Treatment of superficial inflammation with phlegmon of the right or left leg, which is at the initial stage of development, can be carried out through the intramuscular injection of potent antibiotics (Gentamicin, Ampiox, benzylpenicillin sodium salt). For example, taking broad-spectrum antibiotics orally, for example, Biseptol, Sulfadimethoxine, Ampicillin.
Removal of phlegmon is carried out under local or general anesthesia. An incision is made on the skin in the area of the lesion in a longitudinal manner. Small vessels of subcutaneous fat are tamponed. If the subcutaneous tissue and underlying muscle tissue are saturated with purulent or necrotic discharge, tissue bleeding is not observed in this case.
If the discharge from the cavity is very abundant, the surgeon uses an electric suction. If there is a slight scanty discharge from the wound, it is enough to thoroughly blot the tissue with a gauze swab. The wound cavity must be thoroughly washed using furatsilin, chlorhexidine or any other antiseptic substance.
If the pathological process is localized in the abdominal cavity or retroperitoneal space, the complexity of the operation increases. In this case, the intervention is performed under general anesthesia. If the tissue of the abdominal cavity or pelvis is damaged, it is important to prevent the development of such a serious complication as peritonitis. To do this, after removal of purulent and necrotic contents, drainage of the abdominal cavity and peritoneal dialysis are performed. The peritoneal cavity is repeatedly washed with flow with the introduction of broad-spectrum antibiotics.
Drainage of the wound is carried out until it is completely cleared of purulent discharge and the signs of the inflammatory process, both local and general, are reduced. After this, the wound is sutured and bandages with medicinal wound healing agents are applied.
What symptoms do you see a surgeon for:
Cellulitis of the neck
Cellulitis of the neck is defined as a disease with a protracted course, in which damage to the intercellular and interfascial spaces of the neck is observed. In the presence of phlegmon of the neck, filling of certain interfascial spaces with purulent contents is also observed (subcutaneous phlegmon of the neck, intermuscular phlegmon of the neck and interfascial phlegmon of the neck). Keeping in mind the complex anatomical structure of the neck, phlegmon can have different locations. Cellulitis, unlike abscesses that develop in the neck, does not have clear elastic walls and is limited to the fascia.
With phlegmon of the neck, purulent contents spread from one interfascial space to another, contributing to the development of diffuse, extensive areas of damage. Pathogens of the purulent-inflammatory process can easily spread along the interfascial tissue, damaging muscles, blood vessels, connective tissue, and lymph nodes.
As a rule, phlegmon of the neck occurs due to the complicated course of catarrhal tonsillitis, opening of peritonsillar and retropharyngeal abscesses. It can also develop due to alveolitis, periodontitis and osteomyelitis of the lower jaw, otitis media, and injuries. Penetration of the causative agent of phlegmon into fatty tissue can occur in various ways: hematogenously, lymphogenously, with the penetration of pus from nearby inflammatory areas. Pathogenic pathogens for neck phlegmon can be various microorganisms: group A hemolytic streptococcus, staphylococci, Escherichia coli, clastridia, Pseudomonas aeruginosa.
With small phlegmons or with deep-lying phlegmons, external skin manifestations on the neck may be absent. Body temperature generally does not rise beyond low-grade fever. Manifestations of intoxication syndrome are mild. But external or extensive phlegmons of the neck are much easier to identify. On the surface of the skin in the neck area there is noticeable hyperemia, swelling and soreness. When palpating the subcutaneous phlegmon on the neck, fluctuation and severe pain are determined, accompanied by skin tension. The general condition of the patient is presented as severe or moderate.
Also, with phlegmon of the neck, patients complain of difficulty swallowing and breathing, especially when the phlegmon compresses the pharynx or esophagus. With the submandibular form of phlegmon of the neck, it is difficult to open the mouth and chew food. At the same time, the mouth is in a half-open state, and a putrid odor emanates from it. As the disease develops and progresses, the patient's condition may worsen significantly. For phlegmon of the neck, only surgical treatment with drainage of purulent foci in a hospital setting is indicated.
Meaning and outcome[edit | edit code]
If the etiological factor is not destroyed (for example, a large parasite, highly pathogenic microorganisms) and pus remains in the tissues, then its encapsulation is possible with the pus turning into a dry curdled mass. At the same time, purulent inflammation of vital organs poses a great danger to the body. Infectious purulent inflammation, especially phlegmon, can cause corrosion of blood vessels, the introduction of purulent elements and microorganisms into other organs with the flow of lymph and blood, with the development of new ulcers or sepsis in them. An immunodeficiency state, uncompensated bacteremia and decay products in foci of purulent inflammation lead to death. [1]
How does the inflammation process start?
Initially, how the body’s immune system is activated:
• Blood flow to the damaged area increases sharply.
• As a result, the local temperature increases.
• There is a release of the liquid part of the blood and white blood cells from the capillaries into the intercellular space to fight the foreign agent (bacteria).
• Hyperemia in the area of damage (redness).
• Soft tissue swelling causes unbearable pain.
These four signs of hand cellulitis - fever, swelling, redness, and pain - characterize inflammation.
As inflammation of the hand develops, pus begins to form in the tissues. The purulent process with phlegmon spreads quite quickly through the cellular and fascial spaces. Finding the path of least resistance and literally melting soft tissue.
That's why emergency surgery is needed. And no amount of antibiotics or anti-inflammatory drugs can suppress this process that has already begun.
Severe intoxication of the body begins, body temperature rises, and chills appear.
Aseptic phlegmon occurs more mildly, without the formation of pus. But lymph is released from the vascular bed in huge quantities, which causes a sharp increase in pressure in the interfascial spaces, which entails intolerable pain, compression of blood vessels, nerves, even necrosis of the fingers.
In such cases, an emergency operation is also necessary to decompress the cellular and fascial spaces - fasciotomy.
Treatment and possible consequences
Treatment of inflammation of the soft tissues of the foot is a long and painful procedure. It includes a set of methods, the main one being surgery. For patients with diabetes, any intervention in the integrity of tissues is dangerous, since the healing process is very slow and poor.
For the operation, it is important to achieve a decrease in sugar levels and maintain them at a low level throughout the recovery period. For this purpose, increased doses of insulin are usually used, including for people suffering from type 2 diabetes.
The operation itself takes place under general anesthesia. The doctor makes a tissue incision at the location of the pus, removes it, and along with it the dead tissue. Then the drainage is installed without sutures.
The wound is restored by secondary intention.
The operation is complex because the foot contains a large number of blood vessels, nerve endings and tendons.
It is important for the surgeon not to damage them, but to completely clean the wound.
During the healing process, the drainage is changed regularly, and the wound is treated with antiseptics and antibiotics to reduce the risk of new infection and eliminate swelling and inflammation.
The leg, as a rule, is fixed for several weeks so that the patient cannot damage the accreting tissues and the process of their restoration proceeds correctly.
In parallel, drug treatment is used, including:
- Antibiotics, first these are broad-spectrum drugs aimed at relieving inflammation and preventing new infections, then more targeted drugs are used that act on the specific type of microorganism that provoked phlegmon.
- Analgesics are used to reduce postoperative pain and speed up the patient's recovery. They can be used in the form of injections, ointments or tablets.
- Antitoxic drugs prescribed in the form of droppers, the contents of which cleanse the body of microbial waste products.
- General strengthening agents, in this capacity are immunostimulating drugs and vitamin-mineral complexes that increase the overall tone of the body.
Complete recovery takes several months, during which the wound heals and the tissue is restored. The patient is usually prescribed bed rest, and the leg is placed in an elevated position so that excess fluid drains out.
To accelerate wound healing, methyluracil ointment or Troxevasin gel is used. Iruksol ointment and similar products containing enzymes are used to remove dead tissue.
In case of poor healing of the wound and large defects, dermoplasty is used, with the help of which these defects are hidden.
If necessary, medications can be used to maintain a normal cardiovascular system. Drinking plenty of fluids is also recommended to help with detoxification faster.
After treatment, the patient must wear orthopedic shoes, which will prevent re-entry of infection into the tissue.
In the case when the disease was detected at the initial stage, surgical intervention may not be required if the infiltrate has not formed. Then the patient is prescribed compresses with yellow mercury ointment or thermal procedures.
If left untreated, phlegmon of the foot can lead to:
- To the spread of infection to the entire vascular system of the legs and the formation of phlebitis and thrombophlebitis.
- To the spread of infection through the bloodstream throughout the body, resulting in sepsis or infectious-toxic shock.
- To the transition of purulent processes to bone tissue, which is fraught with the development of osteomyelitis.
- To the development of a purulent and necrotic process, its spread throughout the entire limb and the occurrence of gangrene, the elimination of which requires amputation of the limb.
It is impossible to treat a disease such as phlegmon at home on your own. This can lead to the growth of infection and complete loss of a limb, and in severe cases, death.
Video from an expert:
How is phlegmon of the foot treated?
Treatment goals for finger abscesses and cellulitis:
- ensure adequate drainage of purulent exudate;
- prevent the spread of infection (using radical necrectomy);
- create favorable conditions for healing with minimal functional and aesthetic disturbances.
Surgical treatment is carried out against the background of antibacterial therapy (taking into account the antibiotic sensitivity of infectious agents). Pain relief and detoxification are essential conditions for successful treatment in the early stages. Foot operations are performed under general anesthesia. The foot is necessarily ischemicized by placing a tonometer cuff on the lower third of the leg and quickly pumping air to 150-200 mm Hg. During the acute period, immobilization of the ankle joint is also necessary.
For abscesses of the fingers and phlegmon of the rear, outpatient treatment is possible. In case of subgaleal processes, arthritis and osteomyelitis, urgent hospitalization is necessary due to the threat of spread of the purulent process in the proximal direction and to deeper anatomical structures.
Incisions for finger abscesses are made over the site of greatest pain, revealed by palpation with a button probe. To widen the purulent focus, arcuate or club-shaped incisions are made, allowing for complete excision of necrotic tissue. Treatment is continued in accordance with the general principles of management of purulent wounds. When localizing abscesses on the main phalanges, one should remember the possibility of infection spreading to the area of the interpalval spaces and the median fascial space of the sole through the canals of the lumbrical muscles, therefore, if necessary, the incisions are expanded in the proximal direction. To open the dorsal phlegmon, longitudinal incisions are made away from the dorsal artery. In this case, the skin and dorsal fascia are dissected, pus and necrotic tissue are removed, and the resulting cavity is drained. After adequate necrectomy, the operation can be completed by applying a drainage-washing system and primary sutures,
Common subfascial phlegmon of the dorsal foot is treated with an incision along the entire length, and if the tendon sheaths are involved in the process, the cruciate ligament is cut.
If the anterior fascial space of the leg is involved in the purulent process, an incision is made along the anterior surface of its middle third, 2 cm outward from the crest of the tibia. After cutting the skin, subcutaneous tissue and dense fascia through the muscles (between the tibialis anterior muscle and the long extensor digitorum) they penetrate into the perivascular tissue. In a common process, counter-aperture incisions are made through the entire muscle mass of this area for complete drainage. When inspecting a purulent cavity, the interosseous septum must be examined: if pus penetrates through holes or defects in it, it is necessary to open and drain the posterior fascial space of the leg.
For epifascial phlegmon of the sole, it is enough to make a small incision over the place of greatest swelling and pain, radically sanitize the abscess and complete the operation by applying a drainage-washing system (the ends of a perforated polyvinyl chloride tube are removed through punctures in healthy skin) and primary sutures on the skin.
To open the medial space, a Delorme incision is often used in the distal half, corresponding to the projection of the first metatarsal bone. Since infection of this space is prone to rapid spread, when pus enters through defects in the medial intermuscular septum, surgical intervention is supplemented by opening the median cellular space.
When opening the phlegmon of the lateral space, a Delorme incision is made in the distal half, according to the projection of the IV metatarsal bone. After evacuation of pus, necrectomy and sanitation of the wound, the lateral intermuscular septum is examined. If pus enters through defects, the median cellular space should be additionally opened.
One midline incision on the foot in the projection of the third metatarsal bone may not be enough, since the closure of the edges of the incision of the plantar aponeurosis and muscles leads to disruption of the outflow of pus. For adequate opening and drainage, it is advisable to make two lateral incisions in the projection of the vertical osteofascial bridges of the sole, then excise the necrotic areas of the bridges, creating conditions for better outflow of pus, and insert a drainage tube into the deepest part of the median space.
If purulent leaks are detected in the interdigital spaces, the opening of the ulcers is supplemented with a transverse incision in the distal part of the sole, in the area of the distal heads of the metatarsal bones (Fig. 33-6), and when the process moves to the rear - with contraperture incisions on the rear, most often between the II and III metatarsal bones .
When pus spreads into the deep fascial space of the leg (along the flexor tendons and the posterior tibial neurovascular bundle through the ankle canal), it must be opened. An obvious and frequent sign of proximal spread of infection is the appearance of pus in the subgaleal space of the sole when pressing on the lower third of the leg and the inner (medial) retromalleolar region. In this case, it is necessary to open the deep fascial space of the leg with an incision along the inner surface in its lower third, retreating 1 cm from the inner edge of the tibia. After opening the superficial fascia, the soleus tendon is shifted posteriorly and to the side, the internal fascia is exposed and dissected, and then the deep phlegmon is opened. Unfortunately, such separate opening of the deep fascial space of the leg and the subgaleal space can lead to necrosis of the flexor tendons of the ankle canal region. In these cases, a single incision is preferred, allowing access to the subgaleal space, internal malleolar canal and deep fascial space of the leg. The above incisions are combined by dissecting the anterior wall of the ankle canal.
Surgical treatment of combined phlegmon includes elements and features of the intervention technique on each of its components.
For acute purulent extensor tendovaginitis, surgical treatment, if necessary, consists of opening the fascial space of the rear. If the flexor tendons are damaged, the affected tendon sheath is immediately opened, since in these cases tendon necrosis quickly develops and the purulent process spreads to adjacent anatomical areas.
Surgical treatment of purulent arthritis depends on the location and degree of involvement of soft tissues in the process. More often, phlegmon of the foot on the dorsal side is opened. Having opened the deep fascia of the dorsum of the foot and provided good access to the joints, the affected bone structures are treated with a Volkmann spoon and a flow-through drainage-washing system is installed with the application of primary sutures to the skin. After 8-12 days, the drains are removed, and the immobilization of the foot is maintained for another 10-12 weeks.
In the treatment of acute hematogenous osteomyelitis of bones, priority is currently given to antibacterial therapy. If the de-escalation principle of antibiotic therapy is observed, by the 2-3rd day the body temperature is normalized, the pain stops and the sequestration process is stopped. The presence of sequesters and fistulas is an indication for surgical treatment (radical sequestrectomy) in accordance with the general principles of treatment of osteomyelitis. For osteomyelitis of the calcaneus, an incision is made from the Achilles tendon to the anterior edge of the bone through the entire thickness of the soft tissue. The bone is trepanned and cleaned from the inside, being careful not to damage the cortical layer. Loose cortical sequestra are removed by scraping out the residual cavity with a sharp spoon, and the soft tissue is sutured over the drainage placed in the resulting bone defect. In case of osteomyelitis of the talus, an anterior or posterior arthrotomy is performed with sanitation of the pathologically altered bone structure. In case of total damage to the talus, astragalectomy is performed.
Secondary forms of osteomyelitis, unlike hematogenous, are less acute, develop slowly and are not accompanied by large destruction of bone structures.
In the postoperative period, antibiotic therapy in combination with painkillers is indicated. Immobilization with a plantar plaster splint is required for 4-5 days until acute inflammation in the soft tissues resolves.
Source: ilive.com.ua
Symptoms of facial abscess
It looks like a swollen dome-shaped pimple with a white, purulent center. The skin around it is thin and easily injured. If you touch it, severe pain begins, and when you press it a little, pus comes out. The patient's condition does not deteriorate much. Located in the area of the temples, pharynx, deep inside the soft tissues, it is more severe with consequences. It is difficult to swallow, breathe, open your mouth, and intoxication may occur. Sometimes it can be fatal, especially in children.
The skin becomes pale and dry. Body temperature rises to 39°C, rarely to 40°C. The kids begin to feel weak. The first symptom of the disease is pain in the inflammatory area. Then the area swells and the body temperature rises.
The inflammatory focus forms a necrotic core, the skin around it is tense. The center of the shaft becomes filled with liquid pus. The edges of the inflamed area are clear. Sometimes the mucous membrane swells above the surface level. In order to correctly prescribe treatment, it is necessary to accurately diagnose this disease, not to confuse it with a boil, lymphadenitis, purulent atheroma, or chronic cyst.